Volume 23 Number 2
Comparison of a cyanoacrylate liquid skin protectant to skin closure strips for the treatment of injury-related Type I skin tears in elderly patients
Rosemary H Hill
Keywords wound healing, Cyanoacrylate liquid skin, skin closure strips, Type 1 skin tears, wound closure
DOI DOI: 10.35279/jowm2022.23.02.07
Abstract
Background A skin tear is a defined as a wound caused by shear, friction or the result of blunt force. Injury-related Type 1 skin tears are more frequent in elderly patients, due to their more fragile and vulnerable skin.
Aim We compared a cyanoacrylate liquid skin protectant (CLSP) to skin closure strips (SCS) for Type 1 skin tear closure and healing in 14 elderly patients.
Methods Eight patients received CLSP alone, three patients received SCS alone and three others received SCS followed by CLSP.
Results For the eight patients treated with CLSP alone, the skin tear flaps annealed almost immediately and were completely closed within 1–3 days. All skin tears were healed within 1–2 weeks of CLSP application. By contrast, for the three cases that were treated with SCS alone, the skin tears remained open for as long as 10 days and required 3–4 weeks to heal. This resulted in prolonged bleeding, delayed skin tear wound healing, re-opening of the skin tear, additional homecare nursing and dressing care. The three patients treated first with SCS followed by CLSP experienced a delay in wound healing; however, when the SCS were removed and CLSP was applied at 1–3 days, wound healing still occurred within 1–2 weeks of the CLSP application.
Conclusions A CLSP alone is an effective treatment for injury-related Type I skin tears in elderly patients.
Implications for clinical practice The use of CLSP decreased the time and costs required for skin tear wound care and reduced the time to wound healing.
INTRODUCTION
A skin tear is defined as a wound caused by shear or friction resulting in the separation of the epidermis from the dermis (partial-thickness) or separation of both the epidermis and dermis from the underlying subcutaneous tissue (full-thickness).1,2 The incidence of injury-related skin tears is frequently caused by falls in elderly patients and is due to mechanical forces such as shearing, blunt trauma, poor handling, equipment injury or the removal of adherent bandages.3 Historically, the Payne-Martin system has been used to describe the severity of a skin tear.1 In this system, Category I refers to a linear tear with no tissue loss, or a flap-type tear where the epidermal flap covers the dermis. A more recently validated system is the International Skin Tear Advisory Panel (ISTAP) classification system, which defines Types 1, 2 and 3 skin tears. A Type 1 tear has no skin loss, with a linear flap tear that can be repositioned to cover the wound bed.4 A Type 2 tear is characterised by partial flap loss that cannot be repositioned to cover the wound bed. Finally, a Type 3 tear entails total flap loss exposing the entire wound bed.4
Elderly patients are commonly affected by skin tears, due to compromised nutrition, previous skin tears or the challenge of using a wheelchair or bed confinement.5 Especially vulnerable are the residents of long-term care (LTC) facilities, where more than 1.5 million skin tears occur each year, with skin tear prevalence among residents at LTC facilities in the US estimated between 16% and 33%.5 6 The prevalence of Payne-Martin category-typed skin tears were reported at a 114-bed Canadian LTC facility. It was found that 25 out of 113 (22%) residents had skin tears.7 Of those reported, 51% were rated with no skin loss (ISTAP Type 1 equivalent), 16% had partial flap loss (ISTAP Type 2 equivalent) and 33% had total flap loss (ISTAP Type 3 equivalent). The most common skin tear locations were the arms (48%), lower legs (40%) and hands (12%).7 In a recent prospective study of 380 individuals >65 years of age, it was confirmed that the prevalence of skin tears was 20.8% in the LTC population, with an incidence rate of 18.9% in four weeks.8 Many states in the US require LTC facilities to track and report their incidence of skin tears.9 Some skin tears are preventable through the use of skin sleeves, padded side rails, gentle skin cleansers, moisturising lotions, disposable diapers and staff education.9,10 Through implementation of these practices at LTC facilities, the incidence of skin tears can be reduced by 50%.10
Treatment of skin tears
Distinguishing between the types of skin tears is essential for choosing appropriate skin care and avoiding unnecessary pain and discomfort to the patient.2,11 Several commercially available skin products have been used for the treatment of skin tears, including non-adherent mesh dressings, foam dressings, hydrogels, cyanoacrylates, alginates, hydro fibres and silver dressings.12,13 In the past, skin tears were routinely treated using adhesive skin closure strips, but these are no longer a preferred treatment.3,14
Skin tear closure methods
In a multi-centre randomised controlled trial, 814 patients with 934 wounds were enrolled; these included 383 lacerations, 235 skin lesions and 316 minimal and general surgeries.15 The study was designed to compare wound closure using 2-octyl-cyanoacrylate (OCA) to standard wound closure (SWC) methods. Overall, wound closure was significantly faster using OCA (2.9 vs 5.2 minutes, p < 0.001); however, the cosmetic appearance was similar at three months.15
A study of elderly patients (mean age of 83) in an LTC facility were treated with cyanoacrylate topical bandages for severe skin tears, including Category 2 (partial flap loss) and 3 skin tears (total flap loss) that were less than eight hours old.5 Out of 20 patients treated, 90% had complete healing with only one application and within one week of treatment. Only one patient reported experiencing pain during treatment.5
A meta-analysis of 26 randomised controlled trials compared the OCA to SWC methods. A total of 2,105 patients with 2,637 wounds were evaluated and compared.16 Sixteen out of the 26 studies directly compared skin sutures to tissue glue. Of the 16 studies, 14 confirmed that the time for skin closure using tissue glue was considerably faster, compared to skin sutures. Eight of 12 studies reported that patients were more satisfied with the use of tissue glue.
