Volume 25 Number 2
Critical analysis on the consensus document on current advances in risk assessment, prevention, and treatment of skin tears
Carmen Elena Ruiz Henao, Santiago Roviralta Gómez
Keywords skin tears, Hypodermis, layers skin, subcutaneous hematoma, universalisation of definition skin tears
For referencing Henao CER, Gómez SR. Critical analysis on the consensus document on current advances in risk assessment, prevention, and treatment of skin tears. Journal of Wound Management 2024;25(2):72-76.
DOI
10.35279/jowm2024.25.02.08
Submitted 25 February 2024
Accepted 16 May 2024
Key messages
- Skin tears or cutaneous tears are not considered a specific lesion.
- Subcutaneous hematoma, as part of the injury, must be treated as quickly as possible.
- Lack of universalisation of definition is the main reason why they are not adequately diagnosed.
Should the concept of tears be extended to subcutaneous cellular tissue?
Here, we present a critical analysis the International Skin Tear Panel (ISTAP)1 consensus document in which skin tears are incompletely defined, as it does not include all the layers of the skin (the hypodermis is excluded). We would like to declare that as not all tears have the same morphology in terms of depth and tissue structure, depending on the direction and on the intensity of the direct trauma, they do not have the same therapeutic approach.2 Tears developed in the upper layers of the skin, epidermis and dermis, referred as ‘skin tears’ by the ISTAP, would be considered mild skin tears. As this is a consensus document, superficial tears should not be included in a way that excludes consideration of more serious tears. Since skin tears vary according to the intensity of the trauma, it is expected they also affect the deepest layer of the skin, and even compromise the fascia. This is the reason, we believe the subcutaneous cellular tissue should be included in the consensus document, leading to a more comprehensive understanding of the degree of the skin layers’ involvement, as well as any adverse events that may occur including bleeding and the subsequent formation of hematomas.
We consider that a skin tear is not a specific lesion; rather it should be included in the definition of ‘skin lacerations’ (up to the hypodermis) to differentiate it from lacerations in different anatomical sites (such as muscles, tendons or nerves). Because these skin lacerations can affect both superficial and deep structures, they are referred to by some authors2 as suprafascial and subfascial2 avulsions.
Should we take into account the line or direction of the traumatic flap of the tears?
This type of traumatic injury can be due to shearing, bruising, friction, or adhesive removal, and occurs more frequently in patients with skin fragility due to photoaging.1,4,5
Skin lacerations do not have a uniform line, that is, they are not completely horizontal. Figures 1 and 2 shows that many of them are oblique.
In clinical practice is common to see, a traumatic oblique skin flap compromised and reaching the hypodermis, in semicircular shape or ‘V’ shape (see Figure 3).
The appearance may not adequately reflect the degree of force used to cause the injury4; for example, elderly people (especially those taking systemic steroids or anticoagulant) develop senile ecchymosis all over their bodies, but especially on the extremities. They are known to occur with little force, and even spontaneously because of thinning of the perivascular connective tissue.5
Are the different layers of skin in the traumatic skin flap correctly identified?
It is essential to classify the thickness of the traumatic skin flap, to be aware of the compromised layers. If they are very thin, when repositioned they will maintain a morphology like a partial skin graft (Figure 4a (i and ii). In cases of thick traumatic skin flaps, we may be faced with a skin flap called a random pattern flap6, or, on the contrary, a skin perforator6 (as shown in Figure 1b and 4b (i and ii)), which partially or totally preserves the viability of the avulsed skin.
