Volume 23 Number 2
Using the Iowa Model of Evidence-Based Practice to guide development of a skin tear management protocol
Christine AF Bell
Keywords skin tears, evidence-based practice, clinical practice, Iowa model, International Skin Tear Advisory Panel, standardisation
DOI 10.35279/jowm2022.23.02.06
Abstract
This paper describes the process a wound care team used to develop a protocol to standardise the care of skin tears in an orthopaedic specialty hospital.
The aims of the project were to: 1) find a classification tool to implement standardisation and 2) develop and implement a treatment algorithm and guidelines according to current evidence.
A protocol and algorithm were developed to deal with skin tears in a standardised format. Knowledge increased 36% after an educational intervention targeting skin tear aetiology and implementation of the newly developed protocol.
INTRODUCTION
Orthopaedic patients undergoing elective surgeries are at high risk for skin tears (ST) due to risk factors such as immobility, surgical positioning, length of surgery, medical device use and anticoagulation agents that often affect the skin.1,2 Total joint arthroplasty (TJA) and many spinal surgeries are considered to be an elective orthopaedic surgery. Trends for TJA surgery are projected to continue to rise as the population ages and the desire for continued mobility pushes demand.3–8 More than 1 million TJA surgeries are performed annually in the United States (U.S.), with projected increases of up to 4 million annually by 2030. Within the U.S., there is a projection of 11 million citizens who will be living with a hip or knee arthroplasty by 2030.6 Total shoulder arthroplasty (TSA) surgery continues to increase, with more than 800,000 patients currently living in the U.S.9 Spine surgery statistics are difficult to assess, due to the number of differing surgical interventions, but by all projections will continue to increase.10,11 Common risk factors for elective orthopaedic surgeries include: advanced age, degenerative disease, limited function and female sex.1–3,10
The literature has reported ST prevalence rates equal to or greater than pressure injuries, yet standardisations of assessment, treatment and documentation are often lacking.1 STs have been found on patients of all medical specialties and ages, but the population aged 60 years and above presented with more than those under 60 years of age.1,12–14 Skin tears can become chronic issues causing debilitation, pain and decreased quality of life.1,13–18
Background
Skin tears are common and occur at least as often as pressure injuries but are not treated with the same attention.18 An international study exploring current practices in the assessment, prevention and treatment of STs resulted in new knowledge regarding nurses’ perceptions of their challenges in caring for patients experiencing STs. Sixteen countries and 1127 health care providers (HCP) responded. Registered nurses made up 77.4% of the respondents, and advance practice nurses an additional 9.7%. Seventy percent of the respondents (69.6%, n =695) reported problems with the current methods for the assessment and documentation. Ninety percent supported developing a simplified tool for assessment.19
A systematic review of STs by Strazzieri-Pulido et al. (2015)13 found an estimated global prevalence between 3.3% and 22% in acute care settings and 5.5% and 19.5% in home care settings.2,13 Studies out of Brazil found a 12.2% ST prevalence,2 with a range of 3.3–22% in hospitalised adults.2,13 Australian prevalence studies of hospitalised patients ranged from 8.1%–8.9%.15,16 The 10-year analysis of ST prevalence by Miles et al. (2021)16 found 60.7% of reported STs were hospital-acquired, 38.7% of patients had multiple STs and 84.8% of patients with STs were 70 years of age or older.16
The development of a ST definition by the International Skin Tear Advisory Panel (ISTAP) has been instrumental in establishing a consensus of what actually constitutes an ST. An updated definition of STs has been defined as ‘traumatic wounds caused by mechanical forces, including [the] removal of adhesives. Severity may vary by depth (not extending through the subcutaneous layer).20,21 This was expanded from an earlier definition of STs which read ‘…a wound caused by sheer, friction and/or blunt force trauma resulting in the separation of skin layers. A[n] ST can be partial thickness (separation of the epidermis from the dermis) or full thickness (separation of both the epidermis and the dermis from the underlying structures)’.22
In October 2018, wound committee members (Table 1.) of an orthopaedic specialty, Magnet-designated hospital in Boston, Massachusetts discussed the issue of STs in their surgical orthopaedic population and the lack of standardisation in their assessment, documentation and treatment among nurses and medical staff. STs occurring on patients that were both present on admission or sustained during the hospital stay were being assessed, documented and treated in a non-standardised fashion by nursing and medical staff. There was no consistency or common language used in classifying or documenting STs. Treatments used were not evidence-based, and STs were not being routinely identified or documented. Treatment was left up to the individual nurse or licensed independent practitioner (LIP) as to what products to use and how to manage skin repair. To establish standardisation of the above-stated issues, it was decided to create an evidence-based practice protocol. The nursing research committee had previously adopted The Iowa Model Revised (see Figure 1.) as the guiding framework for projects; therefore, the wound care team chose to use this as their guiding model as well.
