Volume 22 Number 3
Case series exploring the healing effects of goat product consumption
Kelsey M Russell-Murray, Pat L Jones
Keywords wound healing, pressure injuries, long-term care, Goat milk, NPUAP, wound staging
DOI DOI: 10.35279/jowm202110.06
Abstract
Background Chronic wounds can have a substantial impact on quality of life, and their treatment and care can be costly. After witnessing the healing of a 4-year wound with the addition of goat’s milk consumption, it was decided to investigate further.
Aim To investigate whether the daily oral consumption of goat products is beneficial for promoting pressure injury healing among residents of long-term care (LTC) facilities.
Methods The subjects were permanent residents of an LTC facility with significant, long-lasting wounds, defined as any pressure injury at Stage 2 or more and existing for four or more months. Subjects were monitored for a six-month period. A total of 250 ml of goat dairy products were provided daily to each subject. Consumption was recorded daily. Wounds were monitored biweekly for size, stage, colour and change in condition. Participants were excluded if unable to complete the study or if less than 50% of the goat products were consumed over any month.
Results A total of 25 participants enrolled in the study; 17 completed the study, and 8 were excluded. A total of 24 pressure injuries were monitored from the 17 participants. Seventeen of the wounds closed during the six-month monitoring period.
Conclusions The results of the study indicate that consuming goat products may potentially promote pressure injury healing. Further study is needed.
Implications for clinical practice The results indicate that goat product consumption is feasible in an elderly population living in LTC, and it may have a positive effect on pressure injury healing. The treatment is minimally invasive and cost-effective.
INTRODUCTION
Chronic wounds in long-term care (LTC) settings can have a substantial impact on a person’s quality of life and well-being.1 Occurring in 10% of the LTC population and frequently under-reported, the economic cost of treating a single pressure injury ranged from CAD $26,800 to $231,000 in 2017 and can increase nursing hours up to 50% for wound treatment.2,3
Due to the complex association among wounds, infections and nutritional deficiency, diet has become part of a multidisciplinary approach to wound care, especially since elderly patients are at higher risk for nutritional deficits.4 While oral nutritional supplements have been previously studied in wound healing5, laypeople speculate that food products such as goat’s milk may also have healing benefits. Possible reasons could include similarities between goat and human milk, anti-inflammatory response and improved digestibility.6,7,8,9 Although research directly investigating the healing benefits of pressure injuries through the consumption of goat’s milk products has not been found in the literature, a study by Astha et al. used the probiotic VITSAMJ1, which was isolated from goat’s milk, as an effective topical intervention for wound healing in female Wistar rats.10 After witnessing the healing of a 4-year wound in an LTC setting with the addition of goat’s milk consumption, and supporting the Canadian Dietitians Food First initiative, we decided to explore the topic as a case series study.
Purpose
The purpose of this case series was to explore whether the daily oral consumption of goat products could be beneficial for promoting pressure injury healing for residents living in long-term care.
METHODS
This case series study took place in southern Ontario, Canada, between 2013 and 2016. Ethics approval was obtained from the LTC ethics committee. The study’s protocol conformed with the ethical guidelines of the Declaration of Helsinki (2013).