In a clinical evaluation of a liquid dressing for minor nonbleeding abrasions and Class 1 and 2 skin tears in the emergency department, 40 adult patients (20–90 years of age) with 39 skin abrasions and 11 skin tears located on the face (n=16), hands (n=14), legs (n=11) and arms (n=9) were treated with 2-octyl cyanoacrylate Marathon™ (Medline Industries, LP).17 All patients were monitored every 1–2 days until complete wound healing was obtained. The median time to complete healing was 10 days (range 7.4–14.0). The complete wound mean healing time was 12.4 days (range 10.8–14.1, occurring in 90% of patients and 92% of wounds treated). Only one wound required additional treatment.
The results of a survey of the members of an ISTAP review panel showed that 85.7% agreed, or somewhat agreed, that cyanoacrylates ‘skin glues’ are appropriate for the treatment of Type 1 and 2 skin tears. Cyanoacrylates have also been used successfully for the treatment of pedal skin fissures, peristomal irritation, and protection against moisture-associated skin damage.18,19,20 In this retrospective case series, we present the data that compared a cyanoacrylate to skin closure strips for the treatment of Type 1 skin tears in elderly patients.
METHODS
Fourteen elderly patients (age 80–98 years) with Type 1 skin tears were evaluated in a retrospective case series at Lions Gate Hospital (a community hospital), in North Vancouver, BC. All patients were treated as outpatients without the need for hospitalisation due to their skin tears. All patients attended an initial nursing visit and two follow-up visits per week between January 2015 and December 2021.
Eight patients (Cases 1–8) were treated exclusively with a cyanoacrylate liquid skin protectant (CLSP) (Marathon™, Medline Industries, LP, Northfield, IL). Three patients (Cases 9–11) were treated exclusively with skin closure strips (SCS) (Steri-Strips™, 3M Corporation, St. Paul, MN) and three patients (Cases 12–14) were treated with a combination of SCS and CLSP. Digital photos of the patients’ wounds were obtained throughout the CLSP and SCS treatments. All patients signed consent and approval for use of the images obtained. This retrospective case series reflects the use of standard practices, whereas the choice of closure method was decided locally at the time of treatment.
In patients who had SCS, these were applied according to the manufacturer’s instructions for use. This requires the skin and skin tear wound area to be cleansed and dried prior to application. The skin tear flap was then approximated to the edge of the skin tear. The SCS were then placed across the wound perpendicular to it and approximately 3 mm apart until the wound was covered. Parallel SCS were applied at approximately 12 mm for the strip ends, in order to reduce the shear force.
For the skin tears treated with CLSP, the solution was applied according to the manufacturer’s instructions. Prior to the CLSP application, the skin tear edges were approximated to the skin tear wound site. The CLSP was dispensed along the skin tear edges from an applicator with ampule. The skin tears were observed for annealing and allowed to dry. All patients received only one application (one ampule) of CLSP. The skin tear was protected from additional trauma by using silicone foam.