Table 1: Wound Care Team
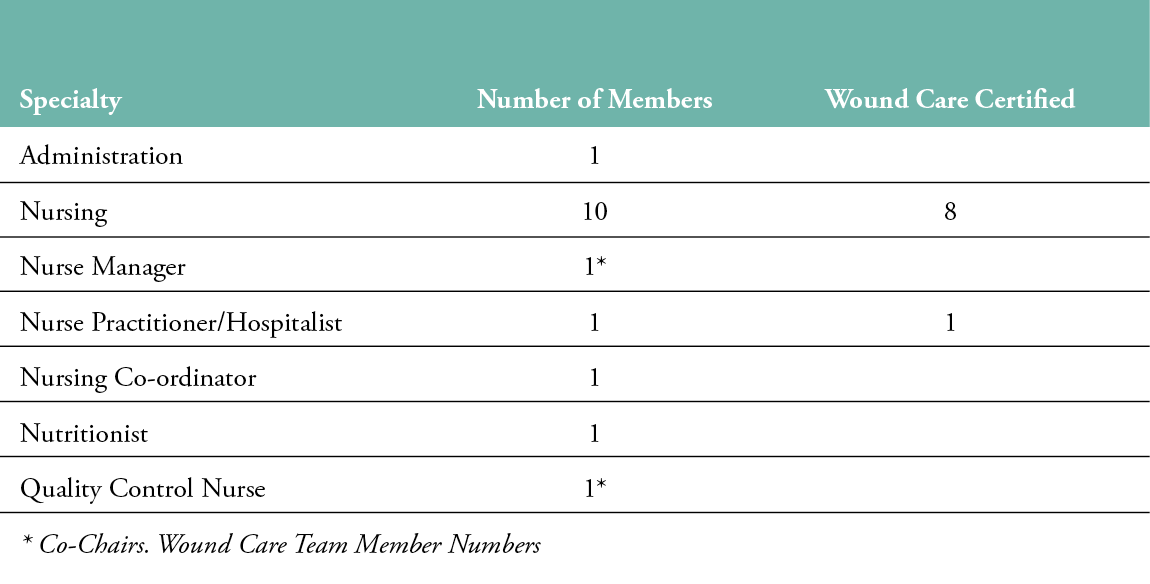
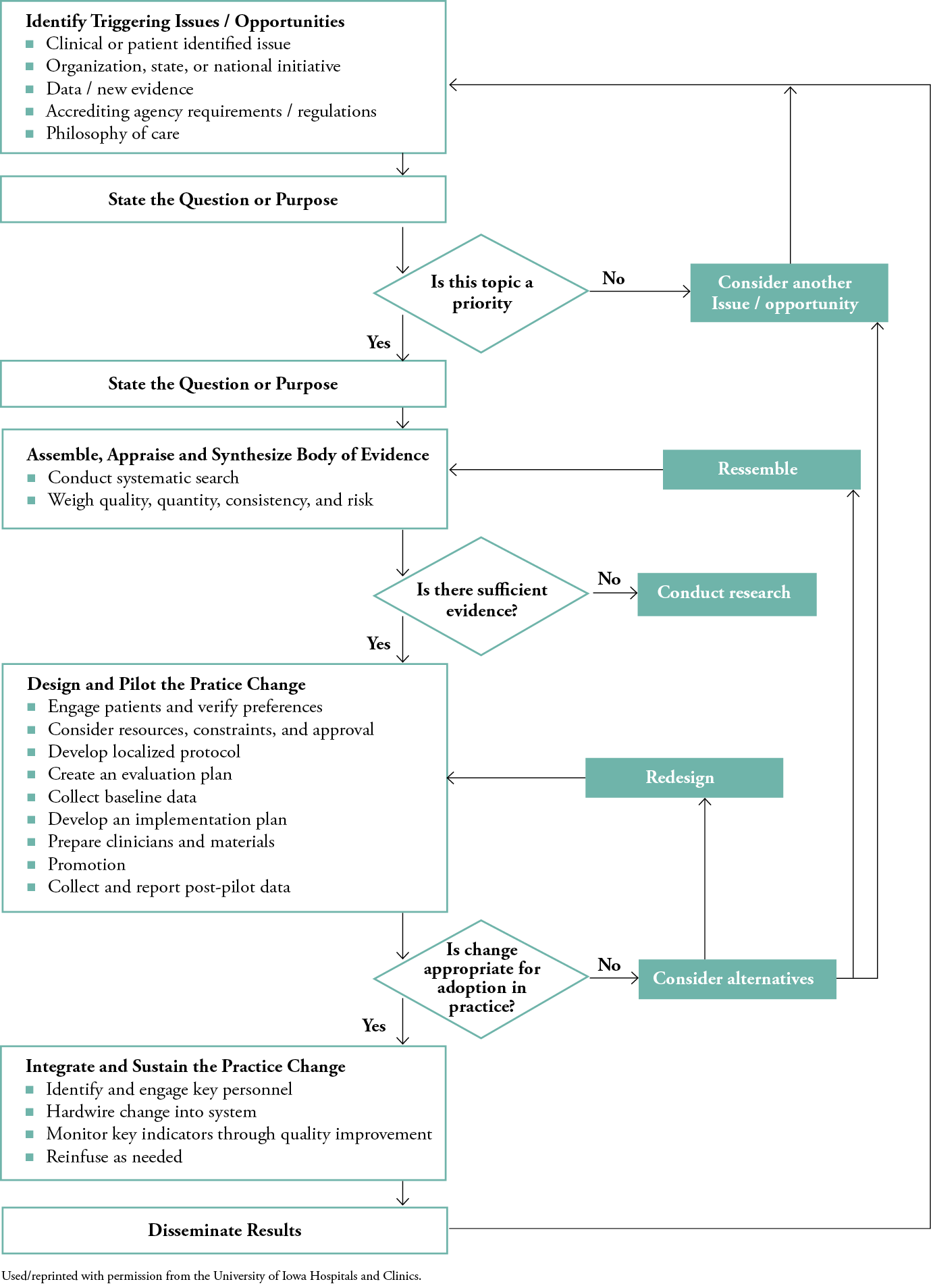
Figure 1: The Iowa Model Revised: Evidence-Based Pratice to Promote Excellence in Health Care
Purpose/Process
The purposes of this evidence-based practice (EBP) project were: 1) to find a classification tool to implement standardised assessment and documentation of STs, both present on admission and those that develop during hospitalisation; 2) to review the literature to find the best practices for treatment protocols; and 3) to develop and implement a treatment algorithm and guidelines according to current evidence that clinical practice nurses could use independently.
METHODS
Study population
A convenience sample of the nursing and hospitalist staff at one institution was used to measure knowledge of STs and institute a new skin tear management set of guidelines.
