Volume 22 Number 3
A community-based approach to the prevention of pressure injuries: A study supported by the European Wound Management Association Research Grant
Vildan Çakar, Ayişe Karadağ
Keywords prevention, education, pressure injuries, pressure ulcers, Digital gamification
DOI 10.35279/jowm202110.08
Abstract
Pressure injuries (PIs) are important health problems all over the world because of their serious effects. Awareness of PIs and their effects has increased in recent years. Since patients’ relatives are part of the care team, they have an important role to play in the prevention of PIs. The most crucial aspect of the prevention of PIs is the education of healthcare professionals, patients and patients’ relatives and caregivers. This study aimed to educate caregivers on the prevention of PIs through the development of a digital game. With this purpose, we developed and used a technological education approach —a digital game— that employs gamification methods.
INTRODUCTION
A pressure injury (PI) is defined as localised damage to the skin and/or underlying tissues, usually over a bony prominence or related to a medical device and/or other devices, due to intense and/or prolonged pressure or pressure in combination with shear. Soft tissue tolerance to pressure and shearing forces are affected by microclimate, perfusion, age, nutrition, acute or chronic health status, comorbidities, soft tissue conditions and a number of contributing or confounding factors associated with PIs, the most important of which is impaired mobility. Patients with limited mobility and those patients confined to bed are at a risk of developing PI.1
The prevalence of PI varies by country and clinical setting (acute care, long-term care, community health care, etc.).1 The overall prevalence of PIs has been determined to be 15.0% in the United States2,3, 10.8% in European countries4, 26.0% in Canada5 and 7.9% in Australia.6 In a point prevalence study on acute care with the largest sample, in which patients from 12 centres from different provinces of Turkey were included (n=5,088), the overall prevalence of PIs was found to be 9.5%.7 In acute care, a systematic review (n=42) by Li et al. (2020) reported that the pooled prevalence and incidence rates of PIs were 12.8% and 5.4% per 10,000 patient-days, respectively.8 In studies on home care conducted in Australia, Belgium and England, the prevalence of PIs was determined to be between 6.8 and 13.0%.6,9,10,11 In a cross-sectional descriptive study that included patients (n=786) receiving services from the home care unit of a training and research hospital in Turkey, the rate of PIs was found to be quite high, 29.8%.12
PIs are considered a major public health problem due to their undesirable effects, such as increased mortality and morbidity, increased healthcare costs, prolonged hospital stay and reduced quality of life for the patients and their families.13,14,15 These negative effects have led to an increased awareness regarding the implementation of prevention strategies.13,16 The evaluation of patients’ risk of developing PI; assessment and proper care of the skin; measures to reduce the effects of pressure, friction and shear; regulation of nutrition; and continuing education practices are among the strategies for the prevention of PIs.1,2,3
Studies on the prevention of PIs can be difficult, especially due to the lack of access to resources and opportunities for education in home care.16 In the home care process, patients’ relatives often take on significant tasks as caregivers.17,18 They play a supportive role in this process by being included in the care team, ensuring the coordination and continuity of care17,19 and in the success of person-centred PI prevention strategies.20 In this context, the education of healthcare professionals and patients’ relatives constitute the most important stage in the implementation of PI prevention strategies and for ensuring compliance with these strategies.1,16,20
A wide variety of methods and approaches, such as classroom education, web-based education and distance education, are used in the education of healthcare professionals, especially nurses, for the prevention of PIs.21,22 Today, along with technological advancements in all aspects of life, there have been innovations and developments in education methods applied in all fields of health. In this context, the concept of digital education has begun to be used and investigated.23,24
It is important to include patients’ family members in all care processes to ensure the success of the disease management efforts and the improvement of health.19 Within the scope of this practice, which constitutes the basis of the person-centred care philosophy17,19, it is necessary to educate, strengthen and increase the health culture of any relatives who take care of the patient.17 A significant contribution can be made to this process with the use of comprehensible, easily accessible and usable, scientific knowledge-based technological education approaches.25 Although there are more innovative methods and studies used for the education of health professionals on PIs21,22, the number of studies on the education of patients and their relatives is limited.16
It is important to educate patients’ relatives, as they are members of the care team, about the prevention of PIs and to develop innovative technology-based approaches in these education efforts, since they play an important role in the care team. Our clinical experiences and observations indicate that encouraging and entertaining educational materials used in the education of patients’ relatives is supportive in increasing their participation and compliance with educational activities. Within the scope of this study, we aimed to develop a digital medical game (DMG), which uses the gamification approach and is among the most-used technological education methods, for the education of patients’ relatives on the prevention of PIs.
