Volume 23 Number 2
A cross-sectional study using the skin tear knowledge assessment instrument (OASES) to assess registered nurse’s knowledge about the identification, classification, prevention, assessment, and management of skin tears in a geriatric rehabilitation hospital
Elaine Formosa, Samantha Holloway
Keywords skin tears, knowledge, nurses
DOI 10.35279/jowm2022.23.02.10
Abstract
Skin tears (STs) are acute traumatic wounds caused by friction, shearing and/or blunt force that result in the rupture of skin layers, the dermis and/or epidermis. Among the main causes are wheelchair injuries (mechanical trauma) and transfers, falls and the removal of adhesives. This study aimed to investigate nurses’ current knowledge of the identification, classification, prevention, assessment and management of STs. The intention was to identify knowledge gaps to design an appropriate education programme for improving skills in the assessment, prevention and identification of STs; to increase awareness; and improve and facilitate existing knowledge of STs. The ST knowledge assessment instrument OASES was used, as this is a validated tool. A pilot phase determined whether the language and content of the tool were understood, and to verify the time required to complete the survey. For the main study, a questionnaire was emailed to 139 registered nurses working in a geriatric rehabilitation hospital located in Malta. In all, 101 responses were gathered over a four-week period (73.4% response rate). The overall results indicated knowledge deficits across the identification, prevention, assessment and management domains of STs. Results for domains related to aetiology, classification and observation, and specific patient groups showed a good level of knowledge, but risk assessment, prevention and treatment showed poor knowledge. Immediate recommendations include the adoption of best practice guidelines and protocols to improve nurses’ awareness and knowledge of STs. This will be facilitated by the development of an education programme to address the knowledge gaps identified.
BACKGROUND
Skin tears (STs) are acute traumatic wounds caused by friction, shearing and/or blunt force, resulting in the rupture of skin layers, the dermis and/or epidermis.1 Among the main causes of STs are wheelchair injuries – which are a type of mechanical trauma – transfers, falls and the removal of adhesives.2 Amongst elderly individuals, most STs are noted on their extremities, most commonly on the arms, the dorsal side of the hands and the lower limbs.3 STs cause significant pain and have an effect on people’s quality of life.3 It is essential that, with an ageing population, health professionals ascertain that they are both confident and competent in managing STs,3 as older adults are at a heightened risk of skin frailty due to the aggregated effect of a combination of intrinsic and extrinsic factors.4
According to the International Skin Tear Advisory Panel (ISTAP) classification system, STs can be classified into three types. Type 1 refers to no skin loss; in this type of ST, there is no skin loss, and the linear or flap tear can be repositioned to cover the wound bed. Type 2 refers to partial skin loss; here, there is a partial flap loss that cannot be repositioned to cover the wound. Type 3 refers to total flap loss; in this case, there is a total flap loss that exposes the entire wound bed.1
According to Van Tiggelen et al.,5 STs are often misdiagnosed. These injuries are generally under-recognised and typically tend not to be well reported within clinical practice. To improve healthcare providers’ knowledge and apply best practices,1 early and more accurate identification of STs is encouraged, followed by proper classification and documentation of the wound and its cause. Furthermore, LeBlanc et al.1 suggested that clinical practices implement an evidence-based treatment protocol.
The Payne-Martin ST classification system, published in 1990, was the first to be developed. The system classified STs into three categories and five types. The classification was driven mainly by the morphological characteristics of the epidermal wound.6 Payne and Martin acknowledged some concerns with respect to the definitions included in their original classification system and later updated the definition of STs and other definitions used within the system accordingly.7 Furthermore, in evaluating the quality of their system, they identified three criteria, internal validity, external validity and utility (usefulness), and claimed that, whilst the first two were well demonstrated, they were concerned about the latter.7 According to White,8 one of the reasons why such criteria were not being met was the lack of awareness and use within care facilities, at least in the case of Australia. In an attempt to improve this, an Australian group of authors led by Professor Keryln Carville9 developed the Skin Tear Audit Research (STAR) ST classification system, with the modified Payne and Martin system as a basis.9 A study was conducted to obtain consensus for the use of the STAR tool and to ensure its availability for use in research.9 Limited literature is available, however, on the use of the STAR tool in the field.
With the aim of continuing to improve on the existing system, the newly developed ISTAP ST classification system consists of three types of wounds (also inclusive of photographic aids). In the next phase, ISTAP tested the system’s intra-reliability by requesting the panel members evaluate and group photos of 30 lesions that had been extracted from a validated photograph database.10 The panel was then asked to re-evaluate the same photos two months later, and the results of both tests were compared and analysed. The system’s inter-observer reliability was then tested through the involvement of 327 clinical nurses by requesting the participants classify the same 30 photos. The results from the external participants were then compared to those of the panel members and analysed.10
While there are a number of existing ST classification systems, awareness and use of them is limited.5 This is also the case in Malta, where the use of such tools in the identification, classification, prevention, assessment and management of ST has not been adopted in clinical practice. According to Chang et al.,11 nurses have a tendency to overlook STs as a type of wound until they deteriorate or become problematic to manage.11 One nurse working in a geriatric rehabilitation hospital in Malta observed that a pressure ulcer staging system was often used incorrectly to classify and document STs. This can lead to misdiagnoses, the under-reporting of STs’ incidence, inappropriate management and inconsistencies in ST assessment and documentation.11 The current study sought to address this issue and to identify aspects of the prevention and management of STs that needed further education using the ISTAP ST classification tool to assess the level of knowledge and the possible impact on outcomes for patients at risk of developing an ST.