Practice setting
New England Baptist Hospital (NEBH) is a 118-bed orthopaedic specialty teaching hospital located in the heart of Boston, Massachusetts. More than 10,000 orthopaedic procedures, including 6,000 primary total hip and knee arthroplasties, are performed annually. This institution performs the second-highest number of joint arthroplasty procedures in the U.S. each year. Ninety percent of patients are over 68 years of age and have associated co-morbidities. Approximately 350 clinical and advance practice nurses/LIPs were employed at NEBH at the time of this project.
Study design
Participants for the educational intervention piece of this project consisted of clinical practice nurses, advance practice nurses and hospitalists who were employed full-time, part-time and casually. Hospitalists in this institution are defined as dedicated in-patient physicians who work exclusively in a hospital setting, as opposed to private practice, and assume the medial care of the in-patient population. All participants had access to HealthStream, the electronic education platform used by the institution to disseminate required education units.
An educational intervention was developed to introduce all end users to the new standard of care. Based on a review of current evidence, a PowerPoint slide presentation highlighting the aetiology, assessment and management of STs and the new algorithm was developed by the wound care team. A pre-/post-test of ten questions was also developed by the wound care team, focusing on risk factors, assessment, classification, treatment and documentation of STs. The pre-test was intended to measure baseline knowledge, and the post-test aimed to measure knowledge after viewing the educational intervention specific to the institution’s new algorithm and guidelines. The pre-/post-test was the same test given before and after the PowerPoint presentation. This PowerPoint and accompanying pre-/post-tests were reviewed by theeducational department for content and deliver-ability.
The Iowa Model Revised: Evidence-Based Practice to promote excellence in health care
The new algorithm and guidelines were developed by the wound care team using The Iowa Model Revised framework to guide this practice change.
The Iowa Model is a framework to guide clinicians in evaluating and connecting research findings into patient care.23 This work was initially based on social scientist E.H. Rogers’ theory of Diffusion of Innovations.24 The most recent model was revised and validated by the Iowa Model Collaborative in 2015.25 Reported benefits of the model are that it is easy to follow, straightforward and assists with the implementation of practice changes. The model emphasises change based on current evidence and support from the entire healthcare system at the hospital and organisational levels. If the project/opportunity topic is not a priority to the organisation, it goes no further. Specific steps along the framework include: 1) identifying a triggering issue or opportunity; 2) stating the purpose, assuring organisational support by identifying this as a priority topic; 3) forming a team, conducting an in-depth literature review to acquire current existing evidence; 4) designing and implementing a pilot for the practice change by engaging staff and paying attention to preferences, resources, constraints and approval; 5) developing a protocol and plan, collecting data and evaluating processes; 6) assessing if the practice change is appropriate and ready for implementation; 7) hardwiring the change into the current system, monitoring key indicators; and finally, 8) disseminating results25 (Figure 1).
Using the model
The Iowa Model for Evidence-Based Practice (EBP) was used as the framework for this project. The following is the template created by the wound care team members (Figure 2.).
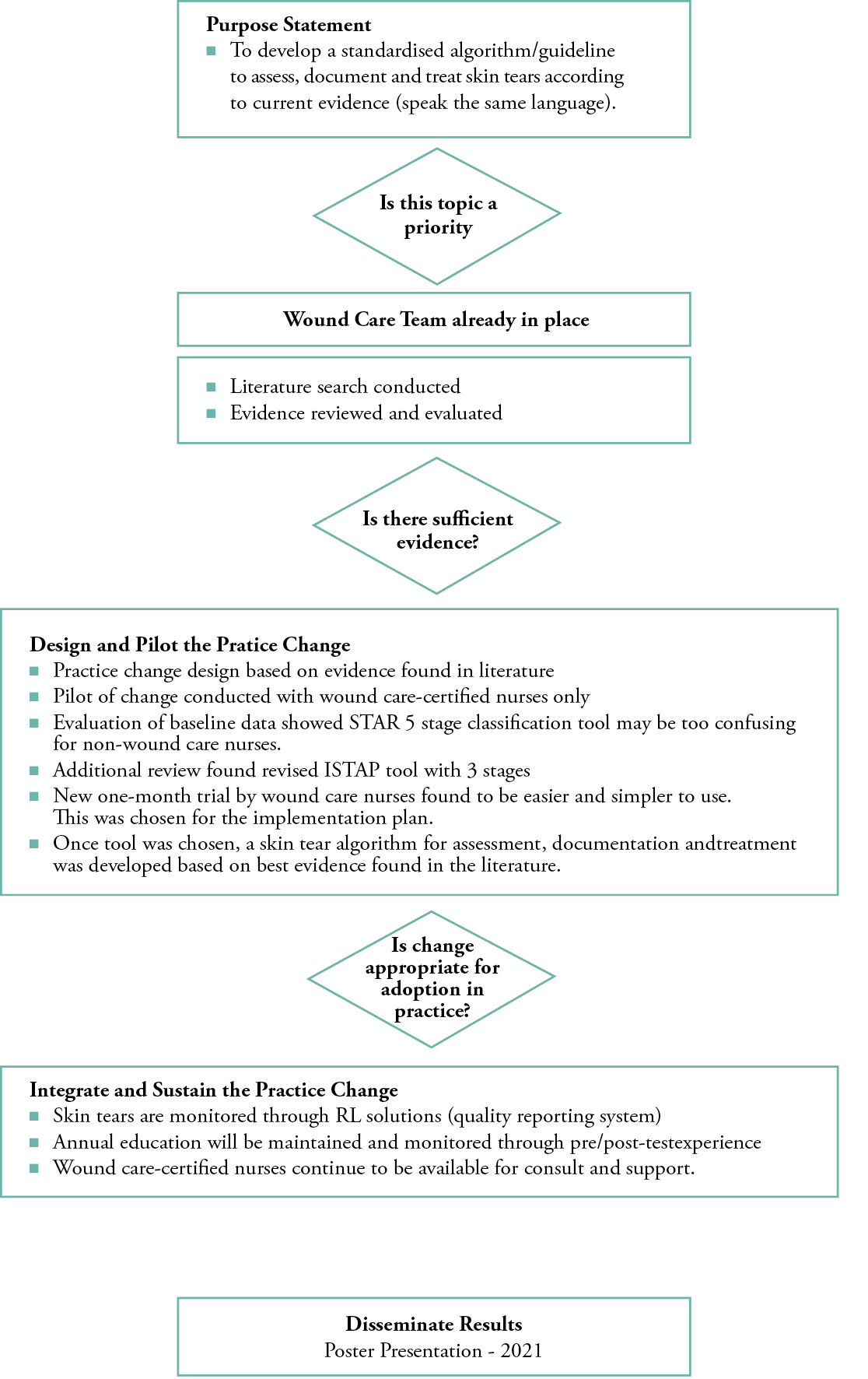
Figure 2: Proposed Practice Change Using Iowa Model Revised
Identify triggering issues: Clinical/patient issue – skin tears are not assessed, documented or treated in a standardised or evidence-based fashion.
