Volume 3 Issue 2
Evaluating methods for effective decontamination of central venous access devices needleless connectors in adult hospital patients: A pilot randomised control trial protocol
Julie M Flynn, Samantha Keogh, Li Zhang, Claire M Rickard,
Abstract
Background: The importance of decontaminating needleless connectors prior to accessing central venous access devices (CVADs) to prevent CVAD-associated bloodstream infection has been highlighted. However, the optimal decontamination time and solution is still under-evaluated.
Aim: This study will compare different decontamination methods of CVAD needleless connectors in adult patients. The aims of this pilot trial are: to assess recruitment feasibility, data collection strategies and proposed methods; and to test the interventions with the control to determine an adequate sample size for a future, larger clinical trial.
Design: A single-centre, parallel, pilot randomised control trial (RCT) with a superiority design.
Methods: There will be three arms: 70% isopropyl alcohol swab (control); 2.0% chlorhexidine gluconate in 70% isopropyl alcohol swab; and a 70% isopropyl alcohol-impregnated cap. The primary outcome of this pilot trial is to assess feasibility for a future, larger clinical trial. The secondary outcome is CVAD-associated bloodstream infection. In total, 120 patients will be recruited over six months with a four-week follow-up. Prospective patients who are scheduled to have a CVAD inserted will be eligible. Randomisation will be computer-generated, central and concealed until allocation. Due to the nature of the interventions it will not be possible to blind clinicians or patients.
Discussion: Preventing CVAD-associated bloodstream infection in hospitalised patients is vital. Interventional decontamination techniques that demonstrate superior performance in preventing CVAD-associated bloodstream infection would improve patient outcomes, reduce patient morbidity and mortality, and health care-associated costs.
Trial Registration: ACTRN12615001120561.
Keywords: Bloodstream infection, CABSI, central venous access device, CVAD, needleless connectors, nursing.
ACKNOWLEDGEMENTS
I wish to acknowledge the Australasian College for Infection Prevention and Control (ACIPC) and ICU Medical for their support with this project.
CONFLICT OF INTEREST STATEMENT
AVATAR, through Griffith University, has received unrestricted investigator-initiated research or educational grants from product manufacturers (3M, Adhezion, Angiodynamics, Bard, Baxter, BBraun, Becton Dickinson, Carefusion, Centurion Medical Products, Cook Medical, Entrotech, Flomedical, ICU Medical, Medtronic, Smiths Medical, Teleflex). Griffith University has received consultancy payments on CM Rickard’s behalf from manufacturers (3M, Bard, BBraun, BD, Carefusion, Mayo Healthcare, ResQDevices, Smiths Medical).
FUNDING STATEMENT
ACIPC Early Career Research Grant 2015 provided partial funding for this project. The SwabCap (ICU Medical, San Clemente, USA) was provided free of charge by ICU Medical. ACIPC and ICU Medical took no part in study design or preparation of this manuscript. The authors were fully responsible for the project design and development of this paper.
ABSTRACT
Background: The importance of decontaminating needleless connectors prior to accessing central venous access devices (CVADs) to prevent CVAD-associated bloodstream infection has been highlighted. However, the optimal decontamination time and solution is still under-evaluated.
Aim: This study will compare different decontamination methods of CVAD needleless connectors in adult patients. The aims of this pilot trial are: to assess recruitment feasibility, data collection strategies and proposed methods; and to test the interventions with the control to determine an adequate sample size for a future, larger clinical trial.
Design: A single-centre, parallel, pilot randomised control trial (RCT) with a superiority design.
Methods: There will be three arms: 70% isopropyl alcohol swab (control); 2.0% chlorhexidine gluconate in 70% isopropyl alcohol swab; and a 70% isopropyl alcohol-impregnated cap. The primary outcome of this pilot trial is to assess feasibility for a future, larger clinical trial. The secondary outcome is CVAD-associated bloodstream infection. In total, 120 patients will be recruited over six months with a four-week follow-up. Prospective patients who are scheduled to have a CVAD inserted will be eligible. Randomisation will be computer-generated, central and concealed until allocation. Due to the nature of the interventions it will not be possible to blind clinicians or patients.
Discussion: Preventing CVAD-associated bloodstream infection in hospitalised patients is vital. Interventional decontamination techniques that demonstrate superior performance in preventing CVAD-associated bloodstream infection would improve patient outcomes, reduce patient morbidity and mortality, and health care-associated costs.
Trial Registration: ACTRN12615001120561.
Keywords: Bloodstream infection, CABSI, central venous access device, CVAD, needleless connectors, nursing.