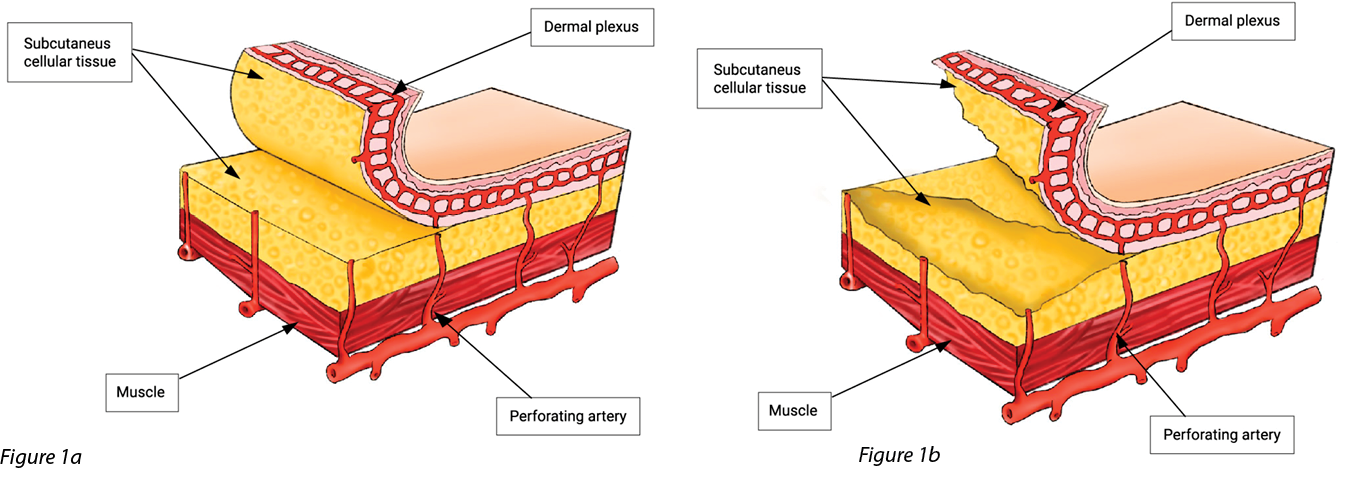
Figure 1. Line or direction of the traumatic flap of the tears: 1a) Horizontal tear. 1b) Oblique tear (including subcutaneous cellular tissue
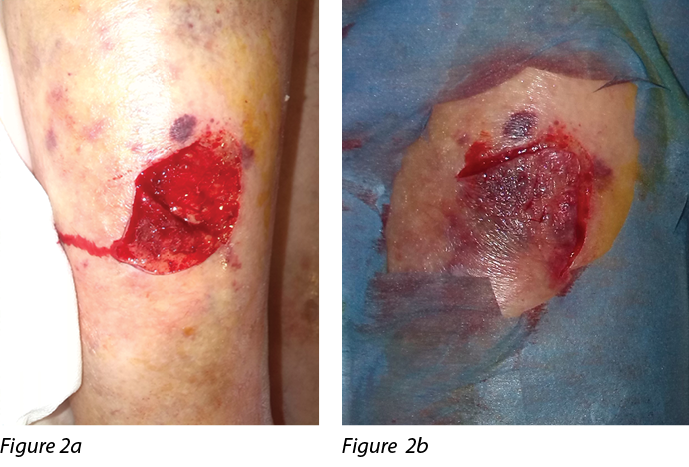
Figure 2. Pretibial laceration with oblique involvement: 2a) The edge of the flap is superficial. 2b) The flap is repositioned in its bed. Photos are from our clinic, used with permission.