Purpose statement: To develop a standardised algorithm/guideline to assess, document and treat STs according to current evidence in this institution (speak the same language and increase consistency of care).
Is this topic a priority: Yes – nursing admini- stration support was strong and demonstrated by providing additional paid time for wound care team members to conduct this project.
Form a team: A wound care team was already in place with active team members. This topic of concern was brought to them at a committee meeting for discussion and the brainstorming of ideas. This team consisted of clinical, critical care and perioperative nurses, several of whom were wound care certified (WCC); a quality improvement nurse; an advance practice nurse practitioner; a nutritionist; a nursing supervisor and a clinical nurse manager (Table 1).
Assemble, appraise and synthesise body of evidence: The literature was searched using the CINAHL and MEDLINE electronic databases for articles. Search terms included ‘skin tears’, ‘orthopedic surgery and skin tears’, ‘surgery’, ‘prevalence’, ‘acute’, ‘inpatient’, ‘hospitalized’, ‘post-operative’, ‘total joint replacement’, ‘arthroplasty’ and ‘spine’. Articles ten years old and newer were accepted into the search. No articles specific to total joint replacement, arthroscopy, spine or elective surgery were found. Peer-reviewed manuscripts from the International Skin Tear Advisory Panel were the most common and up-to-date results returned.
This research confirmed the knowledge gap in the assessment, treatment and management of STs in the specialty of elective orthopaedic surgery.
Is there sufficient evidence: Yes.
Design and pilot the practice change: Based on evidence from the literature and national consensus, a protocol algorithm for assessment and treatment (dressings) was developed. A treatment order set dependent on classification type and wound periphery) was developed and uploaded to the electronic medical record (EMR) system by the information technology (IT) department.
The STAR classification tool26 (5 stages) was discussed and briefly, informally trialed by the WCC nurses, who found it confusing, due to its multiple labels. With one of the goals being ease of use for clinical practice nurses, an additional review was conducted and the revised ISTAP (3 type) classification tool was chosen.12 This classification tool was then trialed for one month by the same WCC nurses and found to be more succinct and easier to use. The pilot consisted of the WCC nurses being the primary clinical personnel to address any ST issues that arose during the month of June 2019. Six skin tears were documented and assessed by WCC nurses, one on the clinical unit and five in the post anaesthesia care unit. The six episodes of care were tracked on a grid sheet in a booklet kept in each patient unit. WCC nurses recorded the skin type, dressing used, time spent on consult, algorithm ease of use (1=easy; 5=difficult), if there would have been a difference in the process before the project began and any questions/concerns. The algorithm and ISTAP instrument were found to be acceptable for practice change.
Integrate and sustain the practice change: Education was then developed for the entire clinical nursing, advance practice nursing and hospitalist staff. Knowledge was measured using pre- and post-tests that accompanied an educational intervention. The educational intervention was in the form of a PowerPoint developed by the wound care team based on current evidence and knowledge. ST incidents were monitored through the RLSolutions system, an electronic event-reporting system used by NEBH, and discussed at the monthly wound care meetings. Discussion is ongoing regarding when to re-educate and assess this practice change. Certified wound care nurses remain available for support and consultation.
Dissemination: In 2022, this project was presented by wound care team members in a virtual poster format at the National Association of Orthopaedic Nurses conference.
