Volume 16 Number 1
Challenges facing the renal nursing workforce
Kathy Hill and Melissa Arnold-Chamney
For referencing Hill K & Arnold-Chamney M. Challenges facing the renal nursing workforce. Renal Society of Australasia Journal 2020; 16(1):4-5.
DOI https://doi.org/10.33235/rsaj.16.1.4-5
There has been extensive research investigating stress in the nursing workforce, known as a ‘caring’ occupation, to assess the impact of the emotional labour of caring. Most of the recent evidence cites increasing nursing workloads contributing to the phenomenon of nursing stress, and this is widely predicted to continue to increase. The current shortage in the renal nursing workforce has largely been considered a ‘subset of overall supply’; however, with hundreds of registered nurse (RN) vacancies in renal globally, as well as increases in population level end stage kidney disease (ESKD), the renal specialty is under additional pressure (Wolfe, 2014).
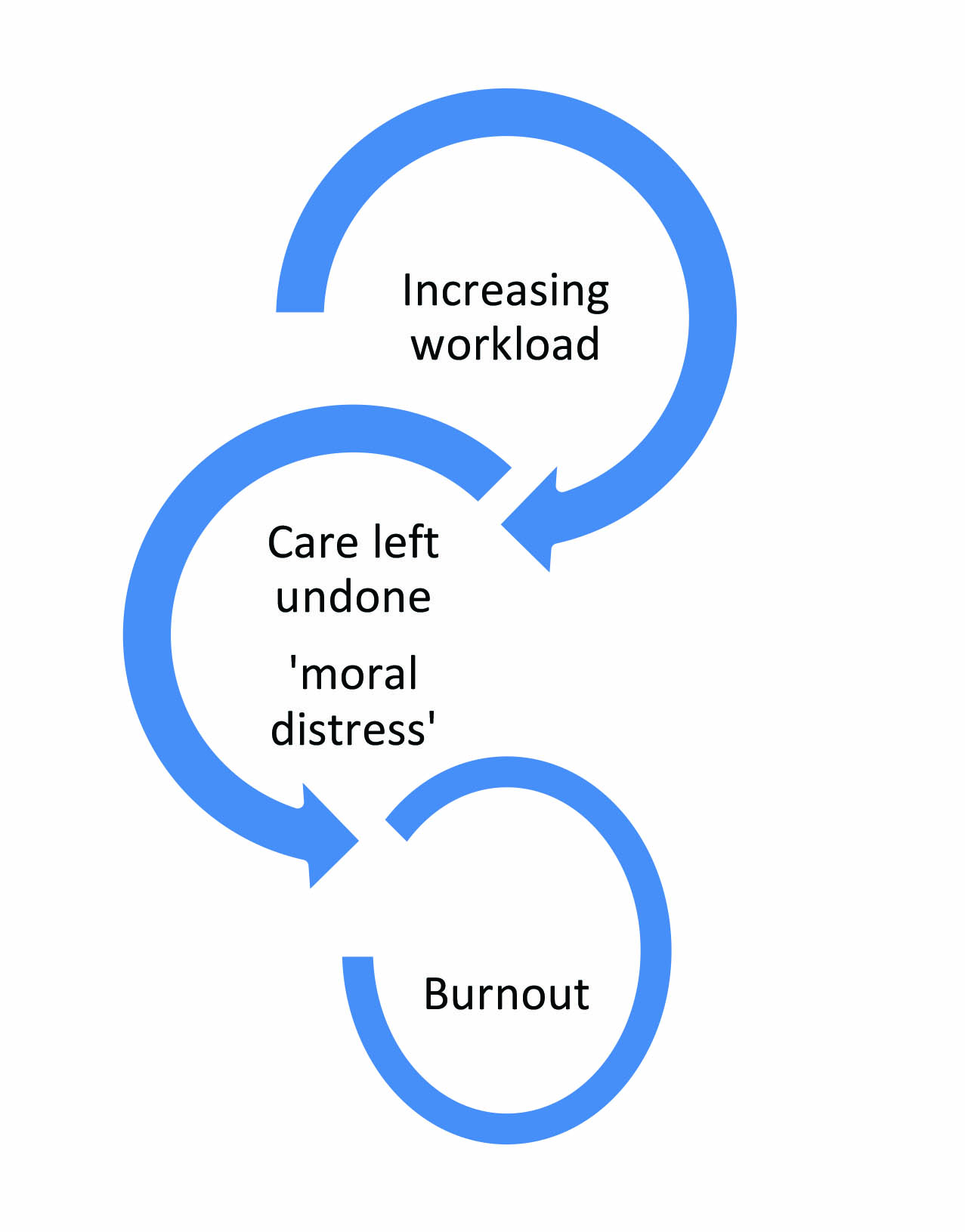
Whilst intrinsic factors can reduce the impact of stress and burnout, critical to supporting nurses to cope with stress is addressing the external environment with adequate staffing, appropriate skill mix and the support to manage extremely unwell patients (Jones, 2014). White, Aiken and McHugh (2019) discuss the interdependent concepts of working in an under resourced setting creating stress and moral distress due to missed care – represented on the image on this page. However, one of the challenges in understanding and addressing the RN workload is that there is no consensus on what this actually means; for example, the level of patient dependency and complexity of care has a major impact on both nurses’ workload and the care they give (Alghamdi, 2016). There is therefore a pressing need to reassess patient acuity in renal care, particularly in dialysis patients, so that this can be used to model adequate and safe staffing levels.
It is also generally agreed that an underlying driver of high stress levels and ‘burnout’ in nursing is compassion fatigue. Cross (2019) describes a cycle of exposure to suffering, empathy, repeat exposure, compassion fatigue and, ultimately, burnout. In addition, the relatively high frequency of ‘near-death experiences’ in dialysis care, coupled with the intensity of long-term relationships between nurses and patients, increases tension in the renal workplace (Ashker, Penprase, & Salman, 2011) and also increases