Volume 40 Number 3
Development of an incontinence-associated dermatitis prevention bundle using an evidence-based framework
Hsiu Hui Wei, Chih-Ling Huang, Wen-Pei Huang and Hsiu-Chin Chen
Keywords Incontinence-associated dermatitis, evidence-based framework, bundle care
For referencing Wei HH et al. Development of an incontinence-associated dermatitis prevention bundle using an evidence-based framework. WCET® Journal 2020;40(3):37-42.
DOI https://doi.org/10.33235/wcet.40.3.37-42
Abstract
Background Incontinence-associated dermatitis (IAD) is a prevalent cause of skin damage in the clinical setting. IAD may cause a heat sensation, pruritus, pain and infection as well as prolong hospital stays and increase healthcare costs.
Objective The aim of this study was to develop a bundle care guideline for IAD based on an evidence-based framework.
Method Three steps were conducted: an IAD bundle care guideline was drafted, consensus among hospital nursing staff and clinical experts was obtained, and an evaluation was made by methodology experts.
Results The initial guideline was approved by 30 nurses and seven clinical experts (two runs) to achieve >80% agreement. Three methodology experts evaluated the quality of the development process as a use recommendation. The IAD bundle care guideline consisted of four aspects with 19 interventions – skin assessment, skin cleansing, skin protection and supportive care. The IAD bundle care guideline was standardised and evidence-based.
Conclusions The developed IAD bundle care guideline integrates information from a systematic literature review and the opinions of nurses, clinical experts and methodology experts, and is recommended for clinical application. Further studies will be implemented to verify its effectiveness.
Introduction
Incontinence-associated dermatitis (IAD) is a prevalent cause of skin damage in the clinical setting. IAD may cause a heat sensation, pruritus, pain and infection as well as prolong hospital stays and increase healthcare costs1. A cross-sectional study in Taiwan found that the prevalence of IAD is 26.3% and that a high proportion of cases occur during hospitalisation2. The incidence of acute nosocomial IAD in the USA is 45.7%, and IAD is associated with a significantly increased prevalence of sacral pressure injury3. Once IAD occurs, empirical care should be provided to shorten healing time and prevent the occurrence of complications4. The IAD assessment and standard care are inconsistent in the different organisations and need to be developed5. A systematic review of IAD care was conducted in the previous study6. The review consisted of four aspects of IAD prevention and treatment interventions – skin assessment, skin cleansing, skin protection and supportive care.
The Institute for Healthcare Improvement introduced the concept of bundle care to improve the quality of care7. In this study, the evidence-based approach was used as a guide to develop an IAD care bundle integrated with the four aspects of interventions. The approach included systematic review, clustering evidence-based interventions, and appraisal of clinical practices. Gray et al. recommend that implementation of standardised strategies would promote integration of IAD prevention and management into practice in order to prevent and treat IAD8. The intervention review showed that there was a lack of consistent and evidence-based IAD prevention and interventions9 and that some trials mostly focused on skin care products and procedures10. Although a previous study included IAD assessment, prevention and management strategies11, these lacked empirical IAD bundle care guidelines. Therefore, the aim of this study was to develop a bundle care guideline for IAD based on an evidence-based framework.
The trials included in this review tested skin care products, procedures and the frequencies of using a skin care product.
Methods
In the systematic review, the databases included the Cumulative Index to Nursing and Allied Health Literature, PubMed, Cochrane Library, Joanna Briggs Institute, National Guideline Clearinghouse, and Best Practice Guidelines. Key words included incontinence-associated dermatitis or incontinence lesion and skin care and prevention and intervention. A total of 27 articles were extracted to evaluate the quality of evidence. The preliminary bundle care guidelines include four major aspects – skin assessment, skin cleansing, skin protection and supportive care – and, originally, 20 care activities6.
First, the care guidelines were subjected to expert validity testing. The importance, applicability and text clarity of the guidelines were reviewed and scored by five wound and ostomy nurses using a 4-point Likert scale. Next, a content review of the care guidelines was performed by 30 clinical nurses with professional advanced level 2 and above, seven clinical experts and researchers, and three methodology experts (Figure 1).
