Volume 40 Number 4
Leakage and peristomal skin complications influences user comfort and confidence and are associated with reduced quality of life in people with a stoma
Chris Juul Hedegaard, Teresa Adeltoft Ajslev, Rikke Zeeberg and Anne Steen Hansen
Keywords quality of life, stoma, leakage of stomal effluents, peristomal skin complications
For referencing Hedegaard CJ et al. Leakage and peristomal skin complications influences user comfort and confidence and are associated with reduced quality of life in people with a stoma. WCET® Journal 2020;40(4): 23-29.
DOI https://doi.org/10.33235/wcet.40.4.23-29
Abstract
Objective The purpose of the research was to investigate how leakage of stomal effluent and peristomal skin complications (PSC) affects the quality of life (QoL) of people living with a stoma.
Method Data were collected from an online questionnaire sent out to approximately 20,000 people living with a stoma. The validated Ostomy-Q scale was used to measure changes in QoL.
Results More than 4,200 people from 13 countries completed the study between 30 August and 3 October 2016. Leakage had a statistically significant impact on the QoL for participants who experienced leakage four times (or more) out of ten baseplates changes. All four domains in the Ostomy-Q scale – confidence in stoma appliance, comfort, discretion and socialising – were affected. Also, people with PSC had a significantly lower QoL than those who had not experienced PSC in the 6 months before the survey. PSC impacted the confidence and comfort domains significantly. The discretion and socialising domains were also significantly affected by PSC but were below the pre-defined limit for a minimal important difference.
Conclusion The data support that leakage and PSC have a significant physical and psychological impact on people living with a stoma.
Introduction
Leakage is a major concern for people living with a stoma. Up to 87% experience leakage of stomal effluent (output) underneath their baseplate1,2. The consequences of leakage are two-sided, with both a psychological and physical impact on everyday life. The psychological impact is seen by the fact that the majority of people with a stoma (91%) worry about leakage2. The physical burden includes irritant contact dermatitis (ICD) which is one type of peristomal skin complication (PSC)3. PSC is associated with a general feeling of discomfort4. Stoma care nurses in the UK reported that more than 60% of their patients showed signs of PSC and 86% of these cases were due to leakage problems4. Stomal effluents in contact with the peristomal skin is believed to cause ICD3. ICD is a very common problem among people with a stoma as seen in a recent survey, where 49% reported incidents of ICD5.
Reducing leakage and improving peristomal skin health was observed to increase quality of life (QoL) in stoma patients suffering from PSC caused by leakage6. A thorough understanding of which underlying parameters are directly associated with QoL remains to be established. The aim of this research was to investigate the relation between output leakage, PSC and QoL and explore if the stoma-related QoL domains – confidence, comfort, discretion and socialising – contribute to these associations.
Methods
Survey methodology was described by Voegeli et al.5 In brief, an online, retrospective, self-reported questionnaire was sent to 19,555 people with a stoma in 13 countries on four continents. Data were collected from 30 August to 3 October 2016. The inclusion criteria were age above 18 years, and having at least one stoma of any type. Respondents who did not complete the survey, who answered ‘Don’t know’ to more than 30% of the questions, or who completed all questions very quickly (within 15 minutes) were excluded from the population. Besides demographics and data on the incidence of PSC (reported by Voegeli et al.5), the survey contained questions on QoL, leakage frequency (leakage incidence within the respondents’ last ten changes of baseplate), and worry of leakage (using a five point Likert scale) that has not been reported previously. The Ostomy-Q scale was used to estimate product-related QoL, a scale which consists of four domains – confidence, comfort, discretion and socialising7. Out of the study population of 4,235 included in the survey (response rate of 22%), 3,638 respondents completed the Ostomy-Q questionnaire (final response rate of 19%).
For statistical analysis, JMP® (Version 13.1. SAS Institute Inc., Cary, NC, 1989–2019) was used. Tukey-Kramers HSD test was used for leakage, and Student’s t-test was used for PSC when analysing statistical difference between levels. Besides statistical difference (p<0.05), a threshold for clinical relevance, the so-called minimal important difference (MID), was defined, so any difference in total QoL between two levels had to be >5.75; and, for the domains, >2.75 for comfort, >2.51 for confidence, >2.54 for discretion and >2.60 for social life7.
Ethical considerations
The survey was a market research study approved by an internal review board. Participation was on a voluntary basis with informed consent. The patients’ data were treated with confidentiality in compliance with the EU General Data Protection Regulation, and data analysis was performed with aggregated anonymous data. There was no intervention nor change in treatment.