INTRODUCTION
A large number of hospital inpatients require a central venous access device (CVAD) for the administration of intravenous fluids, medications, blood products, blood sampling and specialised treatments1. CVADs are accessed by nurses via needleless connectors (NCs) multiple times every day, with NCs either connected directly to the CVAD, or to entry points on the infusion tubing. Nurses disinfect NCs before each access so as not to introduce microorganisms from the injectable surface of the NC into the bloodstream, which can lead to CVAD-associated bloodstream infection (CABSI)2. The introduction of NCs was to prevent needlestick injuries and risk of health care worker exposure to blood-borne viruses such as hepatitis, but this technology has, in some cases, coincided with an increased rate of bloodstream infections3-5. The causes of this involve connector design, patient and practice factors. This research will focus on the effective decontamination of NCs to prevent the introduction of microorganisms into the bloodstream. To our knowledge, there has been no previous randomised control trial (RCT) of NC decontamination methods.
BACKGROUND
The importance of decontaminating NCs prior to accessing CVADs is highlighted by clinical practice guidelines6,7. However, the standard for the decontamination time and the optimal decontamination solution (antiseptic) is still lacking. Some studies show a decontamination time range between 10 and 30 seconds, using friction and 70% isopropyl alcohol (IPA) swab, is required8-10. The use of chlorhexidine in alcohol for skin antisepsis has been widely tested and shown to be superior to other antiseptics prior to device insertion11-14; however, research is lacking on the effectiveness of chlorhexidine in alcohol for the decontamination of needleless connectors. An in vitro study by Flynn15 and colleagues suggested that scrubbing the needleless connector with chlorhexidine in alcohol can decrease microbial contamination of microorganisms, such as Staphylococcus aureus, but this needs to be confirmed in a clinical trial.
The Centers for Disease Control and Prevention (CDC) Guidelines for the Prevention of Intravascular Catheter-related Infections advise NC decontamination with a chlorhexidine in alcohol preparation. However, they do not mention a specific duration for this procedure, other than stating that 70% alcohol solution for 3 to 5 seconds is not adequate7. The National Evidence Based Guidelines for Preventing Healthcare Associated Infections in National Health Service Hospitals in England (Epic3) recommend NC disinfection for a minimum of 15 seconds with 2% chlorhexidine gluconate (CHG) in 70% IPA, then allowing it to dry prior to accessing the system6. The Queensland Health I-Care Guideline for Tunnelled Central Venous Catheters recommends meticulously cleaning the connector with a single-use 70% alcohol-impregnated swab, or an alcoholic CHG swab, and allowing the connector to dry before accessing the CVAD system16. With each guideline providing differing recommendations, clinicians have difficulty deciding which method is optimal.
CURRENT OPTIONS FOR THE DECONTAMINATION OF THE NEEDLELESS CONNECTOR
Seventy per cent IPA swabs are the current standard practice for the decontamination of NCs; however, there is no high-quality evidence to support this method. An alternative to the 70% IPA swab is the CHG in 70% IPA swab, which has been shown to reduce the rate of bloodstream infection in some studies17-19. In the study by Pichler18 the catheter-related bloodstream infection (CRBSI) rate per 1000 catheter days decreased from 3.1/1000 (n = 10/42) to 0.4/1000 (n = 3/50), p = 0.03, after the CHG in 70% IPA swab was introduced. Another option for NC decontamination is a single-use, 70% IPA-impregnated cap left in place on the NC in between use. Several pre-test/post-test studies20-29 have tested this method against the 70% IPA swab. All studies concluded that the IPA cap reduced the rate of bloodstream infection or contamination rates. Thus far, the CHG swab and the IPA-impregnated cap have not been tested against each other.
AIM
The aims of this pilot trial are: to assess feasibility, data collection strategies and proposed methods; and to test the interventions with the control to determine an appropriate sample size for a future, larger clinical trial.
Research questions:
- Is it feasible to conduct a full-scale RCT to compare three NC decontamination techniques in patients with a CVAD, considering eligibility, recruitment, retention, attrition, protocol compliance and missing data?
- In patients with a CVAD, is NC decontamination with CHG in 70% IPA swab (intervention 1), or 70% IPA-impregnated caps (intervention 2), compared to decontamination with 70% IPA swab (control), more effective for the prevention of CABSI?
HYPOTHESIS
Null hypothesis (HO): There will be no difference in rates of CABSI between groups
Alternative hypothesis (HA1): There will be a significantly lower rate of CABSI in the CHG in 70% IPA group compared to the control group.