OBJECTIVES OF THE STUDY
The main aim of the study was to investigate the current level of registered nurses’ knowledge of the identification, classification, prevention, assessment and management of STs. The intention was to identify gaps, so as to design an appropriate education programme to improve nursing staff members’ skills in the assessment, prevention and identification of STs, increase their awareness, improve their knowledge and facilitate the appropriate management of STs.
Ethical approval
Ethical approval was obtained from the Head of Research and Ethics Committee at the hospital prior to the study.
Advice was also sought from the School of Medicine’s Ethics Committee at Cardiff University. The response was that this project did not require ethical approval from the school, however local approval should be sought.
Study design
The study employed a cross-sectional design and survey methodology that entailed the collection of data regarding registered nurses’ existing knowledge of the identification, prevention, assessment and management of STs using the ISTAP ST classification tool. Prior to the study, the registered nurses had no prior knowledge of or experience using any ST classification tool.
Sample size
The sampling frame for the study included all RNs, excluding those nurses who participated in the pilot study (n=139), working in one of the in-patient wards (n=9) of a geriatric rehabilitation hospital in Malta. The outpatient department, practice nurses, nursing officers and deputy nurses were excluded because they have limited contact with patients’ and their wounds, specifically STs.
Data collection tool and procedures
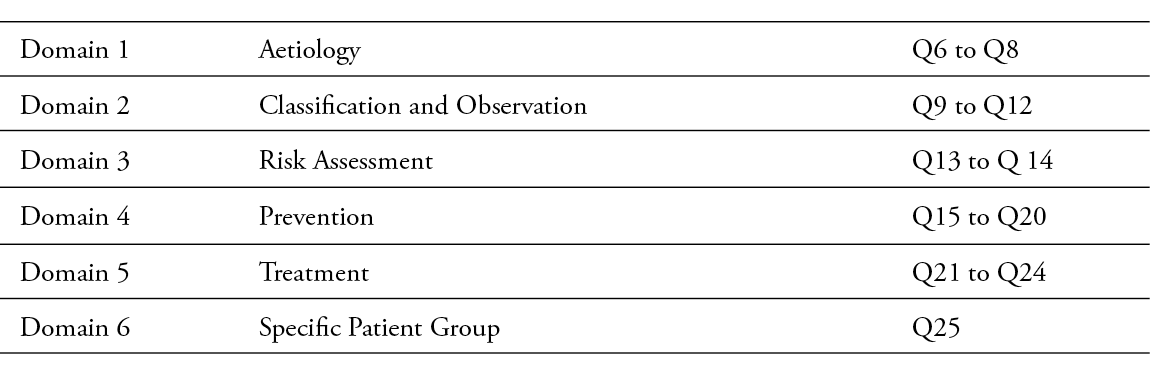
Data were collected using the ST knowledge assessment instrument OASES.12 This instrument contains six domains: aetiology, classification and observation, risk assessment, prevention, treatment and specific patient groups. Permission to use the tool was sought from the original authors prior to commencing the study.
The questionnaire was sent via e-mail to all eligible participants. We included a participant information sheet and a link to access the OASES tool. This ensured that participation was voluntary and that participants gave their consent freely. A reminder was sent once weekly for one month.
The first phase of the study was the pilot of the ST knowledge assessment instrument (OASES), to determine whether the language used, and the content of the tool were understood, and to verify the time required for respondents to complete the survey. The pilot phase took place between May and June 2021. The pilot sample consisted of four nurses chosen randomly from the total eligible population of participants (n=143). They were asked to complete the survey using the OASES tool. This helped determine whether any issues related to the content arose. On the whole, the RNs involved in the pilot study felt that it was very informative and related closely to their area of work. Following the feedback obtained, an additional response option, ‘I don’t know’, was added. This additional response option was also a recommendation made by Van Tiggelen et al.12
Main survey
The main survey ran between June and July 2021. The OASES tool was recreated without any changes using Microsoft Forms and was accessible through a link emailed to participants (n=139). Reminder emails were sent on a weekly basis for the next four weeks. A total of 102 responses were received; however, one respondent had not ticked the consent to participate box, therefore, this response was excluded, leaving 101 participants for inclusion. This gave a 73.4% response rate over the four-week period.
Data analysis
Responses were exported into a Microsoft Excel (Windows XP 2000) spreadsheet, which reduced the risk of errors related to manual data entry. The data were cross-checked by an individual independent of the study.
