Volume 23 Number 2
Analysis of real-world data from North American skilled nursing facilities’ skin and wound records for skin tear prevalence, healing and treatment
Robert D. J. Fraser, Rishabh Gupta, Amy Cassata, Heba Tallah Mohammed, Justin Allport, Sheila C. Wang, Jose L. Ramirez-GarciaLuna
Keywords prevalence, healing, skin tear
DOI 10.35279/jowm2022.23.02.08
Abstract
Background Ageing populations are at risk of skin tears due to changes in their skin. Real-world data sets offer the ability to see current prevalence rates and practice changes to understand the size of the problem and glean practice insights.
Aim Leveraging Swift Medical’s big data set, a point-prevalence analysis was conducted over five years on skin tears in skilled nursing facilities (SNF) in North America, to better understand time to heal and explore the frequency of commonly used treatments and cleansing solutions for skin tears.
Methods This descriptive prevalence study used a subset of an anonymised big dataset from participating SNFs across North America. Data from 188,675 skin tears in patients aged 20 years of age or older from 2017–2021 were included. Relative prevalence compared to other wounds was analysed, and healing times based on skin tear classification and frequency of primary, secondary and cleansing solutions were reported.
Results More than 1.5 million wounds were included in this dataset, and skin tears accounted for 10.3–12.8% of skin tears in SNFs over the five-year period. The prevalence of skin tears increased with age. Median healing time ranged from 15–27 days, based on skin tear classification.
Conclusion Big data sets can provide insight into current wound prevalence and practice patterns. The high prevalence of skin tears highlights the need for standardised tools to assess risk and prevent skin tears, and to educate clinicians on classifying and treating skin tears effectively.
INTRODUCTION
Skin tears are acute wounds where the epidermis is partially or fully separated from the underlying skin structures.1 They are usually caused by mechanical trauma, such as blunt forces, chafing or friction. Although most skin tears are considered minor wounds1, if not adequately treated, they can rapidly progress into chronic complex wounds.2-6
Skin tears are identified as one of the most common wounds among older patients.7 They can also happen among neonates, the critically ill or disabled populations.6,8 Internationally, the prevalence and incidence of skin tears across skilled nursing facilities (SNF) (long-term care and nursing organisations) and hospitals have been explored. Evidence showed that SNFs record the highest incidence rate of skin tears, accounting for up to 92%, and a prevalence rate of up to 26%8 in traditional studies.
A comprehensive understanding of skin tears’ prevalence in SNFs is necessary to inform comprehensive prevention and management strategies that support standardised assessment and better treatment plans. Delayed or inappropriate management and prolonged care may negatively impact the quality of patient care.9
The high prevalence and incidence of skin tears poses a challenge to SNFs. An international study from 16 countries found organisations reported that a lack of reliable assessment tools, poor documentation of skin tears and systematic under-reporting are common barriers to the proper management of these wounds. More than two-thirds of clinicians reported substantial issues with their classification and documentation.10
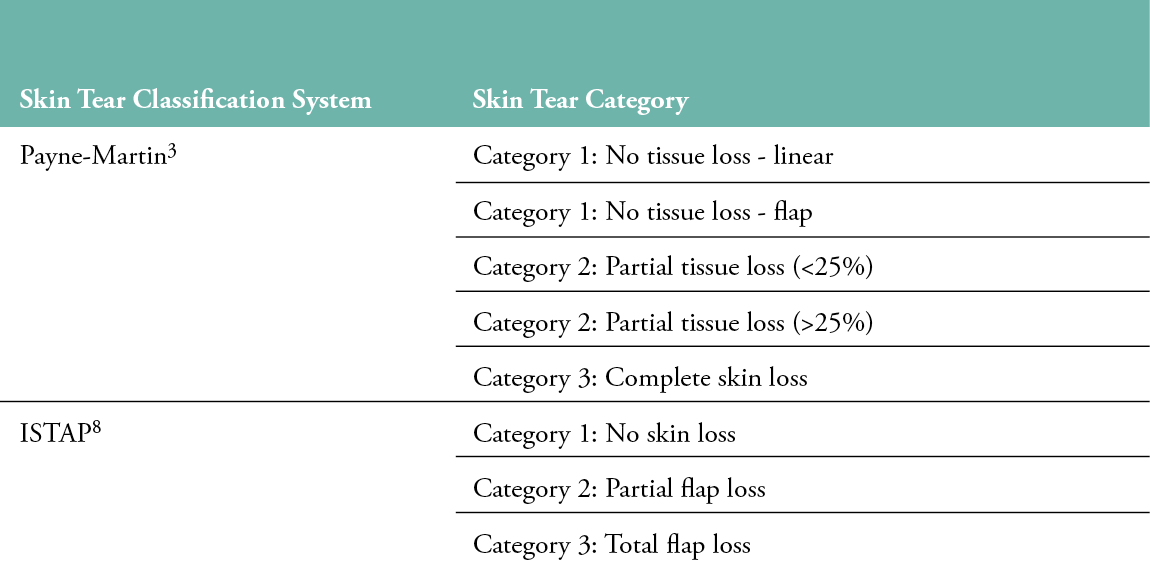
Currently, at least three scales classify skin tears (Table 1). One of these tools ranks skin tears based on the percentage of tissue loss (the Payne-Martin classification). Another adds a skin flap colour distinction (Skin Tear Audit Research [STAR] Classification system).8 However, evidence suggests that clinicians found these tools too complicated to use in practice, or that they lack standardised terminology.11 Therefore, the International Skin Tear Advisory Panel (ISTAP) Classification System was developed to simplify assessment.8 The system is based on the severity of the skin flap’s loss and categorises skin tears with no skin/flap loss as Type 1, tears with partial skin/flap loss as Type 2 and those with complete skin/flap loss as Type 3.8
Table 1: Skin Tear Classification Systems
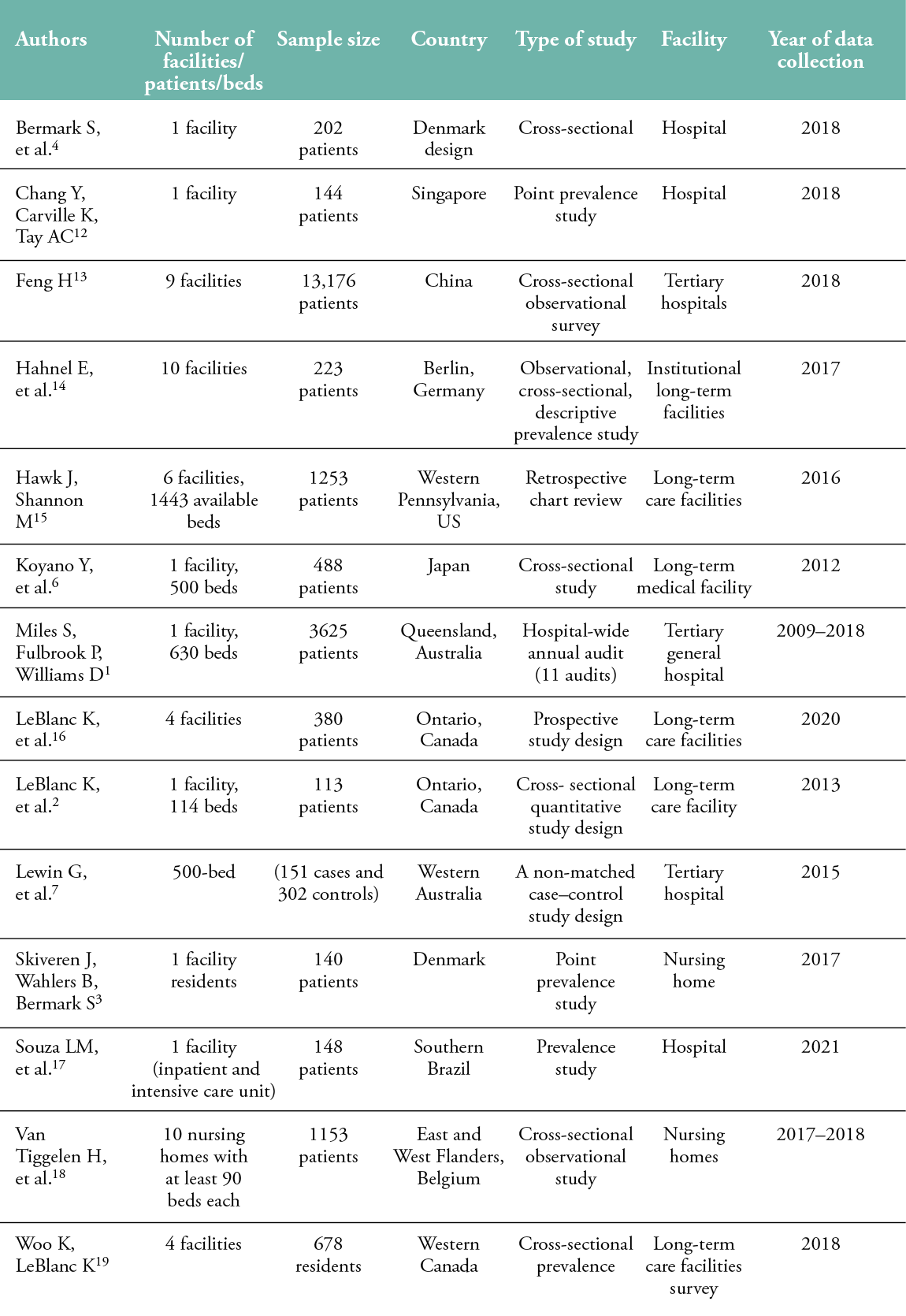
A number of studies have explored the frequency of skin tears across different facilities (Table 2). The data from these studies reflect a wide geographical location, but are generally limited to single facilities, are smaller in size and are mainly cross-sectional.