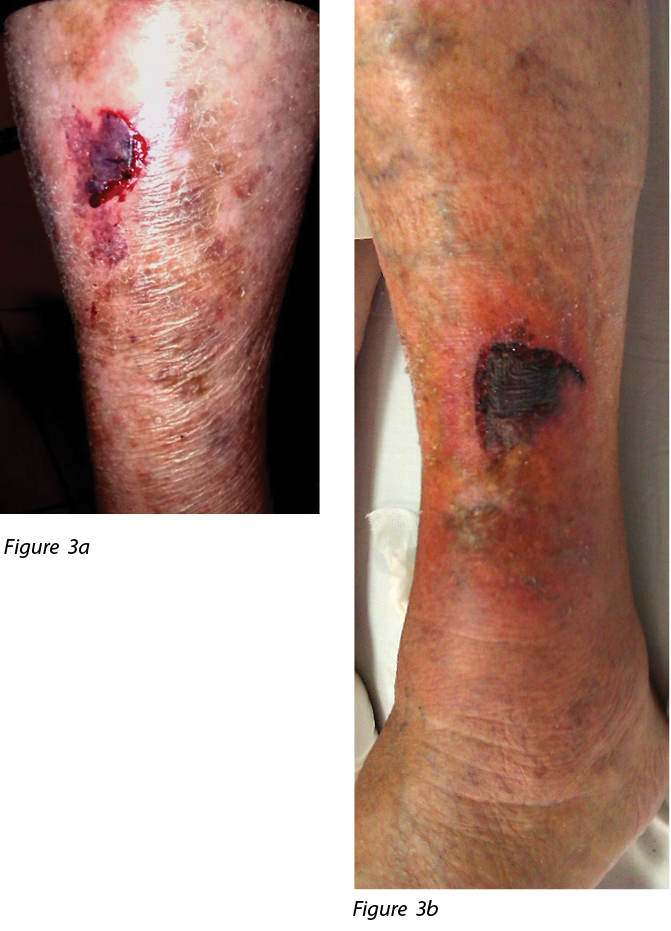
Figure 3. Shapres of traumatic oblique skin flaps reaching the hypodermis. 3a) Semicircular shape. 3B) A ‘V’ shape.
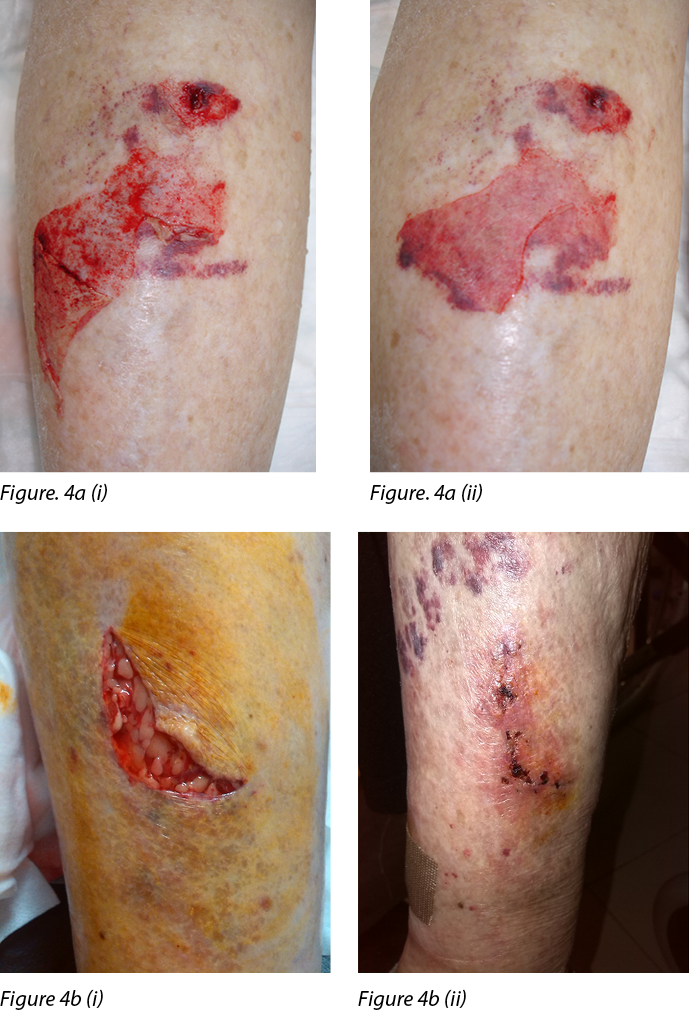
Figure 4. Thickness of traumatic skin flaps
It is fundamental to know the difference between normal tissue morphology and traumatic injuries. If the skin consists of three layers as described by Van Tinglen7 and other authors,7,8 involvement of the hypodermis should be part of the classification of skin tears or lacerations. Let us not forget that in its thickness we can also detect hair follicles, sensory nerves, and blood vessels.9 The subcutaneous cellular tissue is below the reticular dermis, without a defined limit. However, this loose areolar tissue, with its fibers is attached to those of the dermis, forming anchor points; also fixing the skin to the underlying structures (fascia, periosteum, or perichondrium).10 The extreme atrophy of the epidermis and dermis associated with fat thinning due to aging causes the subcutaneous vessels to come into close contact with the more superficial layers.10 Saurat et al3 and Kaya et al11 describe lacerations (and not tears) as stage II and III dermatoporosis.
