Volume 23 Number 2
Prevention and management of skin tears: A survey of nurses in French-speaking Switzerland
Lucie Charbonneau, Sebastian Probst, Georgina Gethin
Keywords Prevention and management, quantitative description, skin tear, survey method, wound care specialists
DOI 10.35279/jowm2022.23.02.05
Abstract
Background Skin tears are common in many care settings. Clinicians’ practices show a lack of knowledge on skin tear classification, prevention and treatment; documentation problems; and a lack of uniform language.
Aim The aim of this study is to investigate nurses’ perceptions, opinions, knowledge and practices on the prevention and management of skin tears in French-speaking Switzerland.
Method A survey was conducted among nurses and wound care specialists in Western Switzerland. Data were collected between 17 November and 14 December 2020 and analysed using descriptive statistical and thematic analyses.
Result A total of 117 nurses and wound care specialists participated in this survey; 89% described skin tears as common. Skin tear definitions (18%, n=15), classification systems (7%, n=6) and risk factors were not well known. Prevention measures were often non-existent (87%, n=82). A standard of care was infrequent (5%, n=6). Pain (76%, n=70), delayed healing (75%, n=70) and frequent dressing changes (72%, n=67) were common issues and complications. Education on dressing choices (89%, n=80); prevention measures (88%, n=79); and aged skin issues (86%, n=77), were identified as important teaching topics.
Conclusion The results contribute to our understanding of wound care specialists’ clinical judgment on preventing and managing skin tears in French-speaking Switzerland and highlight the importance of wound care education.
Implication for clinical practice To enhance nurses’ knowledge of wound care and ensure evidence-based practices, we recommend implementing standard, unified wound curricula for nurses at the undergraduate and post-graduate levels, based on the existing European curricula.
INTRODUCTION
Skin tears are defined as ‘a traumatic wound caused by mechanical forces, including removal of adhesives. Severity may vary by depth (not extending through the subcutaneous layer)’.1 Skin tears occur across all healthcare settings and are related to mechanical trauma such as wheelchairs, adhesive tapes’ removal, transfers or falls.1–5 Their prevalence ranges from 3% to 41% in long-term care settings5–14, 1.1% to 11.4% in acute care15–20, 3.3% to 27% in palliative care19,21,22 and 0.10% to 17% in paediatrics.23,24 Evidence shows that these wounds are often unreported, misdiagnosed and that their clinical and financial impact on the healthcare system is not clearly described.25,26 In addition, the impact of skin tears on the individual is poorly described, but they appear to cause pain and impair quality of life.25,26
Current guidelines recommend an interdisciplinary team approach to implementing a systematic skin tear prevention programme.1 Good skin tear management includes interventions involving both the patient and the caregivers1,27, such as ensuring safe patient handling techniques/equipment or a secure environment; wearing long sleeves, long pants/trousers or knee-high socks; and keeping fingernails and toenails short.3,27 The knowledge base used in skin tear care requires an understanding of the physiology of the skin, which helps in the management of people with skin tears. When a skin tear occurs, effective care should be based on preserving the skin flap and the surrounding tissue and the re-approximation of the wound’s edges, reducing the risk of infection and further injuries while considering any comorbidities.1
Studies have demonstrated a gap between evidence and clinical practices regarding skin tear prevention and management13,28, due to a lack of information and expertise, inadequate communication and limited access to evidence on assessment.13 White28 investigated the knowledge, opinions and clinical practices about skin tears of nurses working in nursing home/residential aged care facilities using a survey method. The results showed that fewer than 50% of the nurses documented the shape of the skin tear, amount of skin lost, depth of the wound or condition of the surrounding skin, and only 24% indicated that their facility had a ‘standard’ for the treatment and management of skin tears.28 Another survey evaluating skin tear knowledge of acute care nurses working in two hospitals showed improved knowledge in skin tear identification and assessment, classification and treatment (97.1%, versus 99.1%).29 A larger study investigated current practices in assessing, predicting, preventing and treating skin tears among health care providers from 16 countries and revealed problems with the current methods for skin tear assessment and documentation (69.6%). Fully 80.9% mentioned that tools or classification systems are not used.30 A survey on acute care nurses’ knowledge of skin tear assessment, prevention and treatment found a lack of knowledge and awareness of risk factors, prevention strategies and skin tear treatment based on the literature.31 A recent study from Germany confirmed nurses’ lack of knowledge on the international classification system, prevention and treatment.32
With the above in mind, we aimed to investigate nurses’ perceptions, opinions, knowledge and clinical practices related to the prevention and management of skin tears in French-speaking Switzerland.
METHODOLOGY
A quantitative, non-experimental descriptive research approach with a survey was employed. A survey questionnaire developed by White28 was identified and translated into French.33 It was distributed among wound care nurses who hold a Certificate or a Diploma of Advanced Studies degree (CAS/DAS HES-SO) in wound care recruited via the University of Applied Sciences and Arts Western Switzerland and the Swiss Association for Wound Care (SAfW-Romande) between 17 November and 14 December 2020. The survey was sent via an email that also explained the purpose of the study. Prospective participants were invited to answer the online survey through the link provided in the email. Since the survey was anonymous, there was no follow-up on the respondents and non-respondents. Two weeks later, a reminder was sent to all participants. The survey was closed after four weeks.
The questionnaire was divided into four sections, with the first focussed on general information about the nurses’ education and the institution within which they worked. The second section assessed their perceptions of skin tears; the third inquired about knowledge of skin tears’ definition and classification; the fourth section addressed clinical issues and difficulties relating to the prevention, management and treatment of skin tears. We analysed the data using descriptive statistical analysis. All open-ended questions were analysed using thematic analysis with a deductive approach, according to Braun and Clarke’s recommendations.34 First, the lead author familiarised herself with the data, generated initial codes and identified themes from the skin tear definition1 and risk factors for skin tear development identified in the literature.1,35,36 Second, LC highlighted words from the respondents’ answers, and the codes and themes were compared and grouped for the final analysis. Third, the thematic analysis was reviewed by SP and GG.