Alternative hypothesis (HA2): There will be a significantly lower rate of CABSI in the 70% IPA-impregnated NC cap group compared to the control group.
DESIGN/METHODOLOGY
A parallel, single-blind, pilot RCT will be conducted in adult patients with a CVAD. The trial will have a superiority design.
SETTING/LOCATION
The study will recruit participants located in a public tertiary metropolitan hospital: the Royal Brisbane and Women’s Hospital, Queensland, Australia.
STUDY POPULATION
The study population will include any eligible adult hospitalised patient undergoing treatment that requires insertion of a peripherally inserted central catheter (PICC) or Hickman catheter (a tunnelled cuffed catheter).
ELIGIBILITY CRITERIA
Inclusion criteria:
- Patients ≥ 18 years of age.
- Requiring a CVAD to be inserted for ≥ 7 days.
- Able to provide informed consent.
Exclusion criteria:
- Current bloodstream infection within previous 48 hours.
- Non-English speaking without an interpreter.
- Previous recruitment to study in current hospital admission (only one CVAD to be studied per patient).
RECRUITMENT
On a daily basis, a research nurse will review the CVAD insertion list and liaise with the unit clinical lead to identify all potentially eligible participants hospitalised over the study period. Patients initially deemed suitable will be approached by their ward nurse to ascertain their willingness to consider participation. If agreeable, patients will then be provided with written information regarding the trial and a verbal explanation from the investigator (Figure 1). They will be given time to consider the information, opportunity to ask questions and have these answered. If patients consent, they will sign a consent form.
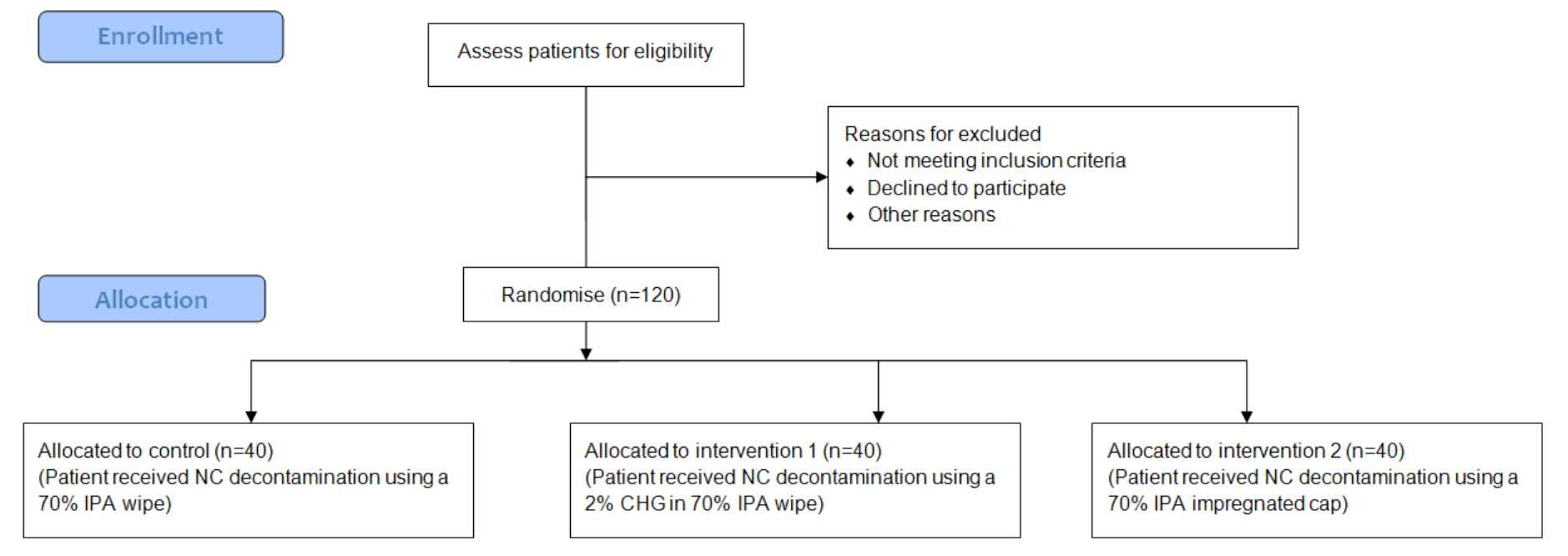
Figure 1: Recruitment flow diagram
STUDY GROUPS
Control: Participants allocated to this group will have their CVAD NCs decontaminated using a 70% IPA (Alcohol Prep Pads, Reynard, New Zealand) disposable swab (0.6 mL). Prior to any procedure requiring CVAD access, the NCs will be swabbed for 5 seconds and allowed to visibly dry. This approach is standard care in the participating units.