Beldon12 reports that Dunkin et al proposed the classification of pretibial injuries, along with an algorithm for their management. The classification was similar to that Payne and Martin12,13 for skin tears, but included larger tears. According to Dunkin’s classification,12,14,15 pretibial lacerations, or type 1 and 2 skin tears (shown in Figure 5;5a,5b), should be treated conservatively, as corroborated by Lo et al1 and Singh et al.16 However, type 3 and 4 injuries (shown in Figure 5;5c,5d) should be referred to emergency services,15,16 and subsequently treated in a mixed way, in order to reduce hospital time, by performing ambulatory cures, and defining appropriate treatments according to their evolution.
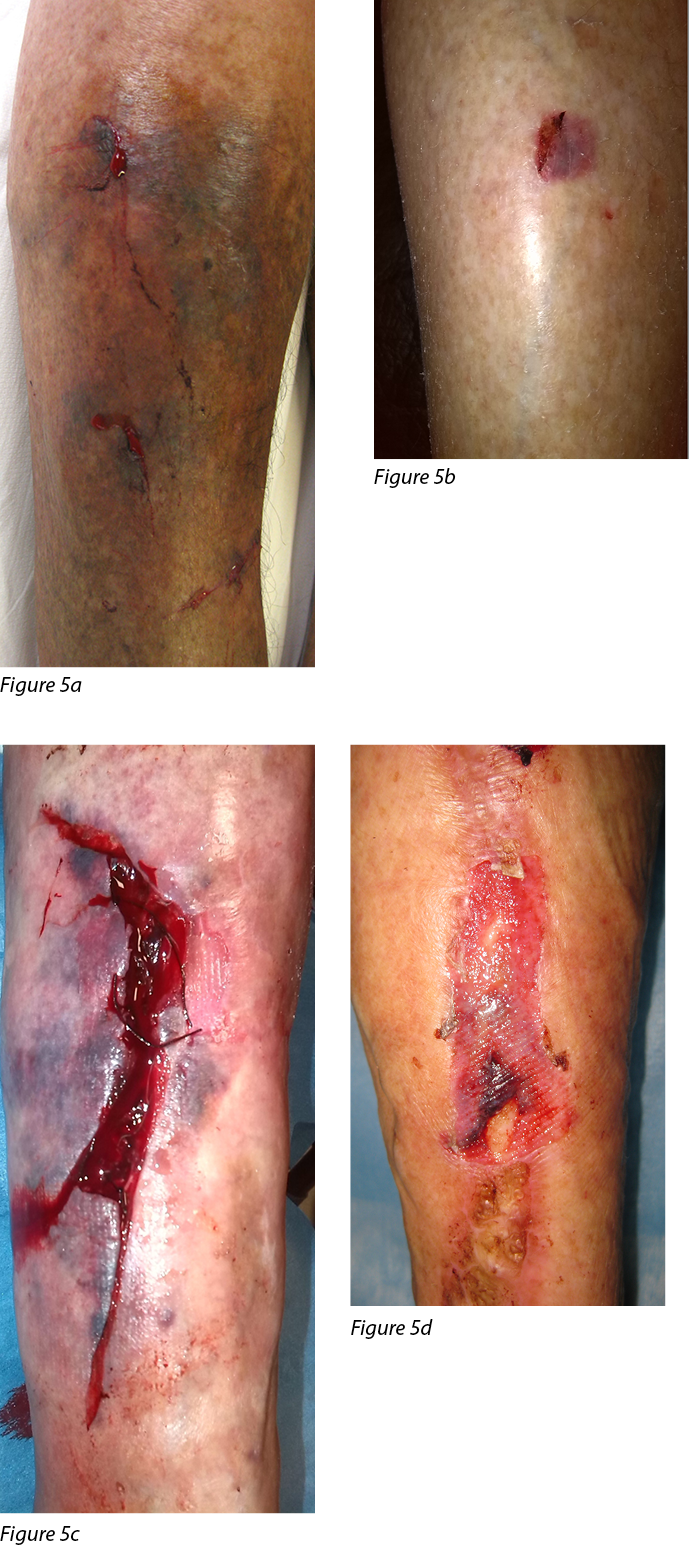
Figure 5. Classification of pretibial lacerations. 5a) Type 1. 5b) Type 2. 5c) Type 3. 5d) Type 4
Hematomas are they part of skin tears or a complication?