Results
The survey population included 46% women, and 66% of the respondents were 60 years or older (Table 1). Colostomy (44%) was the most common type of reported stoma, followed by ileostomy (38%) and urostomy (15%) (Table 1). Output under the baseplate (i.e. leakage) observed during the last ten baseplate changes was reported among 83% of respondents, with 26% reporting leakage during their last seven baseplate changes (Table 1). Furthermore, 73% of the respondents reported to have experienced PSC within the last 6 months (Table 1; also reported in Voegeli et al.5).
Table 1. Participant demographics
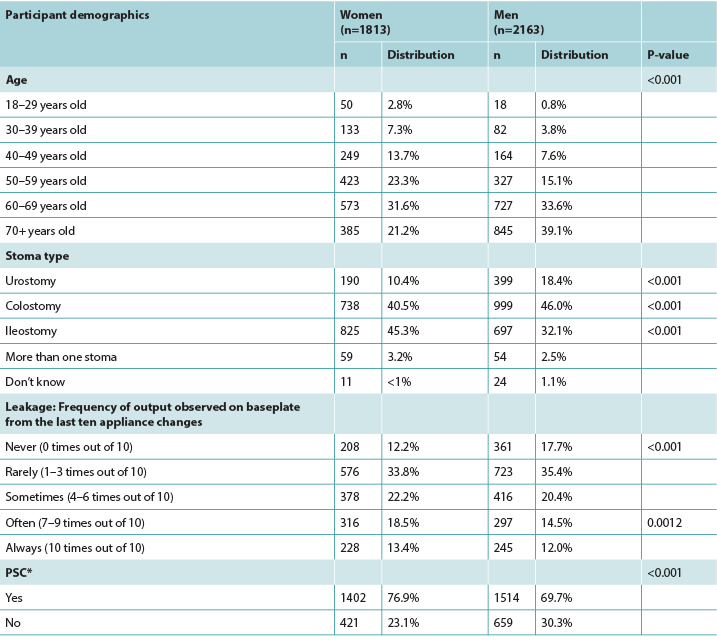
* Based on recall of at least one PSC experience within the last 6 months5
Leakage and QoL
Overall, a stepwise decline in total QoL by each increase in leakage frequency was observed until a plateau was reached, i.e. for those who often or always experienced leakage (seven times or more out of the last ten baseplate changes) (Figure 1). Though the decline in QoL by increased frequency in leakage was statistically significant, the decline in QoL was only clinically relevant when four or more times out of ten baseplates showed signs of leakage (Figure 1).
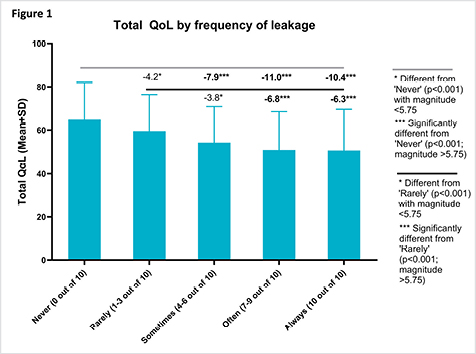
Figure 1. The influence of output under baseplate (leakage) on total QoL
Respondents reported if they experienced output underneath their baseplate during their last ten baseplate changes and completed the Ostomy-Q questionnaire (n=3,638).
(–) Levels compared to Never observing leakage.
(–) Levels compared to Rarely observing leakage.
*Statistically significant difference observed (p<0.001), but with a magnitude less than the clinically relevant MID (<5.75)
*** Difference observed is statistically significant (p<0.001) and greater that the clinically relevant MID (>5.75).
Of the four domains in Ostomy-Q scale, the domain on confidence in stoma appliance was significantly impacted when the frequency of leakage to baseplate was higher than three times out of ten baseplate changes as compared to ‘never’ (p<0.0001; Figure 2A). Leakage also impacted the Ostomy-Q domains of comfort, discretion and socialising; the comfort and discretion domains were impacted when respondents experienced leakage more than six times during the last ten baseplate changes (Figures 2B&C). Leakage also had an impact on social life, but only in the group of respondents who reported leakage on all (ten times out of the last ten baseplate changes) recent baseplate changes (Figure 2D).