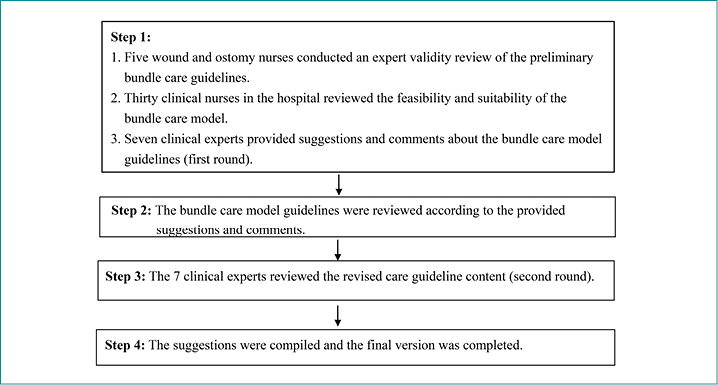
Figure 1. Flowchart of the development of the IAD bundle care guidelines
Clinical nursing staff and clinical experts performed practical reviews and scored the care activities according to implementation feasibility and applicability. The scoring was from 4 (agree) to 1 (disagree) and 0 (not applicable). Concrete suggestions must be provided for ‘disagree’ and ‘not applicable’ items. The care activities must be achieved to an 80% approval rate. At the same time, three methodology experts reviewed the content according to the six quality domains of the Appraisal of Guidelines for Research & Evaluation (AGREE)12 – scope and purpose, stakeholder involvement, developmental rigour, presentation clarity, applicability, and editorial independence – in order to assess the overall guidelines and to review the research quality and rigour of the IAD bundle care guidelines12. A percentage of the maximum possible score for each domain was computed. A domain score was calculated by summing up all the scores of the individual items in a domain.
Results
The content validity index of the preliminary bundle care guidelines was ≥0.8. In the first round of the content rigour review of the care guidelines for the feasibility of implementation, 18 of 20 questions achieved ≥80% approval from 30 clinical nurses. Stool characteristics and quantity were recorded daily (agreement level 60.1%) and a semi-prone position was adopted twice daily (66.7%). Regarding the applicability of implementation, 19 questions achieved ≥80% approval, with an agreement level of 76.6% for recording stool characteristics per day. This item achieved 100% agreement on the expert reviews and then was not revised. The clinical experts mentioned that the IAD assessment scale in the study was very complex and limited usefulness of clinical practices.
The overall evaluation and suggestions by clinical nursing staff were as follows:
- More pictures on the IAD assessment form could be added.
- High-risk patients could be highlighted.
- The stool assessment could be translated into Chinese to facilitate reading and usage by the evaluator.
- Skin cleansing could be performed once a day or after defecation or urination.
- The skin cleansing solutions or protectants involve fees that make these a financial burden for the family.
- Some family members or caregivers may hold on their own views and not be in compliance with health education for care guidance.
- The recommendation of adopting a semi-prone position twice a day may not be performed for patients with ankylosis, limb contractures, or other limitations, so patients’ positions could be performed according to individual conditions.
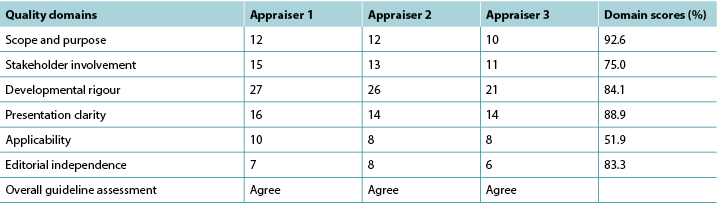
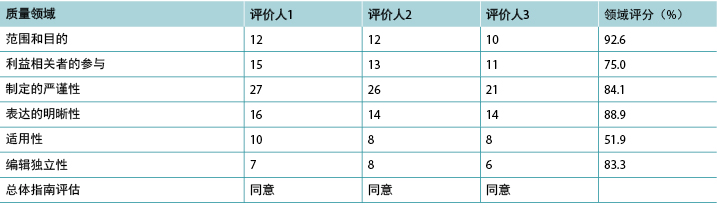
In the first round of consensus results from the seven clinical experts, six of 20 interventions listed did not achieve 80% approval (Table 1). The authors conducted the search and a review of the literature and then revised these items. In the second consensus, all items achieved ≥80% approval. Table 2 shows the results of the six components reviewed by methodology experts. The suggestions provided are as follows:
- The bundle care guideline could be developed using easy-to-understand cards or booklets to facilitate folding and reading.
- This version of the bundle care guidelines and recommendations is for nurses. A caregiver version could be developed in the future.
- The items need to be clarified and revised to promote the readability and feasibility. Table 2 showed the score of applicability domain was the lowest, a standardised score of 51.9%.