We would also like to refer to the vascular anatomy of the skin layers and, subsequently, the clinical manifestations of vessel extravasation, according to intensity. Subcutaneous hemorrhages are referred to vaguely in various sections of the consensus, with terms such as dermal hemorrhages. Figure 6 shows the irrigation of the skin system.17
According to dermatological semiology, there are lesions due to blood extravasation caused by minor traumas and favoured by previous skin lesions caused by aging, called macules.18 They are dermal infiltrates that do not form collections. They may be red (more superficial) and blue (deep), and they do not disappear with vitropressure (diascopy). These lesions are distinguished19 as
Petechiae: Pinpoint and isolated extravasation. Macules ≤ 4 mm (Fig. 7)
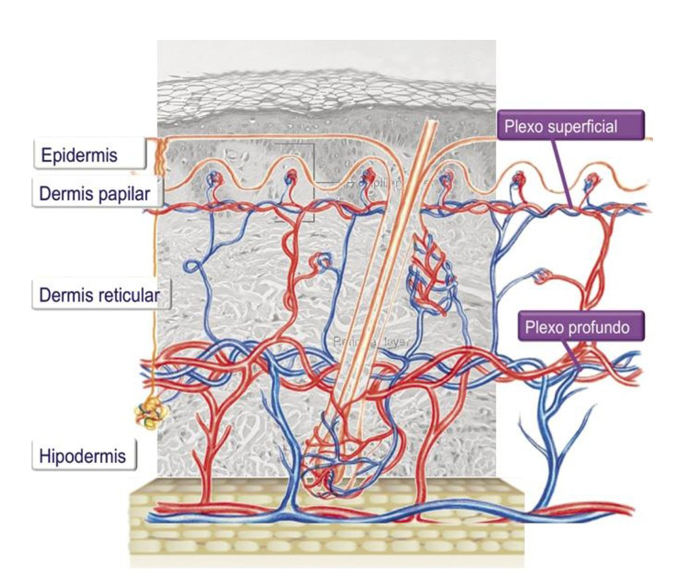
Figure 6. Skin vascular network: Superficial and deep plex; the subcutaneous plex is also seen (Image used with authorization).10
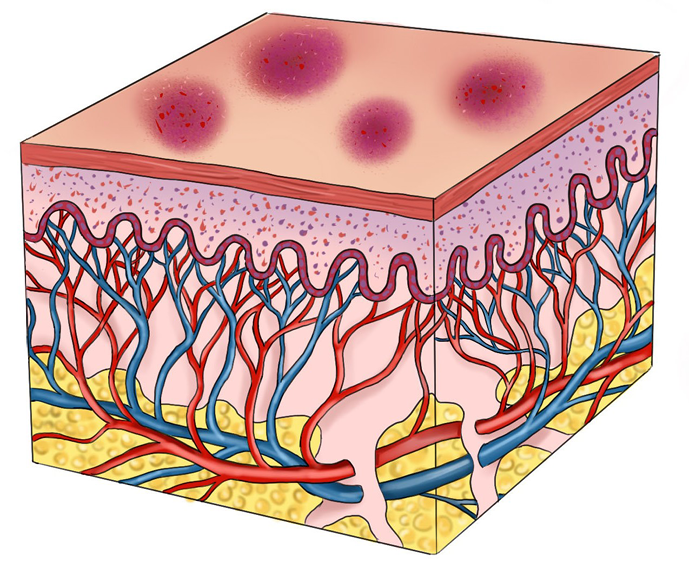
Figure 7. Petequia