The participants in the study were permanent residents in LTC homes in southern Ontario, Canada with significant, long-lasting wounds, defined as any pressure injuries at Stage 2 or more that had existed for four or more months. The National Pressure Ulcer Advisory Panel Pressure Injury Staging System was used to determine each wound’s Stage.11 This tool is recommended by the Registered Nurses’ Association of Ontario Best Practice Guidelines.12
After informed consent was obtained from eligible study participants, those who consented to the study were provided a daily goat product at their preferred time. A total of 250ml of goat’s milk products were provided daily over a six-month period, in addition to participants’ usual nourishment routine. This volume was chosen based on other oral supplement studies with seniors.13
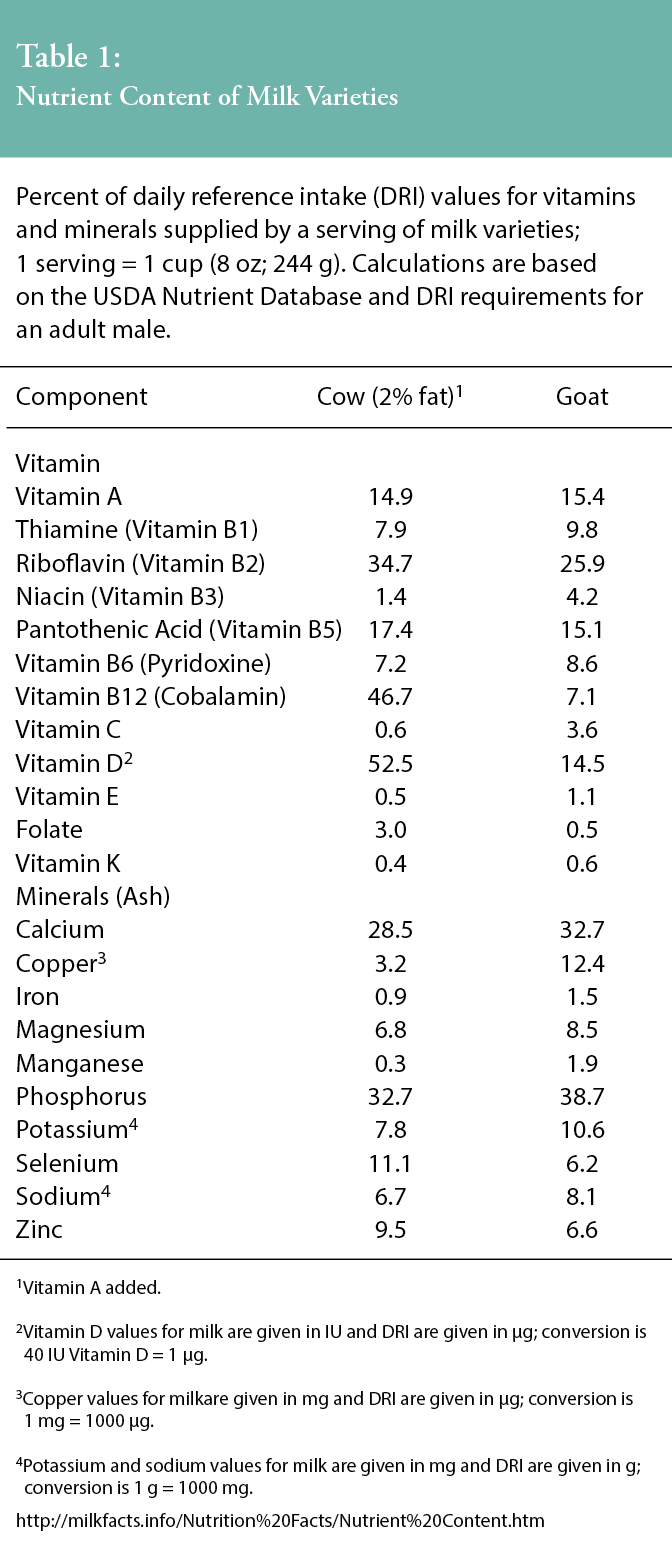
Present best practice nutritional guidelines for wound healing include providing Vitamin A, Vitamin C and zinc supplementation, as well as ensuring adequate calories, protein and fluid intake.14 Compliant with these guidelines, a standard 3.8% whole goat milk was used to provide approximately 168 calories, 10g of fat, 8g of protein and 14.9% of the daily nutritional requirement of Vitamin A in a 250-ml serving per day.14 The nutritional value for 250 ml of 2% cow milk is 122 calories, 4.8 g of fat, 8g of protein and 15.4% of the daily requirement of Vitamin A. See Table 1, Nutritional Comparison of Cow and Goat Milk to review the daily reference intake (DRI) values for vitamins and minerals supplied by a 250-ml serving of cow’s milk and a 250-ml serving of goat’s milk.14
Consumption was recorded daily in each participant’s medical administration record by the charge nurse or on flow sheets by the personal support workers, as per the LTC home’s preference. If a subject’s average goat product intake was less than 50% for any month, they were withdrawn from the study.