Intervention 1: Participants allocated to this group will have their CVAD NCs decontaminated using a 2.0% chlorhexidine gluconate + 70% IPA (Alcohol and chlorhexidine Prep Pads, Reynard, New Zealand) disposable swab (0.6 mL). Prior to any procedure requiring CVAD access, the NCs will be swabbed for 15 seconds and allowed to visibly dry.
Intervention 2: Participants allocated to this group will have their CVAD NCs decontaminated using 70% IPA-impregnated cap (SwabCap, ICU Medical, USA). The cap will be screwed into place on the NC, and remain in place until nursing staff are required to inject medications into the connector. The cap will be discarded, and a new one applied once each treatment has been completed. The cap can stay in position for up to one week, and is required to be in position for at least 5 minutes prior to use so that decontamination can take effect.
OUTCOMES
Primary/Feasibility outcomes
- Proportion of screened patients who are potentially eligible.
- Proportion of eligible participants who are recruited.
- Reasons for non-participation (measured at time of declining to participate).
- Compliance with the trial interventions (measured twice-weekly while participant recruited to study).
- Completeness of data collection for primary outcomes.
- Proportion of participants lost to follow-up or withdrawn.
- Staff satisfaction (collected on study completion).
Feasibility outcomes will be measured at the time of screening, request for consent, and at device removal, patient discharge or four weeks after recruitment, unless otherwise stated.
Secondary outcomes: Proportion of participants with a CABSI infection acquired while participating in the study, and rate of CABSI infections per 1,000 CVAD days. Data for the primary outcome will use laboratory results from pathology specimens collected by clinical staff in response to suspected CVAD-related infections. The CABSI outcome (yes/no) will be made by a blinded rater, who will be provided with de-identified information. Only one CVAD per patient will be studied, not from subsequently inserted CVADs, thus the patient is the unit of measurement. See Table I for CABSI definitions. Time of follow-up will be at device removal, patient discharge or four weeks after enrolment in the study, whichever comes first.
- Primary bloodstream infection.
- CRBSI (Table 1).
- MBI-LCBI: mucosal barrier injury laboratory confirmed bloodstream infection.
- CVAD tip colonisation of > 15 CFU (colony forming units) (Table 1).
- Local infection.
- Duration from CVAD insertion to removal (dwell time) as recorded in clinical documentation (measured at study completion).
- Type and proportion of specific microorganisms present within the NCs. Approximately 10% of participants will have an NC examined by a research microbiologist for identification and quantification of residual microorganisms (measured during participant enrolment of study).
- Participant mortality within 48 hours of participant trial completion.
Secondary outcomes will be measured at device removal, patient discharge or four weeks after recruitment, unless otherwise stated.
SAMPLE SIZE
We will recruit 120 randomised participants to assess feasibility of study outcomes, recruitment and retention procedures. Sample sizes of 40 per group (inclusive of 10% for attrition) are considered sufficient30 to inform sample size calculations and establish study feasibility of subsequent larger studies.
RANDOMISATION AND BLINDING
Randomisation will be computer-generated and undertaken electronically using an independent, centralised service. Once written consent has been provided, the research nurse will access the service to randomise the patient at the time of participant entry to the study. Permuted blocks of randomly varied size, to avoid allocation prediction, will be generated using a 1:1:1 ratio to the two interventions and the control groups. Due to the nature of the interventions, it will not be possible to blind clinicians or patients; however, the microbiologist and hospital laboratory scientists and CABSI rater will be blinded to treatment group.
CVADS AND NC USE AND PROCEDURES
PICCs and Hickman catheters (tunnelled CVADs) will be studied. The PICCs will be inserted by registered nurses in radiology or Wattlebrae procedure room, and the Hickman catheters will be inserted surgically. The patient groups included in the study will be from oncology and surgical wards. Patients will have their intravenous infusion lines changed every third day, and NCs (Smartsite, Carefusion or MaxPlus, Carefusion) at the catheter hub will be changed every seven days. CVADs will be cared for by clinical staff as per hospital policy. Medical staff will order blood cultures as required. Blood cultures are generally ordered when a patient has a temperature of 38.0 °C or greater in the cancer care population, or 38.5 °C in the general medical and surgical wards. The medical staff will determine if a CVAD is required to be removed. Research staff and investigators will have no involvement in the decision to remove CVADs, nor to undertake blood cultures.