Table 2: Skin Tear Prevalence Studies, 2012–2018
Digitally collected health information for clinical documentation offers real-world evidence obtained directly from clinical practice in significantly larger numbers than traditional trials. With appropriate controls and analysis in place, regulators, such as the U.S. Food and Drug Administration, are beginning to accept these data sets as compelling evidence to support indications for medical interventions.20 Using data generated by clinical practice can lower barriers to studying issues and provide access to information about populations that may be excluded from randomised controlled trials, though the challenges of using big data need to be considered. Still, real-world data may address limitations and biases faced by traditional studies (e.g., inclusion criteria, selection bias, information bias).20
A wound management solution (Swift Skin and Wound, Swift Medical Inc.) comprised of a smartphone-based wound application and browser-based dashboard. This wound management solution uses artificial intelligence to capture quality images and provide standardised automatic wound measurement, enabling the easy tracking of wound progress and changes over time. Wound evaluation data collected at the point-of-care from different organisations and facilities are stored by the wound management solution, from which participating organisations’ data are anonymised for research, resulting in a significantly large high-quality dataset ready for exploration and analysis. This study used a North America (NA) subset of the large database and builds on Au and colleagues’ work conducted on a sample of 23,453 residents’ records in SNFs to understand the frequency of skin wounds and lesions and their location.21
The objective of this study was to analyse skin tear point prevalence over a five-year period in SNFs across NA, assess the time to heal these wounds and the most frequent treatments documented.
METHODS
Study Design and Sampling Procedure
This descriptive prevalence study used a subset of anonymised data to collect information on skin tears from participating SNFs across the United States and long-term care facilities in Western and East-Central Canada. Swift complies with privacy requirements under the Health Insurance Portability and Accountability Act in the United States and the Personal Health Information Protection Act in Canada. All patients’ identifying information is removed using the Safe Harbor Process.22 Swift endorses the European Medical Association Declaration of Helsinki for human subjects research. Review of the anonymised wound data set does not involve intervention or impact the care provided, yet can improve our understanding of wounds and improve wound care treatment.
For this study, we included SNFs’ wound documentation from organisations that include the ISTAP or Payne-Martin skin tears classifications. No organisations or facilities were using the STAR classification system. Inclusion criteria for wound evaluations included patients older than 20 years of age, with a wound less than 365 days old. Data before 2017 and after 2021 were excluded, as the full year of data was not available. Evaluations from more than 2,200 facilities monitoring 1,541,884 wounds, including 188,675 skin tears documented by more than 20,000 clinicians (Registered Nurses, Licensed Practical Nurses) from 75,655 patients, were included. Data were summarised into reports comparing the relative wound prevalence of skin tears to all wound types recorded, analyses of the body locations of the skin tears, analyses of healing times and primary treatment types identified.
Data Extraction
The data were extracted from an anonymised cloud data warehouse. With it, we could leverage Structured Query Language (SQL) to query and extract the data, based on the inclusion criteria laid out above, along with the computing summary statistics measures (e.g., frequency, mean, median, standard deviation) reported below. Using SQL queries, we extracted wound characteristics, such as location, aetiology, date of the first evaluation and wound healing status, along with the unique corresponding facility, clinician and patient-level information (e.g., age and sex) from our data warehouse. The patient’s age was grouped into one of 10 different cohorts, where each cohort was set 10 years apart (i.e., ≥ 0–<10, ≥ 10 –<20, …). Patients aged 90 and older were all grouped into one cohort.
