Volume 24 Number 2
Organisation of NPWT in primary care in Europe – a descriptive survey
Ami Fagerdahl
Keywords negative pressure wound therapy, wounds, Wound care, wound management, primary care
For referencing Fagerdahl A. Organisation of NPWT in primary care in Europe – a descriptive survey. Journal of Wound Management 2023;24(2):3-5.
DOI
https://doi.org/10.35279/jowm2023.24.02.03
Submitted 23 January 2023
Accepted 4 May 2023
Abstract
Background Through recent years there has been a shift from inpatient hospital care out to primary care in a home care setting for many patients with different diseases and conditions. This ongoing transition for more primary care-based treatments in general has also been the case for wound treatment with negative pressure wound therapy (NPWT).
Aim To get an overview of the current organisation of NPWT in primary care in different European countries
Method An electronic survey was sent to 53 cooperating organisations of the European Wound Management Association (EWMA) in 35 countries in Europe.
Results In total, representatives from 32 EWMA cooperation organisations in 22 different European countries answered the survey. In 95% of the countries NPWT was used in primary care (n=21); only one country stated that the treatment was not used in primary care at all. The treatment was most commonly initiated from the hospital who prescribes it, and they were also then responsible for the treatment (63%).
Conclusion NPWT in primary care is used, organised, monitored and financed differently in different European countries. The general perception is that treatment with NPWT in primary care is limited and could and should be increased.
Key messages
- Negative pressure wound therapy (NPWT) in primary care is used, organised, monitored and financed differently in different European countries.
- The general perception is that treatment with NPWT in primary care is limited and could and should be increased.
Introduction
In recent years, there has been a shift from inpatient hospital care to primary care delivered in a home care setting for many patients with a variety of diseases and conditions1. Primary care is defined by the Institute of Medicine2 as:
... the provision of integrated, accessible health care services by clinicians who are accountable for addressing a large majority of personal health care needs, developing a sustained partnership with patients, and practicing in the context of family and community.
In this definition, primary care includes all healthcare provided to patients outside a hospital, or in collaboration with a hospital but performed in the patient’s home or community.
Wound treatment with negative pressure wound therapy (NPWT) has been used in clinical practice since the 1990s in a wide range of wound aetiologies3. When NPWT was first recognised as an established treatment method, patients were cared for mainly in inpatient hospital settings; the ongoing transition to more primary care-based treatments in general has included NPWT. The aim of this survey was to get an overview of the current organisation of NPWT in primary care throughout Europe.
Methods
An electronic survey was sent in June 2022 to both the European Wound Management Association (EWMA) cooperating organisation board representative, the representative appointed by each cooperating organisation, and to the president of each cooperating organisation. In some associations, these positions are held by the same person. A total of 82 recipients from 53 organisations based in 35 countries in Europe were invited to participate. A reminder was sent 2 weeks later to all recipients. A second reminder was sent after an additional 2 weeks to 37 recipients who had not responded to the first two emails.
The survey contained eight questions with set possible answers. Each question was followed by a free response question to allow respondents to elaborate on their answers. The initial two questions were demographic, while the others dealt with the organisation of NPWT care, responsibilities, training, monitoring and financial aspects.
This study was conducted according to good clinical practices and the ethical principles in the Declaration of Helsinki.
Results
In total, representatives from 32 EWMA cooperating organisations in 22 countries distributed throughout Europe responded to the survey (Table 1), accounting for 60% of the EWMA cooperating organisations. The results are summarised in Table 2. In 95% of the countries, NPWT was used in primary care (n=21); only one country representative stated that the treatment was not used in primary care at all. Many countries’ representatives said that the use of NPWT in primary care was limited but could and should be used more extensively at that care level.