DATA COLLECTION
Data will be entered directly into REDCap (Research Electronic Data Capture http://project-redcap.org/) using a portable electronic device. Characteristics collected at baseline will include: age, gender, diagnosis, immunosuppression status, weight category, CVAD type, CVAD insertion site, date of insertion, and number of lumens. The research nurse will review participants and their medical notes three times per week, until 48 hours after the participant is no longer in the study, to assess for adverse events (for example, bloodstream infections) and therapy given through the NC (for example, blood transfusions). Other data, such as blood culture reports, will be obtained by the research nurse from patient charts, notes and computer systems.
Once a patient is no longer in the trial, laboratory results for blood, tip, discharge and other cultures will be reviewed to extract data for infection and mortality outcomes. A blinded medical rater will be supplied with the data to rate infection outcomes. Approximately 10% of participants will have an NC subjected to microbiology testing in the research laboratory to determine if bacteria have grown on the internal NC surface. These NCs are usually discarded in the hospital. The research nurse will liaise with ward staff to ascertain when the patient is due for a line change so that the NC can be collected when no longer required. The NC will then be placed into a specimen jar for storage in a refrigerator for a maximum of seven days, whereby the microbiologist will collect the NC for transport to Griffith University laboratory. Following completion of the trial, nurses will be asked to complete a small, paper-based survey for their feedback regarding the acceptability of trial processes and the interventions.
TRIAL FIDELITY
In this pilot study, there is the potential for cross-over between groups, resulting in protocol violations if nurses use the incorrect decontamination. A number of strategies will be employed to minimise cross-over and maintain treatment fidelity, specifically:
- Education and in-service presentations conducted by the principal investigator will be provided to nurses for one month prior to the commencement to the study. A record will be kept of staff that have completed the sessions, and it is anticipated that approximately 80% of nurses will attend the sessions prior to the study commencement.
- Empower patients to remind nurses which arm of the study they are allocated to.
- A label will be attached to each NC to indicate which arm of the trial the participant has been allocated.
- A sign in the bedside chart and on the patient’s bed will also indicate which arm of the trial the participant has been allocated.
- For those participants allocated to groups requiring NC swabbing, a container located at the bedside will hold a supply of the allocated swabs and include a summary of swab/drying times for the allocated group.
- A one-page fact sheet will be made available to all staff in the participating wards.
- Twice-weekly visits will be attended to conduct audits of product supplies. The investigator will be available for any questions or concerns that ward staff may have.
- The research nurse will perform random audits of the nurses’ actual practice to determine if there are any protocol breaches. If < 20% accesses are not using correct method this would be considered per protocol.
STATISTICAL ANALYSES
Feasibility outcomes will be reported descriptively and analysed against objective targets formulated based on previous pilot trials31,32: greater than 80% of patients screened will be eligible; greater than 80% of eligible participants will agree to enrol; greater than 80% of participants in the intervention groups will receive their allocated treatment; there will be less than 5% attrition/drop-out of randomised patients; there will be less than 5% missing data. Participant data will be analysed on an intention-to-treat basis, with patients being the unit of measure (one CVAD per patient studied). Data will be analysed using PASW Statistics (SPSS Inc.). Descriptive statistics will be used to summarise demographics. Comparability of groups at baseline will be assessed using clinical parameters. The feasibility of the statistical analysis that will be used in the larger trial will be tested. Relative incidence rates of CABSI with 95% confidence intervals (CIs) and Cox regression will be used to test difference between study groups. Kaplan-Meier survival curves (with log rank test) will compare CVAD failure due to CABSI over time between groups. Secondary endpoints will be compared between groups using parametric or nonparametric techniques as appropriate. A per protocol analysis will consider the effect of protocol violations. A p value of ≤ 0.05 will be considered statistically significant.
ETHICAL CONSIDERATIONS
The trial has been approved by the Human Research Ethics Committee of the Royal Brisbane and Women’s Hospital (HREC/15/QRBW/553) and Griffith University (GU Ref No: 2016/410). Registration with the Australian New Zealand Clinical Trials Registry (ANZCTR) has been completed (ACTRN: 12615001120561). All three methods to be tested are already used by various hospitals around the world, so there is no risk to participants higher than that inherent in current practice. Eligible patients will be given an information sheet and it will be ensured that they have time to read this, fully understand it and have an opportunity to ask questions. If consent is given, participants will receive a copy of the information sheet, consent form and revocation of consent form in the event that they wish to withdraw. Adverse events will be recorded, and serious adverse events will be reported to the Human Research Ethics Committee. The principles of the NHMRC National Statement on Ethical Conduct for Human Research will be adhered to throughout the conduct of the study. Anonymity and confidentiality of information will be protected. Data storage will be electronic and secured by username and password access. Any non-electronic data will be stored in a locked cabinet in a locked room. The investigator will ensure that this study is conducted in full conformance with principles of the Declaration of Helsinki. A DSMC will not be convened for this pilot trial since the time frame for recruitment is short.