Data analysis
To compute the prevalence of skin tears per year, separate groups were created in cohorts of data grouped by the year when the first evaluation for a wound was created. This resulted in five cohorts corresponding to each year that spanned our dataset. Within each cohort, we computed the frequency of skin tears and all other wounds belonging to different aetiologies. These frequencies were then used to compute the ratio of skin tears amongst a plethora of other wound aetiologies (e.g., pressure injuries, diabetic wounds, venous ulcers). The ratio allowed us to track the prevalence of skin tears per year within our dataset. Additional prevalence analyses were applied for the patient’s sex and age cohorts. Patients missing biological sex data were not excluded from the analysis, but were reported as ‘not assigned’.
Time to heal was computed for each wound by subtracting the first evaluation date from the final evaluation date when the wound was tagged as healed. There were a few wounds within the dataset where the precise start date was not provided; therefore, to be consistent, we assumed the first evaluation date as the starting date for the wound. Subsequently, we computed summary statistics measures across various cohorts of skin tear categorisation systems (i.e., ISTAP and Payne-Martin), age groups, year of first evaluation and sex; these are reported below.
SQL queries of the data warehouse were used to group evaluations by more than 100 different body locations, and then by wound aetiologies. Data were then summarised into descriptive tables to report the frequency of each wound type across each body location. Values in the descriptive table were scaled between 0 and 1 (using a denominator corresponding to the maximum number of wounds across body locations) and then used to generate heat maps at each body location. Additional SQL aggregations were performed to isolate wound locations of a specific wound type, to produce body heat maps for specific wounds.
RESULTS
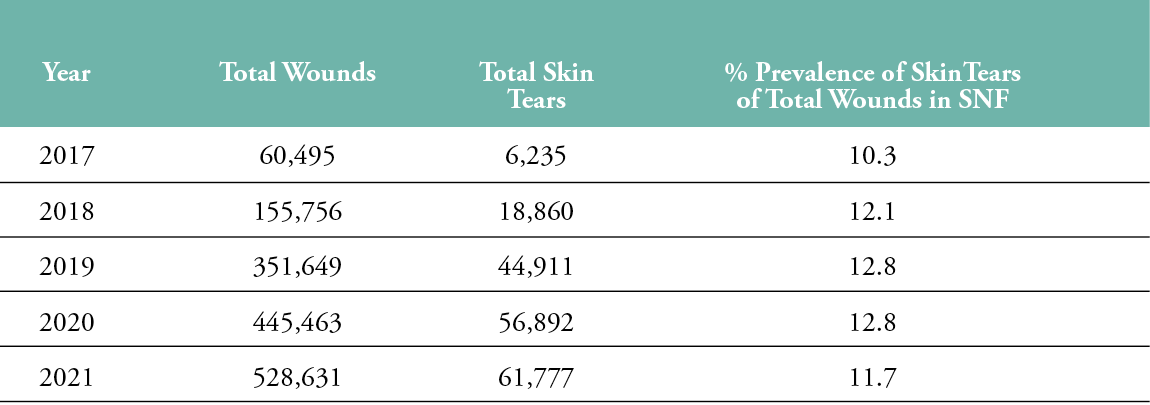
A subset of 1,541,944 wounds from the larger dataset selected based on inclusion–exclusion criteria and quality analysis from the selected five years was used for the subsequent analysis. Table 3 shows an increase in wounds monitored each year, yet a relatively consistent percentage of skin tear prevalence, between 10.3 and 12.8% compared to all wound types.
Table 3: Skin Tear Prevalence from 2017–2019 in Skilled Nursing Facilities
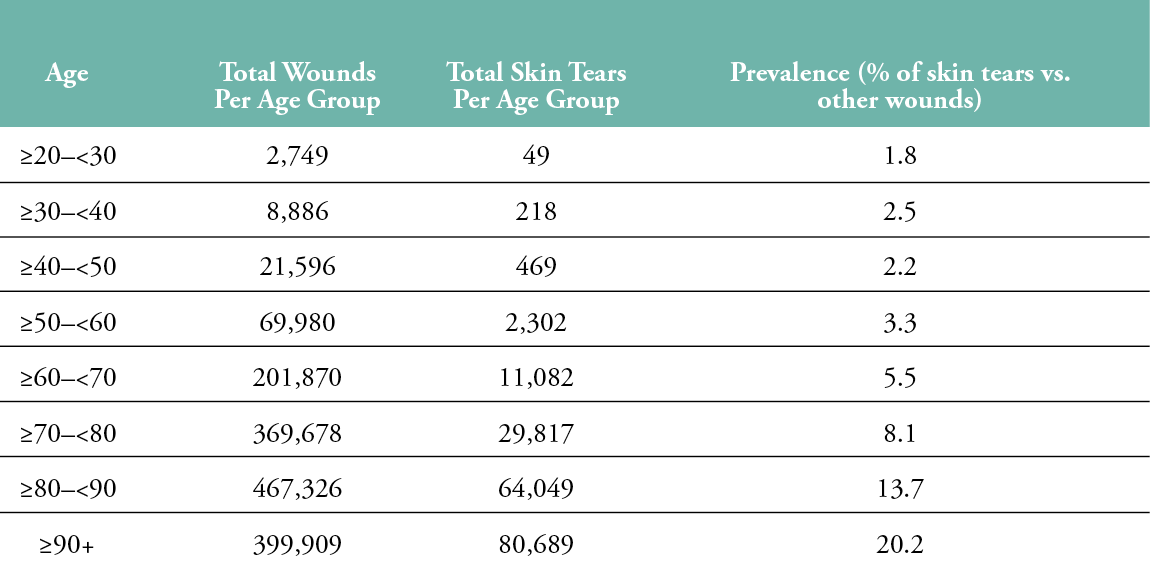
Reviewing the prevalence by age, we can observe a non-uniform distribution of skin tears. Table 4 shows that, as patients age, skin tears are more prevalent as their wound type. Wounds documented in patients aged 80–90 were 13.7%, which was higher than the overall population rates in Table 3. Patients 90 years and older had a 20% prevalence of skin tears, relative to other documented wounds.