Dietitians’ comments about participating residents’ appetites and other observations affecting wound healing were collected. Wounds were monitored biweekly by the nurse in charge of wound care for changes in colour (black, yellow, red/pink) and size (centimetres) over the next six months. The addition of goat products to the diet was the only alteration made to the nutritional and wound care practices conducted in the LTC homes.
RESULTS
All of the subjects were between the ages of 58 and 95, retired and in need of some assistance with daily living. A total of 25 subjects initiated the study, and results are detailed in Table 2, Summary of Wound Status by Resident.
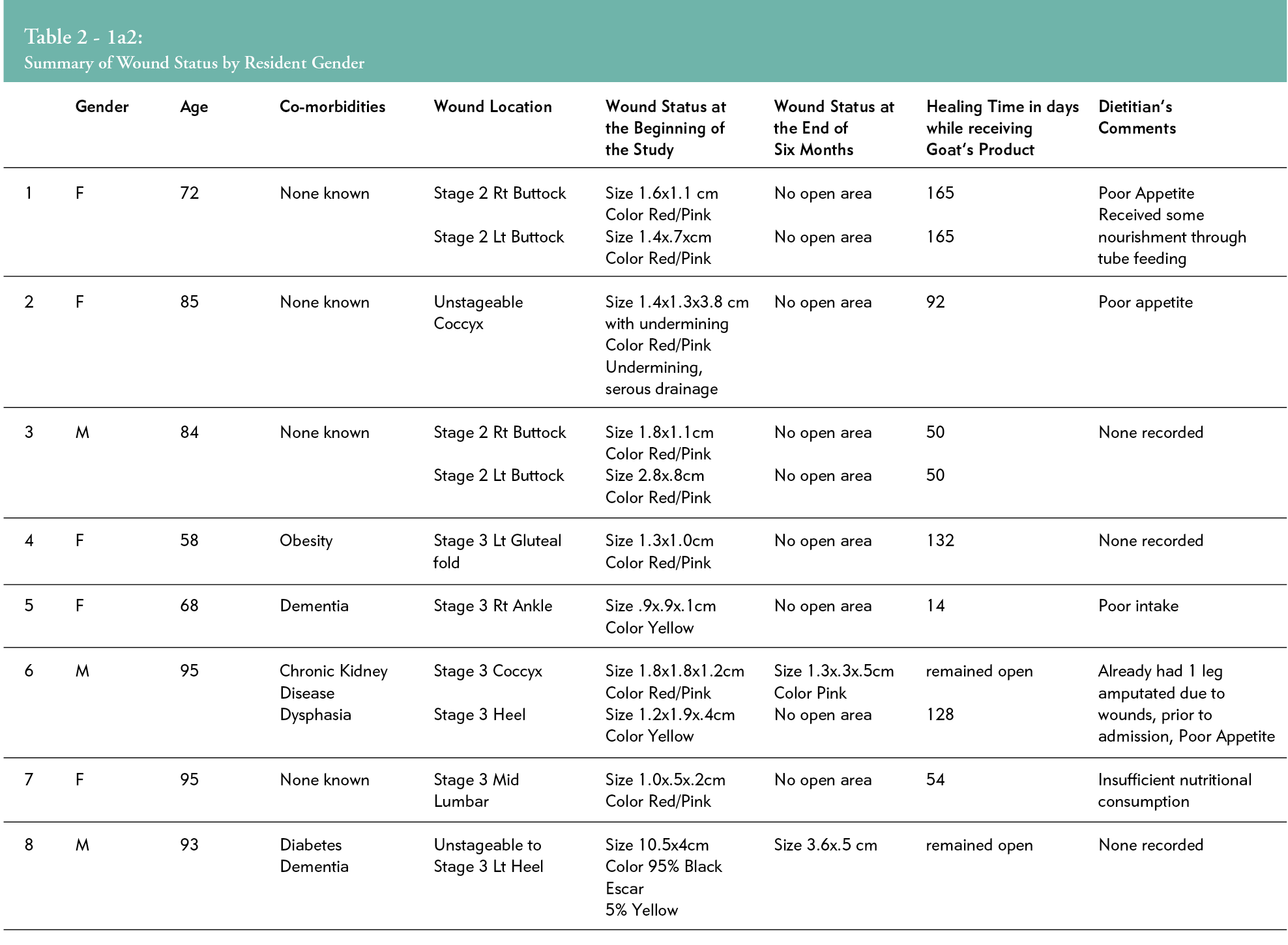
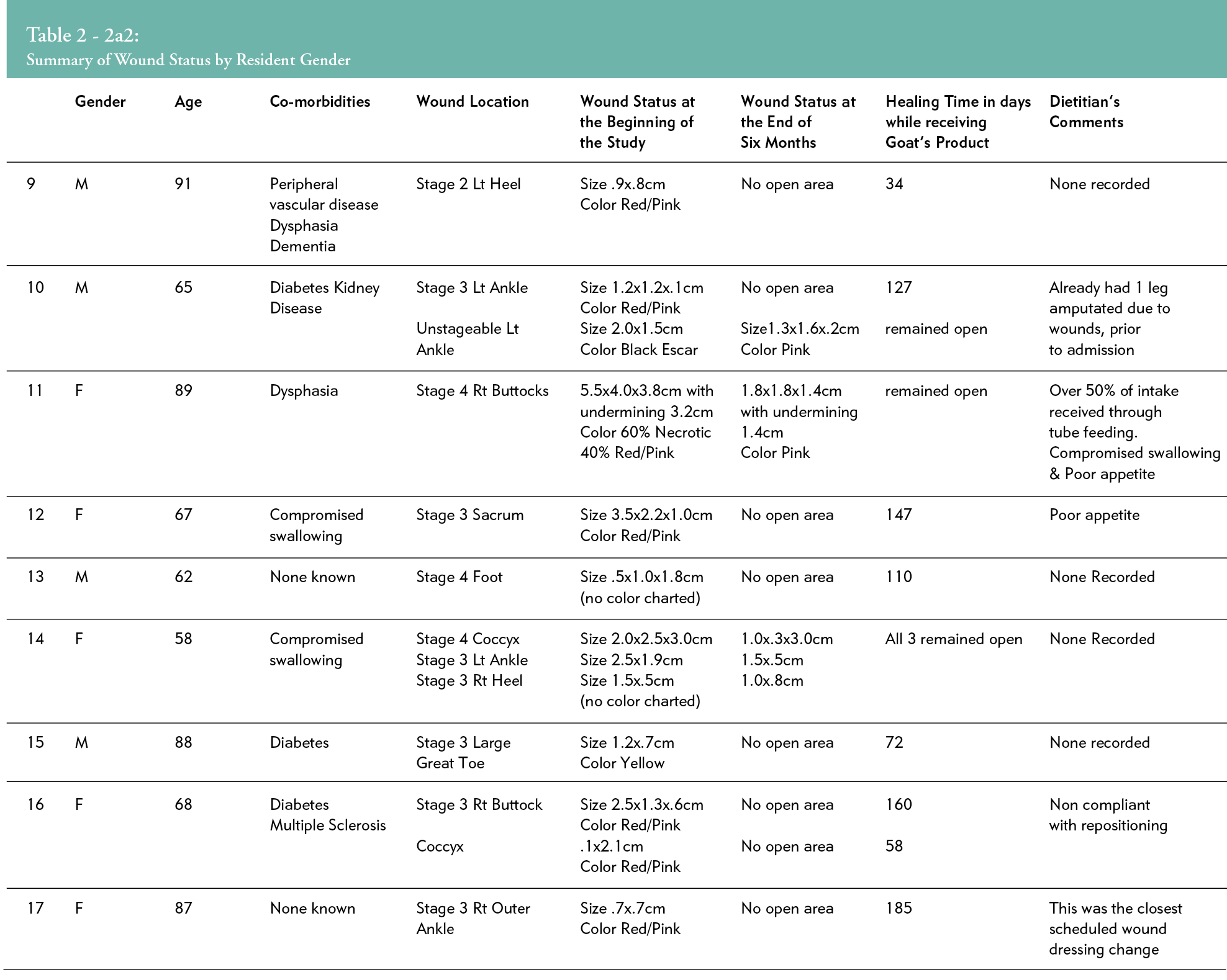
Eight participants passed away prior to the study’s completion (unrelated), and their data were excluded. Only one resident refused to participate because the study included the consumption of goat’s milk products. All participating residents exceeded the criteria of 50% goat product consumption per month, and none were withdrawn due to lack of consumption. Most (70.6%) were offered 125 ml of goat products twice daily, 23% preferred 250 ml once per day and 6.4% switched from 250 ml once per day to 125 ml twice per day part-way through the study. Even though the consumption of goat products was novel for most residents, all residents in the study met the goal intake without behavioural encouragement beyond routine care, indicating a general acceptance of the goat products. Seventeen subjects completed the study. Among them, a total of 24 pressure injuries were tracked. Data included six Stage 2, twelve Stage 3, three Stage 4 and three Unstageable injuries. Of the 24 pressure injuries, five wounds closed in 8 weeks (29%), nine closed in 4 months (38%) and 16–17 wounds healed over 6 months (67–71%). Of the remaining seven wounds, five showed improvement, and only two wounds failed to improve. Wound healing times varied significantly (from 14 days to 165 days, and one patient had a closed wound not assessed until 185 days), as is expected when considering uncontrolled variables in the practice setting. See Table 2, Summary of Wound Status by Resident.
