Volume 23 Number 3
A digital wound management checklist to support clinical decision-making: A qualitative validation study
Sari A. Kaari, Mervi S. Vähätalo, Kirsti M. Ahmajärvi, Milla T. Kallio, Heli M. Lagus, Kirsi M. Isoherranen
Keywords Wound care, Checklist, software, usability, wound navigator
DOI 10.35279/jowm2022.23.03.04
Abstract
Aim The research objective was to explore how a digital wound management checklist (Wound Navigator) affects clinical decision-making. The aim was to understand how physicians view the use of digital checklists in a clinical setting.
Methods The research was conducted as a qualitative case study with a usability testing approach. Nine test subjects were given seven fictional patient cases, which included picture(s) of the wound with some medical history and details of the wound. The results were analysed according to the usability domains effectiveness, efficiency and engagement.
Results With the digital wound management checklist, all test subjects were able to work through patient cases and receive a valid conclusion and recommendations for follow-up procedures. The majority of the test subjects found that it helped in selecting follow-up procedures. Several test subjects reported that the digital wound management checklist brought structure to the patient assessment and commented on its clear user interface. Improvements pointed out by the test subjects included decreasing the number of mouse clicks. Test subjects reported that they could use the digital wound management checklist in clinical work to assist in patient assessment, especially with more complex cases.
Conclusions and implications for clinical practice The digital wound management checklist provides structure to the patient assessment and can either enforce or broaden the clinical decision-making process; thus, it can be useful, especially when assessing more complex cases or when the physician is inexperienced. End-users declared the digital wound management checklist was a tool they would use in their work.
INTRODUCTION
Wounds have a profound effect at both the individual and societal levels, requiring substantial healthcare expenditures while having a drastic effect on quality of life (1,2). The reason why a wound becomes chronic should always be diagnosed; often, there is a chronic condition affecting the persistence of a wound (3,4). The crucial aspects of wound management are well-executed clinical examination and history-taking, which form the foundation for diagnosis and care (5). The aetiology of the wound guides the clinical decision-making process, the selection of interventions and over-all care plan. If the root cause is not established in time, a delayed diagnosis can lead to serious adverse effects and increased costs (3).
Checklists are quick and appropriate tools for clinical practice while including all the items required for an examination. These tools are typically easy to implement within the clinical guidelines for practice (7). For example, the World Health Organization published a surgical safety checklist in 2008 to improve patient safety in surgical procedures. The use of checklists has been proven to promote patient safety. Research on patients suffering from wounds and undergoing surgical procedures reported changes in patient care in nearly 50% of cases due to the use of checklists (7).
Usability is defined in the literature as the ‘extent to which a system, product or service can be used by specified users to achieve specific goals with effectiveness, efficiency and satisfaction in a specified context of use’ (8). Effectiveness refers to the accuracy and completeness with which users achieve specified goals, whereas efficiency is related to the resources spent to achieve the goals. Efficiency reflects the speed of work, either from a quantitative time-consumption perspective or a more subjective perspective, such as a task requiring too many mouse clicks (8,9). The ISO standard defines satisfaction as comfort and acceptability of use. Similarly, the pleasantness and satisfying qualities of the product are combined in the literature as engagement (9). However, engagement can also depend on the perceived overall usability of a system (10).
The research objective of the present study was to explore how a digital wound management checklist (Wound Navigator) affects the clinical decision-making process. In addition, the aim was to understand how physicians view the use of digital checklists in a clinical setting. The research questions were as follows:
- How do digital checklists support clinical decision-making in wound management?
- How do clinical professionals perceive the usability of digital checklists in a clinical setting for wound management?
The digital wound management checklist is an interactive tool that provides sets of questions for the user. The question set varies according to the location of the wound and depending on the answers the user selects, as the questions follow a predefined decision tree. The questions cover the most important aspects of wound assessment and the most typical wound types.
METHOD
The research was conducted as a qualitative case study with a usability testing approach. End-user testing was employed as the data collection method. Usability testing aims to discover what users do and what they do not do. Testing enables us to collect data on users’ perceptions, what they want from a product and whether the product supports users in reaching their goals (10). The sample size was determined by data saturation. Saturation refers to the point where no new data relating to the research questions emerges (11).