Table 4: Skin Tear Prevalence by Age Group
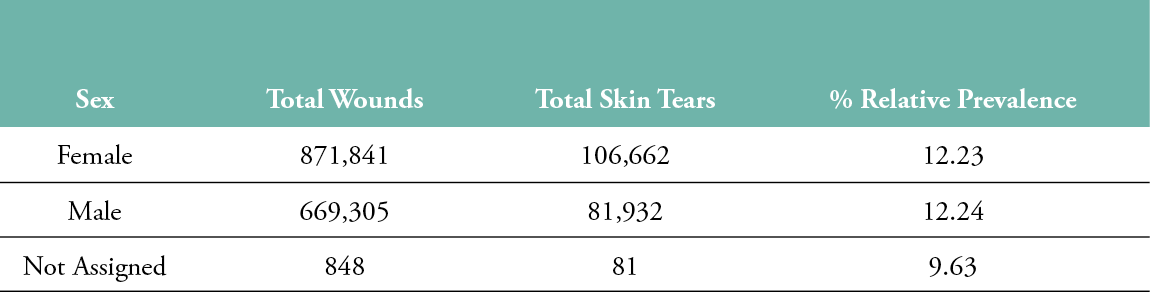
There was no statistical difference in the prevalence of skin tears by sex, as there was an equal prevalence; in females it was 12.23%, and in males it was 12.24% (Table 5). A total of 848 wound evaluations had no sex assigned. Wound evaluations for patients with no sex assigned in the chart had a lower skin tear prevalence (9.62%).
Table 5: Skin Tear Prevalence by Sex
Skin tear location showed high concentrations in certain locations, with 50% of wounds documented on six body locations. The most prevalent body parts for skin tears were the outer forearms (right 12.2%, left 11.7%), nearly double the rate, compared individually, to the next six most-frequent locations (Table 6 and Figure 1).
Table 6: Skin Tear Location Frequency
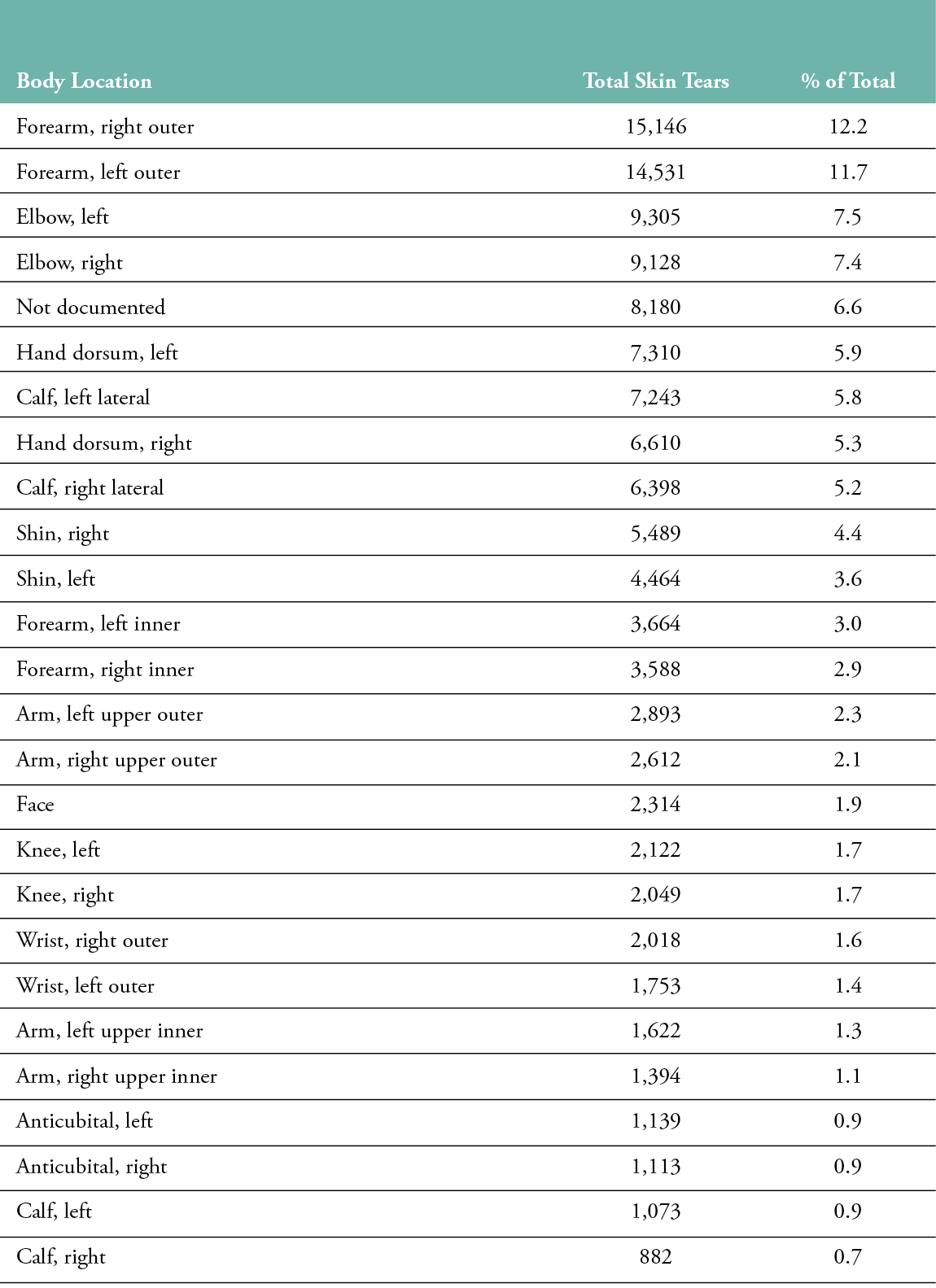
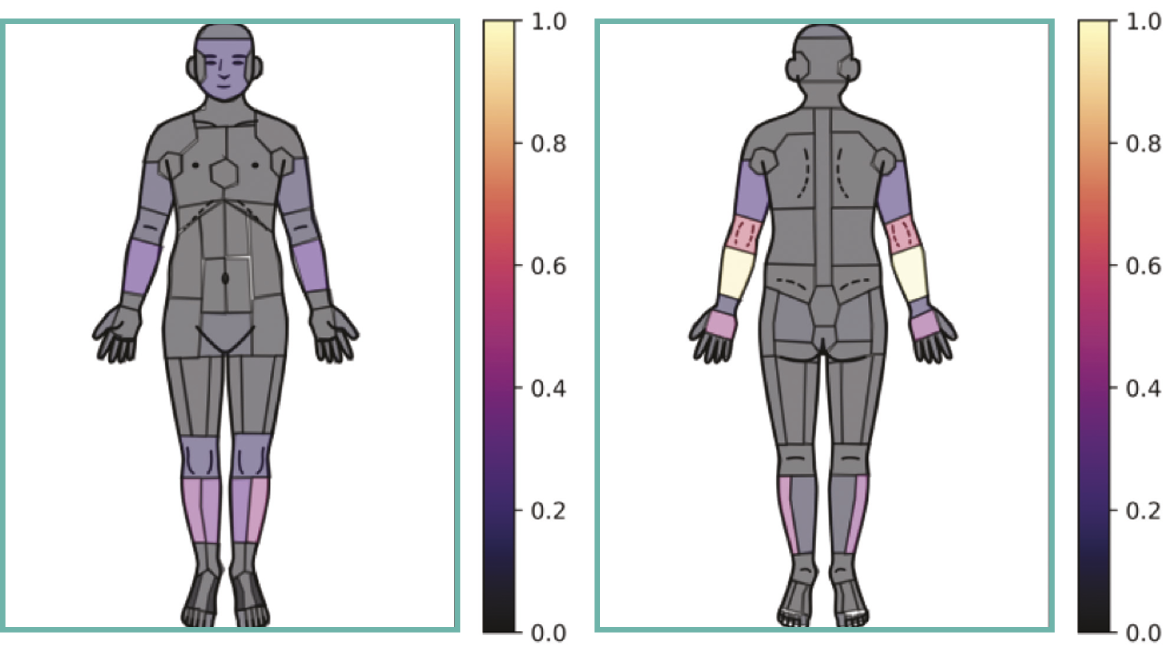
Figure 1: Body Location Heat Map of Skin Tear Frequency
Most skin tears (136,146 evaluations) were categorised on either the Payne-Martin or ISTAP skin tear classifications systems, and the remaining were documented as skin tears but without classification. Table 7 shows the total number of each type of classified skin tear.