RESULTS
A summary of the patients’ demographics, treatment, wound aetiology and cause of skin tear is provided in Table 1. Eight patients were treated with CLSP alone, three patients were treated with SCS alone and another three patients were treated with a combination of CLSP + SCS. Ten patients had single Type 1 skin tears and four patients (Cases 7, 8, 11 and 14) had two Type 1 skin tears. With the exception of one Type 1 (Case 13) skin tear on the face, all skin tears were located on the arms and legs.
Table 1: Summary of Patient Demographics, Treatment and Wound Aetiology
Patient cases treated with CLSP alone
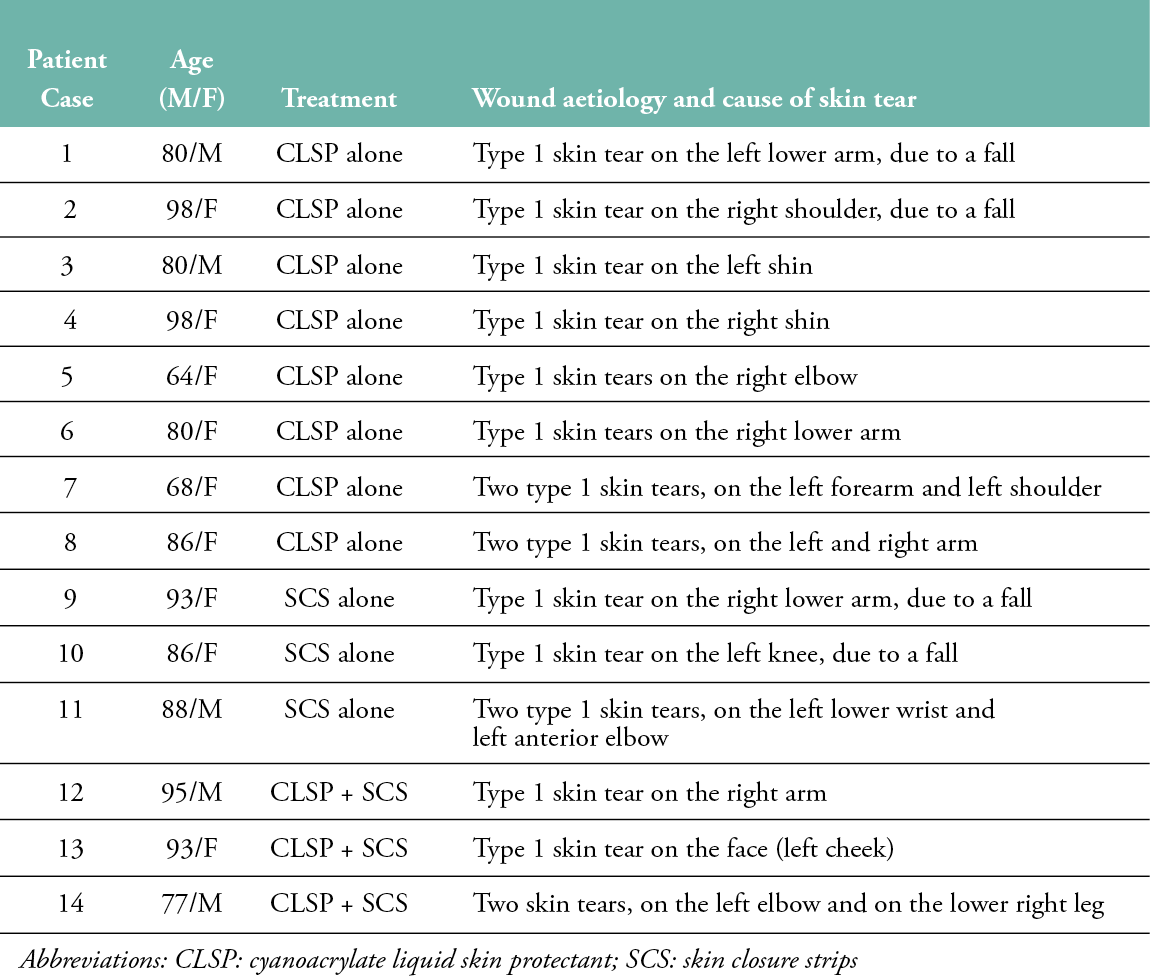
Cases 1 and 2 were patients with Type 1 skin tears of the arm that were, in both cases, caused by falls. Case 1 (Figure 1) was an 80-year-old healthy male who sustained a Type 1 skin tear on the left lower arm. Figure 1, shows images 1A) at Day 0, following flap alignment and prior to CLSP application; 1B) at Day 0, following CLSP application and showing the skin flap was annealed after CLSP was applied to the skin flaps; 1C) at Day 11, showing complete wound closure; and 1D) at Day 18, with complete skin tear healing. Case 2 (image not shown) was a 98-year-old female who sustained a Type 1 skin tear on the right shoulder due to a fall. Following skin flap approximation and alignment, the CLSP was applied. Complete skin tear closure was observed at Day 5, following a single CLSP application.
Figure 1: (Case 1) An 80-year-old healthy male fell and sustained a Type 1 skin tear. Images shown: A) at Day 0, prior to CLSP application; B) at Day 0, immediately after CLSP application; C) at Day 11; and D) at Day 18, following CLSP application.

Cases 3 and 4 were ages 80 and 98 years old, respectively, and provided representation of Type 1 skin tears of the leg. Case 3’s (image not shown) skin tear was caused by a fall that resulted in a Type 1 skin tear of the left shin. Skin tear approximation and flap alignment were performed, followed by CLSP application. By Day 7, the skin tear was completely closed and with no signs of wound dehiscence. Similarly, Case 4 (Figure 2) was a 98-year-old female who sustained a Type 1 skin tear of the right shin that was caused by a sequential compression device. The images in Figure 2 show the skin tear: 2A) at Day 0, prior to CLSP treatment; 2B) at Day 0, immediately after CLSP application; and 2C) at Day 7, after CLSP application. By Day 7, the skin tear was completely closed and there was a good indication of underlying wound site granulation.
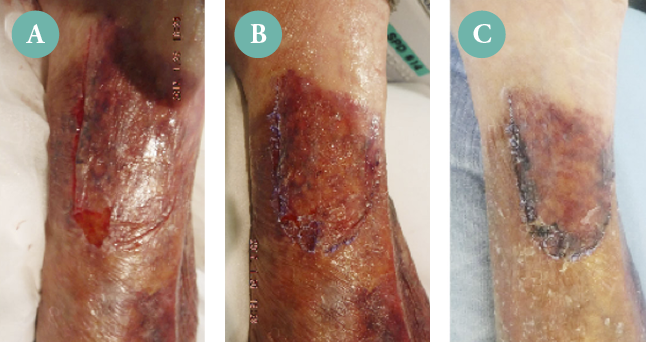
Figure 2: Case 4. A Type 1 skin tear of the right shin. Images shown: A) at Day 0, prior to CLSP application; B) at Day 0, immediately after CLSP application; and C) at Day 7, after CLSP application.
Cases 5 and 6 were Type 1 skin tears on the right elbow and a skin tear of the right lower arm, respectively. They were treated with CLSP alone (images not shown). Type 1 skin tears for both cases were caused by falls. Skin tear flap annealing occurred almost immediately following flap alignment. The skin tears of both Case 5 and 6 were healed within two weeks of CLSP application.