RESULTS
Response rate and participant characteristics
The survey was sent to 139 RNs who worked in one of the nine in-patient wards. A total of 101 RNs gave consent and participated in the survey, which represents a 73.4% response rate. Table 1 shows the response rate for each of the questions.
Table 1: Response rate per question
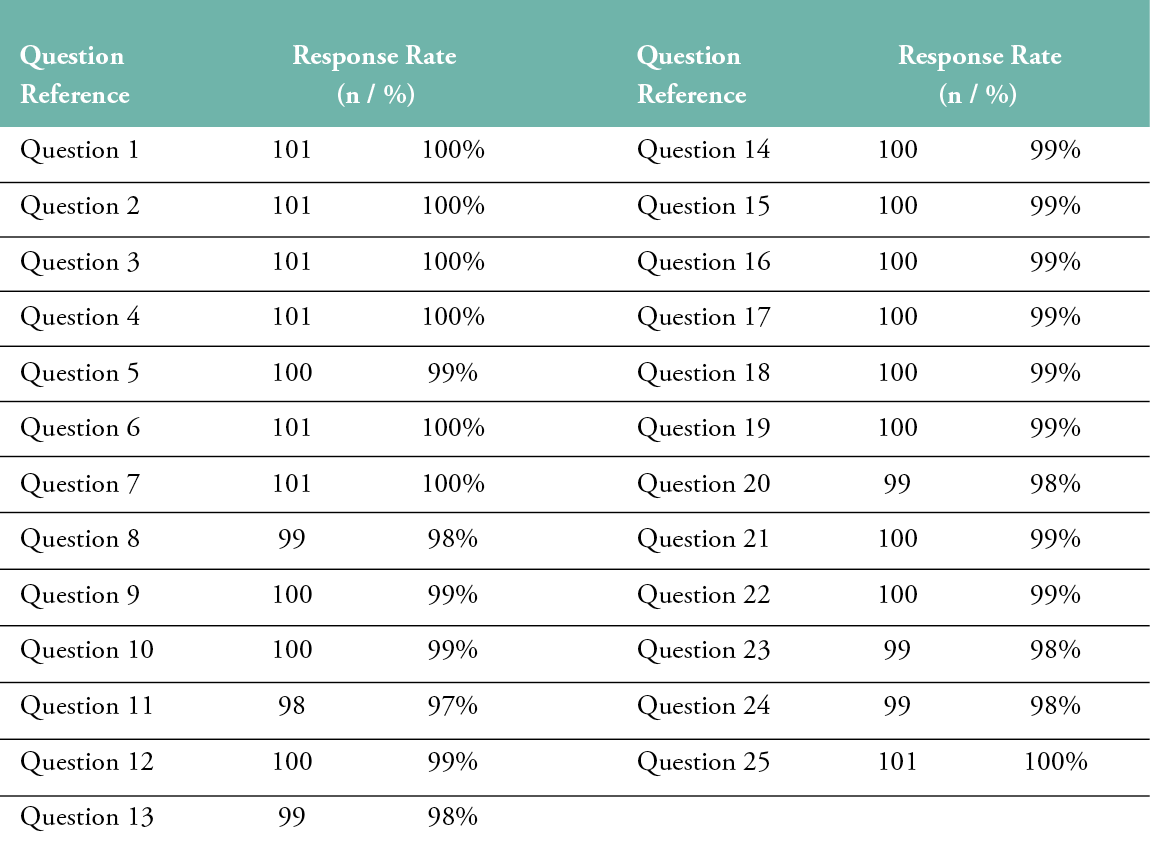
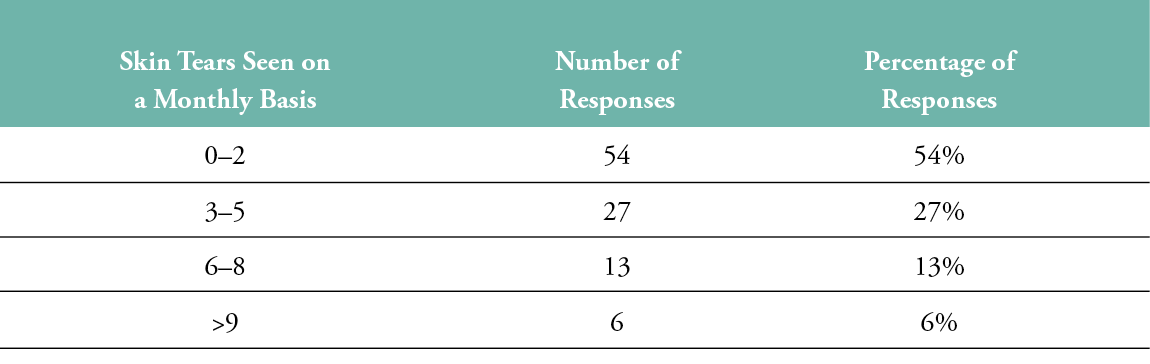
Participants were asked to indicate their educational background (Question 2), with results showing that the majority were at a bachelor’s degree level (44%, n=45), followed by higher school diploma level (30%, n=31) and master’s qualification (25%, n=25) (Figure 1). Participants were also asked how many years of clinical experience they had, with 32% (n=33) having less than 5 years’ experience, 33% (n=34) had 5 to 9 years’ experience and 34% (n=35) had more than 9 years of clinical experience. Finally, participants were asked the frequency of ST instances encountered on a monthly basis (Table 2). A majority of participants encountered none or no more than two ST instances per month.