emotional exhaustion (Chayu & Kreitler, 2011). Nurses in renal dialysis have a unique relationship with the people that they care for given the lengthy and intensive context of care (Wolfe, 2014; Brown et al., 2013). Evidence suggests that the intensity of job burnout resulting from high stress environments is particularly high among renal nurses (Hayes, Douglas, & Bonner, 2014) and that job satisfaction and ‘organisational justice’ is a critical factor that can ameliorate the negative effects of burnout (Hayes, Douglas, & Bonner, 2015; Kavurmaci, Cantekin, & Tan, 2014). Hospital type is a dominant predictor of the quality of nursing care and nurses, being a caring profession, are drawn to organisations that address daily census with appropriate staff–patient ratios to increase the quality of care (Mudallal et al., 2017).
Professional identity is also a strong predictor of personal accomplishment and the driving force to “keep going” (Manomenidis et al., 2017) – as such, this needs constant positive reinforcement to remain high. Membership of the Renal Society of Australasia (RSA) is an important source of maintaining professional identity for renal nurses.
We also need to be mindful of the concept of ‘growing our own’ in renal nursing and developing this from the ground up, starting with the student nurses that are placed in renal clinical areas. The intensity of the workplace and emotional labour for newly graduated RNs can be overwhelming in their first year in the workforce. Bong (2019) identifies that the attrition rate for new graduates is a result of “moral distress”, a concept whereby the carer knows the right thing to do but is unable to do this due to institutional or resource constraints, both of which are compelling enough to cause staff turnover. There is therefore a pressing need to focus on the wellbeing of newly graduated RNs (Liang, Lin, & Wu, 2018). For more established staff, the reality is that the supply versus demand gap is widening, and organisational practices can result in avoidable turnover (Halter et al., 2017). As we continue to strive to promote our professional identity and the important role of the RSA, as a collective we can ‘voice’ our concerns about the sustainability of the renal nursing workforce in Australia and New Zealand. Our annual conference is also a way to join forces and to continue to promote the excellent work that we do every day in caring for people with renal disease.