Table 1. Consensus results of the bundle care guidelines from seven clinical experts
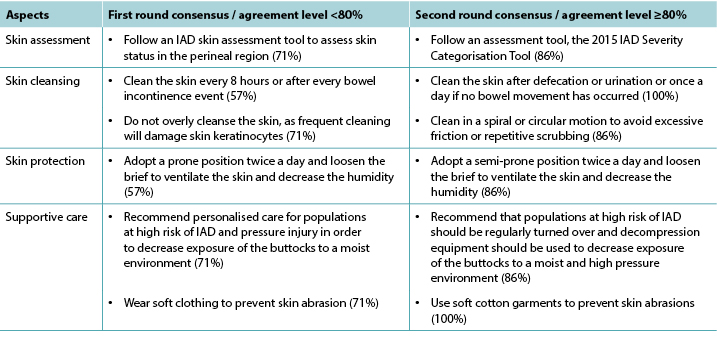
Table 2. Quality domain assessments by methodology experts
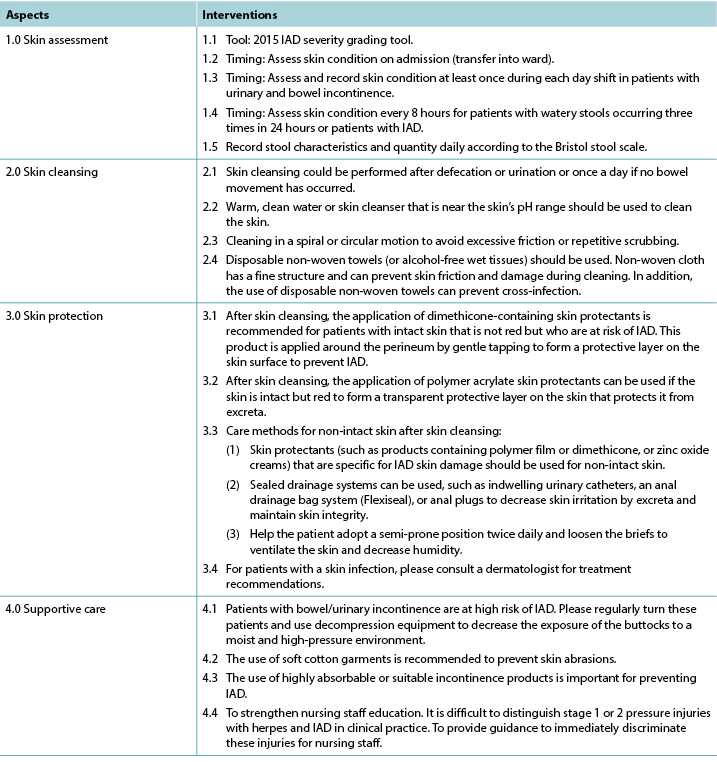
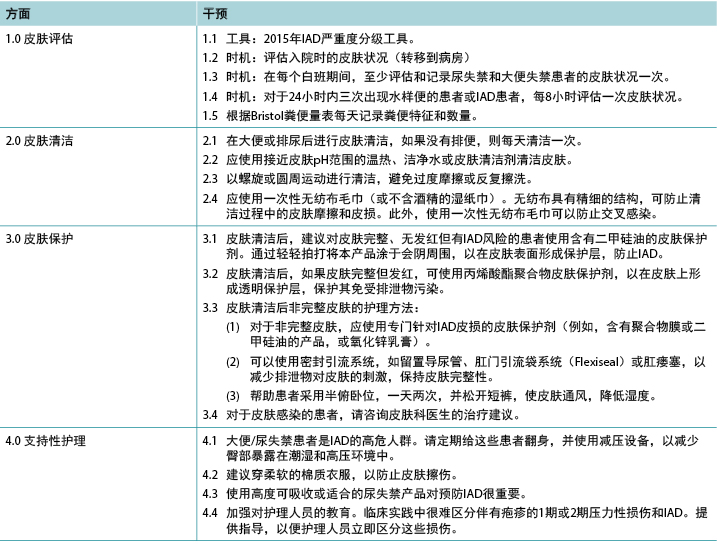
Finally, the recommendations provided by the experts were included in the final version of the bundle care guidelines. One intervention of cleansing activities was removed because of the similarity to “2.3 … to avoid excessive friction or repetitive scrubbing”, and 19 interventions were retained (Table 3). The bundle care guideline did not include new care techniques; rather, it included intervention obtained from experts and research methodologists. A systematic and structured bundle care guideline with a good rigour was developed. The differences between this bundle care guideline and past care standards or protocols were as follows:
- The care guideline comprised of four components – skin assessment, skin cleansing, skin protection and supportive care. The characteristics of this bundle guideline were evidence-based implementation and the feasibility of clinical practices which were validated by clinical experts.