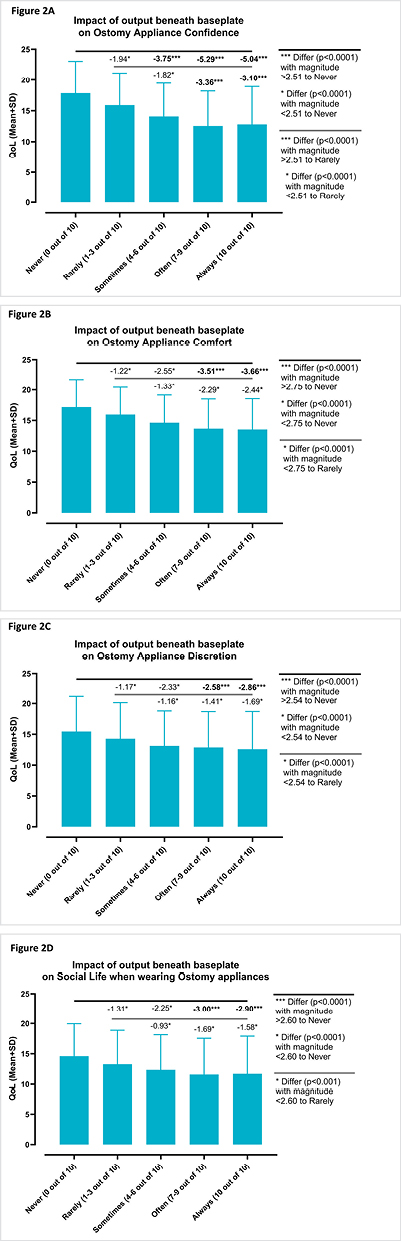
Figure 2. The influence of output under baseplate (leakage) on the domains of Ostomy-Q: (A) confidence, (B) comfort,
(C) discretion and (D) socialising
Respondents reported if they experienced output underneath their baseplate during their last ten baseplate changes and completed the Ostomy-Q questionnaire (n=3,638).
(–) Levels compared to Never observing leakage.
(–) Levels compared to Rarely observing leakage.
* Statistically significant difference observed (p<0.001), but with a magnitude less than the clinically relevant MID
*** Difference observed is statistically significant (p<0.001) and greater that the clinically relevant MID.
PSC and QoL
Respondents who reported skin issues had significantly lower QoL than those who did not experience skin issues during the previous 6 months before the survey (p<0.001; Figure 3).
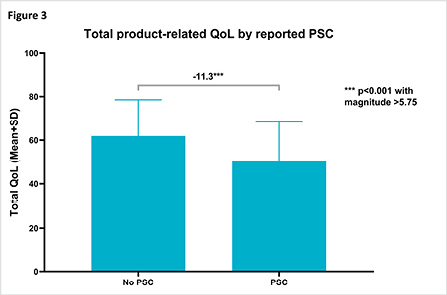
Figure 3. The influence of PSC on total QoL
Respondents reported if they had experienced PSC during the 6 months prior to completing the Ostomy-Q questionnaire (n=3,638).
(–) Levels (PSC no/yes) compared to each other.
*** Difference observed is statistically significant (p<0.001) and greater that the clinically relevant MID (>5.75).
PSC impacted the confidence and comfort domains significantly (p<0.001; Figures 4A&B). Likewise, PSC impacted the discretion and socialising domains significantly (p<0.001), although the difference was below the pre-defined limit for a minimal important difference (Figures 4C&D).
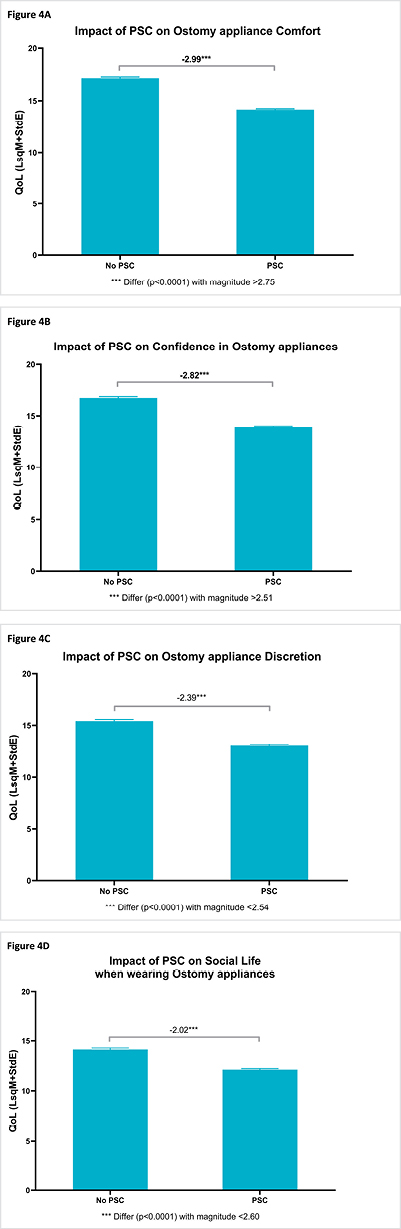
Figure 4. The influence of PSC on the domains of Ostomy-Q: (A) comfort, (B) confidence, (C) discretion and (D) socialising
Respondents reported if they had experienced PSC during the 6 months prior to completing the Ostomy-Q questionnaire (n=3,638).
