Volume 6 Issue 1
Peripherally inserted central catheter-associated complications: a retrospective review of a nurse-led peripherally inserted central catheter-insertion service
Leanne Ruegg, Reto Federi and Keat Choong
Keywords infections, Cost, PICC placement, thrombosis
For referencing Ruegg et al. Peripherally inserted central catheter-associated complications: a retrospective review of a nurse-led peripherally inserted central catheter-insertion service. Vascular Access 2020; 6(1):16-19.
DOI https://doi.org/10.33235/va.6.1.16-19
Abstract
Objective Complication rates from peripherally inserted central catheters (PICC) insertions are reportedly high. The aim of this study is to report positive patient outcomes from a nurse-led PICC insertion team.
Methods We conducted a retrospective analysis of consecutive adults that had a PICC line inserted between 1 January and 31 December 2017. The study examined the prevalence of major complications – catheter-related bloodstream infection (CRBSI) and catheter-related deep vein thrombosis (CRDVT).
Results The total number of PICCs inserted was 661.The total number of catheter days was 10,732 and the average catheter dwell time was 22 days. Four cases of CRBSI (0.37 per 1000 catheter days) were observed. Five patients had CRDVT (0.46 per 1000 catheter days).
Conclusions The nurse-led PICC service demonstrated minimal infection and thrombus complications. Nurses who are trained to insert PICCs can improve patient flow and provide cost savings.
Background
Peripherally inserted central catheters (PICC) are specialised catheters that can provide reliable venous access. PICCs are also commonly used for intravenous therapy in hospital, in the home, or in outpatient antibiotic therapy settings, allowing patient care to continue in non-hospital settings and improve bed utilisation.1 The use of PICCs has risen significantly over the past 35 years, given the many advantages of these devices and the lower complication rates compared with traditional central venous catheters (CVC), e.g. pneumothorax.1,2 PICCs inserted using ultrasound guidance into upper limb veins have a high successful insertion rate and low insertion complication rate.3,4 PICCs were traditionally placed by a medical officer.5 The first nurse-led vascular access team was established in the USA.6 Nurse-led, ultrasound-guided PICC insertion teams decrease waiting times and improve patient flow. In addition, costs are reduced by minimising the use of interventional radiology (IR) facilities as well as using less expensive staff compared to medical officers.5-8
While there are many benefits associated with the use of PICCs, there are risks of bloodstream infections and catheter-related thromboses. In a systematic review, the rate of PICC-related bloodstream infection was reported as 2.4% (2.1 per 1000 catheter days).9 Catheter-related thrombosis is a relatively common complication of PICCs; Lobo and colleagues concluded that 5% of patients undergoing PICC placements in acute care hospitals will develop thromboembolic complications.10 There are often other risk factors (e.g. malignancy and sepsis) that may predispose a patient to a thromboembolic event.11
Our nurse-led service (NLS), run by the vascular access surveillance and education (VASE) team, has been performing PICC insertions at the bedside since 2009. The Sunshine Coast Hospital and Health Service (SCHHS) is located in South East Queensland and serves a population of around 390,000 people. The Health Service consists of Sunshine Coast University Hospital, a tertiary 500-bed hospital, as well as three peripheral hospitals. The VASE team, based at the hospital, comprises a clinical nurse consultant and three clinical nurses. PICC insertions are provided during business hours, 7 days a week. On request, this service is also available to the peripheral sites within the SCHHS, including both inpatient and outpatient populations.
In addition to the clinical component, this service is responsible for facilitating educational and surveillance aspects of vascular access device utilisation across all professional disciplines, and it supports clinical areas across the health service to minimise or prevent healthcare-associated complications related to vascular access devices.
PICCs inserted by the VASE team are entered into a clinical database and reviewed monthly for adverse outcomes by examining the patients’ electronic medical records. A retrospective analysis was performed comparing adverse outcomes of PICCs inserted by our service with the current literature to benchmark the quality of insertion and care we provide. All patients were screened for PICC-related complications from insertion to removal.
