Volume 22 Number 3
Deep vein insufficiency and the results of four-layer compression bandages in the treatment of venous ulcers: A retrospective study
Dr Alberto Garavello, Dr Pietro Franzvea, Dr Massimo Tozzi, Stefania Gilardi, Paola Fiamma
Keywords Chronic Venous Insufficiency, four-layer bandage, venous ulcers
DOI 10.35279/jowm202110.03
Abstract
Background Venous ulcers of the lower limbs affect 1 to 3% of the Western population; at present, elastic compression is the first line of therapy. Some authors have found that insufficient deep venous circulation may delay ulcer healing during compression therapy.
Hypothesis/aim In a group of patients with venous ulcers, we verified whether or not deep venous insufficiency (DVI) associated with superficial venous insufficiency (SVI) may worsen the outcomes of four-layer elastic compression bandage (4LB).
Methods A total of 124 patients participated in the study. Ecocolordopper results of superficial and deep venous circulation examinations and the patient’s data, including age, sex and clinical history, were collected in an Excel database. A 4LB was applied, and patients were checked twice per week at our clinic, where therapeutic outcomes were recorded.
Results/Findings In 62 patients, we found only SVI (66.9%), DVI in 42 patients (33.9%, 38 popliteal veins, 17 femoral veins) and both SVI and DVI conditions in 26 patients (20.9%). In patients with SVI alone, the mean healing time was 81 ± 91 days, and in patients with DVI associated with SVI, it was 108 ± 123 days; the difference between the two groups was not statistically significant (p> 0.2). Ulcer healing was achieved in 90 patients— 41 with SVI alone, 21 with SVI combined with DVI; the difference was not statistically significant.
Conclusions Using 4LB allows ulcer healing with no difference in outcome between patients with SVI alone and those with SVI associated with DVI.
Implication for clinical practice A 4LB is effective in varicose ulcer therapy; the caregivers’ skills are critical, and home assistance for elderly patients is needed because too many live far from the hospital and cannot follow the therapy protocols on their own.
Abbreviations
DVI –Deep venous insufficiency
SVI – Superficial vein insufficiency
4LB –Four-layer bandage
INTRODUCTION
Ulcers of the lower limbs are the most severe stage of chronic venous insufficiency and are present in 1–3% of the Western population.1 Compression is the first line of therapy for this condition, and a review of the most recent literature has demonstrated its effectiveness in both treatment and preventing recurrence. Healing, the resolution of pain and oedema occur by restoring valve continence, reducing venous hypertension, reflux and improving lymphatic outflows from the limb.2,3 Every bandaging technique has its supporters; a caregiver’s skills and a patient’s compliance with compression pressure play a critical role in its success. The 4-layer bandage (4LB) is currently one of the most popular techniques, and randomised studies have demonstrated its cost-effectiveness. Elastic stockings, despite the results of some trials, have not shown a clear superiority over bandaging. Superficial venous insufficiency (SVI) can lead to the onset of an ulcer; however, in some patients, an ecocolordoppler examination (ECD) has shown a primitive or post-thrombotic deep venous insufficiency (DVI), with haemodynamic damage. Some authors have highlighted how DVI may delay ulcer healing during compression therapy3,4,5,6,7,8, while others have reported the favourable outcomes of multicomponent 4LB in these patients.9 In our paper, we examined patients with venous leg ulcer who were treated with a 4-layer multicomponent bandage to evaluate whether the presence of DVI associated with SVI may worsen healing time and recurrence rates.