Study procedure
This doctoral project, supported by a research grant provided to young researchers by the European Wound Management Association (EWMA), is carried out in three stages (Figure 1). Ethical approvals and permissions for the study were obtained, and the pilot test stage for the DMG was initiated.
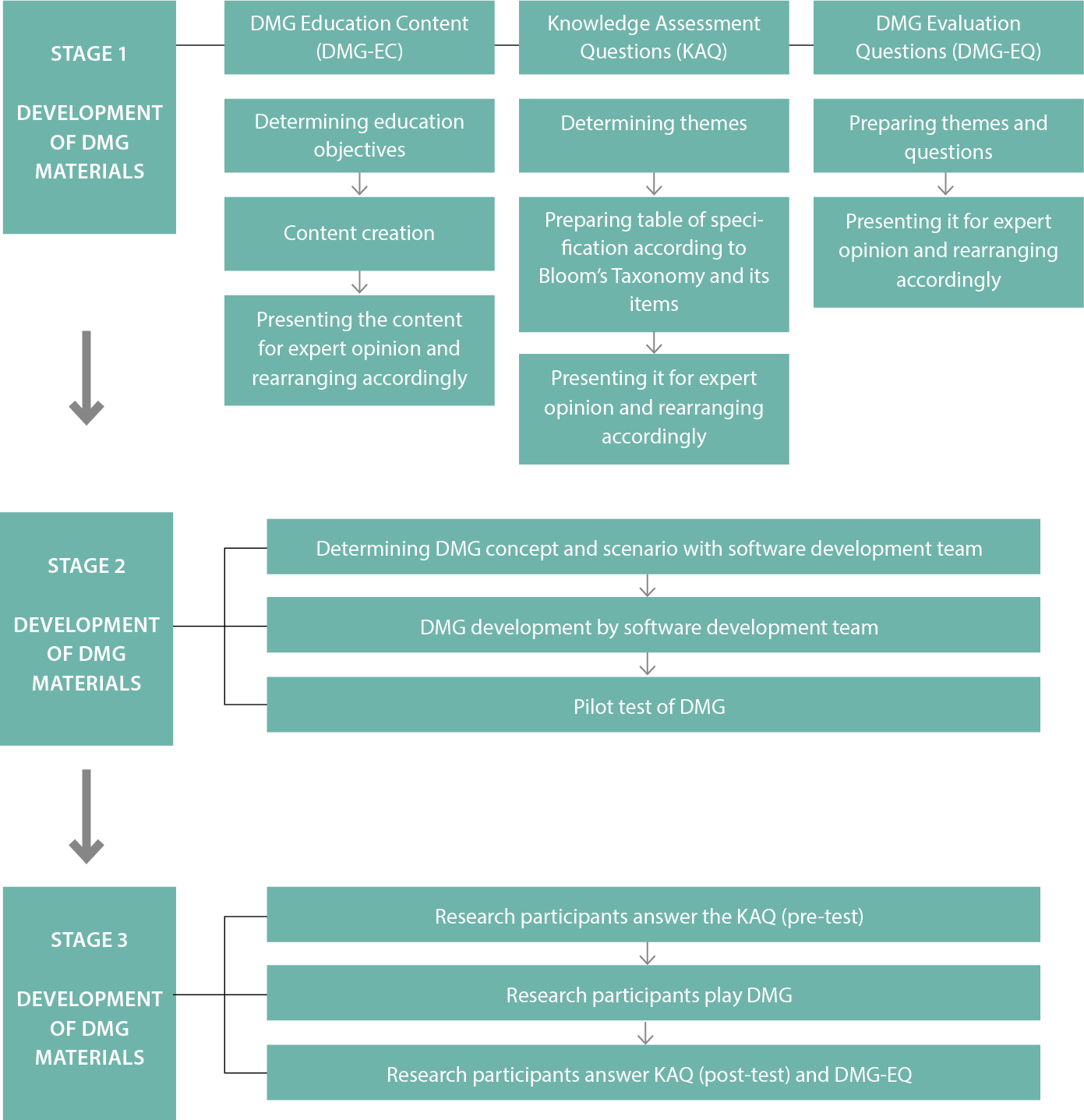
Figure 1: Study Flow Diagram
The original language of the game developed as part of this study was designed in Turkish, and English subtitles were added, with the idea of providing an opportunity for its use among a wider population.