We do hope you enjoy reading this issue which contains articles on a variety of topics which include a letter to the editor to raise awareness within our readership of The International Society of Nephrology, and an article on rural dialysis nurses’ experiences with challenging patients. There are two articles pertaining to peritoneal dialysis; the first article considers irrigation and whether “to flush or not to flush” a newly inserted Tenckhoff catheter postoperatively and the second article considers health related quality of life for peritoneal dialysis patients. The final article is an NEN continuing professional development one which discusses kidney transplantation and interventions to improve medication adherence.
Wishing all our readership a wonderful 2020. We look forward to what inventions and changes may occur in this new decade within renal care for our patients and also for us as renal nurses. Please do keep submitting articles to the journal so that 2020 and beyond is another great year for our readership.
Author(s)
Kathy Hill
University of South Australia
Email Kathy.Hill@unisa.edu.au
Melissa Arnold-Chamney
The University of Adelaide, SA, Australia
Email melissa.arnold-chamney@adelaide.edu.au
References
Alghamdi, M.G. (2016). Nursing workload: A concept analysis. Journal of Nursing Management, 24.
Ashker, V. E., Penprase, B., & Salman, A. (2012). Work-related emotional stressors and coping strategies that affect the well-being of nurses working in hemodialysis units. Nephrology Nursing Journal, 39(3), 231–236.
Bong, H.E. (2019). Understanding moral distress: How to decrease turnover rates of new graduate pediatric nurses (Continuing Nursing Education). Pediatric Nursing, 45(3), 109.
Brown, S., Bain, P., Broderick, P., & Sully, M. (2013). Emotional effort and perceived support in renal nursing: A comparative interview study. Journal of Renal Care, 39(4), 246–255.
Chayu, T., & Kreitler, S. (2011). Burnout in nephrology nurses in Israel. Nephrology Nursing Journal: Journal of the American Nephrology Nurses’ Association, 38(1), 65–77.
Cross, L.A. (2019). Compassion fatigue in palliative care nursing: A concept analysis. Journal of Hospice and Palliative Nursing, 21(1), 21–28.
Halter, M. et al. (2017). The determinants and consequences of adult nursing staff turnover: A systematic review of systematic reviews. BMC Health Services Research, 17(1).
Hayes, B., Douglas, B., & Bonner, A. (2015). Work environment, job satisfaction, stress and burnout among haemodialysis nurses. Journal of Nursing Management, 23, 588–598.
Hayes, B., Douglas, B., & Bonner, A. (2014). Predicting emotional exhaustion among haemodialysis nurses: A structural equation model using Kanter’s structural empowerment theory. Journal of Advanced Nursing, 70(12), 2897–2909.
Jones, C. (2014). Stress and coping strategies in renal staff. Nursing Times, 110(10), 22–25.
Kavurmaci, M., Cantekin, I., & Tan, M. (2014). Burnout levels of hemodialysis nurses. Renal Failure, 36(7), 1038–1042.
Liang, H.F., Lin, C., & Wu, K. (2018). Breaking through the dilemma of whether to continue nursing: Newly graduated nurses’ experiences of work challenges. Nurse Education Today, 67, 72–76.
Manomenidis, G. et al. (2017). Is self-esteem actually the protective factor of nursing burnout? International Journal of Caring Sciences, 10(3), 1348–1359.
Mudallal, R.H. et al. (2017). Quality of nursing care: The influence of work conditions, nurse characteristics and burnout. International Journal of Africa Nursing Sciences, 7, 24–30.
Wolfe, W.A. (2014). Are word-of-mouth communications contributing to a shortage of nephrology nurses? Nephrology Nursing Journal, 41(4), 371–378.
White, E.M., Aiken, l., & McHugh, M. (2019). Registered nurse burnout, job dissatisfaction, and missed care in nursing homes. Journal of the American Geriatrics Society, 67(10), 2065–2071.