Case 7 (Figure 3) is a patient with two Type 1 skin tears of the left forearm (upper panel: 3A–3D) and shoulder (lower panel: 3E–3H). Shown in Figure 3 are images of both skin tears at Day 0, following skin approximation and application of CLSP (3A and 3E); at Day 3, following CLSP application (3B and 3F); at Day 8, following CLSP (3C and 3G); and at Day 15, following CLSP application (3D and 3H). The skin tears of both the left forearm and left shoulder were nearly healed at Day 15 without signs of dehiscence.
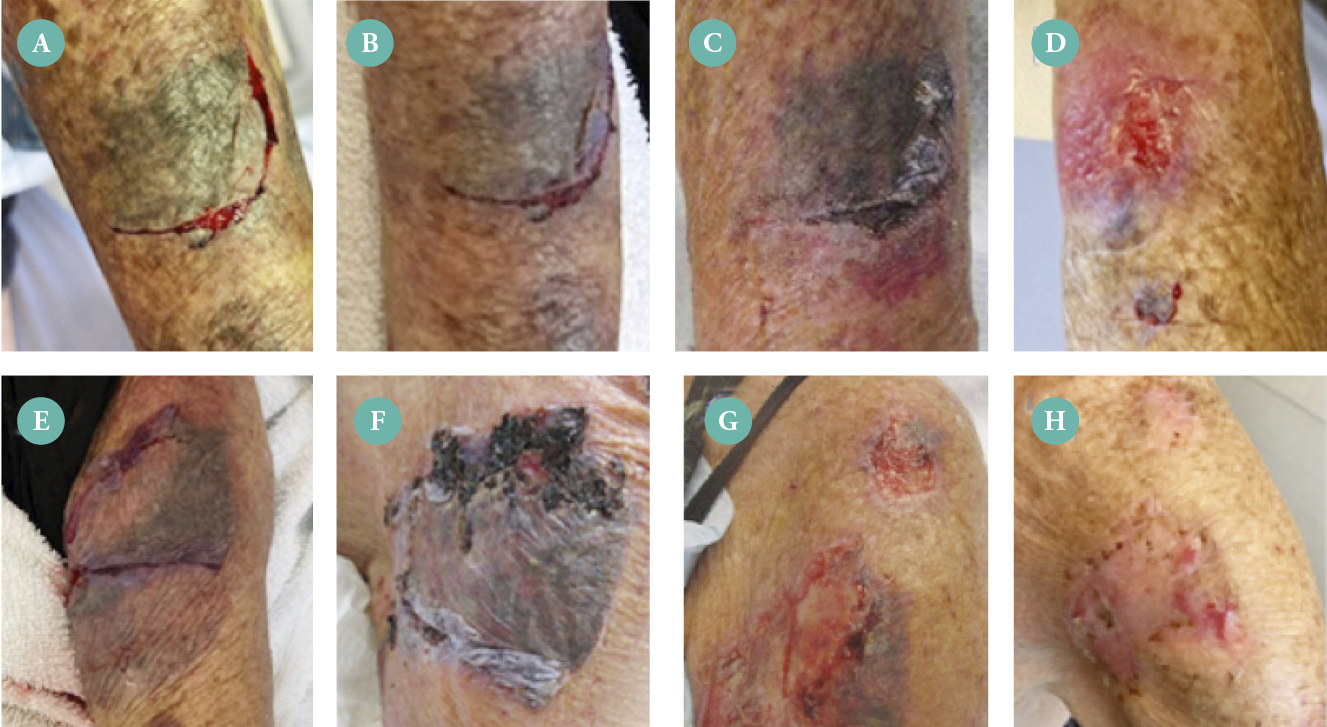
Figure 3: Case 7 with multiple Type 1 skin tears of the left forearm (upper panels) and shoulder (lower panels). Images shown: A and E) Day 0, following CLSP application; B and F) Day 3, following CLSP application; C and G) at Day 8, following CLSP; and D and H) at Day 15, following CLSP application.
Case 8 was another patient with two Type 1 skin tears (images not shown). This patient experienced similar Type 1 skin tears on the left and right arms. Following approximation, flap alignment and CLSP application, skin tear closure was observed by Day 2 for both the left and right arm. Type 1 skin tear healing was observed by Day 12 for the left arm and by Day 14 for the right arm.
In total, eight patients with 10 Type 1 skin tears were treated with CLSP alone. For these eight CLSP only-treated cases, wound closure was observed within 1–3 days following CLSP application, and wound healing was observed within 1–2 weeks of CLSP application. In addition, those patients treated with CLSP alone required one initial nursing visit and four outpatient follow-up visits.
Patient cases treated with SCS alone
Cases 9, 10 and 11 were patient examples of Type 1 skin tears that received SCS alone. Case 9 (Figure 4) was a 93-year-old female patient with a Type 1 skin tear located on the right lower arm that was caused by a fall. Shown in Figure 4 is the skin tear of the right lower arm: 4A) at Day 0, following SCS application; 4B) at Day 10, prior to SCS removal and application of a non-adherent silicone foam bandage; and 4C) at Day 24, with silicone foam bandage. As shown, the wound shows dehiscence at Day 10 and required additional healing time. At Day 24, there were additional signs of bruising that caused delayed healing for an additional two weeks.

Figure 4: Case 9. Type 1 skin tear of the right lower arm. Images shown: A) at Day 0, following application of SCS; B) at Day 10, prior to SCS removal; and C) Day 24, with silicone foam bandage.