RESULTS
Instrument choice
After four weeks of trialling by WCC nurses of the institution, the ISTAP Skin Tear Classification Tool was chosen for use by clinicians to identify, classify and document STs and their types. The ISTAP Skin Tear Classification System (Figure 3) is a part of the Skin Tear Tool Kit developed in 2013 by the International Skin Tear Advisory Panel and based on extensive literature reviews, input from international healthcare professionals (HCP) and experts’ opinions.12,17 Results from the validation study conducted by LeBlanc et al. (2013)12 indicated a high level of agreement and substantial interrater reliability for the expert panel, and moderate interrater reliability for licensed nurses. Diagnostic reliability was found to be high when 1601 participants from 44 countries were asked to classify skin types using photos of different skin tears.17

Figure 3: The International Skin Tear Advisory Panel’s (ISTAP )classification system
The Skin Tear Decision Algorithm (STDA) was designed by ISTAP members to assist HCPs in assessing, classifying and treating STs. This decision algorithm includes treatment and classifications of skin tear types and is intended to be the link between the assessment and treatment of STs, specifically product selection (Figure 4.).18
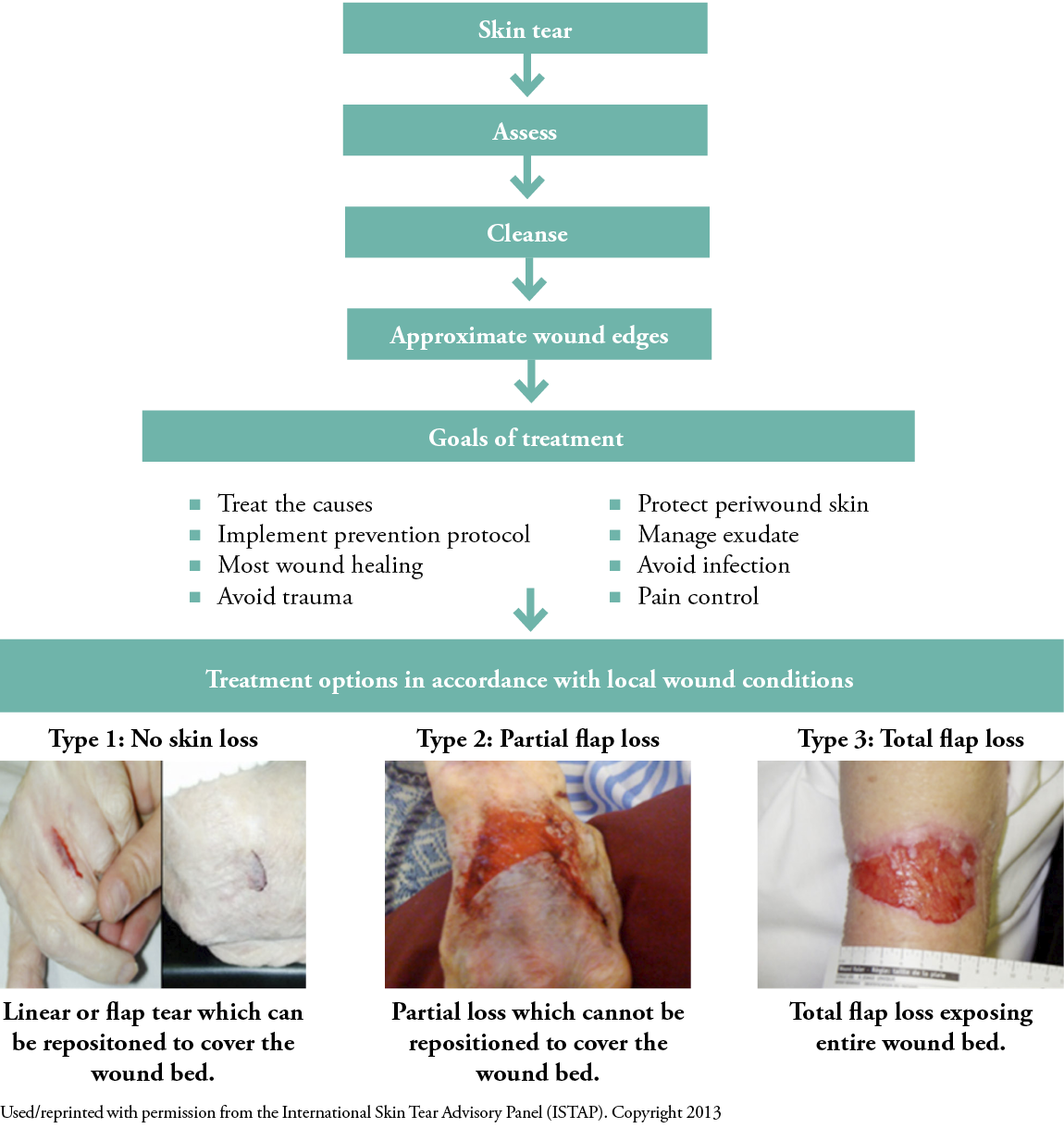
Figure 4: Skin Tear Decision Algorithm (STDA)
Algorithm development
A Skin Tear Management (STM) algorithm that incorporated parts of the STDA was developed by wound care members using the ISTAP classification tool and dressing guidelines found in The Art of the Dressing Selection: A Consensus Statement on Skin Tears and Best Practice.18 Best practice recommendations for a systematic approach to treatment and dressing selection was the foremost goal when building this algorithm. The algorithm included identification of the ST category, guidelines for treatment and dressing choice. Once this algorithm was reviewed by the nursing and medical staff, it was processed through the professional practice council that reviews all new protocols and guidelines before they become the standard of care (Figure 5.).