After the completion of the DMG’s pilot test, Stage 3 of the study (Implementation of the DMG) will be initiated. The study participants for inclusion in Stage 3 will consist of relatives of the patients receiving home care services and hospital care. Interviews are currently being conducted by the researcher to determine eligible participants from among a pool of volunteer patient relatives.
KEY MESSAGES
- Pressure injuries (PIs) are a major health problem all over the world.
- The education of patients’ relatives and healthcare professionals is important for the prevention of PIs.
- It is necessary to develop innovative methods and approaches to the education of patients’ relatives on the prevention of PIs.
Author(s)
Vildan Çakar, RN, MSc, PhD Student in Nursing, Research Assistant, Koç University, Graduate School of Health Sciences,
Koç University Health Sciences Campus, Davutpasa Str. Topkapı, Istanbul, Turkey
Ayişe Karadağ, RN, ET/WOCN, PhD, Professor in Nursing, Advisor, Koç University, School of Nursing,
Koç University Health Sciences Campus, Davutpasa Str. Topkapı, Istanbul, Turkey
Correspondence: vcakar18@ku.edu.tr
Conflicts of interest: None
References
- European Pressure Ulcer Advisory Panel, National Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and treatment of pressure ulcers/injuries: Clinical practice guideline. Emily Haesler (Ed.). City: EPUAP/NPIAP/PPPIA; 2019.
- Berlowitz D, Lukas CVD, Parker V, Niederhauser A, Silver J, Logan C, et al. [Internet]. Preventing pressure ulcers in hospitals: A toolkit for improving quality of care. Agency for Healthcare Research and Quality. Available from: https://www.ahrq.gov/patient-safety/settings/hospital/resource/pressureulcer/tool/index.html.
- Institute for Healthcare Improvement. How-to guide: Prevent pressure ulcers. Cambridge, MA: Institute for Healthcare Improvement; 2011.
- Moore Z, Avsar P, Conaty L, Moore DH, Patton D, O’Connor T. The prevalence of pressure ulcers in Europe, what does the European data tell us: A systematic review. J Wound Care 2019; 28(11)Epub.
- Norton L, Parslow N, Johnston D, Ho C, Afalavi A, Mark M, et al. Foundations of best practice for skin and wound management. Best practice recommendations for the prevention and management of pressure injuries. City: Canadian Association of Wound Care; 2018.
- Clinical Excellence Commission. 2018 NSW pressure injury point prevalence survey report. Sydney: Clinical Excellence Commission; 2019.
- Baykara ZG, Karadağ A, Bulut H, Öztürk D, Avşar P, Duluklu B, et al. [Internet]. Pressure injuries prevalence in Turkey: A multicenter study. Wound Ostomy Incontinence Nurses Society of Turkey. Available from: https://www.yoihd.org.tr/sayfa.aspx?id=142.