Quality criteria for studies on developing and evaluating health status questionnaires exist.37 White’s original survey28 and the updated survey used in this study provided a clear description of the aspects of the development of the questionnaire to grade the content validity. The measurement aims of the survey used were evaluative, and the items were valid for assessing nurses’ knowledge and clinical practices related to skin tears. The survey was adapted to the target population, as the updated version was clearly addressed to nurses and wound care specialists. Item selection and reduction choices were made through the pilot test as part of the translation process.33 Criterion validity refers to the degree to which scores on a particular instrument relate to a gold standard.37 The survey development and update were based on evidence-based guidelines; therefore, it had a positive rating because it was related to a gold standard.
The study was approved by the Ethics Committee in the Canton of Geneva, Reference number: Req-2020-01021.
RESULTS
A response rate of 45% (117/258) was achieved. Participants were almost exclusively from the French-speaking part of Switzerland (97%, n=113), with the remainder from the Italian part. Half (50%, n=59) worked in a hospital environment – either a university hospital, a general hospital or a clinic. Only 34% (n=40) worked in a home care setting or private practice. Complete information on respondents’ working specialities is summarised in Figure 1.
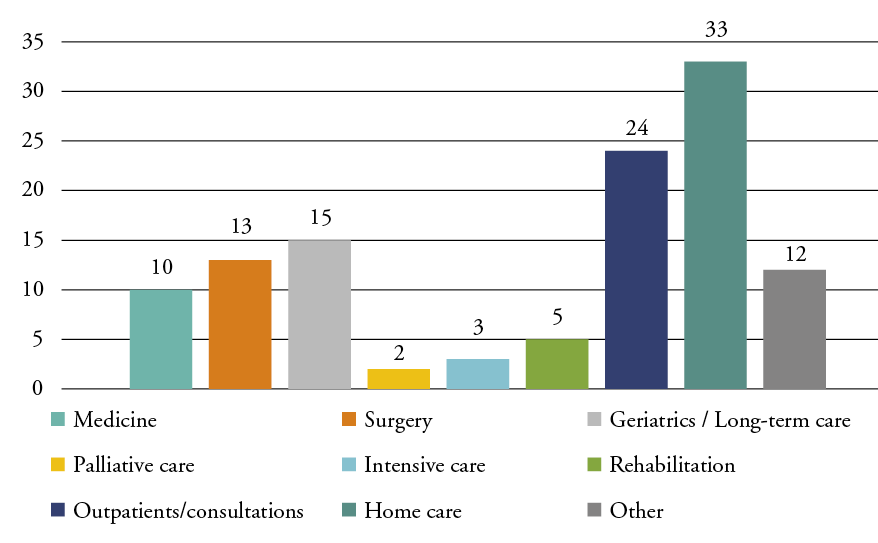
Figure 1: Nurses’working specialities
Nurses’ educational backgrounds
Of the respondents, 56% (n=66) had a Diploma of Nursing, 20% (n=23) a Bachelor of Nursing and 3% (n=4) a Master of Science degree. Fifteen per cent (n=17) had been nurses for 3 to 10 years, 60% (n=70) for 11 to 30 years and 23% (n=27) for 31 to 40 years (median = 21–30 years). The majority (83%, n=97) had completed a Certificate of Advanced Studies in wound care. Sixty-eight per cent (n=79) had up to 10 years of experience as wound care specialists (median = 3–10 years).
Nurses’ perceptions of skin tears
Of the respondents, 89% (n=102) indicated skin tears were ‘common’ to ‘extremely common’. Sixty-five per cent (n=75) indicated being aware of 1–2 skin tears per week, and 7% (n=8) reported knowledge of 3–5 new skin tears per week.
Nurses’ knowledge of skin tears
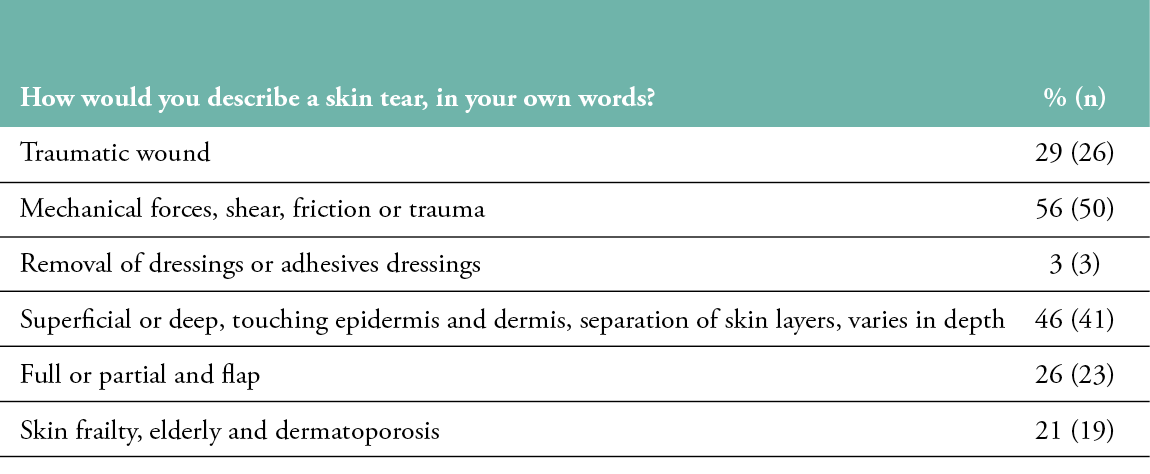
Of the respondents, 78% (n=90) described a skin tear in their own words. Words from these definitions and similarities were highlighted and grouped for analysis (Table 1). All participants used the words ‘wound’ or ‘injury’ to describe a skin tear, but only a few described a skin tear as a ‘traumatic wound’. More than half (56%, n=50) specified that ‘mechanical forces, shear, friction or trauma’ cause skin tears. The ‘removal of dressings or adhesive dressings’ were elements that only a very few nurses included in the definition. Participants used phrases such as ‘superficial or deep’, ‘touching epidermis and dermis’, ‘separation of skin layers’ and ‘varied in depth’ to relate to the notion that the tears’ severity may vary by depth, as in the International Skin Tear Advisory Panel (ISTAP) definition. Although not in the definition, words such as ‘full or partial’ and ‘flap’, or the concept of ‘skin frailty, elderly and dermatoporosis’, were used in the descriptions of skin tears. Ninety-one per cent (n=85) indicated not using a classification system in their care setting, and only 7% (n=6) used the ISTAP classification system.