Case 10 (Figure 5) is an 86-year-old patient with a Type 1 skin tear located on the left knee caused by a fall. Shown in Figure 5 is the skin tear of the knee 5A) at Day 0, prior to SCS application; 5B) at Day 0, after SCS application; 5C) at Day 7, prior to SCS removal; and 5D) at Day 7, after SCS removal. The wound shows dehiscence and failure of the skin tear to completely close at Day 7, thereby delaying healing up to five weeks.
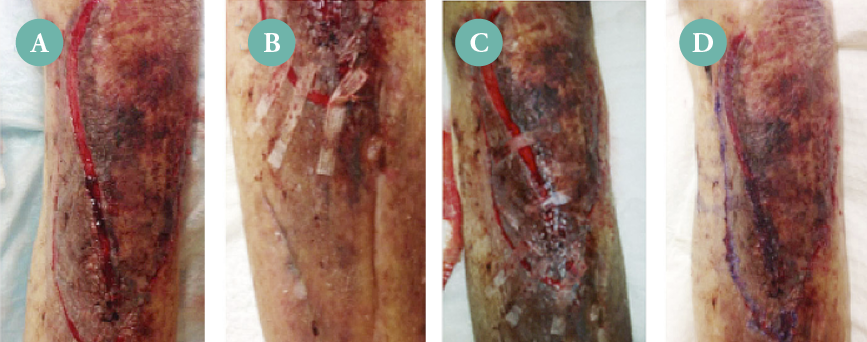
Figure 5: Case 10. Type 1 skin tear of the left knee. Images shown: A) at Day 0, prior to SCS application; B) at Day 0, after SCS application; C) at Day 7, with SCS; and D) at Day 7, with SCS removed.
Case 11 (Figure 6 top panel) is an example of a Type 1 skin tear after just two days of treatment with SCS. The patient presented to the ER with an open and bleeding wound. The images for Case 11 show Type 1 skin tears of the right lower wrist (6A and 6B) and the right anterior elbow (6C). Shown is the skin tear on the left lower wrist after two days before SCS removal (6A) and after SCS dislodgement and removal (6B). The size of the open skin tear wound of the wrist was measured to be approximately 10 cm. Image 6C shows the left anterior elbow after two days with the SCS partially dislodged. As was observed for the skin tears of the wrist and elbow, the dislodgement of SCS at Day 2 led to re-opening and delayed healing of the skin tear wounds. Follow-up treatment for Case 11 included every three days with hydrophilic wound interface and a cover dressing until closure at 3–4 weeks.
Case 12 (Figure 6 bottom panel) is a 95-year-old male with a medical history of congestive heart failure, under palliative care as a result of cancer. The patient fell due to mobility issues and sustained a Type 1 skin tear of the right arm. SCS were first applied but later removed at 12 hours (6A). The CLSP was then applied to the skin flap edge to anneal the skin tear flap to the wound edge (6B). Images taken at Day 2 following CLSP application show that the skin tear wound was completely closed.
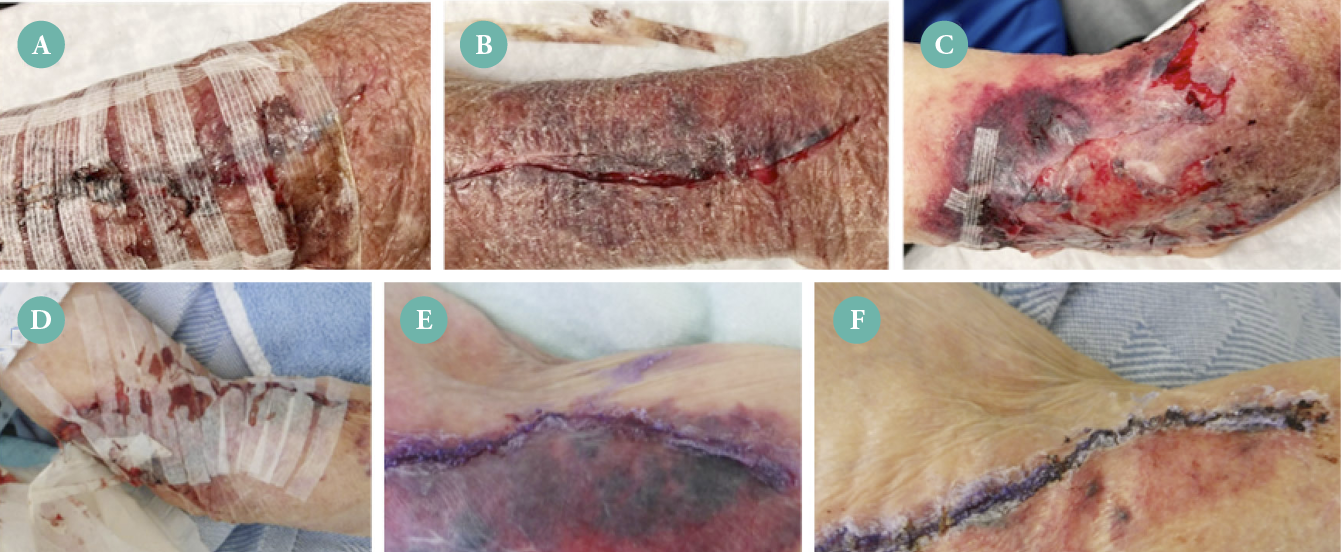
Figure 6: Comparison of Type 1 skin tear closure using SCS or CLSP. Case 11 (upper panel). Type 1 skin tears of the wrist and elbow after two days of treatment with SCS. Images shown: A) wrist at Day 2, prior to SCS removal; B) wrist at Day 2, following SCS removal; C) elbow at Day 2 of treatment with SCS. Case 12 (lower panel) with Type 1 skin tear of the right elbow. Images shown: D) after 12 hours of SCS treatment; E) after SCS were removed and CLSP was applied; and F) Day 2, following CLSP application.