DISCUSSION
While we were initially sceptical, based on anecdotal reports, the results of the case series seem to warrant further evaluation of the properties of goat milk products for wound healing. This case series study aimed to monitor wound healing progress in a group of subjects who had similar long-standing pressure injuries and received daily oral consumption of goat products over a six-month period. While other studies have evaluated oral nutritional supplementation and wound healing in the elderly with positive results13, ours is the first to consider the addition of goat’s milk products. These results can be used to generate hypotheses for future studies.
As a case series led by allied health practitioners, we recognise several study limitations. Due to the lack of a control group, no causal inferences can be made regarding the efficacy of the investigated treatment.16 Medical conditions that are known to impact a participant’s ability to heal, such as diabetes, malnutrition, obesity and reduced mobility should be acknowledged. As well, previous dairy consumption, commercial oral nutritional supplementation and vitamin and mineral intake were not monitored, but are another consideration for future research. The use of antibiotics, repositioning devices, resident mobility and pressure ulcer (PU) risk score tracking should also be considered in future research. In this study, it was assumed that all wounds, whether Stage 2, 3, 4 or unstageable, were considered equal. Concurrent nursing interventions to promote wound healing were not prohibited.
Many of these wounds had been open for months, prior to the participant’s admission into LTC, and residents/caregivers were unsure of the length of time. Considering the age and co-morbidities of this group, wound stages, size and longevity, it would seem that the closing rate of 71% within six months, after the addition of goat’s milk to the diet, would be more than acceptable. As of January 2021, the price of goat’s milk purchased from a large, popular LTC supplier was $2.84/L. The cost of a leading nutritional supplement from the same supplier, at the same date, was $5.73/L.
CONCLUSION
Although the findings are preliminary, the results of
this case series indicate goat product consumption may potentially promote pressure injury healing. This treatment is cost effective, non-invasive and well accepted by LTC residents. More studies are encouraged to investigate this nutritional support in wound treatment.
IMPLICATIONS FOR CLINICAL PRACTICE
The results of this study indicate that goat product consumption is feasible in an elderly population living in LTC, and it may have a positive effect on pressure injury healing. The treatment is minimally invasive and cost-effective. Additionally, it supports the Dietitians of Canada’s Best Practices of the Food First initiative.16 We invite more research in this area.
Implications for clinical practice and further research
Residents and caregivers should be informed that signs of wound improvement often take six or more weeks to develop following the commencement of goat product intake.
Future research in this area should endeavour to collect data such as a patient’s medical condition, diagnosis, PU scores, previous dairy consumption, body mass index, additional supplements, mobility, repositioning devices, treatments and medications.
Acknowledgements
Thanks to Tracy Robinson for providing editorial guidance, writing assistance and for proofreading the article.
KEY MESSAGES
- Consumption of goat products may have a positive effect on pressure injuries.