PICC insertion and care
All PICCs used were BARD Power PICC Solo₂® Polyurethane valved catheters12 inserted by experienced registered nurses performing over 600 insertions per annum collectively. PICC insertions were performed using the Sherlock 3CG® tip confirmation system.13 The system uses a sensor that tracks a magnetic tip at the distal end of the catheter and intraluminal electrocardiogram (ECG) measurements to confirm the position of the catheter tip relative to the heart.1,4 Using this technology to confirm appropriate tip placement, a chest x-ray was avoided for most patients (79%). Subsequently, it provided the opportunity to perform the procedure at the patient’s bedside or in an outpatient clinic. If ECG tip confirmation was contraindicated (e.g. atrial fibrillation or a permanent pacemaker in situ), a chest x-ray was obtained to determine appropriate tip placement. Queensland Health’s diseases and infection prevention guidelines for intravascular device management insertion14 were strictly followed, which included a surgical scrub, maximum barrier precautions and chlorhexidine antisepsis. Optimal catheter size (single or multi lumens) was determined by adequate vein size.1,12,14,16
All PICC lines were secured with an adhesive stabilisation device (StatLock®)17 and a 3M™ Tegaderm™ CHG (Chlorhexidine Gluconate) IV Securement Dressing.18
Queensland Health’s diseases and infection prevention guidelines14 for intravascular device management, care and maintenance, bundles and protocols post-insertion were also followed (e.g. decontamination of needleless connectors performed with impregnated 70% isopropyl alcohol wipes prior to accessing or de-accessing; catheter insertion site checks performed once per shift; weekly dressing changes or as required; and daily review for catheter need).14
Method
The study focused on complications such as catheter-related bloodstream infection (CRBSI) and catheter-related deep venous thrombosis (CRDVT) in the inpatient and outpatient population with a PICC inserted by our team. A retrospective analysis of these outcomes was conducted across two sites over a one-year period from 1 January 2017 to 31 December 2017. The CRBSI data were obtained from a state-wide database where all hospital-acquired infections are reported. The CRDVT data were collected from electronic medical records and our local radiology report database. Our database allowed us to track inpatients and outpatients while a PICC line was in situ.
Complication Definitions
We defined CRBSI as the isolation of a recognised bacterial or fungal pathogen from one or more blood cultures in a patient with a PICC present within 48 hours of the blood collection, according to the Centre for Healthcare Related Infection Surveillance and Prevention, Queensland Health.18 Additionally, the organism was not related to an infection at another site. Organisms that are considered a potential contaminant (e.g. coagulase-negative staphylococci) were only treated as a CRBSI if, within 24 hours (in addition to a PICC being present within 48 hours of collection), the patient had at least one of: fever (>38°C), hypotension, chills/rigors, and either the organism was isolated in at least two separate blood cultures (taken at separate times) within 48 hours or if only a single blood culture taken (with isolation of a potential contaminant), then appropriate antimicrobial therapy was commenced.19
A CRDVT was defined as an occlusive or non-occlusive filling defect in the deep veins (brachial, axillary or subclavian) on the ipsilateral side proximal to the PICC insertion site, confirmed by ultrasound. Superficial vein thrombosis was excluded.
Results
In the inpatient population, five patients (0.46 per 1000 catheter days) had a CRDVT of the upper extremity, confirmed by ultrasound scan. Average time from insertion to confirmed CRDVT was five days. No CRDVT was reported in the outpatient population.
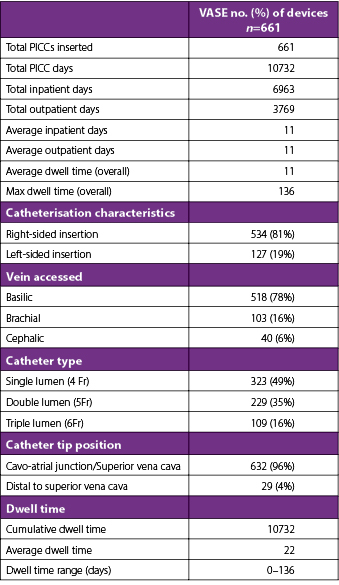
A total of 661 PICCs were inserted during the 10,732 PICC days of the study period (see Table 1). For inpatients and outpatients, the average dwell time was 11 days and the maximum dwell time was 136 days. Indications for PICC insertion included antibiotic administration (61%, n=403), chemotherapy (16%, n=107), total parenteral nutrition (9%, n=58), multiple incompatible medications (8%, n=52), difficult venous access (5%, n=31), and delivery of inotropes (1%, n=10). Of devices used, 49% (n=323) were 4 French single-lumen, 35% (n=229) were 5 French double-lumen, and 16% (n=109) were 6 French triple-lumen PICCs. The incidence rate of insertion-related CRBSI was zero; this was measured within a 48-hour timeframe post-insertion.