- Li Z, Lina F, Thalibb L, Chaboyer W. Global prevalence and incidence of pressure injuries in hospitalised adult patients: A systematic review and meta-analysis. Int J Nurs Stud 2020; 105:103546. doi: 10.1016/j.ijnurstu.2020.103546
- Paquay L, Wouters R, Defloor T, Buntinx F, Debaillie R, Geys L. Adherence to pressure ulcer prevention guidelines in home care: A survey of current practice. J Clin Nurs 2008; 17(5):627–36.
- Stevenson R, Collinson M, Henderson V, Wilson L, Dealey C, McGinnis E, et al. The prevalence of pressure ulcers in community settings: An observational study. International J Nurs Stud. 2013; 50(11):1550–7. doi:10.1016/j.ijnurstu.2013.04.001
- Hopkins A, Worboys F. Establishing community wound prevalence within an inner London borough: Exploring the complexities. J Tissue Viability 2015; 23(4):121–8. doi:10.1016/j.jtv.2014.10.002
- Çubukçu M. Evaluation of risk factors for pressure injuries in home care unit patients. Biomed Res 2018; 29(17):3288–91.
- Demarré L, Van Lancker A, Van Hecke A, Verhaeghe S, Grypdonck M, Lemey J, et al. The cost of prevention and treatment of pressure ulcers: A systematic review. Int J Nurs Stud 2015; 52(11):1754–74.
- Rodrigues AM, Ferreira PL, Ferre-Grau C. Providing informal home care for pressure ulcer patients: How it affects carers’ quality of life and burden. J Clin Nurs 2016; 25(19–20):3026–35.
- Spilsbury K, Nelson A, Cullum N, Iglesias C, Nixon J, Mason S. Pressure ulcers and their treatment and effects on quality of life: Hospital inpatient perspectives. J Adv Nurs 2007; 57(5):494–504.
- Ellis M. Pressure ulcer prevention in care home settings. Nurs Older People 2017; 29(3):29–35.
- Kokorelias KM, Gignac MAM, Naglie G, Cameron JI. Towards a universal model of family centered care: A scoping review. BMC Health Serv Res 2019; 19:564. doi:10.1186/s12913-019-4394-5
- Probst S, Seppänen S, Gerber V, Hopkins A, Rimdeika R, Gethin G. EWMA Document: Home care-wound care. J Wound Care 2014; 23(5th Suppl.):1–S44.
- Lor M, Crooks N, Tluczek A. A proposed model of person, family, and culture-centered nursing care. Nurs Outlook 2016; 64(4):352–66. doi:10.1016/j.outlook.2016.02.00
- Pokorna A, Klugar M, Kelnarova Z, Klugarova J. Effectiveness and safety of patient-centred care compared to usual care for patients with pressure ulcers in inpatient facilities: A rapid review. Journal of the European Wound Management Association 2019; 20(1):61–70. doi:10.35279/jewma201905.07
- Beeckman D, Schoonhoven L, Fletcher J, Furtado K, Heyman H, Paquay L, et al. Pressure ulcers and incontinence-associated dermatitis: Effectiveness of the pressure ulcer classification education tool on classification by nurses. Qual Saf Health Care. doi:10.1136/qshc.2008.028415
- Bredesen IM, Bjøro K, Gunningberg L, Hofoss D. Effect of e-learning program on risk assessment and pressure ulcer classification-A randomized Study. Nurse Educ Today 2016; (40):191–7. doi: 10.1016/j.nedt.2016.03.008
- Friesgaard KD, Paltved C, Nikolajsen L. Acute pain in the emergency department: Effect of an educational intervention. Scand J Pain 2017; 15:8–13. doi: 0.1016/j.sjpain.2016.11.004
- Yao K, Uedo N, Muto M, Ishikawa H, Cardona HJ, Filho ECC, et al. Development of an e-learning system for the endoscopic diagnosis of early gastric cancer: An international multicenter randomized controlled trial. EBioMedicine 2016; 9:140–7. doi:10.1016/j.ebiom.2016.05.016
- Satterfield HM. Technology use in health education: A review and future implications. The Online Journal of Distance Education and e-Learning. 2015; 3(2):87-96.