METHODS
At the Center for Ulcer Therapy at San Filippo Neri Hospital, in Rome, 124 patients with venous ulcers were examined between January 2016 and December 2019; all underwent an ECD examination of the lower limbs with an Esaote MyLab Five (Esaote SpA Genoa - Italy), following International Union of Angiology guidelines.10 Preliminary examinations excluded the presence of arterial disease (ABI <0.8) and other causes of ulcers (connective tissue diseases, skin cancers, etc.). Patient data, including age, sex, clinical history, previous phlebological surgery (stripping and/or phlebectomy of varicose tributaries) and ECD results were collected in an Excel file. Informed consent was obtained from each patient before treatment. This study’s protocol conformed to the ethical guidelines of the Declaration of Helsinki and was approved by the hospital’s ethics committee. Data collection was performed using PASW Statistics version 18.0 (SPSS Inc, Chicago, Ill). Categorical data are presented as number and percentage; categorical variables were analysed using Fisher’s exact test and continuous variables were analysed with the Student’s t-test. Normally distributed continuous data are indicated as mean standard deviation, while normally undistributed continuous data are indicated as median and interval. A P-value <.05 indicated statistical significance. Finally, all patients began elastic compression therapy using a 4-layer multi-component bandage11, with checks and ulcer cleaning twice per week. The endpoint was the complete re-epithelialisation of the ulcer, without eschar and the need for dressing. Debridement of the ulcer and necrotic tissue were obtained either by ‘shaving’ with a scalpel (under local anaesthesia with 5% lidocaine ointment) or a hydrogel*; in very rare cases, exuding lesions were treated with silver sulfadiazine spray.** The skin over the leg bones (when necessary) was protected with a pad*** before applying the bandage layers. No medical therapy was used. The four bandage layers were as follows:
1) A German cotton or, in the case of an allergy, tubular cotton band to cover and fix the dressing to absorb the exudate.
2) Elastocrepe****
3) and 4) A bandage kit composed of one short and one long stretch bandage, with a visual control system to ensure the correct application of 40 mmHg pressure at the ankle.
The bandage was applied by specially trained personnel starting from the base of the toes in a figure eight motion, extending to the upper part of the leg.
RESULTS
A total of 124 lower limb patients with venous ulcers (CEAP6) were evaluated; the patients’ mean age was 57.5 years (range 29–91), with a female predominance (n=75 female patients, 60.5%). Twenty patients had stripping of the right great saphenous vein, one to phlebectomy, 16 to stripping of the left great saphenous vein. SVI was detected in 62 patients (66.9%), DVI in 42 patients (33.9%, n=38 popliteal vein, n=17 femoral vein) and both SVI and DVI in 26 patients (20.9%).
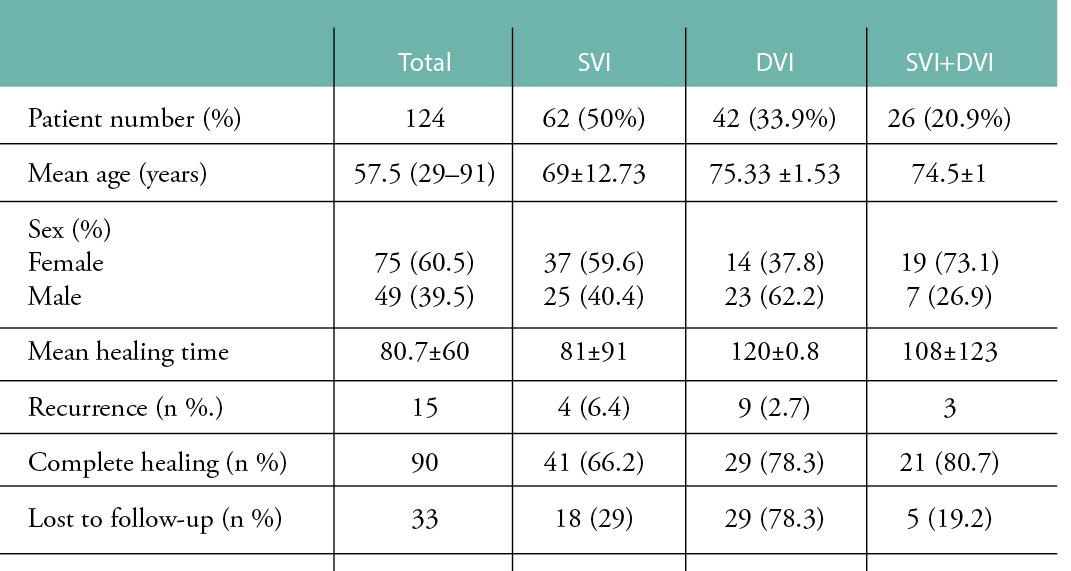
Table 1 reports the general data on the patients. The mean healing time was 80.7 ± 60 days; in patients with SVI alone, the mean healing time was 81 ± 91 days, in patients with SVI associated with DVI it was 108 ± 123 days. The difference between the two groups was not statistically significant (p> 0.2). In 15 patients, the ulcer recurred, and in seven of these, it did so during the study period. In four of these cases, there was only one with SVI, while in three patients there was both SVI and DVI; the difference was not statistically significant (p> 0.42). Healing was achieved in 90 patients, 41 who were affected only by SVI, 21 with SVI and DVI; the differences were not statistically significant. By the end of the study, 33 patients had withdrawn for personal reasons, and one patient died of a stroke. The results presented are based on the number of patients at the start of the study.