Table 7: Classification of Skin Tears by Median Healing Time
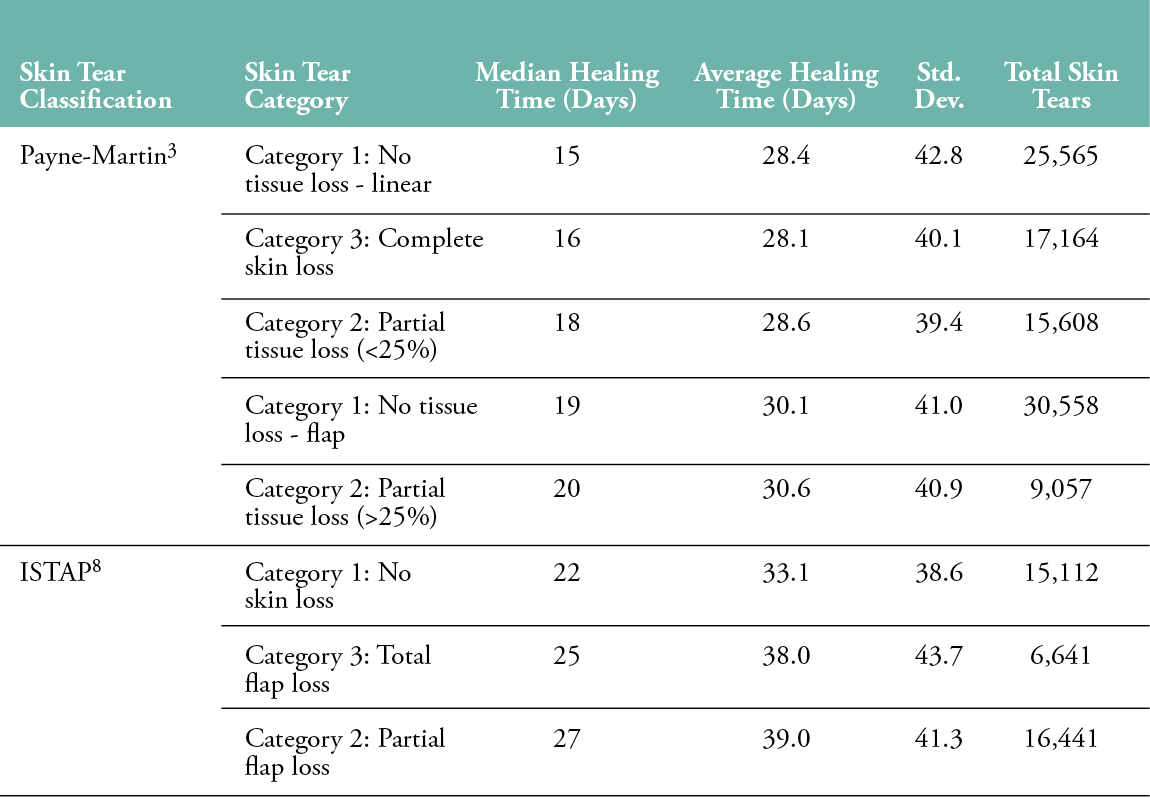
Average healing time was calculated, as was the median, as outliers may skew the average. Skin tears documented as ‘Category 1: No Tissue Loss – Linear’ had the lowest median healing time (15 days) in the Payne-Martin classification system. Skin tears documented with the ISTAP system as ‘Category 1: No Skin Loss’ had the lowest median days to heal (22 days). Interestingly, the second-lowest median days to heal in both systems was complete skin loss (ISTAP: Category 3, Payne-Martin: Category 3).
A review of treatments was conducted and organised according to weeks when the wound evaluations were captured according to primary dressing (Figure 2), secondary dressing (Figure 2) and cleansing solution. The treatment options allowed the selection of generic treatment options for the wound. In the first four weeks of treatment, the most frequent dressing type was noted as ‘other’. Selecting other suggests the applied treatment did not correspond with generic treatment options listed. Some organisations complete their treatment documentation in their primary electronic record or on paper. Information captured outside of the wound management solution was not included in the analysis.
After week 4, ‘no dressing’ application was the most frequently documented treatment. More than 50% of skin tears had no secondary dressing applied in the first four weeks, and that increased in the following weeks. Saline was the most frequently used cleansing solution across all periods.