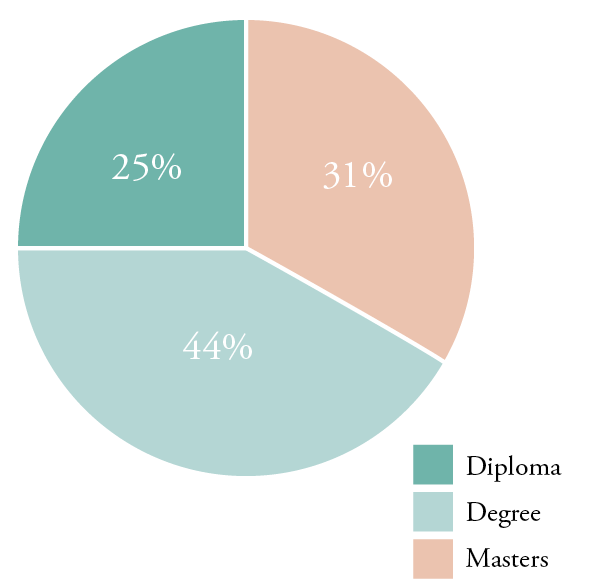
Figure 1: Educational level of participants Q2 - EDUCATION
Table 2: Number of skin tears seen on a monthly basis (self-reported)
OASES domains
The OASES instrument contains six domains: aetiology, classification and observation, risk assessment, prevention, treatment and specific patient groups. Table 3 summarises these. The results are presented according to the domains.
Table 3: Domains of the OASES tool
Aetiology
The aetiology domain includes three questions that focus on the causes of ST. The majority of respondents were able to provide the correct definition of an ST (74%, n=75). When asked about the impact of the ageing process factor with respect to the physiology of the skin, 65% of respondents selected the correct answer, which was the flattening of the dermo-epidermal junction. When asked which factor is associated with dry skin in an elderly population, only 29% of participants replied correctly that these patients experience decreased activity in their sebaceous glands.
Classification and observation
Four questions examined RNs’ knowledge of classification and observation specifically focussing on the identification, classification and documentation of STs. One question required the participants to identify the information that should be documented when performing an ST assessment. In this case, more than half of respondents answered correctly (59%) that the cause, length, width, depth and pain; the type and amount of exudate; integrity of surrounding skin; medications; and general health status, nutrition and mental health status should be documented. Three questions required respondents to classify an ST using the ISTAP Classification System. Just over half of the respondents (51%) answered correctly that the image was a Type 3 skin tear. The second image showed four photos, and the participant had to identify which were Type 1 skin tears. More than three-quarters of the participants (77%) were able to correctly classify these. For the final question in this section, 75% of the participants recognised a Type 2 skin tear.
Risk assessment
Two questions were included in the risk assessment domain. Just over one-third (34%) of the respondents answered correctly regarding why neonates are at risk of developing an ST; that is, they have decreased cohesion between the epidermis and the dermis. A total of 41 respondents indicated that they did not know the answer to this question. Participants were asked to indicate why the long-term use of corticosteroids is considered to be a risk factor in ST development, and 48% answered correctly that they are associated with skin atrophy. An additional 44 respondents selected an incorrect response.
Prevention
There were six questions related to the prevention domain, which focuses on the determination of effective prevention measures to avoid or reduce STs’ occurrence. A majority of respondents (74%) correctly answered that padded wheelchair leg supports were an appropriate preventive measure in the case of a wheelchair patient at risk of an ST on the lower limb. With regards to reasons for applying skin moisturiser to prevent STs, only 39% selected the correct answer, that they replenish the skin’s natural moisture, while 41% of respondents selected the same incorrect answer. A case study was included as a question, and respondents were provided with details about a patient and his medical history. Then, they had to select the most appropriate intervention for ST prevention. Fewer than one-third (30%) indicated the correct answer, which was wearing protective clothing, moisturising the skin and using non-adherent dressings with a silicone coating. Almost half (46%) of respondents selected the same incorrect answer.
Fewer than one-quarter of the respondents (21%) selected the correct response concerning how a humectant supports skin hydration, noting that it draws water from the dermis to the epidermis and compensates for reduced levels of natural moisturisers in the skin. More than one third (38%) of respondents indicated they did not know the answer. Just over half of the respondents (56%) correctly identified which option was not an effective intervention for preventing STs: the use of soap to cleanse the skin. The rest of the participants had varied responses. In the final question, which was related to ST to prevention, respondents were asked to select the most effective option for reducing the risk of developing an ST; only 10 respondents answered correctly that they should minimise the frequency of bathing, if possible.
