Volume 5 Issue 2
Repositioning a peripherally inserted central catheter (PICC) using a high-flow flush technique (HFFT) in an adult patient with non-Hodgkin’s lymphoma
Leanne Ruegg
Keywords Repositioning PICC, high-flow flush technique, HFFT, non-Hodgkin's lymphoma
For referencing Ruegg L. Repositioning a peripherally inserted central catheter (PICC) using a high-flow flush technique (HFFT) in an adult patient with non-Hodgkin’s lymphoma. Vascular Access 2019; 5(2):49-50.
DOI https://doi.org/10.33235/va.5.2.49-50
Peripherally inserted central catheters (PICCs) are specialised central catheters that can provide reliable venous access in many diverse patient populations1,2. PICCs are a convenient means of administering chemotherapy agents3.
However, misplaced PICCs have been reported in various anatomical positions including the arterial system, jugular vein or axillary vein1,3. Detection of a malposition, when not using navigational and tip positioning techniques, can often be frustrating for the inserting proceduralist during the post-insertion chest x-ray (CXR) review. Navigational and electrocardiogram (ECG)-based technologies have reduced the incidence of primary catheter tip malposition in PICCs1.
A 45-year-old male presented to the oncology day unit for his seventh cycle of R-CHOP (cyclophosphamide, doxorubicin, vincristine and prednisone). His history included non-Hodgkin’s lymphoma and diffuse B-cell lymphoma with extensive abdominal disease. Three attempts of peripheral cannulation were unsuccessful by nursing staff in the oncology day unit and, as a result, his treatment needed to be delayed. Consequently, consent was gained by the medical officer for the insertion of a PICC. The patient’s previous presentations had no history of vascular access difficulties and his previous chemotherapy cycles were successfully administered via peripheral cannulas.
The nurse-led bedside PICC insertion team performed ultrasound and located the right basilic vein; however, this was only after two unsuccessful punctures. The right cephalic vein, located using ultrasound scan (USS) guidance, was successfully punctured at first attempt and a guidewire was introduced. An uncomplicated modified seldinger technique was performed and a 5 French dual lumen catheter was inserted with no issues. The nurse-led team used an ECG and tip confirmation system (TCS) to confirm PICC placement. The catheter was inserted to the hub; however, the ECG was indicating that the PICC was not centrally placed in the lower third of the superior vena cava. Various remedies were attempted unsuccessfully to correct the tip position4. Remedies attempted were the abducting of the shoulder to influence the PICC movement and the pulling back of the internal stylet by approximately one inch to allow a floppier catheter tip to follow the direction of the blood flow more easily. Subsequently, the patient was transferred to the Medical Imaging Department (MID) and a CXR was performed to confirm the PICC tip position (see Figure 1).

Figure 1. The PICC is looped in the axillary vein and the tip lies at the junction of the axillary and subclavian veins.
The optimal PICC tip position is at the cavoatrial junction (CAJ). Malpositioned PICCs outside the optimal position result in treatment delays, and previously required lengthy, expensive procedures to reposition or replace the existing PICC. Traditional repositioning techniques require the use of expensive wires and may further delay treatment1,5,6.
An alternate technique is the high-flow flush technique (HFFT). This is a safe and cost-effective intervention to correct PICC malpositions – it has minimal interference to intravenous therapy and only involves a nominal cost1. Another similar technique is a simultaneous rapid saline flush (SRSF)5. The SRSF involves flushing both lumens simultaneously with a saline power flush using 10mL syringes. The patient is placed in the high fowler’s position and instructed to cough, followed by HFFT or SRSF1,5.
In this case, the radiologist notified the PICC team of the PICC’s position and, after a discussion, it was decided to attempt a SRSF while the patient remained in the MID so that a repeat CXR could be performed immediately post-flushing. The decision to use SRSF was based on the patient having a dual lumen 5 French PICC.
The patient was placed in the imaging room and two PICC nurses aseptically connected each lumen with a pre-filled 10mL saline syringe. As aforementioned, the patient was instructed to cough and both lumens were flushed. Immediately, the patient was placed in a standing position to take a post-CXR. In this instance, SRSF was only used once and it was successful, advancing the tip to the CAJ. Post-flush, the control CXR demonstrated a correctly placed PICC with the tip positioned in the superior vena cava (see Figure 2).
In conclusion, instead of repositioning the PICC with time-consuming and costly procedures, such as an over-the-wire exchange, the feasible alternative of a SRSF was successful. The patient received the planned treatment the same day as planned.
DISCLOSURE
The author was involved in the care of the patient.