Table 1: Words or concepts to describe a skin tear
Risk factors and prevention
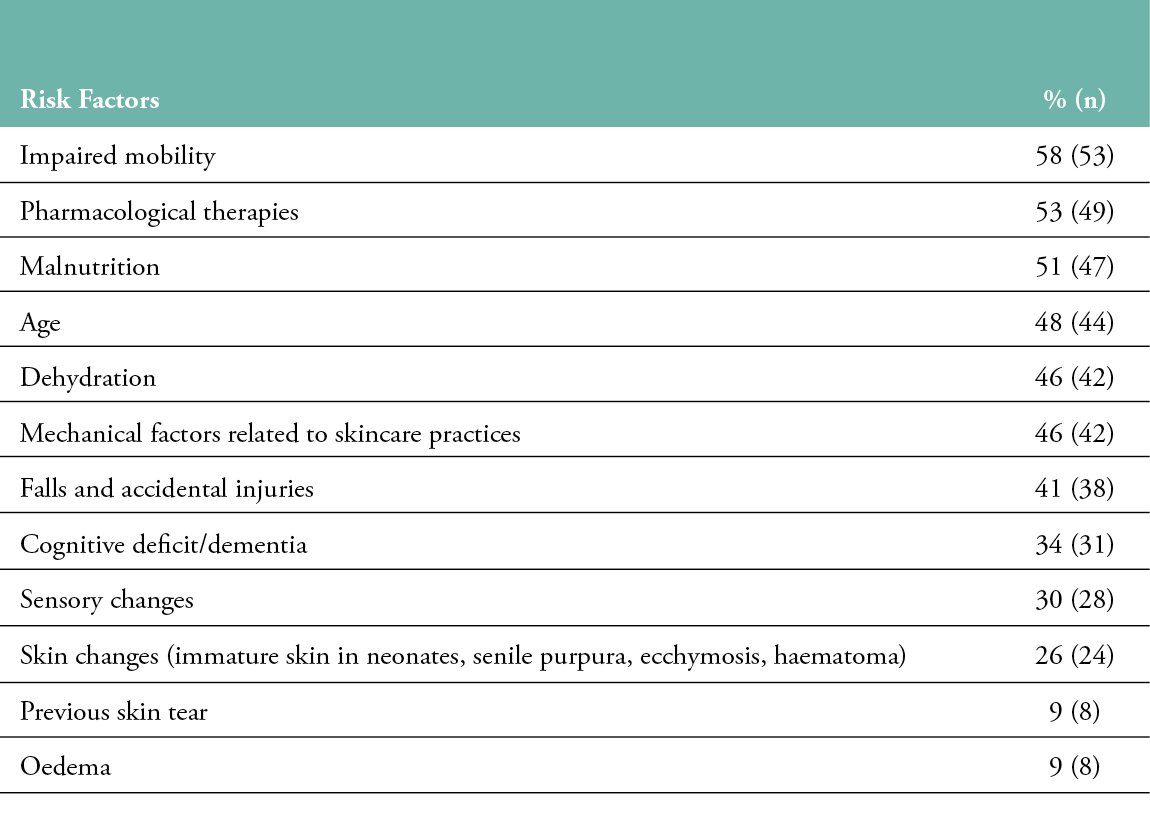
Out of 80% (n=93) of respondents, 68% (n=63) declared having no workplace policy for identifying a person at risk of skin tears. Risk factors for skin tear development identified in the literature1,35,36 were noted by participants and grouped for the analysis (see Table 2). Eleven per cent (n=10) identified alcohol use, smoking and sun exposure as risk factors, and 2% (n=2) listed domestic pets as risk factors for skin tears. Eighty-seven per cent (n=82) of nurses indicated no existing preventive procedure in their organisation. Soap and water (90%, n=83), emollients (8 %, n=7) or other products (e.g., cleansing oils) (2%, n=2) were used to wash or bathe patients, and 93% (n=85) ‘mostly’ to ‘always’ used skin moisturisers on all patients daily.
Table 2: Risk factors for skin tears identified in the literature
Documentation of skin tears
More than 60% of nurses indicated ‘always’ recording the details of the skin tear injury in their nursing notes, care plans and wound charts, whereas 68% (n=75) ‘never’ recorded details in incident forms or risk management software. More than half indicated ‘always’ recording the type, cause and size of a skin tear, the site on the body, exudate and the condition of the surrounding skin.
Treatment
Only 5% (n=6) of 96% of respondents (n=112) declared having a ‘standard of care’ treatment for all skin tears in their care settings. As shown in Table 3, a wide range of products was identified to treat a skin tear, such as non-adherent mesh dressings, foams, calcium alginates or skin closure strips for skin tears’ treatment in their clinical practice.