Table 1: Results of 4LB compression in 124 patients
DISCUSSION
Compression therapy is the treatment of choice for venous leg ulcers. A review of the literature, such as that found in the Cochrane database, highlighted the effectiveness of high pressure, multilayer bandages with an elastic component and showed how 4LB achieves faster healing.12,13,14 These papers were influenced by heterogeneous factors, such as ulcer size, the nurse’s skills in bandage techniques and the patient’s tolerance of compression; therefore, it is difficult to standardise results for comparison.15,16 However, the need for elastocompression is now definitively acquired in ulcer therapy, even though in a 2016 survey by Protz17, only one-third of patients suffering from leg ulcer underwent compression or therapy with an elastic stocking.
All ulcers in the present study were debrided during the study period. Ulcer debridement is crucial for treatment13, but it is not often cited in the literature; we used surgical and/or enzymatic methods according to local conditions, with topical anaesthesia of 5% lidocaine. Ulcer disease may become chronic and often recurs; 30% of ulcers do not heal within six months1, while recurrence is frequent, occurring in 20 to 70% of cases. Surgical treatment lowers recurrence;18–11 however, most of our patients are elderly and refused to undergo surgery, so compression was the only choice. The insufficiency of deep venous circulation, and in particular of the popliteal vein, is a critical factor in healing, due to its importance in the effectiveness of calf pumping.6,7,8
The 4LB technique is the gold standard in the UK; its main advantages are its favourable cost–benefit ratio, few complications and shorter duration of therapy.13,19,12,14,21,22,16,20 Some of the problems with the technique are the need for a skilled caregiver, possible slipping while walking and the bandage’s volume, which can make it difficult to put on shoes or clothing.23,14,24 However, we found that, for elderly patients, who often lack help from a caregiver or relatives, it is extremely difficult to wear an elastic stocking; furthermore, in highly exuding lesions, management of stockings may be problematic, due to the frequent changes required. Other authors have highlighted that compression with stockings may not be suitable for all patients24 and is a cause of their abandoning therapy. Despite the favourable results of some studies, elastic stockings did not show a clear superiority in ulcer healing.23,13,12-17,21 Ashby, in a randomised study on ‘stocking vs. four-layer bandage’, highlighted how, with similar therapeutic outcomes, the stocking group had a higher rate of therapy abandonment.24 Finlayson found similar results on healing with 4LB therapy25; excellent tolerability was also found in a randomised study by Moffat in which 4LB proved advantageous from a cost point of view.20
In our experience, 4LB produces comparable outcomes in patients with SVI and in those with SVI combined with DVI; our healing times are comparable to those reported by other authors.24,22,14 With this in mind, it seems that other factors apart from haemodynamics play a role in the success of therapy; concomitant disease, compliance with treatment, the ability to walk, essential action of the bandage and patient involvement in the programme are critical for healing.25, 26,5 In fact, it should be noted that 33 patients in our study discontinued therapy, which is certainly not a negligible percentage; some did so because of local problems (difficulty in accessing the hospital), while others left due to health problems or a lack of confidence in the therapy. This supports the hypothesis that factors such as the availability of assistance for access to the treatment also plays a role in ulcer healing.24,26
CONCLUSION
In our experience, the 4LB technique allowed the same healing time for patients with SVI alone and in those with DVI combined with SVI; however, a critical factor for success is the experience and competence of the caregiver applying the bandage, as highlighted by several authors. Although surgical therapy has proved effective in preventing relapses, the age of the patients, which is often advanced, often leads them to refuse surgery. Studies on elastic compression have focused on the Achilles heel with different sizes of ulcers and, above all, the experience of the operator; this limitation is difficult to resolve, and is unfortunately a part of the nature of this pathology. The non-negligible percentage of patients who leave therapy suggests that home care will have to be increasingly implemented in the future, because of the difficulty elderly patients have accessing such a complex therapy that requires careful regular follow-up.