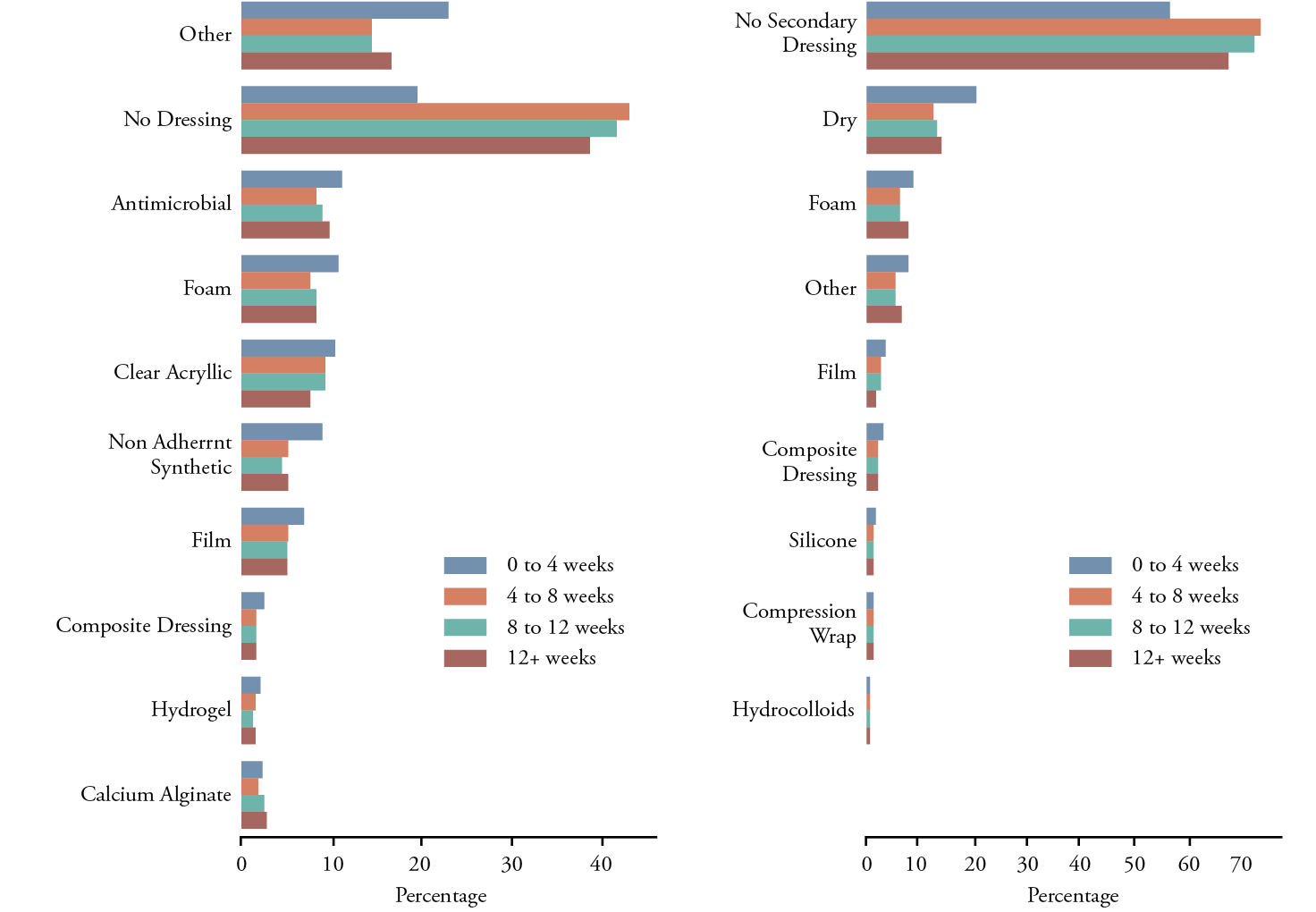
Figure 2: Primary and Secondary Dressing Selection
DISCUSSION
The primary objective of this study was to analyse the large data set generated by this wound management solution to understand the relative skin tear prevalence compared to other wounds, measure healing times and frequently used treatments in SNFs across the US and Canada. Previous studies have been limited by smaller sample sizes, with the largest recent study including 13,176 patients.13 Leveraging this big data set offers the ability to analyse more than ten times the sample of previous studies. Real-world data enables the review of current practice trends to gain further insights into wounds and specific types of injuries like skin tears. To our knowledge, this represents, by far, the largest analysis of skin tear data to date.
The historical data analysed in this study show a stable range of skin tears between 10.3% and 12.8% of all wounds in SNF documentation. Each year, the number of wounds measured continued to grow, as the wound management solution was implemented across more facilities and more patients were monitored. With the growth in the number of wounds documented each year, the prevalence of skin tears remained stable. This indicates that more than 1 out of 10 wounds in SNFs are skin tears; therefore, clinicians working in this setting require knowledge of proper prevention, evaluation, classification and treatment to reduce the incidence and improve healing outcomes.
Prevention should include assessing patients’ risk of skin tears. The recognised factors for skin tears include the need for assistance with activities of daily living (ADL), previous skin tears, blunt force trauma, falls and resisting care.16 Previous prevalence studies suggested the development of standardised tools to assess risk.8 The Braden Scale has been widely adopted for pressure injuries in SNF settings. The use of a standardised risk assessment and interventions matched to risk may help reduce the prevalence of skin tears. Based on current best practice recommendations, prevention should include a consideration of general health (e.g., education, optimising nutrition/hydration), mobility interventions (e.g., safe transitions/repositioning, fall prevention, removing clutter, lighting) and skin safety (e.g., trimming fingernails, moisturising skin, wearing skin-protective clothing).23
Skin tears need to be classified correctly using reliable tools and managed properly.11 Otherwise, these wounds will contribute to clinical and economic burdens on long-term care facilities and the healthcare system.9 Our dataset focused on organisations that used a skin tear classification system. More than 52,000 evaluations – nearly one-third of the total – were labelled as skin tears only, with no subsequent classification by the clinician. This may be due to a lack of understanding of the skin tear classification tools.8 Early identification and treatment are important, as skin tears in older patients with disabilities or chronic diseases can quickly evolve into complex wounds that are harder to heal, prone to infection and require hospitalisation.9
Skin tears are considered acute wounds and, if uncomplicated, may resolve in 14–21 days.16 However, patient-related and external factors may lead to delayed healing and the development of a chronic wound. Wounds in the study that were classified with the Payne-Martin scale ranged between 16 and 20 days for median healing, while skin tears classified on the ISTAP system ranged between 22 and 25 days to heal. This may be due to differences in practices associated with the skin tears in facilities using the skin tear systems. Future analyses should focus on identifying differences in populations, skin tear size, treatments or other factors that may impact healing time.
Analysing skin tear treatment over time allowed insight into changes in wound management. Skin tears older than four weeks more frequently had no dressing applied, and ‘other’ was the most frequently selected or second-most frequent selection. Our data identified the use of dressing types that might not be typically associated with skin tears, including the use of antifungal and pain-controlling dressings. However, this may be related to a variety of factors; for example, a tear may develop in an area of the leg where a compression wrap is being applied, or a clinician may be noting all the preventative measures in place to address pressure injuries (e.g., offloading devices). The majority of skin tears did not have a secondary dressing.