Case studies 9, 10, 11 and 12 emphasise the importance of early wound closure of Type 1 skin tears that is not possible using SCS alone. The wound develops into more than a skin tear when it requires homecare nursing several times per week for up to 3–4 weeks. With CLSP, the skin tears close quickly and thereby avoid substantial homecare nursing and long-term dressing care. In contrast to patients treated with CLSP alone, the three patients (Cases 9, 10 and 11) who were treated exclusively with SCS experienced delayed skin tear closure and open wounds after SCS removal. Wounds remained open after the SCS were removed and showed delayed healing, requiring up to 3–4 weeks of treatment.
In total, three patients with four Type 1 skin tears were treated with SCS alone. For these three SCS only-treated cases, wound closure required up to 10 days following SCS application, and wound healing was observed within 3–4 weeks. In addition, those patients treated with SCS alone required one initial nursing visit and as many as 12 outpatient follow-up visits.
Patient cases treated with SCS followed by CLSP
Although most Type 1 skin tears occur on the arms and legs, we did observe a Type 1 skin tear of the face (left cheek) of a 93-year-old that was caused by a fall. Case 13 (Figure 7) images shown are: A) at 12 hours, with SCS applied to the skin tear; B) at 12 hours, after SCS removal followed by CLSP application; C) at Day 2, with purple bruising noted under the skin because of the fall; D) at Day 14; and E) at Day 16 from the initial injury, showing good wound healing. Case 13 displayed delayed wound closure with SCS, but demonstrated good wound healing once switched to CLSP. We also observed that bleeding and re-opening of the wound were better controlled with CLSP application, compared to SCS. The patient reported minimal scarring at 1 month. Other patients reported similar observations at 1–2 months.
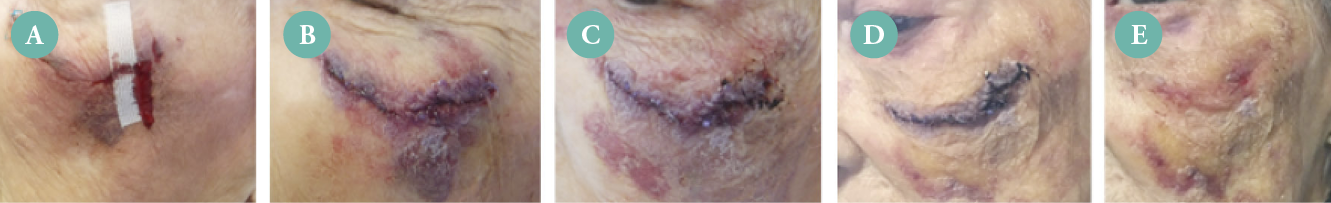
Figure 7: Case 13. Left check of the face with images shown: A) at 12 hours with SCS treatment, B) at 12 hours after SCS removal and CLSP application, C) at Day 2, D) at Day 14 and E) at Day 16.
Case 14 (Figure 8) is a 77-year-old patient who had a fall in the garden that resulted in two Type 1 skin tears, on the left elbow (Figure 8 upper panel) and right lower leg (Figure 8 lower panel). The patient had numerous co-morbidities, including dependence on home oxygen. For treatment of the left elbow, images are shown: 8A) at Day 2, with SCS dislodged; 8B) at Day 2, with SCS removed; 8C) at Day 2, with CLSP applied; 8D) at Day 12, with skin tears on the elbow completely closed and well healed. For the Type 1 skin tear of the right lower leg (Figure 8 lower panel), images are shown: 8E) at Day 2, with SCS dislodged; 8F) at Day 2, with SCS removed; 8E) at Day 2, with skin tear flaps aligned and CLSP applied; 8G) at Day 12, with continued healing; and 8I) at Day 18, with near complete healing. Due to excessive oedema of the leg, the patient required compression socks during the course of treatment.
In total, three patients with four skin tears were treated first with SCS and then CLSP was applied at 1–3 days. Similar to CLSP alone-treated patients, Type 1 skin tear wound healing still occurred within 1–2 weeks of the CLSP application. In addition, those patients treated with SCS and CLSP required one initial nursing visit and 4–6 outpatient follow-up visits.

Figure 8 (Upper Panel): Case 14. Type 1 skin tear of the left elbow with images shown: A) SCS at Day 2; B) SCS removed at Day 2; C) CLSP applied at Day 2; and D) at Day 12, with complete wound closure.
Figure 8 (Lower Panel). Case 14. Type 1 skin tear of the right lower leg with images shown: E) SCS at Day 2, F) SCS removed at Day 2, G) CLSP applied at Day 2, H) at Day 12 and I) at Day 18.
DISCUSSION
In 2010, Groom, et al. estimated a total cost of $287 to $332 per resident per month (25 days) for the care of skin tears in an LTC facility, based on the costs of supplies and labour.21 However, reduced clinician time and decreased costs have been reported with the use of cyanoacrylates to treat skin tears.5,22 For our case series, all patients required one initial outpatient visit for treatment. Subsequently, for patients with CLSP only, four follow-up visits were required, in contrast to the SCS-treated patients, who required up to 12 follow-up visits. Based on current estimates, with skilled nursing costs as much as $150 per visit, the costs for five CLSP treatment visits (1 initial and 4 follow-up visits) would be estimated at $750. In contrast, the costs for 13 (1 initial and 12 follow-up visits) would be estimated at $1950 (personal experience). This would represent an approximately 67% savings in nursing time and healthcare costs for CLSP-treated patients, compared to SCS-treated patients. The material costs of the CLSP and SCS were similar, at approximately $5 per treatment.