IMPLICATIONS FOR CLINICAL PRACTICE
- The 4LB technique seems to be an effective therapy for the treatment of venous ulcers, even in the presence of insufficient deep venous circulation.
- Although surgical therapy allows a reduction in ulcer recurrence, elderly patients often refuse surgery; in these cases, elastic compression is the only alternative.
Acknowledgements
This study received no financial support.
KEY MESSAGES
- Four-layer compression therapy is the gold standard for treating venous ulcers.
- This study investigates whether deep venous in sufficiency worsens the results of compression therapy for the treatment of venous ulcers.
- We found that outcomes following the use of four-layer elastic compression bandage were the same in patients with superficial vein insufficiency and in those who had deep vein insufficiency.
Author(s)
Dr Alberto Garavello
Vascular Surgery Specialist, Emergency Department, Center for Therapy of Lower Limbs Ulcers, San Filippo Neri Hospital, Rome, Italy
Dr Pietro Franzvea
General Surgery Specialist, Policlinico Agostino Gemelli Hospital, Rome, Italy
Dr Massimo Tozzi
Researcher in Statistical Sciences, Rome, Italy
Stefania Gilardi, Paola Fiamma
Nurses Wound Care Specialists, Center for Therapy of Lower Limbs Ulcers, San Filippo Neri Hospital, Rome, Italy
Correspondence: garavellalberto@gmail.com
Conflicts of interest: None
References
- Parker CN, Finlayson KJ, Shuter P, Edwards HE. Risk factors for delayed healing in venous leg ulcers: A review of the literature. Int J Clin Pract 2015 Sep; 69(9):967–77.
- Brikesh N. Compression therapy for venous leg ulcers. Indian Dermatol Online J 2014 Jul–Sep; 53: 378–382.
- Mościcka P, Szewczyk MT , Cwajda-Białasik J, Jawień A. The role of compression therapy in the treatment of venous leg ulcers. Adv Clin Exp Med 2019 Jun; 28(6):847–52.
- Brittenden J, Bradbury AW, Allan PL, Prescott RJ, Harper DR, Ruckley CV. Popliteal vein reflux reduces the healing of chronic venous ulcer. Br J Surg 1998 Jan; 85(1):60–2.
- Robertson L, Lee AJ, Gallagher K, Carmichael SJ, Evans CJ, McKinstry BH et al. Risk factors for chronic ulceration in patients with varicose veins: Acase control study. J Vasc Surg 2009 Jun;49(6):1490–8.
- Melikian R, O’Donnell Jr TF, Suarez L , Iafrati MD. Risk factors associated with the venous leg ulcer that fails to heal after 1 year of treatment. J Vasc Surg Venous Lymphat Disord 2019 Jan;7(1):98–105.
- Pannier F, Rabe E. Progression in venous pathology. Phlebology 2015 Mar;30(1 Suppl):95–7.
- Tzaneva S, Heere-Ress E, Kittler H, Böhler K. Surgical treatment of large vascular leg ulcers: A retrospective review evaluating risk factors for healing and recurrence. Dermatol Surg 2014 Nov; 40(11):1240–8.
- Guest M, Smith JJ, Sira MS, Madden P., Greenhalgh RM, Davies AH. Venous ulcer healing by four-layer compression bandaging is not influenced by the pattern of venous incompetence. BrJSurg 1999 Nov;86 (11):1437–40.