ABORIGINAL AND TORRES STRAIT ISLANDER WOMEN
The research team are aware of, and will follow, the National Guidelines for Ethical Conduct in Aboriginal and Torres Strait Islander Research33. Aboriginal and Torres Strait Islanders represent approximately 3.5% of patients at the participating site. We have designed the recruitment with the aim of ensuring all patients who fit the criteria are offered participation in the study. We can assume that a small number of these will be Aboriginal and Torres Strait Islanders.
DISCUSSION
This RCT will seek to determine if a larger, full-scale RCT is feasible to conduct. Feasibility elements such as eligibility, retention and attrition, protocol adherence, missing data, staff satisfaction and acceptance will be tested. Findings from this pilot study will assist in the development of a larger RCT that will have important implications for clinical practice, policy decisions, education and patient outcomes.
LIMITATIONS
Results will pertain to the intervention testing in this particular vascular access device type and patient group, and may not be generalisable to other populations. In addition, the pilot trial design means that statistical differences in outcomes between groups are not expected to be detected.
CONCLUSION
Reducing the incidence of CABSI in vulnerable populations, such as cancer care, is vital. If one of the interventional decontamination techniques is shown to decrease the rate of CABSI, and therefore improve patient outcomes, this would reduce patient morbidity and mortality, as well as health care costs.
Table 1: Bloodstream infection definitions
|
CRBSI definition34: Criteria 1: Same organism grown from at least one percutaneous blood culture and from the catheter tip, OR Criteria 2: Two blood cultures taken, one from the CVAD hub and one from a peripheral vein, with the CVAD culture positivity > 2 hours versus the peripheral culture. CABSI definition35: A laboratory confirmed bloodstream infection (LCBI) where a CVAD was in place for > 2 calendar days on the date of event, with day of device placement being Day 1, AND The line was also in place on the date of event or the day before. If a CVAD was in place for > 2 calendar days and then removed, the date of event of the LCBI must be the day of discontinuation or the next day to be a CABSI. LCBI definition35: LCBI 1: Patient has a recognised pathogen cultured from one or more blood cultures, AND the organism cultured is not related to an infection in another area of the body (CDC, 2014), OR LCBI 2: Patient has at least one of the following signs or symptoms—fever, chills or hypotension, AND a positive cultured organism that is not related to an infection in another area of the body, AND the same common contaminant is cultured from two or more blood cultures drawn on separate occasions (CDC, 2014). MBI-LCBI definition35: MBI-LCBI 1: Patient of any age meets criterion 1 for LCBI with at least one blood culture growing any of the following intestinal organisms with no other organisms isolated: Bacteroides spp., Candida spp., Clostridium spp., Enterococcus spp., Fusobacterium spp., Peptostreptococcus spp., Prevotella spp., Veillonella spp., or Enterobacteriaceae (CDC, 2014) OR MBI-LCBI 2: Patient of any age meets criterion 2 for LCBI when the blood cultures are growing only viridans group streptococci with no other organisms isolated (CDC, 2014). MBI-LCBI 1 & 2 also needs to meet one of the following:
|
CRBSI: catheter-related bloodstream infection. CABSI: central venous access device associated bloodstream infection. MBI-LCBI: mucosal barrier injury laboratory confirmed bloodstream infection.