- The skin assessment included times and tools.
- Besides skin cleansing after urination or defecation, to clean the skin in the perineal region at least once was added in the guideline.
- Empirical interventions for non-intact skin in the skin protection component were added in the guideline.
Table 3. Bundle care guidelines for IAD
Discussion
In this study, an IAD bundle care guideline was first developed using an evidence-based framework to promote the feasibility and application of implementation. The revision of care guideline consisted of four components (19 interventions) – skin assessment (five items), skin cleansing (four items), skin protection (six items), and supportive care (four items). The existing IAD assessment scale was very complicated, including area of skin breakdown (scores 0–3), skin redness (scores 0–3), and erosion (scores 0–4)13.
Therefore, the authors recommend using the IAD severity grading tool that was proposed based on the 2015 Global IAD Expert Panel recommendations. This assessment tool could be used for the simple discrimination of injury severity of grades 0–2; the higher grade, the more serious the injury11. The literature showed that a combination of this grading tool and care protocol could be used for quality monitoring and research. Although the expert validity of this tool was conducted, its reliability needs to be developed10,11. In 2016, Taiwanese researchers revised this severity grading, evaluation tool, and preventive intervention using picture cards to promote the clinical applicability and caregivers’ compliance of care guidelines14. In addition, the IAD assessment tool and the Braden Scale could be combined in further research to integrate the interventions of complete skin care2.
Regarding the standard of daily cleaning for the perineal region in the day shift and the need for concrete cleansing method, the authors recommend a change in cleansing time and methods in the cleaning component by considering the patient’s rest time and nurse-to-patient ratios in the night shift. In the initial guideline, the statement “repetitive cleaning or forceful cleaning is the direct cause of skin injury” needs to be removed because no relevant articles quantify the number of times and strength for cleaning or back-and-forth scrubbing1,15.
In the skin protection component, there is no relevant literature to provide the evidence of the time duration for semi-prone positioning. Therefore, the intervention was revised not to state the time duration. The skin protectants are not reimbursed by National Health Insurance in Taiwan and the economic burden may result in difficult implementation. In addition, Beeckman et al.16 performed an IAD intervention study – control group: perineal skin care using water and pH-neutral soap; experimental group: use of a 3-in-1 washcloth. The results showed that the use of a 3-in-1 washcloth decreased IAD prevalence. The effectiveness of IAD cleaning products and protectants was confirmed17,18. Therefore, we recommend that the reimbursement of IAD cleaning products and protectants could be included by the National Health Insurance to decrease economic burdens for patients and shorten skin care hours.
In the supportive care, the experts recommended that high-risk patients and individualised care needed to be more specific. The interventions should be implemented, including repositioning and use of pressure-redistributing devices to decrease the exposure of the buttocks to a moist environment1. The use of a soft or cotton cloth to avoid damage by abrasion was recommended by experts in the study and in the previous research12.
In the AGREE evaluation, the score of applicability domain was the lowest, a standardised score of 51.9%. Therefore, the further study would focus on the potential organisational barriers and potential cost implications of applying the IAD care bundle guideline. The IAD bundle care guideline was developed and evaluated at the initial stage.
Limitations
There are important limitations to this study. First, the study was conducted in a medical centre, therefore our findings may not be generalisable to long-term care institutions. A second limitation is a reliable and valid instrument for the assessment of IAD, although the IAD severity grading tool in the study was recognised by the 2015 Global IAD Expert Panel. The assessment tool needs to be developed and evaluated for level of agreement and stability among users. Finally, a further study is needed to develop the interventions based on the various degrees of severity, accompanied with photographic flow charts to increase the feasibility of IAD care bundle guideline in a busy clinical setting.
Conclusions
The development of a bundle care guideline first used an evidence-based framework, including a systematic review, categories of interventions, consensus of clinical experts and nurse staff as well as evaluation of methodological experts. The IAD bundle care guideline consisted of four aspects and 19 interventions to prevent and treat skin breakdown associated with incontinence and further prevent pressure ulcers. In the future, an experimental design is needed to evaluate the efficacy of this IAD bundle care guideline. Moreover, the readability, feasibility and applicability of this initial guideline will be refined and re-evaluated to promote the clinical practice and efficacy in the further study.
Conflict of Interest
The authors declare no conflicts of interest.