Purpura: Small extravasations that densely and symmetrically cover relatively large areas. They can be Macular: intradermal extravasations; or Papular, involving inflammation of the vascular wall and 5–10mm in size (Figure 8).
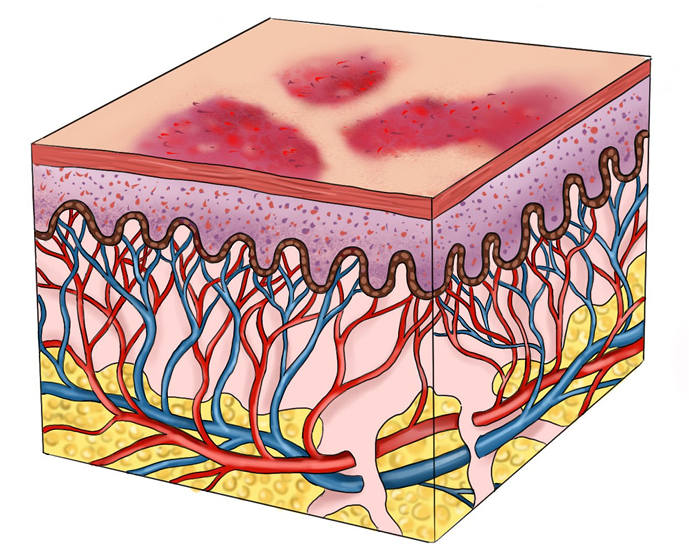
Figure 8. Purpura
Ecchymosis: Extravasation that affects extensive areas, in the form of plate, >1 cm in diameter. Colloquially, it is called bruising (Figure 9).
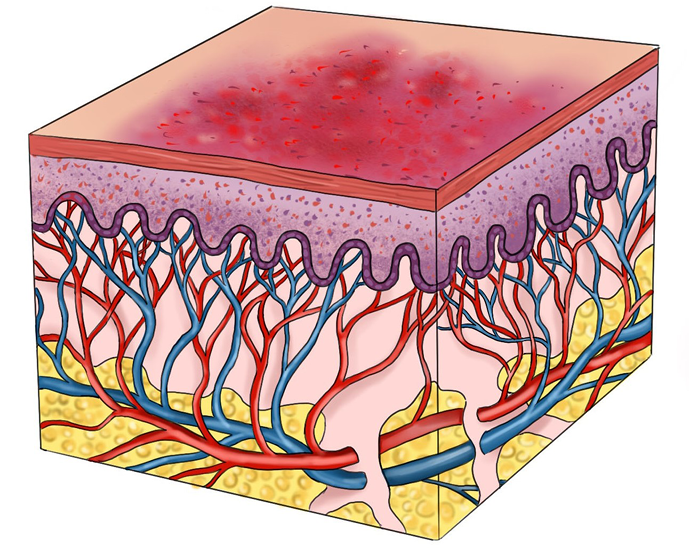
Figure 9. Ecchymosis
Hematoma: Massive extravasations in the form of a cumulus or tumor (Figure 10). The vessels may continue to bleed for some time after the hematoma occurs during the first 24–48 hours.20 Hematomas, depending on the size and depth, are not always palpable. They may be the product of ruptured capillaries in the subpapillary plexus, a vessel in the dermis, or subcutaneous cell tissue. When the subpapillary plexus ruptures, it can form a small subepidermal or intradermal hematoma.