Cyanoacrylate adhesives are designed to adhere and dry within 1–2 minutes of application and to slough off naturally within 1–3 days, as the underlying skin heals. However, when used for the treatment of minor non-bleeding abrasions, including skin tears, sloughing off of the adhesive has been reported to be as long as 5–10 days, with no need to remove the adhesive.23 In our case series, we compared CLSP to SCS for Type 1 skin tear closure and healing in 14 patients. We observed for the eight cases treated with CLSP that, following skin flap alignment, wound annealing to skin flap edges was almost immediate for Type 1 skin tears. This was in contrast to the three cases that were treated with SCS alone, where the wounds remained open for as long as 10 days after SCS treatment, requiring 3–4 weeks to heal. This resulted in prolonged bleeding, delayed skin tear wound healing, re-opening of the skin tear and additional homecare nursing and dressing care. In contrast, the CLSP-treated skin tear flaps were annealed almost immediately and completely closed within 1–3 days of application. In our case series, we did not observe any allergic reactions to CLSP or SCS; however, other investigators have reported allergic contact dermatitis in 2–3% of patients following the use of cyanoacrylates topical skin adhesives to repair foot and ankle surgeries.24
Three patient cases were treated first with SCS followed by CLSP application. However, when the SCS were removed and CLSP was applied at 1–3 days, there was a slight delay in wound closure, but wound healing still occurred within 1–2 weeks of the CLSP application. The practice of using SCS for Type 1 skin tears should be re-evaluated for each case, due to the fact that this can delay overall wound healing, as we have demonstrated in this case series. The ISTAP best practices recommendations are to avoid the use of SCS because of the fragility of aged skin and because Type 1 skin tears are generally not as deep as other types of wounds.3 In some cases, it may be necessary to close larger skin tears with SCS; however, it should be kept in mind that this practice may reduce flap annealing, re-open the skin tear and prolong wound closure. The results of this case series indicate that, whenever possible, CLSP should be applied first to Type 1 skin tears and that SCS should be avoided for these skin tears. Our results are supported by other experts’ opinions, which suggest that SCS are not appropriate for skin tear management.12 While prevention is preferable to treatment, CLSP is a viable treatment option available for Type 1 skin tears.
CONCLUSION
Based on the observations of this case series, we conclude that CLSP can be used as a rapid and effective treatment for injury-related Type 1 skin tears of the arms, legs and face in elderly patients. Skin tear flap annealing occurred within minutes of CLSP application. Skin wound edges annealed rapidly, thereby promoting faster skin tear closure and wound healing, compared to SCS alone. In addition, CLSP was easy to use and provided better wound closure, even with only one CLSP application. Skin tear closure was complete within 1–3 days of CLSP application, with wound healing at 1–2 weeks after treatment with CLSP alone. When compared to SCS alone, wound closure required up to 10 days and 3–4 weeks for wound healing. In addition, CSLP decreased Type 1 skin tear closure and healing time, which resulted in a 67% savings in healthcare time and costs, compared to SCS-treated Type 1 skin tears. We also found that CLSP could reduce scarring of Type 1 skin tears located on the arms, legs and face. This was an incidental finding based on clinical observation and patients’ personal observations. In a review study, the cosmetic results using cyanoacrylates to close surgical wounds or lacerations have been shown to be superior or equivalent to sutures.23
IMPLICATIONS FOR CLINICAL PRACTICE
- A cyanoacrylate liquid skin protectant (CSLP) can be used to treat Type 1 skin tears in elderly patients.
- When compared to skin closure strips (SCS), we observed a decrease in the time and cost required for skin tear wound care and reduced time to wound healing.
- One application of CSLP was sufficient to effectively anneal Type 1 skin tears.
- CLSP was still able to heal Type 1 skin tears that were initially treated with SCS and removed within 1–3 days.
Limitations of the case series
This retrospective case series included a small number of patients for SCS alone and CLSP with SCS (three patients per group), and eight patients were included in the CLSP alone group, for a total of 14 patients in the study. Although promising results were observed, due to the small sample size, additional study is warranted with a larger sample size.
Future research
Future studies are warranted to evaluate if CLSP may be an option for treating Type 2 skin tears where there is partial skin flap loss. In addition, a patient satisfaction survey with regard to CLSP use on skin tears would also be beneficial, including pain management, scarring and personal care (e.g., showering or bathing).
Key messages
- A cyanoacrylate liquid can be used as a rapid and effective treatment for injury-related Type 1 skin tears on the arms, legs and faces of elderly patients.
- Skin tear wound edges annealed rapidly, thereby promoting faster skin tear closure and wound healing compared to skin closure strips alone.
- The use of a cyanoacrylate liquid skin protectant decreased the time and costs required for skin tear wound care and reduced the time for wound healing.
- Skin closure strips are not recommended for the treatment of Type 1 skin tears.