In this analysis, saline was the most common wound cleansing solution used. This finding is in line with ISTAP Best Practice statements recommending that skin tears and the surrounding skin be cleansed.11 No cleaning solution was used for 12.7% of skin tears and peaked at 29% across later weeks. This may be an opportunity for future analysis of how this impacts healing times and adverse events such as infection.
In this study, skin tear prevalence increased with age and nearly doubled for those over 90 years of age. Our findings concur with Van Tiggelen and colleagues’ study, which found age was significantly associated with skin tears in nursing home residents.18 Intrinsic factors, such as changes in the epidermis and dermis (e.g., epidermal thinning, lower epidermal stem cells, the longer turnover time of the epidermis)24,25 or age-related comorbidities may contribute to these higher rates. Extrinsic factors (e.g., hydration status, bathing frequency, medical adhesive product use) may be another element. The high prevalence in ageing populations highlights where efforts for screening and prevention should be directed, and where a review of treatments to minimise the risk of skin tears may prove beneficial.
The location of skin tears aligns with findings from smaller-scale studies, which showed that these injuries frequently occur on the outer aspect of the limbs.3,17,18,21 Requiring assistance with ADLs, falling and resisting care are known risk factors for skin tears16, which highlights the impact of mobility and immobility. Turning and repositioning, getting skin caught on assistive devices (e.g., walkers) or doorknobs may also contribute to skin tears in these areas. Arms can be commonplace for the securement of medical adhesive, which is also a known risk factor for skin tears.16 An interesting observation was the similarity between the right and left sides of the body. Given the preference for mobilising and the use of certain sides of the body, it might be expected that there would a difference, yet we see tears on the forearm, elbow, hand, calf and shin all occurring at similar frequencies (Table 6).
An additional consideration is that sun exposure-related skin damage may lead to irreversible changes, predisposing individuals to an injury. Ultraviolet light thins the skin, which may make it more vulnerable to mild trauma and skin tears.16 Our data showed that the lower and upper extremities had the highest rate of skin tears, and the face has an elevated risk, which may align with this concept. However, the back of the neck and ears are also exposed to the sun, yet did not have the same elevation in rates of skin tears. Therefore, sun damage may make skin more susceptible to skin tears, but other contributing factors (e.g., trauma, friction, shear, adhesive placement) may be why they are more prevalent in particular sun-exposed areas. Overall, the data suggest that, in our population, skin tears are a combination of different factors related to risk and causative mechanisms.
Future analyses may enable a better understanding of significant differences in healing data. Statistical analyses of specific treatment types may help shed light on promising practice patterns. Big data may also be used to support quality improvement and feedback regarding practices that may impair healing.
Evaluation of the study
Real-world data sets provide large amounts of information, yet have other limitations. Due to the different education and training backgrounds of clinicians (20,835 clinicians documented wounds in this dataset), documentation skills may vary. This may be why some wounds were not classified. Documentation is undertaken in real-world settings and may not always be complete, as was evident by null answers. These answers needed to be excluded, as it was not clear if the local organisation documents by exception and none was inferred, or if it was missed documentation.
Our dataset comes from NA and may not be broadly generalisable. Previous prevalence studies have shown variations (3.9–20.8%) among international studies on skin tears.3,4,16,18,26 The expansion of standardised tools like wound management solutions into international practice settings would help in comparing differences at the national level.
For this analysis, the first date of the wound was noted as the first evaluation date. This may slightly influence the days, depending on when the wound was first captured. Treatment forms also use generic treatment terms to enable wide use across different formularies. This may be the reason ‘other’ was selected frequently as an option; clinicians may not recognise the generic name for the wound product they are using. Further research would benefit from exploring specific treatment products used, as a better analysis of outcomes related to specific product usage could be conducted.
Although this is the largest set of skin tears published to date, only data documented within the wound management solution app could be aggregated and monitored. This means other information in the electronic medical records, such as medications, could not be analysed. In the future, being able to include other health-related data may shed new light on risks for skin tears.
The ability to study big data to understand current practices is a strength of this paper. As far as we know, our study is the first large-scale analysis of a real-world data set to study skin tear prevalence. Documentation is standardised, allowing for easier multi-centre analysis. The data set provides a five-year review of real-world wound care documentation in SNFs. The data set includes thousands of facilities from across NA. Rather than conducting a smaller study and extrapolating the results, leveraging big data provides insight into direct practice patterns.
CONCLUSION
Skin tears are a common challenge in SNFs. The implementation of an AI-powered wound management solution provided standardised documentation and the collection of real-world data to generate insights into skin tear prevalence, body location and treatment frequency. Historically, skin tear prevalence studies have included only hundreds or thousands of patients, and big data offers the opportunity to learn from significantly larger data sets.
Advanced digital assessment tool adoption in clinical practice offers the opportunity to better understand current practice trends. Future analysis of this type of real-world data set could help analyse differences across geographic regions, care settings, treatment practices and patient populations. Initial analysis of this dataset gives insight into ways we can leverage the documentation clinicians complete in their daily care as tools for improving patient care and outcomes. Further research should focus on unclassified skin tears to see if there are differences in treatments and outcomes.
IMPLICATIONS FOR CLINICAL PRACTICE
- Real-world data provide insights into current trends for skin tears.
- Skin tears represent 10.3–12.8% of wounds in skilled nursing facilities in North America and increase in prevalence with age.
- Clinicians in this setting need to understand prevention, classification and treatment for skin tears.
Further research
- The development of standardised risk assessments and interventions to prevent skin tears could help reduce their prevalence in skilled nursing facilities.
- The use of real-world data can help to understand the most effective treatments and reduce healing times.
- Aim to determine if using skin tear classification tools is associated with better healing outcomes.
Key messages
- A comprehensive understanding of skin tears’ prevalence in skilled nursing facilities is necessary to inform comprehensive prevention, assessment and treatment strategies.
- Real-world data offer the potential to leverage clinical documentation to understand current practice challenges and opportunities better.
- Access to a subset of big data enabled the analysis of 1,541,944 wounds, including 188,675 skin tears, from 75,655 patients within five years to identify relative prevalence.
- Skin tears represent more than one in ten wounds in skilled nursing facilities, which highlights the need for knowledge of prevention and management strategies when working with this population.
Author(s)
Robert D. J. Fraser,1,2 MN, RN, Rishabh Gupta,1 Ph.D., Amy Cassata,1 BSN, RN, WCC
Heba Tallah Mohammed,1 Ph.D., Justin Allport,1 BASc, Sheila C. Wang,1 Ph.D., MD, Jose L. Ramirez-GarciaLuna,1,3 Ph.D., MD
1 Swift Medical Inc., Toronto, ON, Canada. 2 Arthur Labatt Family School of Nursing, Western University, London, ON, Canada
3 Division of Experimental Surgery, McGill University Health Centre, Montreal, QC, Canada
Correspondence: rob.fraser@swiftmedical.com
Conflict of interest: SW and JA are co-founders of Swift Medical Inc. RDJF, RG, AC, HTM and JLRG are employees of Swift.