Funding
This research was supported by the Chi Mei Medical Center, Taiwan (Grant Number: CMHCR10435).
使用循证框架开发的失禁相关性皮炎预防组合
Hsiu Hui Wei, Chih-Ling Huang, Wen-Pei Huang and Hsiu-Chin Chen
DOI: https://doi.org/10.33235/wcet.40.3.37-42
摘要
背景 失禁相关性皮炎(IAD)是临床环境中皮损的一个流行的病因。IAD可能引起热觉、瘙痒、疼痛和感染,以及住院时间延长和医疗成本增加。
目的 本研究旨在以循证框架为基础为IAD制定组合式护理指南。
方法 进行三个步骤:起草一份IAD组合式护理指南,获得医院护理人员和临床专家的共识,以及由方法学专家进行评价。
结果 初始指南由30位护士和7位临床专家(两轮)批准,获得了超过80%的同意。三位方法学专家评价了制定过程的质量,建议使用。IAD组合式护理指南包括四个方面(皮肤评估、皮肤清洁、皮肤保护和支持性护理),涉及19种干预。IAD组合式护理指南是标准化且基于证据的。
结论 制定的IAD组合式护理指南结合了系统性文献综述的信息和护士、临床专家和方法学专家的意见,建议临床应用。将实施进一步研究来验证它的有效性。
引言
失禁相关性皮炎(IAD)是临床环境中皮损的一个流行的病因。IAD可能引起热觉、瘙痒、疼痛和感染,以及住院时间延长和医疗成本增加1。台湾的一项横断面研究发现IAD的患病率为26.3%,较高比例的病例发生在住院期间2。美国急性医院获得性IAD的发生率为45.7%,IAD与骶骨压力性损伤的患病率显著增加有关3。一旦发生IAD,应提供实证护理,以缩短愈合时间,防止并发症的发生4。IAD评估和标准护理在不同组织中不一致,需要进行开发5。在先前的研究中对IAD护理进行了系统性综述6。该综述包括四个方面的IAD预防和治疗干预(皮肤评估、皮肤清洁、皮肤保护和支持性护理)。
医疗保健改进研究所引入了组合式护理的概念,以提高护理质量7。在本研究中,以循证方法为指导,开发了一套结合了四个方面干预的IAD护理组合。该方法包括系统性综述、集束化循证干预和临床实践评价。Gray等人建议道,实施标准化策略会促进IAD预防和管理与实践的结合,以便预防和治疗IAD8。干预综述表明,缺乏一致的循证IAD预防和干预9,并且一些试验主要针对皮肤护理产品和操作10。尽管先前的一项研究包括IAD评估、预防和管理策略11,但这些都缺乏实证IAD组合式护理指南。因此,本研究旨在以循证框架为基础为IAD制定组合式护理指南。
本综述中包括的试验测试了皮肤护理产品、操作和使用皮肤护理产品的频率。
方法
在系统性综述中,数据库包括护理与联合卫生文献累积索引、PubMed、考克兰图书馆、乔安娜布里格斯研究所、美国国家临床指南中心和最佳实践指南。关键词包括失禁相关性皮炎(incontinence-associated dermatitis)或尿失禁病变(incontinence lesion)与皮肤护理、预防和干预(skin care and prevention and intervention)。总共抽取了27篇文章来评价证据质量。初步组合式护理指南包括四大方面(皮肤评估、皮肤清洁、皮肤保护和支持性护理)以及最初的20项护理活动6。
首先,对护理指南进行专家效度检验。由5名伤口和造口护士使用四分制李克特量表对指南的重要性、适用性和文本明晰性进行审查和评分。接下来,由30名2级及以上的高级专业级别的临床护士、7名临床专家和研究人员、以及3名方法学专家对护理指南进行内容审查(图1)。
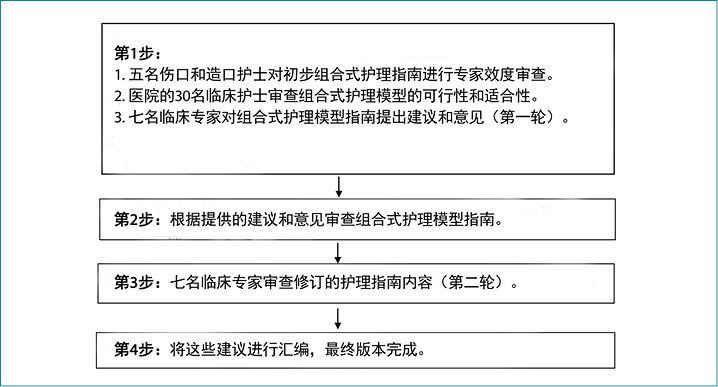
图1. IAD组合式护理指南制定的流程图
临床护理人员和临床专家进行实际审查,并根据实施的可行性和适用性对护理活动进行评分。评分为从4(同意)到 1(不同意)和0(不适用)。对于“不同意”和“不适用”的项目,必须提供具体的建议。护理活动必须达到80%的赞成率。同时,三名方法学专家根据指南研究与评价(AGREE)12的六个质量领域(范围和目的、利益相关者的参与、制定的严谨性、表达的明晰性、适用性和编辑独立性)对内容进行了审查,以评估指南总体,并对IAD组合式护理指南的研究质量和严谨性进行审查12。计算每个领域的最大可能评分的百分比。通过将领域中各个条目的所有评分相加来计算领域评分。