There were four cases (0.37 per 1000 catheter days) of CRBSI necessitating PICC removal. Cultured organisms included Staphylococcus epidermis, Enterobacter cloacae, Candida albicans, Streptococcus parasanguinis, and Streptococcus salivaris (one infection was a polymicrobial infection). The average time from insertion to infection was 16 days.
Table 1. Catheter day summary
The saving per procedure is approximately $165.95 AUD per insertion. PICC insertion consumables were drawn up and the costings were identical for both the IR department and the VASE team (see Table 2).20
Table 2. Staff cost comparison
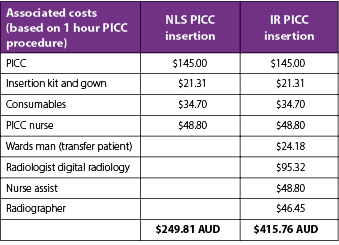
Note: values are based on Queensland Heath wages and consumable costs from a Queensland Health perspective.20
Discussion
This retrospective study was performed to benchmark our local data with current literature. The review found low rates of CRBSI and CRDVT when PICC insertion was performed by a nurse-led team. These results are reassuring, considering the increasing use of PICC lines in the health service. To date, the VASE team continues to insert the majority of PICCs; however, difficult insertions (kinking of catheter despite several attempts, unsuitable veins for insertion) are referred to the IR department.
Chopra and McDiarmid showed higher rates of PICC-related bloodstream infections in patients with cancer (1.8-7.7/1000 catheter days) than those without (1.1/1000 catheter days).1,8 Our study also demonstrated an increased incidence rate of CRBSI in cancer patients (0.7/1000 catheter days) compared with non-cancer patients (0.3/1000 catheter days).
By comparison, our CRBSI rate for PICCs was lower than in other studies. Also, no CRBSI occurred within 48 hours of insertion, suggesting that strict surgical asepsis was maintained throughout the procedure in accordance with the NLS PICC insertion bundle.15 Contributing factors in relation to ongoing line management are contributing to the CRBSI risk rather than insertion technique. Follow-up education and surveillance has since been recommended in the general clinical wards to reinforce post-care maintenance bundles.
Additionally, in our patient cohort we found that CRDVT was uncommon (0.75%). Chopra21 reported that CRDVT was a common and costly event in patients with cancer, with reported rates of 3.4–7.8% in this cohort. PICC size is a contributing factor for CRDVT,9,21,22 which is consistent with our study. Sixty percent (three from five) of CRDVT occurred in the setting of 6 French, triple-lumen PICCs. The choice of PICC size and the number of lumens was based on vessel size and specific clinical needs of the patient. While our study demonstrated low numbers of CRDVT, consideration still should be given to minimising the lumen size.
Conclusion
We reported lower rates of CRBSI and CRDVT than those recently published. We attribute our low rates to an experienced nurse-led team following a standardised insertion bundle and the use of a tip navigation/confirmation system. We also found financial savings associated with the nurse-led model.
The study highlighted monitoring patient outcomes can lead to steering quality improvement activities. In this study, interventions such as device reminders to promote adherence to maintenance bundles may be important in preventing PICC complications.
Author(s)
*Leanne Ruegg1; Reto Federi2; Keat Choong3
¹Clinical Nurse Consultant, Vascular Access Surveillance and Education, Sunshine Coast Hospital and Health Service, QLD, Australia
²Clinical Nurse, Vascular Access Surveillance and Education, Sunshine Coast Hospital and Health Service, QLD, Australia
³Infectious Diseases Physician, Infectious Diseases Department, Sunshine Coast Hospital and Health Service, QLD, Australia
*Corresponding author
Leanne Ruegg, Clinical Nurse Consultant, Medical Services Group, Sunshine Coast University Hospital, 6 Doherty Street, Birtinya, QLD 4575, Australia
Email Leanne.ruegg@health.qld.gov.au
References
- Chopra V, Ratz D, Kuhn L, Lopus T, Chenoweth C, Krein S. PICC-associated bloodstream infections: prevalence, patterns, and predictors. Am J Med. 2014;127(4):319-328.