Author(s)
*Julie M Flynn, RN, BN, MAdvPract(HCR) National Centre of Research Excellence, School of Nursing & Midwifery, Griffith University, Nathan, Qld, Australia Alliance for Vascular Access Teaching and Research (AVATAR), Menzies Health Institute Queensland, Griffith University, Nathan, Qld, Australia Royal Brisbane & Women's Hospital, Herston, Qld, Australia Email julie.flynn@griffith.edu.au Samantha Keogh, RN, BSc(Hons), PhD Alliance for Vascular Access Teaching and Research (AVATAR), Menzies Health Institute Queensland, Griffith University, Nathan, Qld, Australia Royal Brisbane & Women's Hospital, Herston, Qld, Australia School of Nursing and Institute of Health and Biomedical Innovation, Queensland University of Technology, Brisbane, Qld, Australia Li Zhang, BMed(Hons), PhD National Centre of Research Excellence, School of Nursing & Midwifery, Griffith University, Nathan, Qld, Australia Alliance for Vascular Access Teaching and Research (AVATAR), Menzies Health Institute Queensland, Griffith University, Nathan, Qld, Australia Claire M Rickard, RN, BN, GradDipNurs(Crit Care), PhD National Centre of Research Excellence, School of Nursing & Midwifery, Griffith University, Nathan, Qld, Australia Alliance for Vascular Access Teaching and Research (AVATAR), Menzies Health Institute Queensland, Griffith University, Nathan, Qld, Australia Royal Brisbane & Women's Hospital, Herston, Qld, Australia *Corresponding author Pages 8-13
References
- Green J. Care and management of patients with skin-tunnelled catheters. Nurs Stand 2008; 22(42):41–8.
- Mahieu LM, De Muynck AO, Ieven MM, De Dooy JJ, Goossens HJ & Van Reempts PJ. Risk factors for central vascular catheter-associated bloodstream infections among patients in a neonatal intensive care unit. J Hosp Infect 2001; 48(2):108–16.
- Menyhay SZ & Maki DG. Disinfection of needleless catheter connectors and access ports with alcohol may not prevent microbial entry: the promise of a novel antiseptic-barrier cap. Infect Control Hosp Epidemiol 2006; 27(1):23–7.
- Jarvis WR, Murphy C, Hall KK, Fogle PJ, Karchmer TB, Harrington G et al. Health care-associated bloodstream infections associated with negative- or positive-pressure or displacement mechanical valve needleless connectors. Clin Infect Dis 2009; 49(12):1821–7.
- Jarvis WR. Choosing the best design for intravenous needleless connectors to prevent healthcare-associated bloodstream infections. Infection Control Today 2010; 14(8):1–3.
- Loveday H, Wilson J, Pratt R, Golsorkhi M, Tingle A, Bak A et al. epic3: national evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J Hosp Infect 2014; 86:S1–S70.
- O'Grady NP, Alexander M, Burns LA, Dellinger EP, Garland J, Heard SO et al. Guidelines for the prevention of intravascular catheter-related infections. Am J Infect Control 2011; 39(4 Suppl 1):S1–34.
- Lockman JL, Heitmiller ES, Ascenzi JA & Berkowitz I. Scrub the hub! Catheter needleless port decontamination. Anesthesiology 2011; 114(4):958.
- Simmons S, Bryson C & Porter S. ‘Scrub the hub’: cleaning duration and reduction in bacterial load on central venous catheters. Crit Care Nurs Q 2011; 34(1):31–5.
- Zack J. Zeroing in on zero tolerance for central line-associated bacteremia. Am J Infect Control 2008; 36(10):S176 e1–2.
- Mimoz O, Lucet J-C, Kerforne T, Pascal J, Souweine B, Goudet V et al. Skin antisepsis with chlorhexidine–alcohol versus povidone iodine–alcohol, with and without skin scrubbing, for prevention of intravascular-catheter-related infection (CLEAN): an open-label, multicentre, randomised, controlled, two-by-two factorial trial. Lancet 2015; 386(10008):2069–77.
- Ayoub F, Quirke M, Conroy R & Hill A. Chlorhexidine-alcohol versus povidone-iodine for pre-operative skin preparation: a systematic review and meta-analysis. International Journal of Surgery Open 2015; 1:41–6.
- Lee I, Agarwal RK, Lee BY, Fishman NO & Umscheid CA. Systematic review and cost analysis comparing use of chlorhexidine with use of iodine for preoperative skin antisepsis to prevent surgical site infection. Infect Control Hosp Epidemiol 2010; 31(12):1219–29.
- Privitera GP, Costa AL, Brusaferro S, Chirletti P, Crosasso P, Massimetti G et al. Skin antisepsis with chlorhexidine versus iodine for the prevention of surgical site infection: A systematic review and meta-analysis. Am J Infect Control 2017; 45(2):180–9.
- Flynn JM, Rickard CM, Keogh S & Zhang L. Alcohol caps or alcohol swabs with and without chlorhexidine: an in vitro study of 648 episodes of intravenous device needleless connector decontamination. Infect Control Hosp Epidemiol 2017; 1–3.
- Queensland Government. Tunnelled central venous catheters 2013 [31/10/2016]. Available from: https://www.health.qld.gov.au/publications/clinical-practice/guidelines-procedures/diseases-infection/governance/icare-tcvc-guideline.pdf.