Table 3: Products used in skin tear treatment
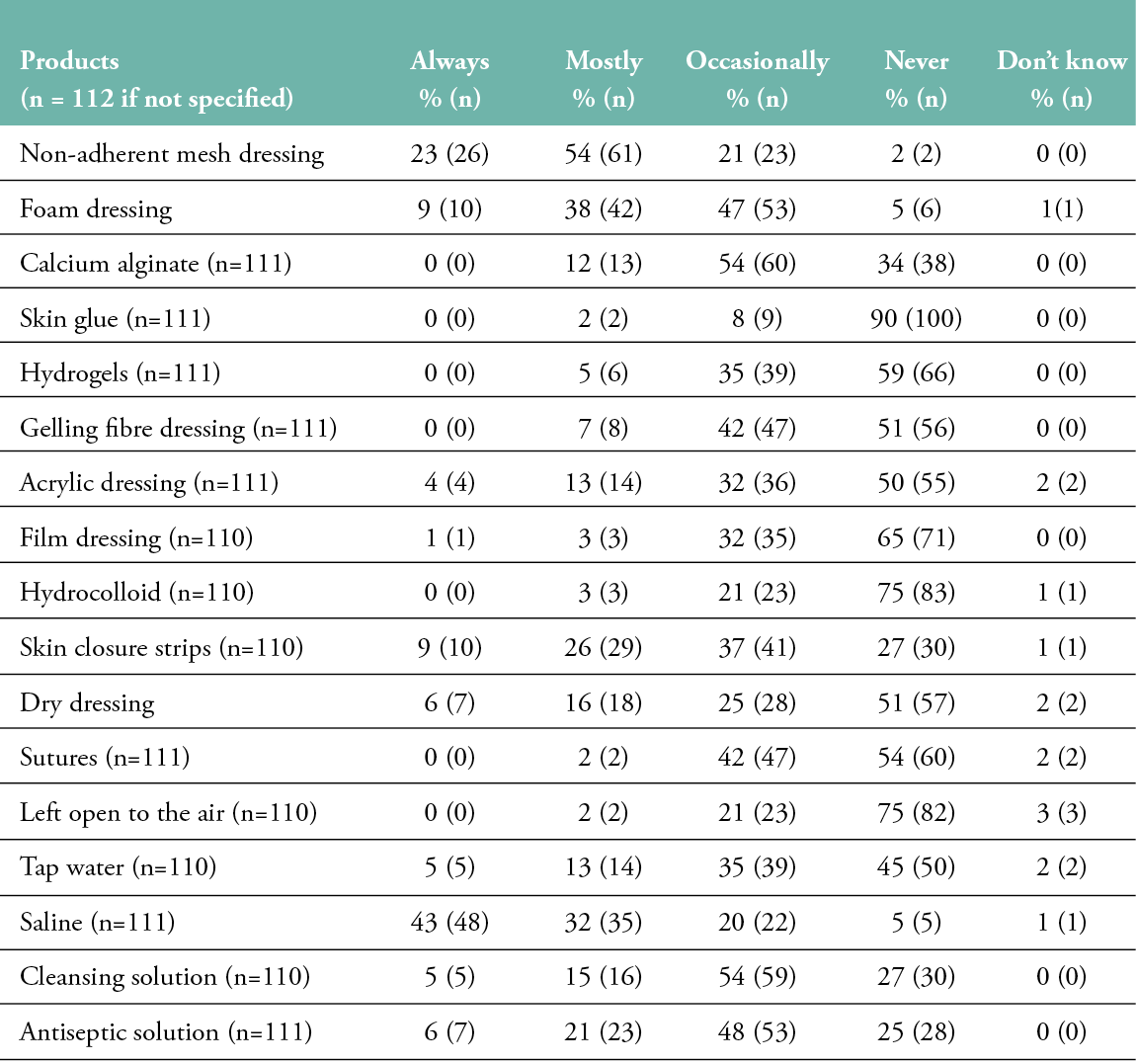
When choosing a dressing for a skin tear, the most important consideration was that it should not cause any trauma on removal. In addition, more than 70% considered ‘very important’ the fact that a dressing provides a physiological healing environment and is easy to apply and remove.