The nine test subjects represented two groups: medical students and physicians working in primary care. The test subjects represented the defined user group for the digital wound management checklist. They were given seven fictional patient cases with typical and atypical wounds, which they evaluated based on their clinical knowledge. These fictional cases represented tasks for usability testing; five were typical lower limb wounds, while two represented atypical wounds. The test cases were written following the method for key feature problems (KFP), which is generally used for clinical decision-making skills testing. The KFP method allows researchers to identify the critical issues related to clinical decision-making and represents a validated measure for diagnostic accuracy (12,13). This approach was used to compare the results of the patient case evaluations.
The seven fictional patient cases included picture(s) of the wound with some medical history and wound details (Figure 1). When the test subjects evaluated these cases, they could ask for further details, for example regarding the ankle brachial index. If they did not ask for further details, such information was not automatically provided. The seven patient cases represented typical and atypical wounds, as follows:
1. An atypical lower limb wound with a wound infection (pyoderma gangrenosum related to Crohn’s disease)
2. Lower limb wound related to swelling in the limb
3. Lower limb wound related to ischemia and swelling
4. Ischemic pressure wound in lower limb
5. Diabetic and neuropathic lower limb wound
6. Pressure wound in the buttock area
7. Post-operative atypical (pyoderma gangrenosum) wound in upper limb
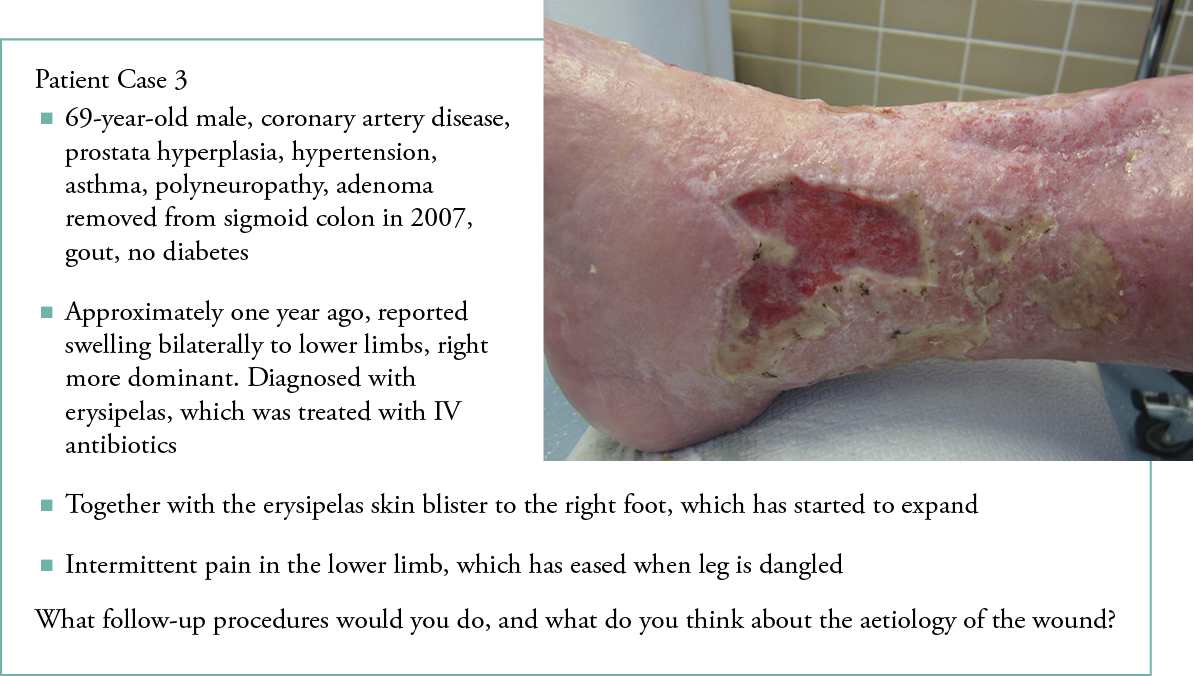
Figure 1: Example of a patient case
The test subjects were not able to use any reference materials or support tools while evaluating the fictional patient cases, thus they needed to rely on their previous experiences of treating patients suffering from a wound. The test subjects stated their conclusions and defined the follow-up procedures, which were recorded and analysed according to the predefined key features. After going through the seven patient cases, the test subjects used the digital wound management checklist and went through the cases again. The action suggestions given by the digital wound management checklist were recorded and analysed again according to their key features. The results from each patient case, without and with the digital wound management checklist, were then compared and evaluated for differences.