结果
初步组合式护理指南的内容效度指数≥0.8。在对护理指南的实施可行性进行的第一轮内容严谨性审查中,20个问题中有18个获得了30名临床护士中至少80%的赞成。每天记录粪便的特征和数量(同意率为60.1%),采用半俯卧位,一天两次(66.7%)关于实施的适用性,19个问题获得≥80%的赞同,每天记录粪便特征的同意率为76.6%。这一条目在专家审查中获得100%的同意,随后未作修订。临床专家提到,本研究中的IAD评估量表非常复杂,临床实践的有效性有限。
临床护理人员的总体评价和建议如下:
• 可以在IAD评估表中添加更多图片。
• 高危患者可以突出显示。
• 粪便评估可以翻译成中文,方便评价者阅读和使用。
• 皮肤清洁可以每天进行一次,也可以在大便或排尿后进行。
• 皮肤清洁液或保护剂所涉及的费用给家庭带来了经济负担。
• 一些家庭成员或照护者可能持有自己的观点,不依从健康教育的护理指导。
• 对于患有关节强硬、肢体挛缩或其他限制的患者,可能不建议采用一天两次的半俯卧位,因此患者的体位可以根据个人情况而定。
在七名临床专家的第一轮共识结果中,列出的20种干预中有6种没有获得80%的赞同(表1)。作者对文献进行了检索和综述,然后对这些条目进行了修订。在第二轮共识审查中,所有条目获得≥80%的赞同。表2显示了方法学专家审查的六个组成部分的结果。提供的建议如下:
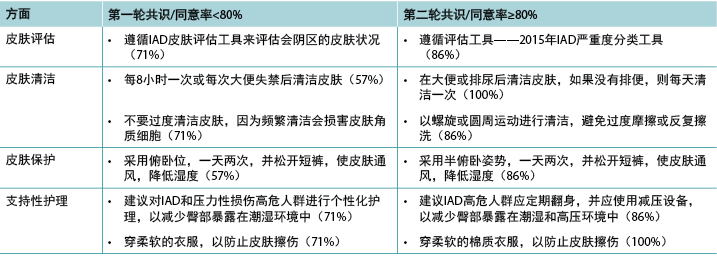
表1.七位临床专家对组合式护理指南的共识结果
• 可以使用易于理解的卡片或小册子来制定组合式护理指南,以便于折叠和阅读。
• 此版本的组合式护理指南和建议适用于护士。未来会制定照护者版本。
• 条目需要明晰和修订,以提高可读性和可行性。表2显示适用性领域的评分最低,标准化评分为51.9%。
表2.方法学专家进行的质量领域评估
最后,专家提供的建议已包含在组合式护理指南的最终版本中。由于与“2.3……避免过度摩擦或反复擦洗”相似,因此删除了一种清洁活动干预,保留了19种干预(表3)。组合式护理指南不包括新的护理技术;相反,它包括从专家和研究方法学家处获得的干预。制定了一套系统性、结构化且具有良好严谨性的组合式护理指南。本组合式护理指南与过去的护理标准或方案之间的差异如下:
• 护理指南由四个方面(皮肤评估、皮肤清洁、皮肤保护和支持性护理)组成。该组合式指南的特点是循证实施和已得到临床专家确认的临床实践的可行性。
• 皮肤评估包括时间和工具。
• 除了排尿或大便后的皮肤清洁外,指南中添加了清洁会阴区皮肤至少一次。
• 指南在皮肤保护部分添加了对非完整皮肤的实证干预。
表3. IAD的组合式护理指南
讨论
在本研究中,首先使用循证框架制定了一种IAD组合式护理指南,以促进实施的可行性和应用。护理指南的修订版包括四个组成部分(19种干预):皮肤评估(五个条目)、皮肤清洁(四个条目)、皮肤保护(六个条目)和支持性护理(四个条目)。现有IAD评估量表非常复杂,包括皮肤皲裂(0-3分)、皮肤发红(0-3分)和糜烂(0–4分)等领域13。
因此,作者建议使用基于2015年全球IAD专家小组建议而提出的IAD严重度分级工具。该评估工具可用于0-2级损伤严重度的简单区分;等级越高,损伤越严重11。文献表明,此分级工具和护理方案的组合可用于质量监测和研究。尽管对该工具进行了专家效度审查,但其可靠性仍有待研究10,11。2016年,台湾研究人员使用图片卡修订了这一严重度分级、评价工具和预防性干预,以提高临床适用性和照护者对护理指南的依从性14。此外,IAD评估工具和Braden量表可以在进一步的研究中结合使用,以整合完整皮肤护理的干预2。
关于白班中会阴区每日清洁的标准和具体清洁方法的需求,作者考虑了夜班中患者的休息时间和护患比,建议改变清洁部分中的清洁时间和方法。在初始指南中,“反复清洁或用力清洁是皮肤损伤的直接原因”这一陈述需要删除,因为没有相关文章量化清洁或反复擦洗的次数和强度1,15。