Table 1. Geographical distribution of representatives (n=32)
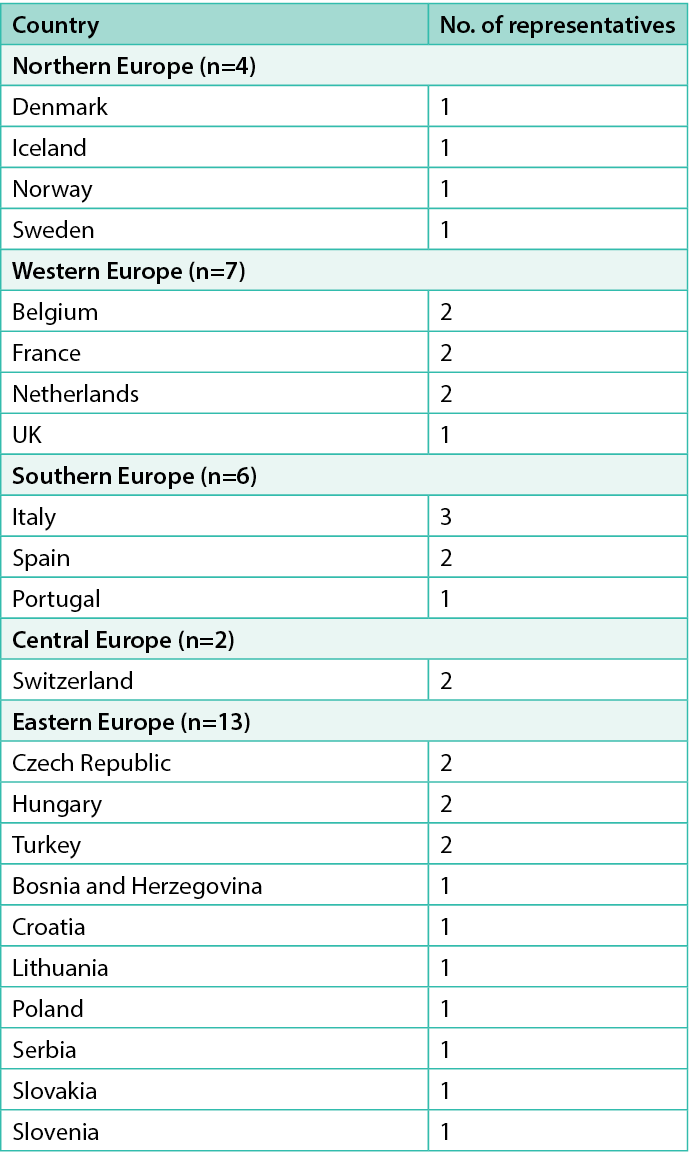
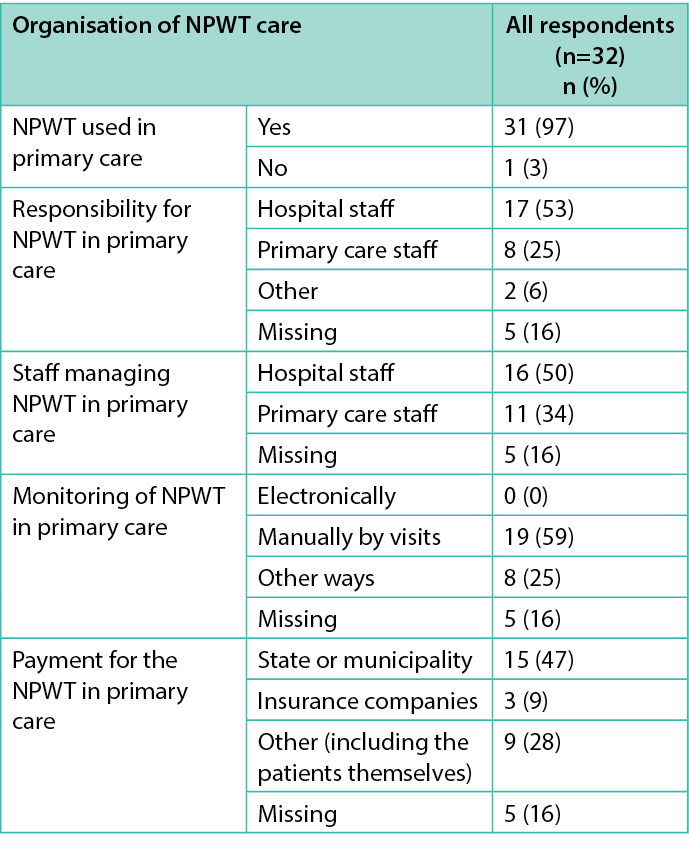
Table 2. Overview of the organisation of NPWT in European countries
Treatment organisation
The most common description of NPWT organisation in primary care was that the treatment is initiated by the hospital prescribing it, and that the hospital is also responsible for providing the treatment (63%). In some cases, the primary care efforts continue the care prescribed by a hospital and takes over the responsibility, but this scenario only seems to be occurring in a few countries.
Regarding management of the treatment and dressing changes, 59% of the respondents stated that this was done by the hospital staff, and in 41% of cases by primary care staff; thus, in the most common cases, the treatment was performed by staff members who had the required competence and skills for the task, irrelevant of care level. Some primary care nurses were trained to manage the treatment before discharge from the hospital, thus allowing the treatment to continue in primary care instead of necessitating an extended hospital stay.
Educational aspects of staff-managed NPWT in primary care
The descriptions of training requirements for staff performing NPWT in primary care varied. Some respondents described formal training as non-existent, but instead reliant upon the individual staff members’ experience and bedside teaching amongst colleagues, while others reported that the staff received education from the manufacturers of the NPWT systems they used. There were also descriptions of more extensive staff training with regular follow-up and continuous learning. Several respondents mentioned online learning tools and digital learning platforms. Despite the lack of formal educational guidelines for managing NPWT in primary care, almost all respondents stated that there was some type of informal and local training for all staff involved in delivering the treatment.
Treatment monitoring of NPWT in primary care
The most common way to monitor NPWT in primary care was, by far, manually during visits. Some respondents noted that the patients were informed about troubleshooting and self-management of the device, including how and when to contact the caregiver if experiencing difficulties; for example, Iceland has a phone number for the patients to call, day or night, if problems occur.