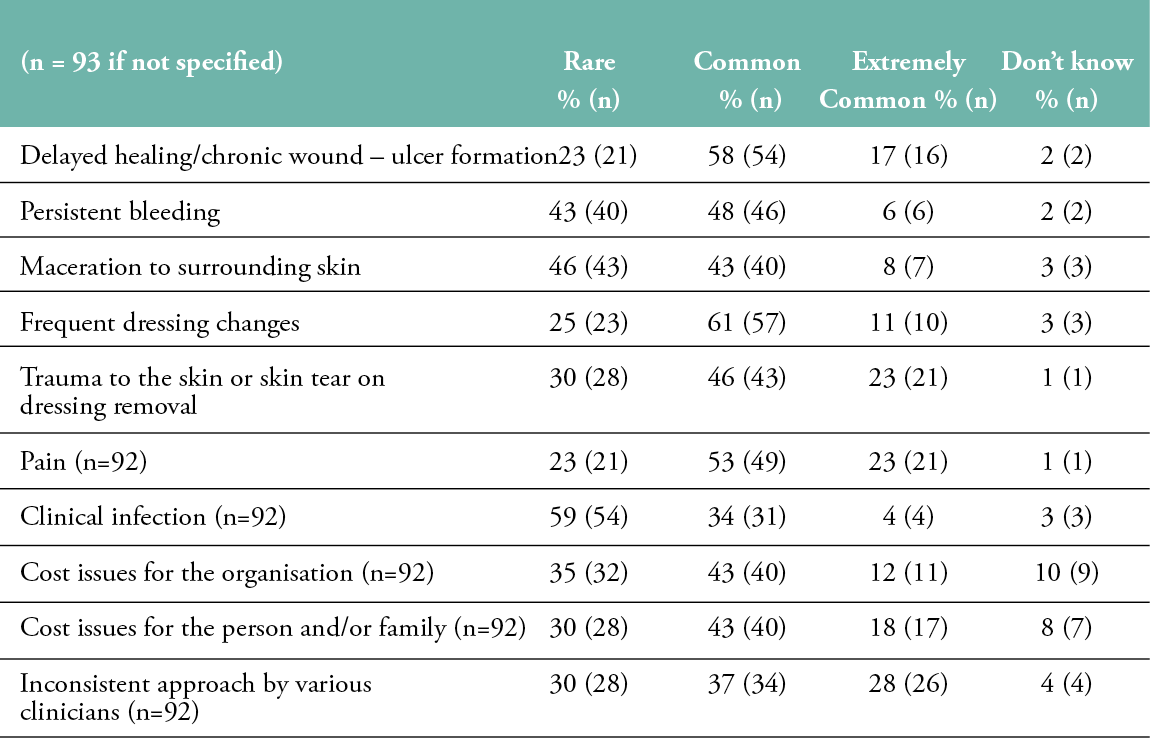
Pain, delayed healing/chronic wound–ulcer formation and frequent dressing changes were ‘common’ to ‘extremely common’ issues and complications for the respondents when managing skin tears. However, clinical infection was a rare issue/complication in skin tears (Table 4).
Table 4: Issues and complications in skin tear management
Nurses’ education
For future educational programmes for Registered Nurses, the first three topics related to skin tears requested by the nurses were: dressing choices (89%, n=80); prevention measures (88%, n=79); and extremes of aged skin issues, such as dry/fragile skin (86%, n=77). Only 66% (n=59) of the nurses identified patient and caregivers’ education and awareness as a topic for nurses’ educational programmes.
DISCUSSION
The overall response rate was 45%; however, evidence demonstrates that surveys involving healthcare professionals are known to have relatively low response rates, with an estimated overall survey response rate among this group at 53%, with varying rates of response of 57% for mail surveys and 38% for web-based surveys.38 If the topic is highly salient to potential respondents, they are more likely to respond to the survey39, and one or two follow-ups have been proven effective for increasing response rates.38 An introductory text to the survey explaining the purpose of the research, the researcher’s identity and affiliation and the implications of participation should be the first step of any online survey.40 In this study, the overall response rate was slightly low, even though the survey began with a welcome message and one follow-up email was sent to all prospective participants two weeks after the survey was launched. Drop-out rates can reach 15–20% in some Internet surveys and could be related to the use of open-ended questions or questions arranged in tables41, as was the case in this survey research. Scheele et al.32 noted many drop-outs in their study and suggested that this could be related to participants’ insufficient knowledge of skin tears.
This study revealed that education on skin tears and their management should be a part of future education programmes for Registered Nurses. Several implementation project studies have described the importance of staff education for reducing the prevalence and incidence of skin tears.13,36,42 For example, an implementation project for patients in acute aged care and rehabilitation units with pre- and post-implementation audits showed a significant change in staff compliance to the skin tear guidelines, with a considerable increase in staff education regarding their prevention (from 20% to 98%) and a decrease of the point prevalence rate from 10% to 0.15%.42 Another study from Australia demonstrated that ongoing training and education positively impacted the management of skin tears and improved awareness of skin integrity as a crucial element of skin tear prevention among people at risk.43 Edwards and colleagues13 supported the implementation of the Champions for Skin Integrity model to reduce wound prevalence, specifically skin tears (23% vs 19%), and increased evidence-based wound assessment, prevention and treatment. Providing education to all multidisciplinary team members, patients and their carers is essential for raising awareness of the problem.1,44–46
Research has shown that education is needed to improve the prevention, assessment, treatment and management of wound types, including skin tears.47 In addition, the rapid evolution in treatment strategies and the increasing complexity of care are creating a need for greater knowledge among nurses. Thus, institutions need to develop a comprehensive understanding of the factors that hinder the transfer of wound care knowledge into practice.48
The study’s results highlighted a lack of knowledge on skin tear definition, classification and risk factors. This might be related to the fact that the first certificate wound course (CAS HES-SO) began in 2005, but the specific topic of skin tears has only been taught since 2017. Only half of the wound care specialists with up to two years of experience could describe a skin tear using terminology related to the skin tear’s definition. Additionally, the term ‘skin tear’ is not unanimously used, and professionals often use general terms such as ‘laceration’ or, in French, lacération or dermabrasion1,49,50, making awareness problematic. Only one third identified a skin tear as a ‘traumatic wound’, and slightly more than 50% referred to ‘mechanical forces, friction or shear’. Terms like ‘skin frailty’, ‘elderly’ and ‘dermatoporosis’, when used in describing a skin tear, are inappropriate because they relate to skin conditions and should be identified by nurses as risk factors for developing skin tears.35,36,51
Concerning skin tear classification, most participants (91%) did not use a classification system in their clinical practice, and more than half (55%) declared not knowing the three types of skin tears based on ISTAP classifications; this is similar to findings in other studies.30,32 For example, in LeBlanc and colleagues’ survey30, 80.9% of respondents did not use any classification system, and 96% of nurses reported no knowledge of any classification system in the German survey.32
More than two-thirds (68%) of the respondents declared having no workplace policies concerning the identification of patients at risk of skin tears. The top four most frequent risk factors were impaired mobility, pharmacological therapies, malnutrition and age. Characteristics of older patients that are highly associated with having developed a skin tear are ecchymosis (bruising), senile purpura, haematoma and evidence of a previously healed skin tear, oedema and the inability to reposition oneself independently.35 Risk factors identified are age-related skin changes, dehydration, malnutrition, sensory changes, mobility impairment, pharmacological therapies and mechanical factors related to skincare practices.36 Surprisingly, few nurses identified skin changes (26%), previous skin tears (9%) and oedema (9%) as risk factors. Addressing skin tear risk factors should be part of a common-sense approach to patient care.1,2,27 Appropriate knowledge of the risk factors could reduce, or even avoid, the occurrence of skin tears.36