Treatment
Four questions related to the treatment domain, which focuses on the management of STs and the use of appropriate wound care and dressings. Based on a case study, where an ST was caused following the removal of an intravenous catheter, only 42% of respondents indicated the appropriate care for the patient was to control bleeding, cleanse the wound, re-approximate the skin edges with adhesive strips, manage infection/inflammation and exudate, apply a gauze dressing and then re-assess after 24 hours. With regards to products, respondents had to select one of the products presented to them as best for using with an ST. The results showed that 66% provided the correct response, which was to use non-adherent dressings with a silicone coating.
Respondents also had to select which of three statements were true, with respect to the properties of the ideal dressing for managing an ST. Answers were varied, with only 40% (n=39) of respondents providing the correct answer was 1, 2 and 3. The final question in this section presented a case study involving a Type 2 ST and observations noted after cleansing the wound. Participants were asked to recommend the treatment to apply. Only 22% of respondents selected the correct answer, which was to apply a silicone mesh dressing that can be kept in place for 6–7 days, and then to cover it with a secondary dressing. However, the wound should be cleansed daily without removing the silicone mesh dressing, and a layer of hydrogel should be applied.
Specific patient groups
The final question related to the specific patient groups domain, which is focused on the population at higher risk for ST development. When asked who, out of four possible patient groups, had the highest risk of developing a ST, 76% of respondents answered correctly that premature babies and the elderly are at the greatest risk.
An assessment range was used for each domain, as shown in Table 4. The ranges varied; 0–25% indicated a very poor level of knowledge, 26–50% showed a poor level of knowledge, 51–75% implied a good level of knowledge and 76–100% showed a very good level of knowledge. The correct response rates for all 20 questions under the six domains are shown in Table 5.
Table 4: Assessment ranges used to score knowledge level
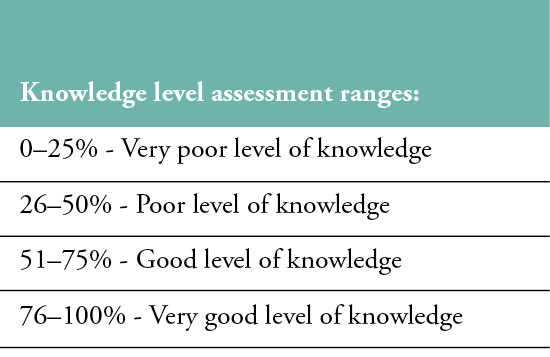
Table 5: Summary of results per question
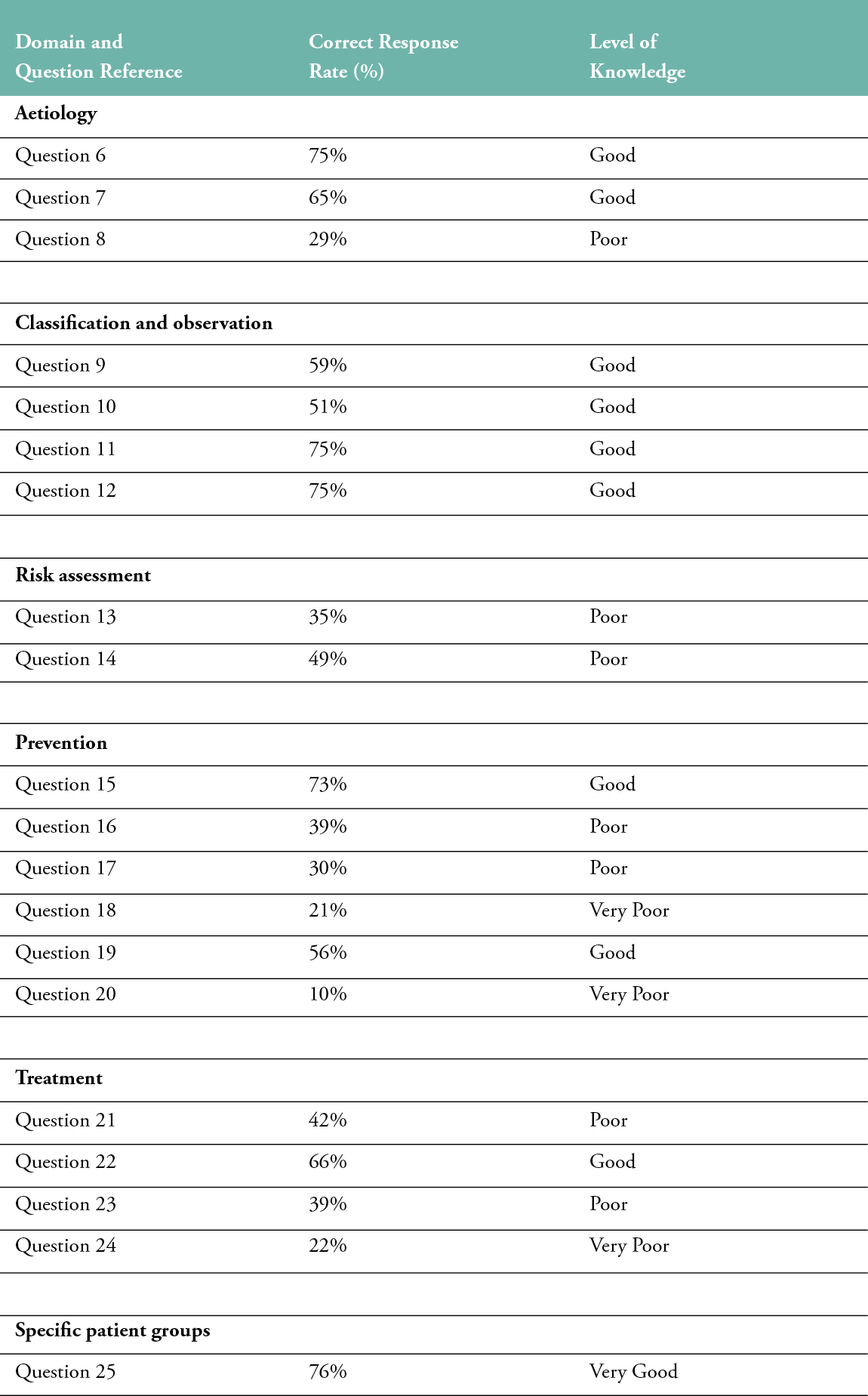
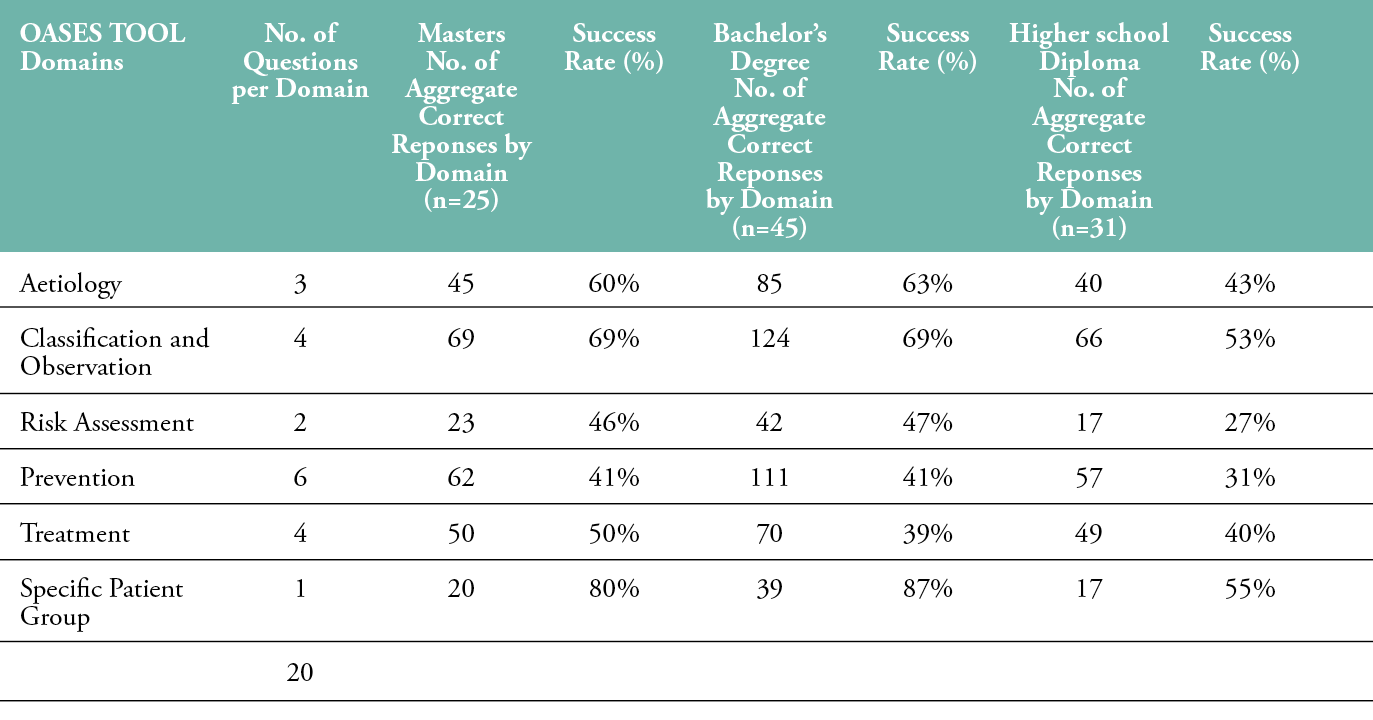
Levels of knowledge and educational background
The results were summarised further in terms of participants’ level of education, clinical experience and (self-reported) monthly exposure to STs (see Table 6). Overall, 76% (n=19) of respondents with a master’s bachelor’s degree and 71% (n=32) of respondents with a bachelor’s degree level earned a passing mark of 50% or higher. However, only 35% (n=11) of respondents with a higher school diploma level of education earned a passing score. Results based on clinical experience did not vary significantly, with the average score ranging from 46–51% and the pass rate ranging from 58–68%.