In addition to fictional patient case evaluations, the test subjects were interviewed regarding the digital wound management checklist’s usability as a part of clinical work. The interviews were semi-structured, to facilitate clarifying and deepening the discussion on possible issues raised during the interviews. The interview questions covered various aspects of checklists in clinical settings and the digital wound management checklist. For example, one question was, ‘How do you feel using digital checklists in your work?’ The semi-structured interview method allows flexibility, as the interviewer may change the order of the questions (14).
The interviews were recorded and transcribed verbatim. The full end-user testing session was observed, when possible, and any findings related to the use of the digital wound management checklist were noted and included in the data collection. The findings from the data collection phase were themed according to three usability domains: effectiveness, efficiency and engagement. These domains and concepts represented the themes for analysis. Following the thematisation, the findings were subject to qualitative content analysis.
RESULTS
Effectiveness
The effectiveness dimension of usability measures whether the tasks given were completed successfully (9). In this study, this was evaluated using patient cases with KFP. During the data analysis, findings from the patient case evaluations were complemented with the semi-structured interview answers related to the clinical decision-making process.
The test subjects were more confident when evaluating patient Cases 2–5, which were represented as ease and swiftness in determining the follow-up procedures and possible aetiology. In addition, for more familiar cases, the test subjects often reported possible diagnoses and were confident in their decisions. Cases 1, 6 and 7 were clearly more difficult to assess. Case 7 caused the greatest uncertainty among the test subjects, most of whom reported that they did not have any idea what the aetiology of the wound might be. However, most of them were able to identify the recommended procedure (biopsy). One test subject was not able to select any follow-up procedures for Case 7.
After evaluating the seven patient cases, the test subjects went through the same cases again with the help of the digital wound management checklist. They answered the questions in the digital wound management checklist and received a summary of their answers and procedure recommendations for each patient case. With the digital wound management checklist, all test subjects were able to complete each patient case evaluation and to proceed from one question to the next without issues, completing the full question set for each of them. After answering the questions, the subjects received a valid conclusion and follow-up procedure recommendations for each patient case.