The results showed no institutional policies for nurses to declare skin tears (75%) on an incident form/risk management software. Furthermore, there is no specific coding for a skin tear in the World Health Organization International Classification of Diseases (ICD) 11th edition, but there is coding related to all types of laceration with or without a foreign body.52 The lack of coding contributes to the perception that skin tears are insignificant injuries and leads to the poor frequency reports of these injuries.49 In addition, the previous literature has reported problems with skin tear documentation because of a lack of consistent and universal language for their documentation and assessment.28,30–32,53,54
Only 6% of the respondents declared having preventive measures for skin tears in their care settings. Nonetheless, a substantial number of respondents (93%) reported using skin moisturisers daily on all patients, and soap and water (90%) to wash patients. Regular moisturising should be seen as an essential part of skincare for people presenting frail skin, to promote general skin health and reduce the risk of skin damage, restore the skin’s barrier function, reduce itching and increase the level of hydration.51
A randomised controlled trial evaluating the effectiveness of a twice-daily moisturising regimen showed a nearly 50% reduction in the incidence of skin tears in residents living in aged care facilities.55 Supporting these findings, the application of a pH-friendly, non-perfumed moisturiser twice daily to the extremities resulted in a significant reduction of the incidence of skin tears.56 Furthermore, a systematic review on the efficacy and effectiveness of basic skincare interventions for maintaining skin integrity in the aged suggest that liquid soaps are better than traditional soaps, and the application of moisturisers with humectant has a clear positive effect of reducing dry skin conditions and enhancing the skin’s barrier function.57
Our results show that only six participants followed a ‘standard of care’, and physicians were not often involved in wound treatment prescriptions. However, even though nurses cannot prescribe wound dressings in Switzerland, they frequently propose the local wound’s treatment in clinical practice.
Additionally, the survey results revealed that pain, delayed healing/chronic wound–ulcer formation and frequent dressing changes were common issues and complications when managing skin tears. Pain and decreased quality of life have been reported by individuals suffering from skin tears.25,58 This is problematic when skin tears occur on the lower limbs, or in patients with multiple comorbidities.1 Thus, traumatic wounds can become chronic wounds.59 In addition, frequent dressing changes may prejudice wound healing, lower patient satisfaction, cause pain or lead to cross-contamination or infection due to frequent exposure of the wound.60 Therefore, selecting a comfortable dressing that does not cause pain, anxiety and stress when changed or while worn, and a possible extended wear time, is important for patient acceptability and comfort.60
Strengths and limitations of the study
To our knowledge, this was the first study in French-speaking Switzerland on this topic. It is limited by including only wound care nurse specialists. Although not intended to be generalised, the results are not valid for a German- or Italian-speaking Swiss cohort.
Point-prevalence studies on skin tears might have enlightened the scope of the problem in clinical settings; however, access to nurses and patients in different clinical settings was restricted during this study, due to the COVID-19 pandemic.
CONCLUSION
The results identified a lack of nurses’ knowledge on skin tears, insufficient prevention measures, inadequate treatment measures and a need for education. It highlights the importance of wound care education at all levels to enhance the implementation of evidence-based practice guidelines.
RECOMMENDATIONS
To enhance nurses’ knowledge of wound care in general and to ensure evidence-based practices in particular, we recommend the implementation of standard and unified wound curricula for nurses at the undergraduate, graduate and post-graduate levels, based on the existing European curricula. Additional research should be done to explore non-specialised wound care nurses’ perceptions, opinions, knowledge and clinical practices on the prevention and management of skin tears. Point prevalence studies are recommended to gain insights into the scope of the problem of skin tears in clinical settings.
Key messages
- Although skin tears are common in French Switzerland, their definition, classification and risk factors are not well known among nurses.
- Implementing standard and unified wound curricula for nurses at the undergraduate and post-graduate levels is needed to enhance nurses’ knowledge of wound care in general and to ensure evidence-based practices.
- Research is required to gain insights into the scope of the problem of skin tears in clinical settings.
Author(s)
Lucie Charbonneau, M.Sc., RN, DAS in Wound Care, Assistant lecturer UAS1,2
Sebastian Probst, DClinPrac, MScN RN, Professor of Tissue Viability and Wound Care1,3,4
Georgina Gethin, Professor of Nursing, Director of Alliance for Research and Innovation in Wounds1,4,5
1 Geneva School of Health Sciences, HES-SO University of Applied Sciences and Arts Western Switzerland, Geneva, Switzerland
2 Lausanne University Hospital, Lausanne, Switzerland
3 University Hospital Geneva, Geneva, Switzerland
4 Faculty of Medicine Nursing and Health Sciences, Monash University, Melbourne, Australia
5 School of Nursing and Midwifery, NUI Galway, Galway, Ireland
Correspondence: lucie.charbonneau@hesge.ch
Conflict of interest: None
References
- LeBlanc K, Campbell K, Dunk AM, Harley C, Hevia H, Holloway S, et al. Best practice recommendations for the prevention and management of skin tears in aged skin. Wounds Int 2018.