- The methodology supports the Dietitians of Canada’s Best Practices of the Food First initiative.
- This treatment is minimally invasive and cost-effective, and goat milk is well tolerated in an elderly population in long term care.
Author(s)
Kelsey M Russell-Murray
RD, MSc, HBSc, Registered Dietitian, St Thomas Elgin General Hospital
Pat L Jones
RD, BASc, Registered Dietitian, McGarrell Place
Correspondence: pjones@start.ca
Conflicts of Interest: Pat Jones was on the board that provided ethics approval for the research.
Hewitt Dairy provided goat milk free of charge to some of the LTC homes.
References
- Gorecki C, Brown JM, Nelson EA, Briggs M, Schoonhoven L, Dealey C, et al. Impact of pressure ulcers on quality of life in older patients: A systematic review. J Am Geriatr Soc 2009 Jul; 57(7):1175–83.
- Denny K, Lawand C, Perry SD. Compromised wounds in Canada. Healthc Q 2014; 17(1):7–10.
- Clarke HF, Bradley C, Whytock S, Handfield S, Van Der Wal R, Gundry S. Pressure ulcers: Implementation of evidence‐based nursing practice. J Adv Nurs 2005 Mar; 49(6):578–90.
- Donnelly J, Shaw J. Developing a multidisciplinary complex wound care service. Br J Nurs 2000 Oct; 9(19 Suppl):S50–1, S53, S55.
- Serena TE, Yaakov RA, DeLegge M, Mayhugh TA, Moore S. Nutrition in patients with chronic non-healing ulcers: A paradigm shift in wound care. Chronic Wound Care Manag Res 2018; (5):5–9.
- Robinson F. Goats milk – a suitable hypoallergenic alternative? Br Food J 2001; 103(3):198–208.
- Kiskini A, Difilippo E. Oligosaccharides in goat milk: Structure, health effects and isolation. Mol Bio Cell 2013; 59(1):25–30.
- Jirillo F, Magrone T. Anti-inflammatory and anti-allergic properties of donkey’s and goat’s milk. Endocr, Metab Immune Disord 2014; 14(1):27–37.
- Park, YW. Relative buffering capacity of goat milk, cow milk, soy-based infant formulas, and commercial nonprescription antacid drugs. J Dairy Sci 1991; 74(10):3326–33.
- Astha S, Shakti S, Madhumathy M, Jabez Osborne W. Probiotic bacteria in wound healing; An in-vivo study. Iran J Biotechnol 2019 Dec; 17(4):e2188.
- Edsberg LE, Black JM, Goldberg M, McNichol L, Moore L, Sieggreen M. Revised national pressure ulcer advisory panel pressure injury staging system: Revised pressure injury staging system. J Wound Ostomy Continence Nurs 2016 Nov/Dec; 43(6):585–97.
- Registered Nurses’ Association of Ontario [Internet]. [cited: 21 Sep 2020]. RNAO Best Practices: Risk Assessment & Prevention of Pressure Ulcers. Available at: https://rnao.ca/bpg/guidelines/risk-assessment-and-prevention-pressure-ulcers
- Collins CE, Kershaw J, Brockington S. Effect of nutritional supplements on wound healing in home-nursed elderly: A randomized trial. Nutrition 2005 Feb1; 21(2):147–55.
- Hurd, TA. Nutrition and wound-care management/prevention. Wound Care Canada 2004; 2(2):20–4.
- Milk Facts [Internet]. USA. [cited 2021 Sept 8]. Table 3; Available at: http://milkfacts.info/Nutrition%20Facts/Nutrient%20Content.htm
- Mann CJ. Observational research methods. Research design II: cohort, cross sectional, and case-control studies. Emerg Med J 2003; 20:54–60.
- Dietitians of Canada [Internet]. Best practices for nutrition, food service, and dining In LTC homes 2019 A working paper of Ontario LTC Action Group 2019 Available at: https://www.dietitians.ca/DietitiansOfCanada/media/Documents/Resources/2019-Best-Practices-for-Nutrition,-Food-Service-and-Dining-in-Long-Term-Care-LTC-Homes.pdf