The results received with the digital wound management checklist were compared with the evaluations made without the digital wound management checklist with the help of KFPs. Key features mentioned by the test subjects without the digital wound management checklist were compared to the key features covered by the results received from the digital wound management checklist. The comparison is presented as a summary in Table 1. The quantitative summary is for visualisation purposes.
Table 1: Summary of patient case evaluation comparisons
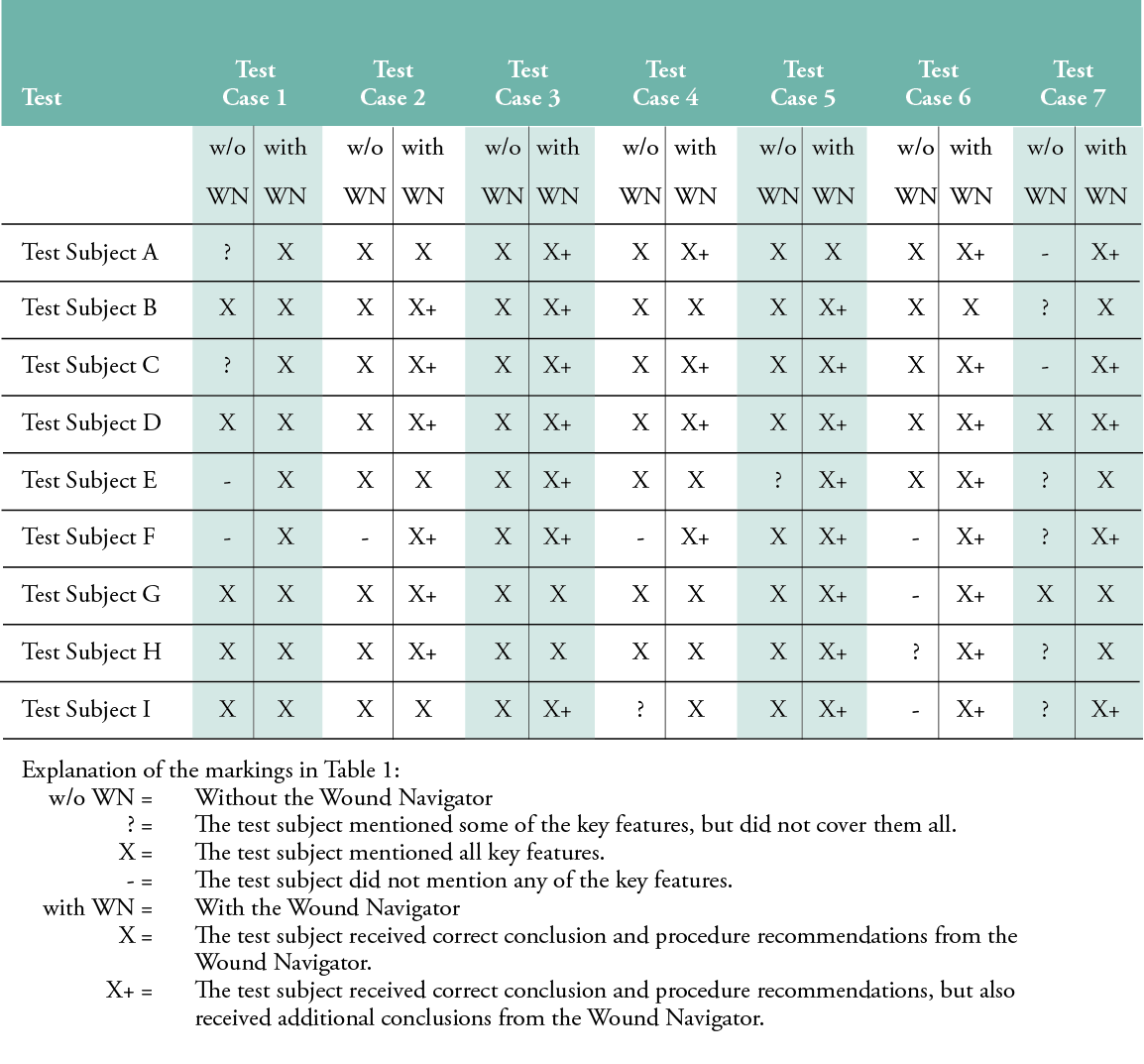
According to the interview results, most test subjects found that the digital wound management checklist helped them to select and narrow down the possible follow-up procedures, especially in the more complex cases. Several pointed out and observed during end-user testing that some of the medical terms and descriptions used in the digital wound management checklist were not familiar; examples of these were ‘purple rim around the wound’, as it was not defined more precisely, and ‘sinus pilonidalis’, which might not be a familiar term. The user might not be able to complete the questions if they do not understand what is being asked. This would hinder them from completing the task, thus affecting the effectiveness dimension of usability. Another issue related to the concepts used that could weaken the effectiveness dimension was observed during the testing sessions: test subjects seemed to perceive that the wound had signs of infection, even when there were no evident clinical signs of infection. This was possibly caused by an unclear description of the clinical signs of infection.
Several test subjects reported the digital wound management checklist’s benefits as bringing structure to the patient assessment, which can be especially difficult for more complex wounds. They felt that it covered a variety of issues that can affect the wound, some of which they would not necessarily have noticed themselves.
Efficiency and engagement
Efficiency relates to how quickly a task can be completed, whereas engagement, in this context, relates to the pleasantness of using the software (9). Efficiency was partly studied in the patient case evaluation and complemented with the semi-structured interview answers, whereas the engagement dimension was covered by interview replies.
During the end-user testing, the test subjects pointed out that the user interface was clear to them. For example, they said, ‘the digital wound management checklist worked smoothly and was clear’ and ‘It was clear and did not have too many options to choose from’. Not having too many options or in-depth questions made it faster to use. In addition, one subject mentioned that there was no need for operational instructions. Similar conclusions were drawn while observing the testing. The test subjects neither stopped to think about how to proceed nor asked for instructions on how to use the digital wound management checklist during testing. A clear interface promotes efficiency, as the user does not have to spend time figuring out how the software functions. Additionally, time is saved if the user does not need to look for instructions.