- Clothier A. Assessing and managing skin tears in older people. Nurse Prescribing 2014; 12(6):278–82.
- LeBlanc K, Baranoski S. Skin tears: State of the science: Consensus statements for the prevention, prediction, assessment, and treatment of skin tears. Adv Skin Wound Care 2011; 24(9 Suppl):2–15.
- Wang D, Xu H, Chen S, Lou X, Tan J, Xu Y. Medical adhesive-related skin injuries and associated risk factors in a pediatric intensive care unit. Adv Skin Wound Care 2019; 32(4):176–82.
- Hawk J, Shannon M. Prevalence of skin tears in elderly patients: A retrospective chart review of incidence reports in 6 long-term care facilities. Ostomy Wound Manage 2018; 64(4):30–6.
- Woo K, LeBlanc K. Prevalence of skin tears among frail older adults living in Canadian long-term care facilities. Int J Palliat Nurs 2018; 24(6):288–94.
- Van Tiggelen H, Van Damme N, Theys S, Vanheyste E, Verhaeghe S, LeBlanc K, et al. The prevalence and associated factors of skin tears in Belgian nursing homes: A cross-sectional observational study. J Tissue Viability 2019; 28(2):100–6.
- Skiveren J, Wahlers B, Bermark S. Prevalence of skin tears in the extremities among elderly residents at a nursing home in Denmark. J Wound Care 2017; 26(Sup2):S32–6.
- Parker CN, Finlayson KJ, Edwards HE, MacAndrew M. Exploring the prevalence and management of wounds for people with dementia in long-term care. Int Wound J 2020; 17(3):650–9.
- LeBlanc K, Christensen D, Cook J, Culhane B, Gutierrez O. Prevalence of skin tears in a long-term care facility. J Wound Ostomy Continence Nurs 2013; 40(6):580–4.
- Koyano Y, Nakagami G, Iizaka S, Minematsu T, Noguchi H, Tamai N, et al. Exploring the prevalence of skin tears and skin properties related to skin tears in elderly patients at a long-term medical facility in Japan. Int Wound J 2016; 13(2):189–97.
- Hahnel E, Blume-Peytavi U, Trojahn C, Kottner J. Associations between skin barrier characteristics, skin conditions and health of aged nursing home residents: A multi-center prevalence and correlational study. BMC Geriatr 2017; 17(1):1-12.
- Edwards HE, Chang AM, Gibb M, Finlayson KJ, Parker C, O’Reilly M, et al. Reduced prevalence and severity of wounds following implementation of the Champions for Skin Integrity model to facilitate uptake of evidence-based practice in aged care. J Clin Nurs 2017; 26(23–4):4276–85.
- LeBlanc K, Woo KY, VanDenKerkhof E, Woodbury MG. Skin tear prevalence and incidence in the long-term care population: A prospective study. J Wound Care 2020; 29(Sup7):S16–22.
- Munro EL, Hickling DF, Williams DM, Bell JJ. Malnutrition is independently associated with skin tears in hospital inpatient setting-Findings of a 6-year point prevalence audit. Int Wound J 2018; 15(4):527–33.
- Feng H, Wu Y, Su C, Li G, Xu C, Ju C. Skin injury prevalence and incidence in China: A multicentre investigation. J Wound Care 2018; 27(Sup10):S4–9.
- Chang YY, Carville K, Tay AC. The prevalence of skin tears in the acute care setting in Singapore. Int Wound J 2016; 13(5):977–83.
- Bermark S, Wahlers B, Gerber AL, Philipsen PA, Skiveren J. Prevalence of skin tears in the extremities in inpatients at a hospital in Denmark. Int Wound J 2018; 15(2):212–7.
- McErlean B, Sandison S, Muir D, Hutchinson B, Humphreys W. Skin tear prevalence and management at one hospital. Prim Intent 2004; 12(2):83–8.
- Santamaria N. Woundswest: Identifying the prevalence of wounds within western Australia’s public health system. EWMA Journal 2009; 9(3):13–8.
- Amaral AFDS, Pulido KCS, Santos VLCDG. Prevalência de lesões por fricção em pacientes hospitalizados com câncer. Revista da Escola de Enfermagem da USP. 2012; 46(spe):44–50.
- Maida V, Ennis M, Corban J. Wound outcomes in patients with advanced illness. Int Wound J 2012; 9(6):683–92.
- McLane KM, Bookout K, McCord S, McCain J, Jefferson LS. The 2003 National Pediatric Pressure Ulcer and Skin Breakdown Prevalence Survey: A multisite study. J Wound Ostomy Continence Nurs 2004; 31(4):168–78.
- Pancorbo-Hidalgo PL, Torra-Bou JE, Garcia-Fernandez FP, Soldevilla-Agreda JJ. Prevalence of pressure injuries and other dependence-related skin lesions among paediatric patients in hospitals in Spain. EWMA Journal 2018; 19(2):29–37.
- Baranoski S. Meeting the challenge of skin tears. Adv Skin Wound Care 2005; 18(2):74–5.
- LeBlanc K, Baranoski S, Christensen D, Langemo D, Edwards K, Holloway S, et al. The art of dressing selection: A consensus statement on skin tears and best practice. Adv Skin Wound Care 2016; 29(1):32–46.
- Benbow M. Assessment, prevention and management of skin tears. Nurs Older People 2017; 29(4):31–9.
- White W. Skin tears: A descriptive study of the opinions, clinical practice and knowledge base of RNs caring for the aged in high care residential facilities. Prim Intent 2001; 9(4):138–49.
- McTigue T, D’Andrea S, Doyle-Munoz J, Forrester DA. Efficacy of a skin tear education program: Improving the knowledge of nurses practicing in acute care settings. J Wound Ostomy Continence Nurs 2009; 36(5):486–92.