在皮肤保护部分中,没有相关文献提供半俯卧位持续时间的证据。因此,将干预修订为不声明持续时间。台湾的国民健康保险不报销皮肤保护剂的费用,经济负担可能会导致实施困难。此外,Beeckman等人16进行了一项IAD干预研究–对照组:使用水和pH中性肥皂护理会阴皮肤;实验组:使用3合1毛巾。结果表明,使用3合1毛巾可以降低IAD患病率。这证实了IAD清洁产品和保护剂的有效性17,18。因此,我们建议将IAD清洁产品和保护剂的报销纳入国民健康保险,以减轻患者的经济负担,缩短皮肤护理时间。
在支持性护理中,专家建议高危患者和个性化护理的表述需要更加具体。应实施干预,包括重新调整体位和使用压力再分布器械,以减少臀部暴露在潮湿环境中1。在这项研究和先前的研究中,专家建议使用软布或棉布,以避免擦伤造成的皮损12。
在AGREE评价中,适用性领域的评分最低,标准化评分为51.9%。因此,进一步的研究将集中研究应用IAD护理组合指南的潜在组织障碍和潜在成本影响。在初始阶段制定并评价了IAD组合式护理指南。
局限性
本研究存在重大的局限性。首先,这项研究是在一个医疗中心进行的,因此我们的研究结果可能不适用于长期护理机构。第二个局限性是用于IAD评估的工具的信度和效度,不过本研究中的IAD严重度分级工具得到了2015年全球IAD专家小组的认可。评估工具需要进行有关用户间同意度和稳定性的开发和评价。最后,需要进行进一步的研究来开发基于不同严重度的干预措施,并附上带照片的流程图,以增加IAD护理组合指南在繁忙的临床环境中的可行性。
结论
组合式护理指南的制定首先使用循证框架,包括系统性综述、干预分类、临床专家和护理人员的共识以及方法学专家的评价。IAD组合式护理指南包括4个方面和19种干预,目的是预防和治疗与失禁相关的皮肤皲裂,并进一步预防压疮。将来,需要使用一个实验性研究设计来评价该IAD组合式护理指南的有效性。此外,本初步指南的可读性、可行性和适用性将进一步优化和重新评价,以促进临床实践和进一步研究中的有效性。
利益冲突
作者声明没有利益冲突。
资助
该研究得到了台湾奇美医疗中心的支持(基金编号:CMHCR10435)。
Author(s)
Hsiu Hui Wei
RN, MSN, CWOCN
Department of Nursing, Chi Mei Medical Center, Tainan City, Taiwan
Chih-Ling Huang
RN, PhD
Professor, Department of Nursing, Fooyin University, Kaohsiung, Taiwan
Wen-Pei Huang
RN, PhD student, CWOCN
Department of Nursing, Chi Mei Medical Center, Tainan City, Taiwan
Hsiu-Chin Chen*
RN, PhD
Chief Director of Nursing, Chi Mei Medical Center, Tainan, Taiwan
Assistant Professor, Department of Senior Services, Southern Taiwan University of Science and Technology, Tainan, Taiwan
Email 300006@mail.chimei.org.tw
* Corresponding author
References
- Beeckman D, Van Lancker A, Van Hecke A, Verhaeghe S. A systematic review and meta-analysis of incontinence-associated dermatitis, incontinence, and moisture as risk factors for pressure ulcer development. Res Nurs Health 2014 June;37(3):204–218.