During the interview, test subjects pointed out a couple of issues relating to the digital wound management checklist’s efficiency. There were two improvement suggestions for the tool: combining several questions into one view, and showing some of the procedure recommendations in the digital wound management checklist itself, instead of using a pdf document. In the version of the digital wound management checklist that was tested, the questions were presented to the user one at a time, so that after they answered one question, the next question appeared. Combining several questions onto one screen would decrease the number of clicks the user has to make, thus speeding up the answering process and improving the efficiency of the software.
The digital wound management checklist gives procedure recommendations in two ways: short recommendations directly after the user has answered all questions, and longer, more comprehensive instructions given in a separate pdf document, which the user can download and open when necessary. The test subjects wished that some of the additional instructions could have been added to the digital wound management checklist from the pdf document. This would improve the digital wound management checklist’s efficiency, as the user would not need to open the pdf. Another issue relating to the pdf recommendations also related to the number of clicks. This matter was raised through observation. Test subjects needed to make several mouse clicks to open the pdf procedure recommendations, again affecting efficiency.
When the engaging dimension of usability was explored from the data collected, several matters were revealed. All test subjects reported that they could use the digital wound management checklist in their clinical work to assist in wound patient assessment. Their reactions included, ‘…it is like a game!’, ‘it’s quite the bomb, in a positive way’, and ‘…nice, compact tool…’. These positive comments from the users indicate that the digital wound management checklist’s user interface aroused positive feelings among the test subjects, and positive feelings promote engagement with the software. Several test subjects were eager to start using the digital wound management checklist in their clinical work as soon as possible. The notion that the digital wound management checklist resembles a game could imply that the user felt engaged with the software. Gamification is commonly used in digital service design to increase users’ engagement (15).
DISCUSSION
This study studied how a digital wound management checklist can support clinical decision-making and how clinical professionals perceive the usability of digital checklists in the clinical setting for wound management. The results of this study indicate that digital checklists can bring structure to the patient assessment process, especially in more complex cases, by helping to select and narrow down the possible follow-up procedures. The digital wound management checklist’s user interface was clear to use, and test subjects reported that they could use it in their clinical work. Checklists have frequently been used in healthcare, and research has shown that using checklists can reduce adverse effects and improve quality of care.(16,6) Digital checklists have also been shown to support clinical decision-making and improve the usability of checklists (17).
Digital checklists in clinical decision making
Based on the findings from this study, a digital wound management checklist can have a positive impact on clinical decision-making. Two scenarios clearly stood out from the test subjects’ feedback:
- Complex or otherwise atypical wound patient assessment
- Unexperienced physicians (those with less experience in, or when it has been a long time since, treating a patient suffering from a wound), especially in primary healthcare.
A digital wound management checklist can provide structure to the patient assessment process, as it prompts the user to go through the questions required to produce procedure recommendations. The questions are evidence-based and follow predetermined decision trees, which supports the implementation of clinical guidelines in practice (6). Thus, it can remind the user of various factors that can affect wound healing. The user can follow the questions when evaluating the patient’s case, to ensure that all relevant factors are considered during the evaluation. This is especially helpful in complex patient cases, where there can be multiple comorbidities affecting the wound.
Another benefit of a digital wound management checklist in clinical decision-making is that it can either enforce or broaden the process. As it provides procedure recommendations, the user can compare their own reasoning to the results received from the digital wound management checklist. The physician is always responsible for the decision-making, but by using the digital checklist, the procedure recommendations can be used to ensure that all recommended procedures are performed. Surgical checklists have had a positive effect on decision-making (7), and based on the results of this study, the same potential can be seen in the digital wound management checklist.
The test subjects reported that they had not used checklists widely in their clinical work; however, they did report that checklists could support it. The subjects also reported that they had used some digital tools in their work, but it is surprising how few digital tools had been used, as the subjects came from an age group that can be considered digital natives. Based on the findings in this research, it seems that there is an unmet need for digital checklists, especially as the literature has shown that their use can reduce adverse effects in healthcare.
Usability of digital checklists
Usability is defined in the literature as the ‘extent to which a system, product or service can be used by specified users to achieve specified goals with effectiveness, efficiency and satisfaction in a specified context of use’ (8). In this study, the usability of the digital wound management checklist was studied from three key dimensions: efficiency, effectiveness and engagement. Implementation of checklists requires motivation from the professionals, and the use of checklists should be effective to be beneficial (16). Better usability can engage users with the service and improve productivity, as time is not lost deciphering complicated and illogical digital tools (18).