- LeBlanc K, Baranoski S, Holloway S, Langemo D, Regan M. A descriptive cross-sectional international study to explore current practices in the assessment, prevention and treatment of skin tears. Int Wound J 2014; 11(4):424–30.
- Liu H. Nurses’ knowledge about assessment, prevention, and treatment of skin tears in the acute care setting. Case Western Reserve University Doctor of Nursing Practice; 2019.
- Scheele CM, Gohner W, Schumann H. Cross-sectional study on skin tears in fragile, aging skin: Nursing deficits in a common problem in Germany. Pflege 2020; 33(3):123–32.
- Charbonneau L, Probst S, Gethin G. Translation and cross-cultural adaptation of a survey on skin tears among nurses in French-speaking Switzerland. J Wound Manag 2021; 22(1):45–50.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psycho 2006; 3:77–101.
- Lewin GF, Newall N, Alan JJ, Carville KJ, Santamaria NM, Roberts PA. Identification of risk factors associated with the development of skin tears in hospitalised older persons: A case–control study. Int Wound J 2016; 13(6):1246–51.
- Serra R, Ielapi N, Barbetta A, de Franciscis S. Skin tears and risk factors assessment: A systematic review on evidence-based medicine. Int Wound J 2018; 15(1):38–42.
- Terwee CB, Bot SDM, De Boer MR, Van Der Windt DAWM, Knol DL, Dekker J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol 2007; 60(1):34–42.
- Cho YI, Johnson TP, Vangeest JB. Enhancing surveys of health care professionals. Eval Health Prof 2013; 36(3):382–407.
- Dillman DA. Mail and internet surveys: The tailored design method. 2nd ed. New York: J. Wiley; 2000.
- Ball HL. Conducting online surveys. J Hum Lact 2019; 35(3):413–7.
- Ganassali S. The influence of the design of web survey questionnaires on the quality of responses. Surv Res Methods 2008; 2:21–32.
- Lopez V, Dunk AM, Cubit K, Parke J, Larkin D, Trudinger M, et al. Skin tear prevention and management among patients in the acute aged care and rehabilitation units in the Australian Capital Territory: A best practice implementation project. Int J Evid Based Healthc 2011; 9(4):429–34.
- Woolhouse T, Moola S. Evidence based approach to the management and prevention of skin tears within an aged care setting: A best practice implementation project. JBI Evid Synth 2014; 12(9):502–14.
- Langemo DK, Williams A, Edwards K. Skin tears: Prevention and management. Nursing 2019; 49(4):66–9.
- Idensohn P, Beeckman D, Campbell KE, Gloeckner M, LeBlanc K, Langemo D, et al. Skin tears: A case-based and practical overview of prevention, assessment and management. J Community Nurs 2019; 33(2):32–41.
- LeBlanc K, Langemo D, Woo K, Campos HMH, Santos V, Holloway S. Skin tears: Prevention and management. Br J Community Nurs 2019; 24(Sup9):S12–8.
- Kuhnke JL, Keast D, Rosenthal S, Evans RJ. Health professionals’ perspectives on delivering patient-focused wound management: A qualitative study. J Wound Care 2019; 28(Sup7):S4–13.
- Gagnon J, Lalonde M, Polomeno V, Beaumier M, Tourigny J. Le transfert des connaissances en soins de plaies chez les infirmières: Une revue intégrative des écrits. Recherche Soins Infirmiers 2020; (143): 45–61.
- Rayner R, Carville K, Leslie G, Roberts P. A review of patient and skin characteristics associated with skin tears. J Wound Care 2015; 24(9):406–14.
- De Saint Leger A-S, Moiziard A-S, Meaume S. Les plaies de la personne âgée ou très âgée. Soins 2009; 56(734):21–6.
- Beeckman D, Campbell K, LeBlanc K, Campbell JL, Dunk AM, Harley C, et al. Best practice recommendations for holistic strategies to promote and maintain skin integrity. Wounds Int2020.
- World Health Organization [Internet]. International Classification of Diseases 11th Revision 2019. Available at [https://icd.who.int/browse11/l-m/en].
- Carville K, Smith J. A report on the effectiveness of comprehensive wound assessment and documentation in the community. Prim Intent 2004; 12(1):41–9.
- LeBlanc K, Baranoski S, Holloway S, Langemo D. Validation of a new classification system for skin tears. Adv Skin Wound Care 2013; 26(6):263–5.
- Carville K, Leslie G, Osseiran-Moisson R, Newall N, Lewin G. The effectiveness of a twice-daily skin-moisturising regimen for reducing the incidence of skin tears. Int Wound J 2014; 11(4):446–53.
- Finch K, Osseiran-Moisson R, Carville K, Leslie G, Dwyer M. Skin tear prevention in elderly patients using twice-daily moisturiser. Wound Pract Res 2018; 26(2):99–109.
- Kottner J, Lichterfeld A, Blume-Peytavi U. Maintaining skin integrity in the aged: A systematic review. Br J Dermatol 2013; 169(3):528–42.
- LeBlanc K, Baranoski S, Christensen D, Langemo D, Sammon MA, Edwards K, et al. International Skin Tear Advisory Panel: A tool kit to aid in the prevention, assessment, and treatment of skin tears using a Simplified Classification System. Adv Skin Wound Care 2013; 26(10):459–76; quiz 77–8.
- Probst S, Séchaud L, Bobbink P, Skinner MB, Weller CD. The lived experience of recurrence prevention in patients with venous leg ulcers: An interpretative phenomenological study. J Tissue Viability 2020; 29(3):176–9.
- Brindle T, Farmer P. Undisturbed wound healing: A narrative review of the literature and clinical considerations. Wounds Int 2019; 10(2):40–8.