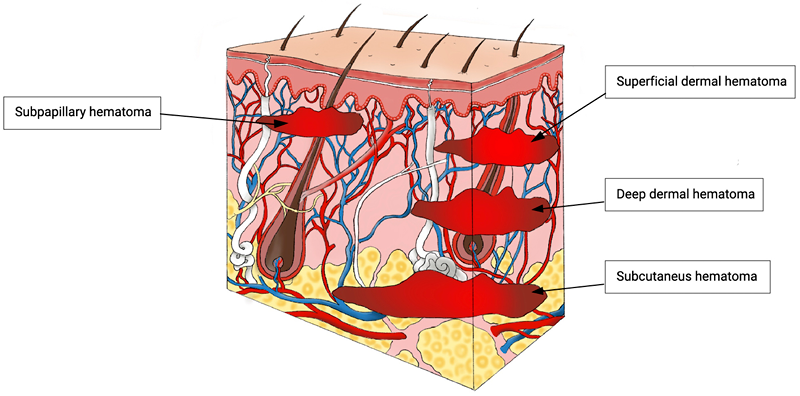
Figure 10. Potential origin sites of hematoma in the skin
Conclusion
Given that ISTAP does not consider the hypodermis in its skin tears classification,1 we conclude that skin tears must correspond to suprafascial avulsive skin lacerations.2 Therefore, we propose this definition should be revised and should include the term skin lacerations, since they compromise all of the skin.
Furthermore, the classification should not only analyse whether there is a skin flap or not, but also define its line or direction, as well as its thickness.
The presence of a hematoma should also be considered, which is derived from the rupture of the vascular plexuses, and it is an entity which should be described as part of the injury and treated as quickly as possible, due to the complications that they may cause.
The morphological and conceptual terms still need to be clarified, as well as reaching a consensus in the translation of terms from English to Spanish and other languages, evaluating whether the concepts are similar. Many times, we accept terms when we have never questioned if they are totally accurate!
Discussion
The lack of universal coding is perhaps the main reason why these lesions are not adequately diagnosed. The daily management of traumatic wounds entails providing a diagnosis according to their anatomical and clinical description. Subsequently, in practice, the WHO global coding system should be applied (ICD 9, ICD 10, or ICD 11 depending on the institution or country). However, if within these codes the types of injuries are not specified according to the anatomical site affected and only a general term appears, for example: “open wounds - complicated or not”, or the type of laceration is not identified, such as skin, this can constitute a barrier to future studies.
Conflict of Interest
The authors declare no conflicts of interest.
Funding
The authors received no funding for this study.
Author(s)
Carmen Elena Ruiz Henao*1, Santiago Roviralta Gómez2
1MD. MSc in deterioration of skin integrity, ulcers and wounds. FREMAP. Burela (Lugo-Spain)
2Nurse coordinator. M.Sc in deterioration of skin integrity, ulcers and wounds. Ribadeo Primary Care Service, Ribadeo (Lugo-Spain)
*Corresponding author email ruizhenaoc@yahoo.es
References
- Van Tiggelen H, Beeckman D. Skin tears anno 2022: An update on definition, epidemiology, classification, aetiology, prevention, and treatment. J Wound Managment. 2022;23(2):38-51. doi:10.35279/jowm2022.23.02.09
- Henao CER, Gómez SR. Revisión narrativa:¿Laceraciones pretibiales, avulsiones o desgarros cutáneos? J Wound Care. 2020. Oct 1;29(LatAm Sup2):35–39.