The test subjects underlined the importance of ease of use during the interviews. Each subject emphasised that they would use digital checklists if they were quick and easy to use and readily available. The subjects considered the wound management checklist to have a clear user interface that supported task completion, and thus the effectiveness of the digital wound management checklist. To further improve the efficiency dimension, the number of mouse clicks required was noted as a development matter for the software. The test subjects mentioned that the lack of time and resources can prevent the use of digital tools in a clinical setting, however useful they might be. The efficiency dimension of usability was thus considered critical. Digital checklists must not only provide the features needed, emphasis must also be put on the time resources required to use them. Overly complex and time-consuming tools are not usable in the current healthcare setting; there is a great need to produce tools that save time, rather than spend it. Still, it should be noted that time used in examining the wound to resolve its aetiology is time well spent, as it leads to speedier recovery. Thus, time spent using the digital wound management checklist can be considered an efficient use of time.
The engagement dimension is considered an important factor in usability. Users expect good usability, and if those expectations are not met, users will not engage with the software (10). End-users considered the tool pleasant to use and were satisfied with it. They reported that the checklist was a tool that they would use in their work, and some even expressed eagerness to begin using the checklist as soon as possible. Such findings provide insight into the engaging qualities of the software and indicate that the software has managed to engage the test subjects and would be accepted for use. In combining the end-users’ tests findings in the context of the three usability dimensions, we can conclude that each of these is important for users hoping to adopt the tool in their work routines.
In addition to the above, the finding mentioned in the efficiency portion of the Results section, that the user interface was described as clear, can be perceived as also related to the engaging dimension. An easy and pleasurable user interface promotes engagement with and satisfaction in the software. Several users emphasised that the digital wound management checklist would be useful, especially with more complex cases, as it provides ‘concrete instructions and simple questions’. As for the digital wound management checklist’s good features, the test subjects mentioned that the recommendations were clear and concise, and the procedure recommendations gave them assurance on how to handle difficult wounds. Such assurance can promote engagement with the software.
Limitations
The sample size in the study was small, which limits the generalisation of the results regarding the effects of the checklist on the clinical decision-making process. The number of end-users involved in the testing was limited, due to the Covid-19 pandemic, as professionals’ time and resources were tied up by the acute situation. However, the number of test subjects can be considered adequate for usability tests. According to the literature, a small number of test subjects is enough, since the number of new findings decreases with each participant (19). This was also observed here, as there were significant similarities among the test subjects’ answers. New information was not emerging from the data; thus, the data had reached saturation with this sample size.
The generalisation of the results may also be limited, due to the non-random selection of the sample. Five of the nine test subjects had previously worked with one of the co-authors. The other four test subjects, by contrast, were selected by their supervisors, who had no connection to the study; none had used a digital wound management checklist. Still, the co-author did not participate in the end-user testing or interviews.
Another limitation was that the researcher knew the patient cases and the KFPs related to the patient cases. They were planned so that they covered the different areas included in the digital wound management checklist, as the testing was part of the tool’s validation. This could have affected the objectivity of the research, as the patient cases did not represent a random sample as would be the case of patients arriving at a clinic. However, the patient cases were selected to cover the most common types of wounds seen in primary healthcare settings.
CONCLUSION
A digital wound management checklist provides structure to the patient assessment and can either enforce or broaden the clinical decision-making process, thus it could be useful, especially when assessing more complex cases or when the physician is inexperienced. End-users reported that the wound management checklist was a tool they would use in their work.
Future research
- Future research could include replicating the research design with actual patients. This would provide insights on using the digital wound management checklist in a real-world setting.
Acknowledgements
This study received no financial support.
Key messages
- Checklists provide a quick tool for clinical settings and promote patient safety.
- This study investigates how a digital wound management checklist affects the clinical decision-making process.
- The digital wound management checklist can provide support in examining patients who suffer from wounds and support clinical decision-making. To be useful in clinical settings, digital checklists should be straight-forward to use.