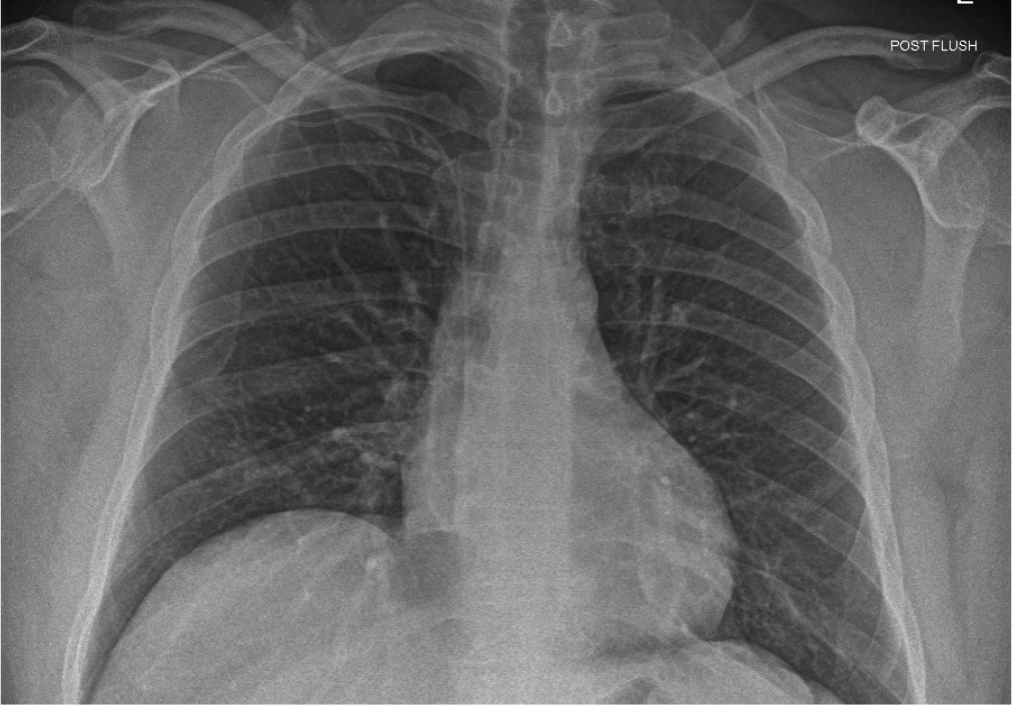
Figure 2. Post-flushing, the PICC courses normally from the right upper limb with the distal tip appropriately positioned at the cavoatrial junction.
Author(s)
Leanne Ruegg
Clinical Nurse Consultant, Medical Services Group, Sunshine Coast University Hospital, 6 Doherty St, Birtinya, QLD 4575, Australia
Email leanne.ruegg@health.qld.gov.au
References
- Spencer TR. Repositioning of central venous access devices using a high-flow flush technique – a clinical practice and cost review. J Vasc Access 2017;18(5):419–25.
- Walker G, Todd A. Nurse-led PICC insertion: is it cost effective? Br J Nurs 2013;22(19):S9–15.
- Song L, Li H. Malposition of peripherally inserted central catheter: experience from 3,012 patients with cancer. Exp Ther Med 2013;6(4):891–3.
- Pittiruti M, Bertollo D, Briglia E, Buononato M, Capozzoli G, De Simone L, et al. The intracavitary ECG method for positioning the tip of central venous catheters: results of an Italian multicenter study. J Vasc Access 2012;13(3):357–65.
- Natividad E, Rowe T. Simultaneous rapid saline flush to correct catheter malposition: a clinical overview. J Assoc Vasc Access 2015;20(3):159–66.
- Wang L, Liu ZS, Wang CA. Malposition of central venous catheter: presentation and management. Chin Med J (Engl) 2016;129(2):227–34.
Vascular Access — Call for papers
The deadline for submissions is 19 JANUARY 2020
The Australian Vascular Access Society (AVAS) is an association of healthcare professionals founded to promote the vascular access specialty (http://avas.org.au/). Our multidisciplinary membership strives to advance vascular access research, promotes professional and public education to shape practice and enhance patient outcomes, and partners with industry to develop evidence-based innovations in vascular access.
The electronic journal Vascular Access is the official publication of AVAS, and provides a venue for national and international scholars and practitioners to publish high-quality, peer-reviewed research and educational reviews relevant to vascular access in Australia and globally. The journal also provides a space for evidence-based discussions and debate on issues of importance to patients requiring vascular access.
Vascular Access is published twice a year (April and October) and manuscripts pertaining to this specialty are invited. The editor welcomes manuscripts in the form of research findings, clinical papers, case studies, reports, review articles, letters and product appraisals. Video submissions are also welcomed. Submissions will be accepted from any country but must be in English.
For more information, please see the Author Guidelines or contact the Editor at editor@avas.org.au