- Saurat JH, Mengeaud V, Georgescu V, Coutanceau C, Ezzedine K, Taïeb C. A simple self-diagnosis tool to assess the prevalence of dermatoporosis in France. J Eur Acad Dermatol Venereol. 2017;31(8):1380–1386.
- Dolinak D, Matshes EW, Lew EO. Forensic Pathology: principles and practice.1st ed. Elsevier. 2005.
- Schwartz RA. Actinic Púrpura. Updated: Apr 07, 2021. Available from: https://emedicine.medscape.com/article/1087008-overview.
- Thorne CH, Chung KC, Gosain AK, et al. Grabb and Smith´s Plastic Surgery. 7th ed. Wolters Kluwer. 2014.
- Van Tiggelen H. Skin tears: Epidemiology, classification and measurement. PhD thesis Ghent University. 2022. Available from: htps://biblio.ugent.be/publication/8751140.
- Navarrete Franco G. Histología de la piel. Rev Fac Med UNAM. 2003. Julio-Agosto;46 (4):130–133.
- Buendía Eisman A, Mazuecos Blanca J, Camacho Martínez FM. Sección I: Temas generales. Capítulo 1. Anatomía y fisiología de la piel. In: Editor: Conejo-Mir J, Moreno JC, F. M. Camacho FM, Manual de Dermatología. Grupo Aula Medica. 2018:2–27. Available from: https://www.berri.es/pdf/MANUAL%20DE%20DERMATOLOGIA%E2%80%9A%202%20Vols.%20(Tapa%20Dura)/9788478856282
- García Dorado J, Alonso Fraile P. Pediatría Integral. Pediatra Integral 2021; 25(3):156e1–e13
- Kaya G, Jacobs F, Prins C, Viero D, Kaya A, Saurat JH. Deep dissecting hematoma: an emerging severe complication of dermatoporosis. Arch Dermatol. 2008 Oct;144(10):1303–1308.
- Beldon P. Classifying and managing pretibial lacerations in older people. Br J Nurs. 2008;17(Sup 5):4–18.
- Payne RL, Martin ML. Defining and classifying skin tears: need for a common language. Ostomy Wound Manage. 1993. Jun;39(5):16–20, 22–24, 26.
- Dunkin CS, Elfleet D, Ling C, Brown TP. A step-by-step guide to classifying and managing pretibial injuries. J Wound Care. 2003 Mar;12(3):109–111.
- Lo S, Hallam MJ, Smith S, Cubison T. The tertiary management of pretibial lacerations. J Plast Reconstr Aesthet Surg. 2012. Sep;65(9):1143–1150.
- Singh P, Khatib M, Elfaki A, Hachach-Haram N, Singh E, Wallace D. The management of pretibial lacerations. Ann R Coll Surg Eng. 2017;99(8):637–640.
- Reto Wettstein R, Erni D. Basic anatomical principles and functions of soft tissue and bone. In: Volgas D et al, 1st ed. Manual of Soft-Tissue Management in Orthopaedic Trauma, Theime. 2011, Chapter 2. doi:10.1055/b-0034-84272
- Braun- Falco O, Plewig G, Wolff HH, Winkelmann RK. Dermatology. Springer-Verlag Ibérica. 1991.
- Ball JW, Dains JE, Flynn JA, Solomon BS, Stewart RW. Examen de la piel. Púrpuras, 7 tipos de lesiones y sus causas. Guía Seidel de exploración física. 9 editions. Ed. Paises Bajos.Elsevier. 2019.
- Randeberg LL, Winnem AM, Langlois NE, Larsen EL, Haaverstad R, Skallerud B, Haugen OA, Svaasand LO. Skin changes following minor trauma. Lasers Surg Med. 2007;39(5):403–413.