Author(s)
Sari A. Kaari, MSc, IT Management, Helsinki University Hospital, Helsinki, Finland
Mervi S. Vähätalo, RN, MNSc, PhD (business & admin.), Satakunta University of Applied Sciences, Pori, Finland
Kirsti M. Ahmajärvi, MD, Specialist in general practice, Special competence in wound management, PhD Student, Department of General
Practice and Primary Health Care, University of Helsinki and Helsinki University Hospital, Helsinki, Finland
Milla T. Kallio, MD, PhD, Helsinki University Hospital and Helsinki University Abdominal Center, Vascular Surgery, Helsinki, Finland
Heli M. Lagus, MD, PhD, Department of Plastic Surgery and Wound Healing Centre, Helsinki University Hospital, University of Helsinki, Helsinki, Finland
Kirsi M. Isoherranen, MD, PhD, Helsinki University Hospital, University of Helsinki, Helsinki, Finland
Correspondence: Sari Kaari, kaari.sari@gmail.com
Conflict of interest: None
References
- Lindholm C, Searle R. Wound management for the 21st century: Combining effectiveness and efficiency. Int Wound J 2016; 13(S2):5-15.
- Guest JF, Fuller GW, Vowden P. Cohort study evaluating the burden of wounds to the UK’s National Health Service in 2017/2018: Update from 2012/2013. BMJ Open 2020; 10(12).
- Ahmajärvi K, Isoherranen K. Kroonisten haavojen hoito perusterveydenhuollossa [Treatment of wound patients in primary health care]. Suomen Lääkärilehti [Finnish Medical Journal] 2017; 72(8):524-8.
- Isoherranen K, Kallio M, Jordan O’Brien J, Lagus H. Clinical characteristics of lower extremity ulcers. J Wound Manage 2020; (21)1:51-8.
- Mooij MC, Huisman LC. Chronic leg ulcer: Does a patient always get a correct diagnosis and adequate treatment? Phlebology 2016; 31(1 Suppl):68-73.
- Snyder RJ, Jensen J, Applewhite AJ, Couch K, Joseph WS, Lantis JC, et al. A standardized approach to evaluating lower extremity chronic wounds using a checklist. Wounds 2019; 31(5 Suppl):S29-44.
- Myers JW, Gilmore BA, Powers KA, Kim PJ, Attinger CE. The utility of the surgical safety checklist for wound patients. Int Wound J 2016; 13(5):848-53.
- ISO 9241-210. Ergonomics of Human-System Interaction - Part 210: Human-Centered Design for Interactive Systems. International Organization for Standardization 2010.
- Quesenbery W. Balancing the 5Es: Usability. Cutter IT Journal 2004; 17(2):4-11.
- Barnum CM. Usability testing essentials: Ready, set… test! Burlington, VT: Elsevier Inc.; 2011.
- Saaranen-Kauppinen A, Puusniekka A [Internet]. Kyllääntyminen [Saturation]. [2022 Aug 13]. Available at https://www.fsd.tuni.fi/menetelmaopetus/kvali/L6_2_2.html
- Farmer EA, Page G. A practical guide to assessing clinical decision-making skills using the key features approach. Med Educ 2005; 39(12):1188-94.
- Page G, Bordage G. The Medical Council of Canada’s key features project: A more valid written examination of clinical decision-making skills. Acad Med 1995; 70(2):104-10.
- Tuomi J, Sarajärvi A. Laadullinen tutkimus ja sisällönanalyysi [Qualitative reseach and content analysis]. Helsinki: Kustannusosakeyhtiö Tammi; 2018.
- Interaction Design Foundation [Internet]. Gamification. [2021 Dec 6]. Available at https://www.interaction-design.org/literature/topics/gamification
- Shaw R, Ramachandra V, Lucas N, Robinson N. Management essentials for doctors. Cambridge: Cambridge University Press; 2011.
- Sarcevic A, Rosen BJ, Kulp LJ, Marsic I, Burd RS. Design challenges in converting a paper checklist to digital format for dynamic medical settings. International Conference on Pervasive Computing Technologies for Healthcare; 2016 16th – 19th May: Cancun: p.33-40.
- Nielsen J [Internet]. Usability 101: Introduction to usability. [2012 Jan 3;2021 May 3]. Available at https://www.nngroup.com/articles/usability-101-introduction-to-usability/
- Nielsen J [Internet]. Why you only need to test with 5 users. [2000 Mar 18;2022 Feb 9]. Available at https://www.nngroup.com/articles/why-you-only-need-to-test-with-5-users/