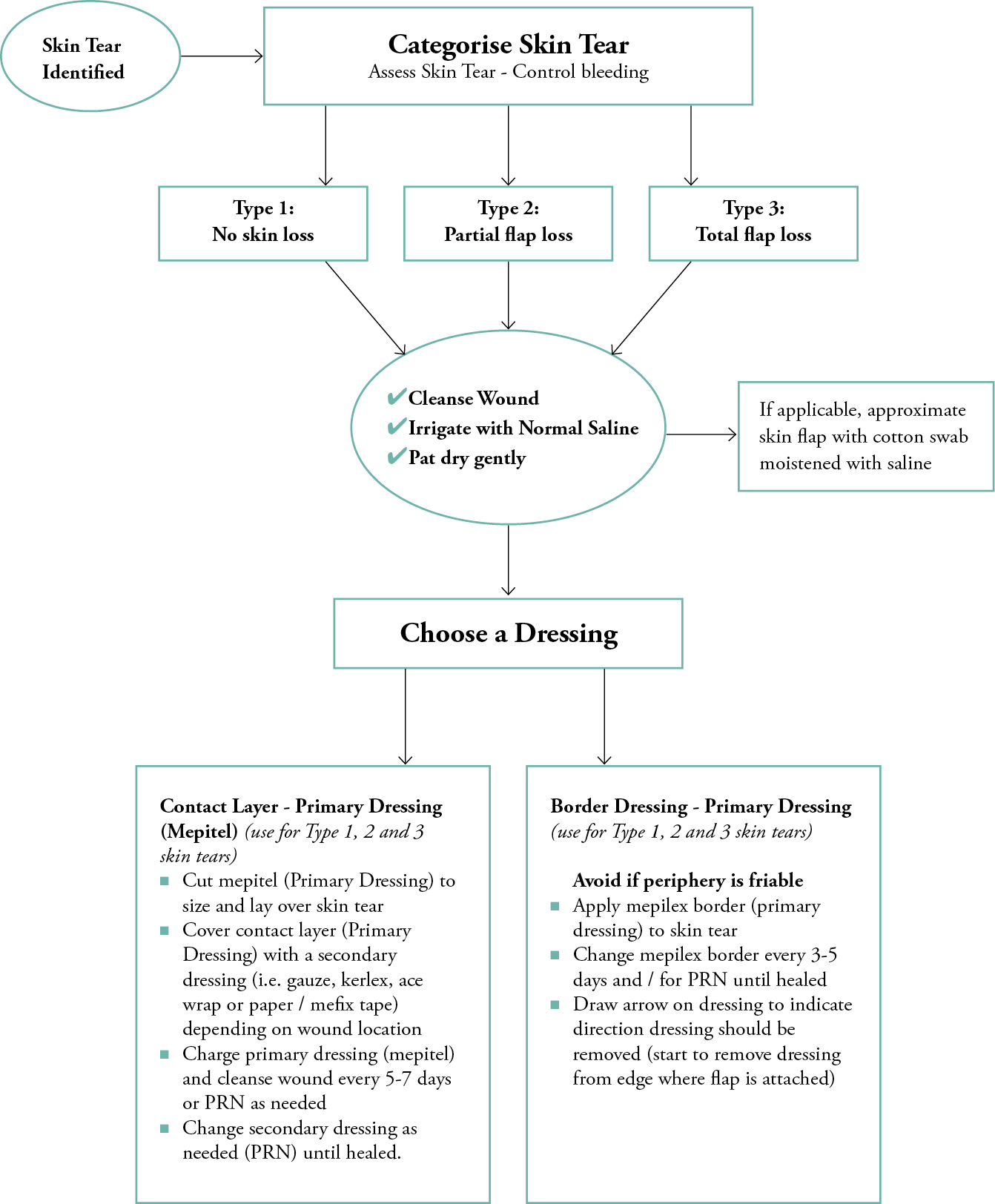
Figure 5: Skin Tear Management Algorithm developed for New England Baptist Hospital, 2019 New England Baptist Hospital Skin Tear Management Algorithm (STM)
After review by all necessary departments, the STM algorithm was built into the EMR system by the IT department. The algorithm consisted of a bundle of orders accessed under ‘Skin Tear Management’ in the EMR order section. When this order set was chosen, the practitioner is able to order treatment and dressing selection for an ST.
Documentation and order set
Documentation followed the ISTAP classification of Type 1–3.12,18 A new category, ‘skin tear’, was added to the wound chapter in the institution’s EMR with a drop-down option to choose: Type 1 (no flap loss), Type 2 (partial flap loss) or Type 3 (full flap loss). Additional documentation consisted of anatomical location and duration of ST, partial or full thickness tear, measurements of the ST, wound bed and periphery description, type and amount of exudate, degree of flap necrosis, signs of infection, associated pain and type of dressing applied. A clinical note was added in the notes section of the nursing assessment, and a copy was sent to the wound care team for review and data collection.
The order set available for the wound management algorithm was entitled ‘Skin Tear Management’ (STM) and placed under the common order choices of the EMR. Checking the STM box created a drop-down menu of the order set. The steps, which follow the STM Algorithm (Figure 5.), were listed 1–6, so they could be kept together in the current nursing order screen once added. The orders come as a set and cannot be separated. The steps are as follows: 1) implement a nurse-driven protocol for STM; 2) assess ST and classify (control bleeding); 3) cleanse wound; 4) approximate skin flap; 5) choose dressing, initial and date; 6) do not use the following dressings: tegaderm transparent adhesive film, hydro fibres, sutures, staples or steri-strips. Clinical staff were educated on how to choose a dressing. Choices were condensed to a border adhesive silicone foam dressing, if peripheral skin was appropriate, or a non-adherent, two-sided, silicone contact layer. A non-adhesive anchoring of the contact layer was part of the order, if peripheral skin was deemed to be fragile and at risk of additional STs, or if further injury was thought possible. Instructions on marking the dressing with a directional arrow for future removal was also part of the educational intervention.
Educational intervention and practice change
Once the instrument of assessment and treatment was decided upon and the documentation process embedded into the EMR, education of the clinical staff was implemented. The educational intervention consisted of a PowerPoint presentation (described earlier) for all licensed clinical staff members. This group consisted of clinical practice nurses, advance practice nurses and hospitalists. The goals of this intervention were to: 1) measure knowledge after an educational intervention and 2) introduce the new practice change to the clinical staff, including the STM algorithm developed by team. This assisted with the goal of standardising the assessment, treatments being ordered and documentation.
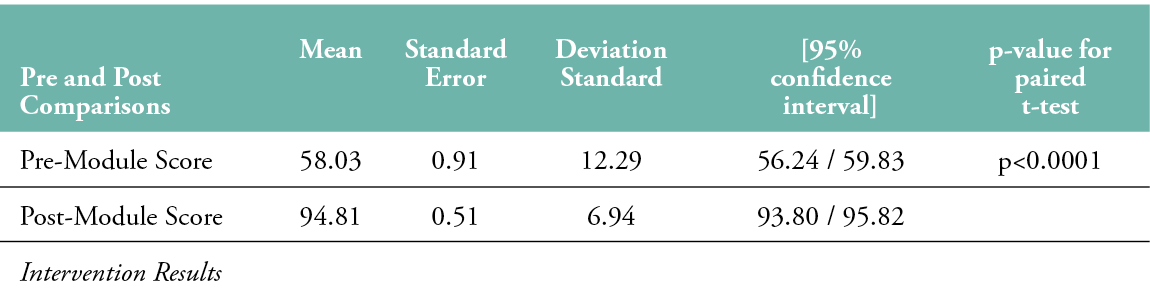
The educational unit was viewed by a total of 340 clinical staff members (n=340). Completed pre- and post-tests were submitted by 183 clinical staff members (n=183), resulting in a 55% completion rate. Statistical analysis was performed using STATA.15 Pre- and post-test scores were compared using a paired t-test analysis. Results revealed a statistically significant increase in post-educational intervention knowledge p<0.0001 (Table 2).