- Shiu SR, Hsu MY, Chang SC, Chung HC, Hsu HH. Prevalence and predicting factors of incontinence-associated dermatitis among intensive care patients. JNHR 2013 Sep;9(3):210–217.
- Gray M, Giuliano KK. Incontinence-associated dermatitis, characteristics and relation to pressure injury: a multisite epidemiologic analysis. J Wound Ostomy Continence Nurs 2018 Jan/Feb;45(1):63–67.
- Payne D. Incontinence associated dermatitis: reducing the risk. NRC 2015 Mar;17(3):144–149.
- Beeckman D, Woodward S, Gray M. Incontinence-associated dermatitis: step-by-step prevention and treatment. Br J Community Nurs 2011 Aug;16(8):382–389.
- Wei HH. To develop the bundle care of the incontinence associated dermatitis in disabled patients: a evidence-based framework. Tainan City, Taiwan: Chang Jung Christian University, Department of Nursing; 2016.
- Resar R, Griffin FA, Haraden C, Nolan TW. Using care bundles to improve health care quality. IHI Innovation Series white paper. Cambridge, Massachusetts: Institute for Healthcare Improvement; 2012. Available from: http://www.IHI.org
- Gray M, McNichol L, Nix D. Incontinence-associated dermatitis: progress, promises, and ongoing challenges. J Wound Ostomy Continence Nurs 2016 Mar–Apr;43(2):188–192.
- Ousey K, O’Connor L. Incontinence-associated dermatitis made easy. Wounds UK 2017 Mar;13(1):1–6. Available from: http://www.wounds-uk.com
- Beeckman D, Van Damme N, Schoonhoven L, Van Lancker A, Kottner J, Beele H et al. Interventions for preventing and treating incontinence-associated dermatitis in adults. Cochrane Database Syst Rev 2016 Nov 10;11(11):CD011627.
- Beeckman D, Campbell J, Campbell K, Chimentao D, Coyer F, Domansky R et al. Incontinence associated dermatitis: moving prevention forward. Proceedings of the Global IAD Expert Panel. Wounds International; 2015 Feb 13. Available from http://www.woundsinternational.com.
- Brouwers M, Kho ME, Browman GP, Cluzeau F, Feder G, Fervers B et al. AGREE II: advancing guideline development, reporting and evaluation in health care. Can Med Assoc J 2010 Dec;182:E839–842. doi:10.1503/cmaj.090449
- Kennedy KL, Lutz L. Comparison of the efficacy and cost effectiveness of three skin protectants in the management of incontinent dermatitis. Proceedings of the European Conference on Advances in Wound Management; 1996 October 4.
- Hsu MY, Lin YC, Chen YJ. Prevention and photo classification treatment for incontinence-associated dermatitis. Tzu Chi Nurs J 2016;15(5):60–63.
- Cowdell F, Jadotte YT, Ersser SJ, Danby S, Walton S, Lawtone S et al. Hygiene and emollient interventions for maintaining skin integrity in older people in hospital and residential care settings. Cochrane Database Syst Rev 2014 Dec;12:CD01137. doi:10.1002/14651858. CD01137.pub1.
- Beeckman D, Verhaeghe S, Defloor T, Schoonhoven L, Vanderwee K. A 3-in-1 perineal care washcloth impregnated with dimethicone 3% versus water and pH neutral soap to prevent and treat incontinence-associated dermatitis: a randomized, controlled clinical trial. J Wound Ostomy Continence Nurs 2011 Nov–Dec;38(6):627–634.
- Brennan MR, Milne CT, Agrell-Kann M, Ekholm BP. Clinical evaluation of a skin protectant for the management of incontinence-associated dermatitis: an open-label, nonrandomized, prospective study. J Wound Ostomy Continence Nurs 2017 Mar/Apr;44(2):172–180.
- Kon Y, Ichikawa-Shigeta Y, Iuchi T, Nakajima Y, Nakagami G, Tabata K et al. Effects of a skin barrier cream on management of incontinence-associated dermatitis in older women: a cluster randomized controlled trial. J Wound Ostomy Continence Nurs 2017 Sep/Oct;44(5):481–486.