References
- Miles SJ, Fulbrook P, Williams DM. Skin tear prevalence in an Australian acute care hospital: A 10-year analysis. Int Wound J [Internet]. [cited 2022 Jan 7];n/a(n/a). https://doi.org/10.1111/iwj.13735
- LeBlanc K, Christensen D, Cook J, Culhane B, Gutierrez O. Prevalence of skin tears in a long-term care facility. J Wound Ostomy Continence Nurs 2013 Nov; 40(6):580–4.
- Skiveren J, Wahlers B, Bermark S. Prevalence of skin tears in the extremities among elderly residents at a nursing home in Denmark. J Wound Care 2017 Feb; 26(Sup2):S32–6.
- Bermark S, Wahlers B, Gerber AL, Philipsen PA, Skiveren J. Prevalence of skin tears in the extremities in inpatients at a hospital in Denmark: To determine the prevalence of skin tear and explore factors. Int Wound J 2018 Apr; 15(2):212–7.
- LeBlanc K, Baranoski S. Skin tears: Best practices for care and prevention. Nursing (Lond) 2014 May; 44(5):36–46.
- Koyano Y, Nakagami G, Iizaka S, Minematsu T, Noguchi H, Tamai N, et al. Exploring the prevalence of skin tears and skin properties related to skin tears in elderly patients at a long-term medical facility in Japan: Skin tears prevalence and risk factors. Int Wound J 2016 Apr; 13(2):189–97.
- Lewin GF, Newall N, Alan JJ, Carville KJ, Santamaria NM, Roberts PA. Identification of risk factors associated with the development of skin tears in hospitalised older persons: A case–control study. Int Wound J 2015 Sep 24; 13(6):1246–51.
- Van Tiggelen H, LeBlanc K, Campbell K, Woo K, Baranoski S, Chang YY, et al. Standardizing the classification of skin tears: Validity and reliability testing of the International Skin Tear Advisory Panel Classification System in 44 countries. Br J Dermatol 2020 Jul; 183(1):146–54.
- Strazzieri-Pulido KC, Peres GRP, Campanili TCGF, Santos VLC de G. Skin tear prevalence and associated factors: A systematic review. Rev Esc Enferm USP 2015 Aug; 49(4):674–80.
- LeBlanc K, Baranoski S, Holloway S, Langemo D, Regan M. A descriptive cross-sectional international study to explore current practices in the assessment, prevention and treatment of skin tears. Int Wound J 2014; 11(4):424–30.
- LeBlanc K, Campbell K, Beeckman D. Best practice recommendations for the prevention and management of skin tears in aged. Wounds Int 2018. Available at: https://www.woundsinternational.com/resources/details/best-practice-recommendations-prevention-and-management-periwound-skin-complications
- Chang YY, Carville K, Tay AC. The prevalence of skin tears in the acute care setting in Singapore: Skin tears prevalence. Int Wound J 2016 Oct; 13(5):977–83.
- Feng H, Wu Y, Su C, Li G, Xu C, Ju C. Skin injury prevalence and incidence in China: A multicentre investigation. J Wound Care 2018 Oct 1; 27(Sup10):S4–9.
- Hahnel E, Blume-Peytavi U, Trojahn C, Kottner J. Associations between skin barrier characteristics, skin conditions and health of aged nursing home residents: A multi-center prevalence and correlational study. BMC Geriatr 2017 Dec; 17(1):263-275.
- Hawk J, Shannon M. Prevalence of skin tears in elderly patients: A retrospective chart review of incidence reports in 6 long-term care facilities. Ostomy Wound Manage 2018 Apr 1; 64(4):30–6.
- LeBlanc K, Woo KY, VanDenKerkhof E, Woodbury MG. Skin tear prevalence and incidence in the long-term care population: A prospective study. J Wound Care 2020 Jul 1; 29(Sup7):S16–22.
- Souza LM de, Teixeira G da S, Silva DM da, Ruiz L da S, Coppola I dos S, Meirelles LC da S. Prevalence of skin tears in hospitalized adults and older adults. Rev Esc Enferm USP 2021; 55:e03683.
- Van Tiggelen H, Van Damme N, Theys S, Vanheyste E, Verhaeghe S, LeBlanc K, et al. The prevalence and associated factors of skin tears in Belgian nursing homes: A cross-sectional observational study. J Tissue Viability 2019 May; 28(2):100–6.
- Woo K, LeBlanc K. Prevalence of skin tears among frail older adults living in Canadian long-term care facilities. Int J Palliat Nurs 201824(6). https://doi.org/10.12968/ijpn.2018.24.6.288
- Fife CE, Eckert KA. Harnessing electronic healthcare data for wound care research: Standards for reporting observational registry data obtained directly from electronic health records: Standards for reporting observational data from electronic health records. Wound Repair Regen 2017 Apr; 25(2):192–209.
- Au Y, Laforet M, Talbot K, Wang SC. Skin and wound map from 23,453 nursing home resident records: Relative prevalence study. JMIR Dermatol 2018 Oct 9; 1(2):e11875.
- Health Information Privacy. Guidance regarding methods for de-identification of protected health information in accordance with the Health Insurance Portability and Accountability Act (HIPAA) privacy rule [Internet]. HHS.gov; 2012 [cited 2022 Jan 22]. Available at: https://www.hhs.gov/hipaa/for-professionals/privacy/special-topics/de-identification/index.html
- LeBlanc K, Baranoski S, Christensen D, Langemo D, Sammon MA, Edwards K, et al. International Skin Tear Advisory Panel: A tool kit to aid in the prevention, assessment, and treatment of skin tears using a simplified classification system. Adv Skin Wound Care 2013 Oct; 26(10):459–76.
- LeBlanc K, Baranoski S. Skin tears: State of the science: Consensus statements for the prevention, prediction, assessment, and treatment of skin tears. Adv Skin Wound Care 2011; 24(9):2–15. DOI: 10.1097/01.ASW.0000405316.99011.95
- Wysocki A. Anatomy and physiology of skin and soft tissue. In: Bryant RA, Nix D, editors. Acute & chronic wounds: Current management concepts. 5th ed. St Louis: Mosby; 2015, p. 40–62.
- Assis TG, Palhares DM, Alkmim MB, Marcolino MS. Teledermatology for primary care in remote areas in Brazil. J Telemed Telecare 2013 Dec; 19(8):494–5.