No respondents reported that monitoring was performed mostly electronically, though in Denmark and France, which are countries at the forefront of telemedicine, the possibility of using this form of monitoring is available and used occasionally.
Financial issues regarding treatment with NPWT in primary care
Regarding the question of who pays for the treatment, the answers varied and, in many cases, depended on the healthcare system of the country in question. In the majority of countries, financial issues related to the treatment were handled by the state or municipality. In some, NPWT costs are covered by private health insurance. Without insurance, the treatment is sometimes financed by the national healthcare system, or the patients must pay for it themselves. A few respondents stated that NPWT in primary care is solely patient-financed and not covered by insurance or the healthcare system.
Discussion
The shift from inpatient care to primary care in a home setting is increasing, as is the case for NPWT. NPWT in outpatient settings has been shown to be more cost effective and associated with lower costs than treatments delivered in a hospital4–6.
This study shows that there is a consensus across Europe that the use of NPWT in primary care is limited but could and should be expanded. Still, there are some challenges. For example, there are major differences among European countries regarding the financing of healthcare, its organisation and structure7. This was also seen in the descriptions in this survey of how NPWT in primary care is organised and by whom it is performed. When looking at the education levels of nurses and healthcare personnel managing wound care, there are great differences from one country to the next. There is a particular lack of coordination of regulations regarding specialist nursing education; there are also differences in academic levels, duration of education and agreement on the role and independence afforded to caregivers among European countries and even within countries8. Wound care in home settings is also often performed by informal caregivers, often a relative, or staff members in different domestic positions without nursing or healthcare education1. These organisational and educational differences make it difficult to establish a common approach to advanced wound treatment, such as NPWT, in primary care, which is another of the results highlighted in this survey.
Developing European guidelines for organisation and minimum recommendation concerning the knowledge and skills needed for healthcare personnel managing NPWT in primary care could be a way to enhance the use of this treatment method in an outpatient setting. This is of importance from both economic and societal perspectives, as they could be rendered more cost-effective4–6, and because research shows that it can be an advantage and beneficial for patients to be treated at home5,9.
Limitations
One limitation of the study to consider may be the use of representatives from the different associations as the sample. Their answers may not be completely representative of the entire country due to the possibility of different healthcare organisations in different regions within the country. However, the aim of this study was to get an overview and examples of the organisation of NPWT in primary care, not to compare the healthcare organisations among countries.
Conclusion
NPWT in primary care is used, organised, monitored and financed differently across Europe. The most common way to manage the treatment in primary care is as a prescription from a hospital, which is also responsible for performing, monitoring and financing the treatment in an outpatient setting. The general perception is that NPWT in primary care is limited at present but could and should be expanded.
Conflict of interest
The authors declare no conflicts of interest.
Funding
The authors received no funding for this study.
Author(s)
Ami Fagerdahl* RN
Department of Clinical Science and Education, Södersjukhuset, Karolinska Institutet, Stockholm, Sweden
Wound Centre, Södersjukhuset, AB, Sjukhusbacken 10, Stockholm, Sweden
*Corresponding author email ami.fagerdahl@ki.se
References
- Probst S, Seppänen S, Gerber V, Hopkins A, Rimdeika R, Gethin G. EWMA Document: home care-wound care: overview, challenges and perspectives. J Wound Care 2014;23(Suppl 5a):S1–41.
- Institute of Medicine Committee on the Future of Primary Care. In: Donaldson MS, Yordy KD, Lohr KN, Vanselow NA, editors. Primary care: America’s health in a new era. Washington, DC: National Academies Press; 1996.
- Apelqvist J, Willy C, Fagerdahl AM, Fraccalvieri M, Malmsjö M, Piaggesi A, et al. EWMA document: negative pressure wound therapy. J Wound Care 2017;26(Sup3):S1–154.
- Dowsett C, Davis L, Henderson V, Searle R. The economic benefits of negative pressure wound therapy in community-based wound care in the NHS. Int Wound J 2012;9(5):544–52.
- Santosa KB, Keane AM, Keller M, Olsen MA, Sears ED, Snyder-Warwick AK. Inpatient versus outpatient management of negative pressure wound therapy in pediatric patients. J Surg Res 2020;254:197–205.
- Stryja J, Staffa R, Říha D, Stryjová K, Nicielniková K. Cost-effectiveness of negative pressure wound therapy in outpatient setting. Rozhl Chir 2015;94(8):322–8.
- Myndigheten för vård- och omsorgsanalys. Primärvården i Europa. En översikt av finansiering, struktur och måluppfyllelse [Primary care in Europe. An overview of financing, structure and goal completion]. Stockholm: Vårdanalys; 2017.
- Tiliander A, Olsson C, Kalèn S, Ponzer SS, Fagerdahl AM. Factors affecting nurses’ decision to undergo a specialist education and to choose a specialty. Nurs Open 2023;10(1):252–63.
- Monsen C, Acosta S, Kumlien C. Patients’ experiences of negative pressure wound therapy at home for the treatment of deep perivascular groin infection after vascular surgery. J Clin Nurs 2017;26(9–10):1405–13.