Table 2: Educational Intervention Results
The wound management order set is now incorporated as standard practice, and clinicians follow the algorithm to assess, order treatment and document STs that are noted on admission or developed during the hospital stay.
DISCUSSION
After searching the literature for evidence to assist in managing the orthopaedic/spine population at our institution and finding no specific studies that focus on this population, a knowledge gap was identified. Several peer-reviewed, current articles from the ISTAP were found and provided considerable assistance in the development of this project. The majority of articles found were either mixed acute care patients (hospital and home or rehabilitation) or focused on home care/rehab patients. No articles focusing on surgical patients, particularly elective surgical patients, were found.
Using the Iowa Model Revised gave a framework to structure this project and keep it on track. The process and new developments were shared at the monthly wound care meetings, and new goals were established based on where we were in the framework.
This EBP project was determined to have high priority by administration and wound care members. STs are now being assessed, treated and documented in a more standardised process. The STM algorithm and standing order set have become tools the staff use consistently. Evidence-supported treatment choices were narrowed down to two products and no longer include tegaderm films, steri-strips or hydro fibres. The diverse membership of the wound care team (see Table 1.) ensured the availability of knowledgeable clinical staff members at every level of patient contact. This promoted role support and guidance for the staff when the implementation of the order set and algorithm occurred. Patient satisfaction was not specifically measured, but patients have been included in the treatment process and patient education has been made a priority. The WCC nurses still comment on the decrease in calls to assess STs since the STM algorithm was added in monthly meetings.
Patient safety is a primary concern, whether it is focused on managing current STs or preventing them from occurring during the surgical process and recovery. STs are continuing to be tracked by the wound care team and the quality department, with the largest number of incidences occurring in the operating room. This tracking has led to much discussion regarding the identification of risk, prediction of potential skin tear issues and ways to mitigate STs during surgery. There is ongoing progress towards identifying ST risk factors, especially in those patients with high BMIs and/or co-morbidities. By having a standard process, STs are being managed using the most current evidence with the goal of proper healing, less pain and no infections.
CONCLUSION
There has been no literature highlighting STs in the elective orthopaedic surgical population. This population is at high risk due to age, mobility issues, mechanical and assistive devices, surgery and pharmacological interventions. Standardising the assessment, treatment options and documentation of STs has assisted all clinicians in managing STs more consistently, increasing patient safety and comfort. Consults with the WCC nurses for basic ST management have, anecdotally, decreased as clinical practice nurses and hospitalists have become more familiar and confident in requesting the STM order set be instituted and the algorithm followed. Focused work is ongoing to refine risk factors in the operating rooms. Future work should include the positioning of at-risk patients and enhanced identification of patients at high risk on admission. Future work is also being discussed related to assessing how well clinical practice nurses are using this algorithm. Informally, there has been strong positive feedback as to the process being defined and standardised.
IMPLICATIONS FOR CLINICAL PRACTICE
- Surgical orthopaedic patients are under-investigated as a high-risk population for skin tears.
- Standardising assessment, treatment and documentation can increase compliance with best practices by clinical nurses and LIPs.
- Patient safety and satisfaction will be increased by using evidence-based protocols and standardising care.
Future research
- The tracking of STs occurring during surgical procedures is needed.
- Measuring nurses’ perceptions of their competence and confidence is necessary for assessing ongoing role support needs.
Acknowledgements
Authored on behalf of the wound care team of New England Baptist Hospital. Members at time of project: Sandra Anderson BSN, Marjorie Bennet MSN, WCC, Susan DeBerardinis BSN, WCC, Ann Ell, BSN, WCC, Megan Gilmore BSN, WCC, Mary Beth Hamilton* MSN, Melanie Hughes BSN, WCC, Sharon Higgins MSN, NP, WCC, Tricia Ides DNP, Lauren Koloski* MSN, Laura Morgan MSN,WCC, Patricia Peters BSN, Elizabeth Weisberger BSN, WCC, Maureen White BSN, WCC *co-chairs
Author(s)
Christine AF Bell, PhD, Rn, New England Baptist Hospital, Boston, Massachusetts
Authored on behalf of the Wound Care team of New England Baptist Hospital
Correspondence: cabell@nebh.org
Conflict of interest: None
References
- LeBlanc K, Baranoski S, Skin Tear Consensus Panel Members. Skin tears: state of the science: consensus statements for the prevention, prediction, assessment, and treatment of skin tears. Adv Skin Wound Care 2011; 24(9 Suppl):2-15. doi:10.1097/01.ASW.0000405316.99011.95
- Souza LM, Teixeira GS. Silva DM, Ruiz LS, Coppola IS, Meirelles LCS. Prevalence of skin tears in hospitalized adults and older adults. Rev Esc Enferm USP 2021; 55:e03683. doi:10.1590/S1980-220X2019025103683
- American Academy of Orthopaedic Surgeons. Projected volume of primary and revision total joint replacement in the U. S. 2030–2060. [Presskit]; 2018. Available at: https://aaos-annualmeeting-presskit.org/2018/research-news/sloan_trj].