Table 6: Summary of results for each domain by education level
DISCUSSION
With respect to the aetiology domain, respondents showed overall ‘good’ knowledge; however, some areas within the domain had low scores, for example, Question 2 elicited correct responses in only 42% of cases. A ‘good’ level of knowledge was noted with respect to topics within the classification and observation domain, but response rates varied from one end of the range to the other, which indicates that further understanding is required. ‘Poor’ results were noted on topics in the risk assessment domain; Question 13 attracted correct responses only 35% of the time, and Question 14 had only a 49% correct response rate. The lowest correct response rates were recorded in the prevention domain. Question 15 had 73% correct responses, Question 16 had a 39% correct rate, Question 17 was answered correctly 30% of the time, Question 18 was correct 21% of the time, Question 19 drew a 56% correct answer rate and Question 20 was only answered correctly 10% of the time, although ‘good’ knowledge was noted for a few of the topics in this area. Once again, ‘poor’ results were noted in the treatment domain, where Question 21 had a correct response rate of 42%, Question 22’s rate was 66%, Question 23 was correct 39% of the time and Question 24 was answered correctly by 22% of participants. Finally, a ‘very good’ level of knowledge was recorded within the specific patient groups domain, with a correct response rate of 76% for Question 25.
Respondents with either a master’s or a bachelor’s degree level of education showed ‘very good’ knowledge of the specific patient group domain, and a ‘good’ level of knowledge of the aetiology and classification and observation domains. Respondents with a higher school diploma level of education did not show a ‘very good’ level of knowledge in any of the six domains, but showed a ‘good’ level of knowledge of the classification and observation and specific patient group domains. Respondents across all three levels of education had a ‘poor’ level of knowledge of the risk assessment, prevention and treatment domains. Respondents with a higher school diploma level of education also had a ‘poor’ level of knowledge of the aetiology domain.
A majority of participants answered 50% of the questions correctly; however, the results indicated that further education on the identification, prevention, assessment and management of STs is needed. When looking at the RNs’ years of clinical experience, it was observed that, whilst an average score of 46% was achieved from RNs with less than five years of experience, those with more experience only managed to achieve an average score of 51%. This indicates that knowledge was not being gained through years of experience; this possibly is mainly due to the fact that no educational programmes on STs have ever been delivered to the RNs working at this healthcare facility. The intention of this study is to develop a programme for the hospital to address this gap.
Further analysis of the results indicated that respondents’ scores were between 35–65%, which is insufficient, considering that these RNs work on a daily basis with elderly patients at a heightened risk of STs. While the survey indicated that a majority of respondents (54%) stated they are exposed to 0–2 STs per month, there is a need to assess whether this is due to low ST occurrence within the healthcare facility, or due to a lack of proper ST identification by the RNs. To further investigate this finding, an audit should be conducted to determine the hospital’s ST prevalence level. An additional cross-sectional study should also be performed, to indicate whether wounds are being documented properly. This will indicate whether the RNs’ identifications of STs are accurate. If STs are not being recognised and are documented incorrectly, further education will be needed.
Table 7: Summary of results by education level, clinical experience and ST exposure
Strengths and limitations
The key strength of this study was the creation of a data pool, based on the assessment of RNs’ existing knowledge of the identification, prevention, assessment and management of STs. This pool can now be used as a benchmark for other studies and to track progress at this specific facility. This was the first study of this kind in Malta and may serve as a platform for further studies to be undertaken. Furthermore, the very high response rate of 73.4% provides a representative view of this healthcare facility’s RNs’ knowledge. A further strength of this study was that it has provided useful information for the design of an educational programme to target knowledge gaps, especially within the risk assessment, prevention and treatment domains.
The main limitation of the study was its small sample size and the results being limited to RNs employed by only one healthcare facility. Therefore, the results of the survey may not be generalisable to the overall RN population of the country and may not be easily transferrable to other jurisdictions. Another limitation of the study was the lack of historical information on the baseline prevalence or incidence of STs at this healthcare facility. Such data could have provided useful information for consideration when interpreting the survey results.
Recommendations
Further studies need to be conducted to gain a better understanding of the prevalence and incidence of STs, and to identify the frequency of STs’ occurrence. Such data are required before and after the adoption of BPG within the hospital and the implementation of an education programme, so it is possible to assess the impact of these initiatives on STs’ occurrence. The education programme should be tailored to educate RNs on the existence and implementation of ST tools and train them to evaluate the impact on the outcomes of ST prevention and treatment. Regular updates should also be provided to ensure that RNs remain up to speed with the best practices available. The enhancement of nurses’ knowledge requires strategies related to recent guidelines, tools and protocols and made available in the hospital, so they can focus on the identification, classification, prevention, treatment and management of STs. This will mitigate the RNs’ currently poor awareness of STs. Knowledge may also be enhanced by training undergraduate students, including higher school diploma students, on wound care as a topic in their curriculum, so that their understanding is tested before they graduate. Finally, online resources, such as BPG and slide decks used as part of the educational programme, should be made for all RNs and updated regularly, to ensure that they are following the most recent guidelines.