- Gibson C, Connolly BL, Moineddin R, Mahant S, Filipescu D, Amaral JG. Peripherally inserted central catheters: use at a tertiary care pediatric center. J Vasc Interv Radiol. 2013;24(9):1323-1331.
- Ng PK, Ault MJ, Ellrodt AG, Maldonado L. Peripherally inserted central catheters in general medicine. Mayo Clinic Proceedings. 1997;72(3):225-233.
- Alexandrou E, Murgo M, Calabria E, Spencer TR, Carpen H, Brennen K, et al. Nurse-led central venous catheter insertion-procedural characteristics and outcomes of three intensive care based catheter placement services.” Int J Nurs Stud. 2012;49(2):162-168.
- Alexandrou E, Spencer T, Frost SA, Parr M, Davidson PM, Hillman KM. Establishing a nurse-led central venous catheter insertion service. JAVA. J Assoc Vasc Access. 2010;15(1):21-27.
- Walker G,Todd A. Nurse-led PICC insertion:is it cost effective? BJN 2013;22(19)20-26.
- Robinson MK, Mogensen KM, Grudinskas GF, Kohler A, Jacobs DO. Improved care and reduced costs for patients requiring peripherally inserted central catheters: the role of bedside ultrasound and a dedicated team. JPEN J Parent Enteral Nutr. 2005;29(5):374-379.
- McDiarmid S, Scrivens N, Carrier M, Sabri E, Toye B, Huebsch L et al. Outcomes in a nurse-led peripherally inserted central catheter program: a retrospective cohort study. CMAJ Open. 2017;5(3):E535-E539.
- Spencer, T.R., Mahoney, K.J. Reducing catheter-related thrombosis using a risk reduction tool centered on catheter to vessel ratio. J Thromb Thrombolysis. 2017;44:427-434.
- Lobo BL, Valdean G, Broyles J, Reaves AB, Shorr RI. Risk of venous thromboembolism in hospitalized patients with peripherally inserted central catheters. J Hosp Med. 2009;4(7):417-422.
- Wall C, Moore J, Thachil J. Catheter-related thrombosis: A practical approach. J Intensive Care Soc. 2016;17(2):160-167.
- Bard Access Systems, Inc. Power PICC Solo2®: polyurethane valved PICC with microintroducer. 2016. Available from http://www.bardaccess.com/assets/literature/0741199_PowerPICC_SOLO_RN_IFU_Web.pdf
- Bard Access Systems, Inc. Sherlock 3cg®: Tip Confirmation System (TCS). 2016. Available from https://www.bardaccess.com/products/imaging/sherlock-3cg
- Department of Health, Queensland. Peripherally inserted central venous catheters (PICC). 2015. Available from https://www.health.qld.gov.au/_data/assets/pdf_file/0032/444497/icare-picc-guideline.pdf
- Dale M, Higgins A, Carolan-Rees G. Sherlock 3CG((R)) Tip confirmation system for placement of peripherally inserted central catheters: A NICE medical technology guidance. Appl Health Econ Health Policy. 2016;14(1):41-49.
- Royal College of Nursing, Intravenous Therapy Forum. Standards for infusion therapy (4th ed.). London, UK: Royal College of Nursing; 2016.
- Bard Access Systems. Statlock®. https://www.bardaccess.com/products/stabilization/pcl-picc-plus
- 3M. 3M™ Tegaderm™ CHG Chlorhexidine Gluconate IV Securement Dressing. https://www.3m.com/3M/en_US/company-us/all-3m-products/~/3M-Tegaderm-CHG-Chlorhexidine-Gluconate-I-V-Securement-Dressing/?N=5002385+3293321978&rt=rud
- Centre for Healthcare Related Infection Surveillance and Prevention, Queensland Health. Surveillance Manual Third Edition (July 2009). https://www.health.qld.gov.au/clinical-practice/guidelines-procedures/diseases-infection/infection-prevention/intravascular-device-management
- Queensland Health wage rates https://www.health.qld.gov.au/hrpolicies/salary
- Chopra V, Anand S, Krein SL, Chenoweth C, Saint S. Bloodstream infection, venous thrombosis, and peripherally inserted central catheters: reappraising the evidence. Am J Med. 2012:125(8):733-741.
- Evans RS, Sharp JS, Linford LH, Lloyd JF, Tripp JS, Jones JP, et al. Risk of symptomatic DVT associated with peripherally inserted central catheters. Chest. 2010;138(4):803-810.