- Casey A, Worthington T, Lambert PA, Quinn D, Faroqui M & Elliott T. A randomized, prospective clinical trial to assess the potential infection risk associated with the PosiFlow®needleless connector. J Hosp Infect 2003; 54(4):288–93.
- Pichler J, Soothill J & Hill S. Reduction of blood stream infections in children following a change to chlorhexidine disinfection of parenteral nutrition catheter connectors. Clin Nutr 2014; 33(1):85–9.
- Soothill JS, Bravery K, Ho A, Macqueen S, Collins J & Lock P. A fall in bloodstream infections followed a change to 2% chlorhexidine in 70% isopropanol for catheter connection antisepsis: a pediatric single center before/after study on a hemopoietic stem cell transplant ward. Am J Infect Control 2009; 37(8):626–30.
- Cameron-Watson C. Port protectors in clinical practice: an audit. Br J Nurs 2016; 25(8):S25–31.
- DeVries M, Mancos PS & Valentine MJ. Reducing bloodstream infection risk in central and peripheral intravenous lines: initial data on passive intravenous connector disinfection. J Assoc Vasc Access 2014; 19(2):87–93.
- Kamboj M, Blair R, Bell N, Son C, Huang Y-T, Dowling M et al. Use of disinfection cap to reduce central-line–associated bloodstream infection and blood culture contamination among hematology–oncology patients. Infect Control Hosp Epidemiol 2015; 1–8.
- Merrill KC, Sumner S, Linford L, Taylor C & Macintosh C. Impact of universal disinfectant cap implementation on central line-associated bloodstream infections. Am J Infect Control 2014; 42(12):1274–7.
- Nicolás FG, Casariego GJN, Romero MMV, García JG, Diaz RR & Perez JAP. Reducing the degree of colonisation of venous access catheters by continuous passive disinfection. Eur J Hosp Pharm 2015; ejhpharm-2015-000732.
- Patel PA, Boehm S, Zhou Y, Zhu C, Peterson KE, Grayes A et al. Prospective observational study on central line-associated bloodstream infections and central venous catheter occlusions using a negative displacement connector with an alcohol disinfecting cap. Am J Infect Control 2016.
- Ramirez C, Lee AM & Welch K. Central venous catheter protective connector caps reduce intraluminal catheter-related infection. J Assoc Vasc Access 2012; 17(4):210–3.
- Stango C, Runyan D, Stern J, Macri I & Vacca M. A successful approach to reducing bloodstream infections based on a disinfection device for intravenous needleless connector hubs. J Infus Nurs 2014; 37(6):462–5.
- Sweet MA, Cumpston A, Briggs F, Craig M & Hamadani M. Impact of alcohol-impregnated port protectors and needleless neutral pressure connectors on central line-associated bloodstream infections and contamination of blood cultures in an inpatient oncology unit. Am J Infect Control 2012; 40(10):931–4.
- Wright MO, Tropp J, Schora DM, Dillon-Grant M, Peterson K, Boehm S et al. Continuous passive disinfection of catheter hubs prevents contamination and bloodstream infection. Am J Infect Control 2013; 41(1):33–8.
- Hertzog MA. Considerations in determining sample size for pilot studies. Res Nurs Health 2008; 31(2):180–91.
- Keogh S, Flynn J, Marsh N, Mihala G, Davies K & Rickard C. Varied flushing frequency and volume to prevent peripheral intravenous catheter failure: a pilot, factorial randomised controlled trial in adult medical-surgical hospital patients. Trials 2016; 17(1):348.
- Marsh N, Webster J, Flynn J, Mihala G, Hewer B, Fraser J et al. Securement methods for peripheral venous catheters to prevent failure: a randomised controlled pilot trial. J Vasc Access 2015; 16(3):237–44.
- NHMRC. Values and Ethics: A guide for ethical conduct in Aboriginal and Torres Strait Islander health research. Canberra: National Health and Medical Research Council 2003.
- APIC. Guide to the elimination of catheter-related bloodstream infections 2009 [31/10/2016]. Available from: http://www.apic.org/Resource_/EliminationGuideForm/259c0594-17b0-459d-b395-fb143321414a/File/APIC-CRBSI-Elimination-Guide.pdf.
- CDC. Bloodstream Infection Event (Central line-associated bloodstream infection and non-central line-associated bloodstream infection) 2016 [31/10/2016]. Available from:http://www.cdc.gov/nhsn/PDFs/pscManual/4PSC_CLABScurrent.pdf.