- Etkin CD, Springer BD. The American Joint Replacement Registry-the first 5 years. Arthroplast Today 2017; 3(2):67-9. doi:10.1016/j.artd.2017.02.002
- Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007; 89(4):780-5. doi:10.2106/JBJS.F.00222
- Kremers HM, Larson DR, Crowson CS, Kremers, WK, Washington RE, Steiner CA, et al. Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg Am 2015; 97(17):1386-97. doi:10.2106/JBJS.N.01141
- Williams SN, Wolford ML, Bercovitz A. Hospitalization for total knee replacement among inpatients aged 45 and over: United States, 2000–2010. NCHS Data Brief 2015; 201:1-8.https://www.cdc.gov/nchs/data/databriefs/db210.pdf
- Wolford ML, Palso K, Bercovitz A. Hospitalization for total hip replacement among inpatients aged 45 and over: United States, 2000–2010. NCHS Data Brief 2015; 186:1-8. https://pubmed.ncbi.nlm.nih.gov/25714040
- Farley KX, Wilson JM, Kumar A, Gottschalk MB, Daly C, Sanchez-Sotelo J, et al. Prevalence of shoulder arthroplasty in the United States and the increasing burden of revision shoulder arthroplasty. JB JS Open Access 2021; 6(3):e20.00156. doi:10.2106/JBJS.OA.20.00156
- Kobayashi K, Ando K, Nishida Y, Ishiguro N, Imagama S. Epidemiological trends in spine surgery over 10 years in a multicenter database. Eur Spine J 2018; 27(8):1698-703. doi:10.1007/s00586-018-5513-4
- Grotle M, Småstuen MC, Fjeld O, Grovle L, Helgeland J, Stroheim K, et al. Lumbar spine surgery across 15 years: Trends, complications and reoperations in a longitudinal observational study from Norway. BMJ Open 2019; 9(8):e028743. doi:10.1136/bmjopen-2018-028743
- LeBlanc K, Baranoski S, Christensen D, Langemo D, Gammon MA, Edwards K. et al. International Skin Tear Advisory Panel: A tool kit to aid in the prevention, assessment, and treatment of skin tears using a Simplified Classification System ©. Adv Skin Wound Care. 2013; 26(10):459-78. doi:10.1097/01.ASW.0000434056.04071.68
- Strazzieri-Pulido KC, Teixeira GS, Silva DM, Ruiz LS, Coppola IS, Meirelles LCS. Skin tear prevalence and associated factors: A systematic review. Revista da Escola de Enfermagem da U S P 2015; 49(4):674-80. doi:10.1590/S0080-623420150000400019
- Strazzieri-Pulido KC, Peres GR, Campanili TC, de Gouveia Santos VL. Incidence of skin tears and risk factors: A systematic literature review. J Wound Ostomy Continence Nurs 2017; 44(1):29-33. doi:10.1097/WON.0000000000000288
- Munro EL, Hickling DF, Williams DM, Bell JJ. Malnutrition is independently associated with skin tears in hospital inpatient setting-Findings of a 6-year point prevalence audit. Inter Wound J 2018; 15(4):527-33. doi:10.1111/iwj.12893
- Miles SJ, Fulbrook P, Williams DM. Skin tear prevalence in an Australian acute care hospital: A 10-year analysis. Int Wound J 2021; 1-10. doi:10.1111/iwj.13735
- Van Tiggelen H, LeBlanc K, Campbell K, Woo S, Baranoski S, Chang AM, et al. Standardizing the classification of skin tears: Validity and reliability testing of the International Skin Tear Advisory Panel Classification System in 44 countries. Br J Dermatol 2020; 183(1):146-54. doi:10.1111/bjd.18604
- LeBlanc K, Baranoski S, Christensen D, Langemo D, Edwards K, Holloway S, et al. The art of dressing selection: A consensus statement on skin tears and best practice. Adv Skin Wound Care 2016; 29(1):32-46. doi: 10.1097/01.ASW.0000475308.06130.df. PMID: 26650095.
- LeBlanc K, Baranoski S, Holloway S, Langemo D, Regan M. A descriptive cross-sectional international study to explore current practices in the assessment, prevention and treatment of skin tears. Int Wound J 2014; 11(4):424-30. doi:10.1111/iwj.12203
- Campbell KE, LeBlanc K, Woo K. Best practice recommendations for prevention and management of skin tears in aged skin: An overview. Wound Intern 2018; 9(1):66-77. www.woundsinternational.com/uploads/resources/5cd2a0928a6a935aef5389ce961fce44.pdf
- Campbell KE, Baronoski S, Gloeckner M, Holloway S, Idensohn P, Langemo D, et al. Skin tears: Prediction, prevention, assessment and management. Nurs Prescrib 2018; 16(12): 600-7. doi:10.12968/npre.2018.16.12.600
- LeBlanc D, Baranoski S. Skin tears: Best practices for care and prevention. Nurs 2014 May; 44(5):36-46. doi: 10.1097/01.NURSE.0000445744.86119.58
- Titler MG, Kleiber C, Steelman VJ, Rakel BA, Budreau G, Everett LQ, et al. The Iowa Model of evidence-based practice to promote quality care. Crit Care Nurs Clin North Am 2001; 13(4):497-509.
- LaMorte WW. Diffusion of Innovation Theory. 2019
- https://sphweb.bumc.bu.edu/otlt/mph-modules/sb/behavioralchangetheories/behavioralchangetheories4.html [accessed January 25, 2022]
- Iowa Model Collaborative, Buckwalter KC, Cullen L, Hanrahan K, Kleiber C, McCarthy AM, et al. Iowa model of evidence-based practice: Revisions and validation. Worldviews Evid Based Nurs 2017 Jun; 14(3):175-82. doi: 10.1111/wvn.12223 Erratum in: Worldviews Evid Based Nurs 2017 Oct; 14 (5):425. PMID: 28632931
- Carville K, Lewin G, Newall N, Haslehurst P, Michael R, Santamaria N. STAR: A consensus for skin tear classification. Primary Intention: The Australian Journal of Wound Management 2007; 15(1):18-28.