Author(s)
Rosemary H Hill, BSN, CWOCN, WOCC(C)a and Stephen L. Smith, PhDb
a Vancouver Coastal Health, Lions Gate Hospital, North Vancouver, BC, Canada
b Medline Industries LP, Northfield, IL, USA
Correspondence: Rosemary.hill@vch.ca
Conflict of interest: None
References
- Payne RL, Martin MC. Defining and classifying skin tears: Need for a common language. Ostomy Wound Manage 1993; 39(5):16–26.
- LeBlanc K, Baranoski S. Skin tears: State of the science: Consensus statements for the prevention, prediction, assessment, and treatment of skin tears. Adv Skin Wound Care 2011; 24(9 Suppl):2–15.
- LeBlanc K. Campbell KE, Wood E, Beeckman D. Best Practice Recommendations for Prevention and Management of Skin Tears in Aged Skin: An Overview. J Wound Ostomy Continence Nurs. 2018 Nov/Dec;45(6):540-542. doi: 10.1097/WON.0000000000000481.
- LeBlanc K, Baranoski S, Holloway S, Langemo, D. Validation of a new classification system for skin tears. Adv Skin Wound Care 2013; 26(6):263–5.
- Milne CT, Corbett LQ. A new option in the treatment of skin tears for the institutionalized resident: Formulated 2-octylcyanoacrylate topical bandage Geriatr Nurs 2005; 26:321–5.
- LeBlanc K, Kozell K, Martins L, Forest-Lalande L, Langlois M, Hill M. Is twice-daily skin moisturizing more effective than routine care in the prevention of skin tears in the older adult population? J Wound Ostomy Continence Nurs 2016; 43(1):17–22.
- Leblanc K, Christensen D, Cook J, Culhane B, Gutierrez O. Prevalence of skin tears in a long-term care facility. J Wound Ostomy Continence Nurs 2013; 40(6):580–4.
- LeBlanc K, Woo KY, VanDenKerkhof E, Woodbury MG. Skin tear prevalence and incidence in the long-term care population: A prospective study. J Wound Care 2020 Jul 1; 29(Sup7):S16–22.
- Wick JY, Zanni GR. Skin tears: Prevention and treatment. Consult Pharm 2008; 23(7):508–10.
- Hodgkinson B, Nay R. Effectiveness of topical skin care provided in aged care facilities. JBI Libr Syst Rev 2005; 3(4):1–56.
- LeBlanc K, Baranoski S, Christensen D, Langemo D, Sammon MA, Edwards K. International skin tear advisory panel: A tool kit to aid in the prevention, assessment, and treatment of skin tears using a simplified classification system. Adv Skin Wound Care 2013; 26(10):459–76.
- LeBlanc K, Baranoski S, Christensen D, Langemo D, Edwards K, Holloway S. The art of dressing selection: A consensus statement on skin tears and best practice. Adv Skin Wound Care 2016; 29(1):32–46.
- Singer AJ, Quinn JV, Hollander JE. The cyanoacrylate topical skin adhesives. Am J Emerg Med. 2008 May;26(4):490-6.
- Holmes RF, Davidson MW, Thompson BJ, Kelechi TJ. Skin tears: Care and management of the older adult at home. Home Healthcare Nurse 2013; 31(2):90–101.
- Singer AJ, Quinn JV, Clark RE, Hollander JE, TraumaSeal Study Group. Closure of lacerations and incisions with octylcyanoacrylate: A multicenter randomized controlled trial. Surgery 2002 Mar; 131(3):270–6.
- Chow A, Marshall H, Zacharakis E, Paraskeva P, Purkayastha S. Use of tissue glue for surgical incision closure: A systematic review and meta-analysis of randomized controlled trials. J Am Coll Surg 2010 Jul; 211(1):114–25. doi: 10.1016/j.jamcollsurg.2010.03.013.
- Singer AJ, Chale S, Taylor M, Domingo A, Ghazipura S, Khorasonchi A, et al. Evaluation of a liquid dressing for minor nonbleeding abrasions and class I and II skin tears in the emergency department. J Emerg Med 2015 Feb; 48(2):178–85.
- Vlahovic TC, Hinton EA, Chakravarthy D, Fleck, CA. A review of cyanoacrylate liquid skin protectant and its efficacy on pedal fissures. J Am Coll of Cert Wound Specialists 2010; 2:79–85.
- Milne CT, Saucier D, Trevelini C. Evaluation of a cyanoacrylate dressing to manage peristomal skin alterations under ostomy skin barrier wafers. J Wound Ostomy Continence Nurs 2011; 38(6):676–9.
- Woo KY, Beeckman D, Chakravarthy D. Management of moisture-associated skin damage: A scoping review. Adv Skin Wound Care 2017; 30(11):494–501.
- Groom M, Shannon RJ, Chakravarthy D, Fleck, CA. An evaluation of costs and effects of a nutrient-based skin care program as a component of prevention of skin tears in an extended convalescent center. J. Wound Ostomy Continence Nurs 2010; 37:46–51.
- LeBlanc K, Christensen D. Evaluation of a cyanoacrylate liquid skin protectant for the treatment of Type 1 and 2 skin tears at a long-term care facility. Wounds Inter 2020; 11:2:40–6.
- Singer AJ, Quinn JV, Hollander JE. The cyanoacrylate topical skin adhesives. Am J Emerg Med 2008 May; 26(4):490–6.
- Park YH, Choi JS, Choi JW, Kim HJ. Incidence and risk factor of allergic contact dermatitis to 2-octyl cyanoacrylate and n-butyl cyanoacrylate topical skin adhesives. Sci Rep 2021 Dec 9; 11(1):23762.