- Antignani PL, Benedetti-Valentini F, Aluigi L, Baroncelli TA, Camporese G, Failla G. Diagnosis of vascular disease. Int Angiology 2012; 31(Suppl. 1,5):52–6.
- Moffat C. Four-layer bandaging: From concept to practice. Int J Low Extrem Wounds 2002 Mar; 1(1):13–26.
- O’Meara S, Cullum N, Nelson EA, Dumville JC. Compression for venous leg ulcers. Cochrane Database Syst Rev 2012 Nov 14;11(11): 1-151.
- Mauck KF, Asi N, Elraiyah TA, Undavalli C, Nabhan M, Altayar O, et al. Comparative systematic review and meta-analysis of compression modalities for the promotion of venous ulcer healing and reducing ulcer recurrence. J Vasc Surg 2014 Aug; 60(2 Suppl):71S–90S, e1–2. doi: 10.1016/j.jvs.2014.04.060
- O’Meara S, Tierney J, Cullum N, Bland JM, Franks PJ, Mole T et al. Four layer bandage compared with short stretch bandage for venous leg ulcers: Systematic review and meta-analysis of randomized trials with data from individual patients. BMJ 2009; 338: b1344.
- Asaf M, Salim N, Tuffaha M. Challenging the use of bandage compression as the baseline for evaluating the healing outcomes of venous leg ulcer-related compression therapies in the community and outpatient setting: An integrative review. Dubai Med J 2018; 1:19–25.
- De Carvalho MR, Utzeri Peixoto B, Andrade Silveira I, Baptista de Oliveria BGR. A meta-analysis to compare four-layer to short-stretch compression bandaging for venous leg ulcer healing. Ostomy Wound Manage 2018 May; 64(5):30–7.
- Protz K, Heyer K, Dissemond J, Temme B, Münter KC, Verheyen-Cronau I et al. Compression therapy - current practice of care: Level of knowledge in patients with venous leg ulcers. J DtschDermatolGes 2016 Dec;14(12):1273–82.
- Konschake W, Valesky E, Stege H, Jünger M. Evidence of compression therapy. Hautarzt 2017 Aug; 68(8):625–31.
- Castonguay G. Short-stretch or four layer compression bandages: An overview of the literature. Ostomy Wound Manage 2008 Mar; 54(3):50–5.
- Moffatt C, McCullagh L, O’Connor T , Doherty DC, Hourican C, Stevens J et al. Randomized trial of four layer and two layer bandage systems in the management of chronic venous ulceration. Wound Repair Regen May–Jun 2003; 11(3):166–71.
- Szewczyk MT, Jawien A, Cierzniakowska K. Comparison of the effectiveness of compression stockings and layer compression systems in venous ulceration treatment. Arch Med Sci 2010 Oct; 6(5):793–9.
- Nelson EA , Iglesias CP, Cullum N, Torgerson DJ, VenUS I collaborators. Randomized clinical trial of four-layer and short-stretch compression bandages for venous leg ulcers (VenUS I). BrJSurg 2004 Oct; 91(10):1292–9.
- Stücker M, Link K, Reich-Schupke S, Altmeyer P, Doerler M. Compression and venous ulcers.Phlebology 2013 Mar; 28 Suppl 1:68–72. doi: 10.1177/0268355512475120
- Ashby RL, Gabe R, Ali S, Saramago P, Chuang KH, Adderley U et al. VenUS IV (Venous leg Ulcer Study IV) - compression hosiery compared with compression bandaging in the treatment of venous leg ulcers: A randomised controlled trial, mixed-treatment comparison and decision-analytic model. Health Technol Assess 2014 Sep;18(57):1–293, v–vi. doi: 10.3310/hta18570
- Finlayson K, Edwards H, Courtney M. Relationships between preventive activities, psychosocial factors and recurrence of venous leg ulcers: A prospective study. J Adv Nurs 2011 Oct; 67(10):2180–90.
- Karen F, Mauck KF. Comparative systematic review and meta-analysis of compression modalities for the promotion of venous ulcer healing and reducing ulcer recurrence. J Vasc Surg 2014 Aug; 60(2 Suppl):71S–90S,e1–2.