CONCLUSION
The aim of this study was to determine nurses’ current level of knowledge about the identification, prevention, assessment and management of STs. The use of the OASES tool proved helpful in determining the RNs’ knowledge. Furthermore, knowledge gaps were identified, so they can now be addressed by the proper implementation of an ST classification system, the education of staff and the monitoring of patient outcomes. More specifically, the results showed that, in the domains of aetiology, classification and observation and specific patient groups, there was good knowledge overall. The domains of risk assessment, prevention and treatment are marked by poor knowledge among RNs. Based on the results of this study, we plan to implement existing evidence-based ST protocols and guidelines for the development and dissemination of an educational programme aimed at the areas of ST risk assessment, prevention and treatment.
Acknowledgements
This study was the basis for the Dissertation requirements for the Masters in Wound Healing and Tissue Repair at Cardiff University
Author(s)
Elaine Formosa, Senior Staff Nurse. Karin Grech, Rehabilitation Hospital, Steward Healthcare, Malta.
Samantha Holloway, Reader, Cardiff University School of Medicine, Centre for Medical Education, College of Biomedical and Life Sciences,
Cardiff University, Wales
Correspondence: elaineformosa@gmail.com
Conflict of interest: None
References
- LeBlanc. K· Karen E Campbell, Eleanor Wood and Dimitri Beeckmant et al. Best practice recommendations for the prevention and management of skin tears in aged skin. Wounds Int 2018 45(6):540-542. Available at: [www.woundsinternational.com]. DOI: 10.1097/WON.0000000000000481
- Groom M, Shannon RJ, Chakravarthy D, Fleck CA, et al. An evaluation of costs and effects of a nutrient-based skin care program as a component of prevention of skin tears in an extended convalescent centre. J Wound Ostomy Continence Nurse 2010; 37(1):46-51. Doi: 10.1097/WON.0b013e3181c68c89.
- Clothier A. Assessing and managing skin tears in older people. Nurse Prescribing, 2014; 12(6) 8.23. https://doi.org/10.12968/indn.2014.8.23
- Moncrieff George & Van Onselen, Julie & Young, T et al. The role of emollients in maintaining skin integrity. Wounds UK 2015; 11(1):68–74.
- Van Tiggelen Hanne & Leblanc, Kimberly & Campbell, K. & Woo, Kevin & Baranoski, S. & Chang, Y.Y. & Dunk, Ann & Gloeckner, M. & Hevia, H. & Holloway, Samantha & Idensohn, P. & Karadag, Ayise & Koren, E. & Kottner, Jan & Langemo, D. & Ousey, Karen & Pokorná, Andrea & Romanelli, M. & Santos, V.L.C.G. & Beeckman, Dimitri., et al. Standardizing the classification of skin tears: Validity and reliability testing of the International Skin Tear Advisory Panel Classification System in 44 countries. Br J Dermatol 2020a; 183:146–54.10.1111/bjd.18604
- Payne RL, Martin ML. The epidemiology and management of skin tears in older adults. Ostomy Wound Manage 1990; 26:26–37.
- Payne RL, Martin ML. Defining and classifying skin tears: Need for a common language. Ostomy Wound Manage 1993; 39(5):16–20.
- White W. Skin tears: A descriptive study of the opinions, clinical practice and knowledge base of RNs caring for the aged in high care residential facilities. Primary Intention 2001; 9(4):138.
- Carville, K.J., Lewin, G.F., Newall, N., Haslehurst, P.I., Michael, R., Santamaria, N., & Roberts, P.A. (2007). STAR: A Consensus for Skin Tear Classification. Primary Intention: The Australian Journal of Wound Management, 15, 18-28.
- LeBlanc, K., Baranoski, S., Christensen, D.M., Langemo, D.K., Sammon, M.A., Edwards, K., Holloway, S., Gloeckner, M., Williams, A., Sibbald, R.G., & Regan, M. (2013). International Skin Tear Advisory Panel: a tool kit to aid in the prevention, assessment, and treatment of skin tears using a Simplified Classification System ©. Advances in skin & wound care, 26 10, 459-76; quiz 477-8.
- Chang, Y.Y., Carville, K.J., & Tay, A.C. (2016). The prevalence of skin tears in the acute care setting in Singapore. International Wound Journal, 13.
- Van Tiggelen, H., Alves, P., Ayello, E.A., Bååth, C., Baranoski, S., Campbell, K.E., Dunk, A.M., Gloeckner, M., Hevia, H., Holloway, S., Idensohn, P., Karadağ, A., Langemo, D.K., LeBlanc, K., Ousey, K.J., Pokorná, A., Romanelli, M., Santos, V.L., Smet, S., Williams, A., Woo, K.Y., Van Hecke, A., Verhaeghe, S., & Beeckman, D. (2020). Development and psychometric property testing of a skin tear knowledge assessment instrument (OASES) in 37 countries. Journal of advanced nursing. Mar;77(3):1609-1623. doi: 10.1111/jan.14713. Epub 2020 Dec 10. PMID: 33305504.