(–) Levels (PSC no/yes) compared to each other.
*** Difference observed is statistically significant (p<0.001) and greater that the clinically relevant MID (>5.75).
Discussion
Our data show that there is a clear relation between leakage incidences and reported QoL; subjects who experience leakage to four or more baseplates out of the last ten baseplate changes had a significantly lower total QoL. Leakage has previously been reported to have both emotional and physical implications – the emotional impact was recorded by Nafees et al.8 in which the authors developed a scale for measuring the impact of leakage on domains such as emotional, socialising, and coping and control – but people’s experience and its impact is not well understood.
This study aimed to establish a definition of leakage through clinical and user input. This information was used to develop and validate a new measurement tool to understand the impact of leakage for people using a stoma appliance in the UK, US, France and Denmark. Participants were recruited from a panel of users, hosted by Coloplast, that included people who currently use Coloplast products. Six clinicians and 41 users took part in concept elicitation interviews. The qualitative findings were used to draft items. A panel of clinical experts was organised to develop and validate items (n=6). The impact of leakage became significantly more important when stomal output reached outside the baseplate area and onto the participants’ clothes8. As our data suggests, even if the output stays inside the baseplate area it appears to have an impact on QoL as the users lose confidence in their stoma appliances.
It is not known whether the high reporting of leakage incidences is influenced by a lack of compliance or knowledge of users in how to avoid leakages. However, if the numbers do reflect that users struggle with managing their stoma appliance, there may be room for preventing poor QoL by advising users on good stoma care practice. The lack of comfort and confidence may also be impacted by the physical implications of the leakage. As the output from ostomies contain digestive enzymes9–11, faeces can cause ICD which is the most common type of PSC5,12. Thus, leakage and PSC appear to negatively impact total QoL by impacting the domains of confidence in and comfort of the stoma appliance. In the present study, users were asked to recall any skin issue during the last 6 months to ensure to capture all users who struggle with skin problems from time to time, and QoL was only measured at one timepoint. Thus, due to the limitations of the present study with cross-sectional data collection, it is not possible to point to a causal relationship between PCS and QoL. However, in a previous prospective study, lower QoL was also observed in patients suffering from PSC6.
Conclusion
The data support that leakage has a significant physical and psychological impact on people living with a stoma. Thus, prevention of leakage incidents has the potential to improve QoL, including the domains of comfort and confidence, as well as reduce PSC. Moreover, as almost all respondents expressed a worry of leakage, and as leakage impacts confidence in stoma appliances, these results warrant for solutions that can enforce confidence by reducing the worry of leakage.
Ethics
The survey was carried out as market research and was approved by an internal review board.
Acknowledgements
We would like to thank Senior Biostatistician Helle Doré Hansen and Head of Evidence and Education Anni Rønfeldt Thomsen for their assistance.
Conflict of interest
All authors are employees of Coloplast A/S.
Funding
The article was funded entirely by Coloplast A/S.
渗漏和造口周围皮肤并发症影响用户舒适度和信心并且降低造口患者的生活质量
Chris Juul Hedegaard, Teresa Adeltoft Ajslev, Rikke Zeeberg and Anne Steen Hansen
DOI: https://doi.org/10.33235/wcet.40.4.23-29
摘要
目的 本研究旨在了解造口渗出液渗漏和造口周围皮肤并发症(PSC)如何影响造口患者的生活质量(QoL)。
方法 向大约20,000名造口患者发送了在线问卷并从中收集数据。使用经过确认的造口患者生活质量(Ostomy-Q)量表测量QoL变化。
结果 2016年8月30日至10月3日,来自13个国家的4,200多名造口患者完成了研究。对于十次底盘更换中经历了四次(或更多次)渗漏的参与者而言,渗漏对QoL的影响具有统计学意义。造口患者生活质量量表的所有四个领域(对造口装置的信心、舒适度、自主性和社交)均受到了影响。而且,出现PSC患者的QoL显著低于那些在调查前6个月未发生PSC的患者。PSC对信心和舒适度领域有显著影响。自主性和社交领域也受到了PSC的显著影响,但低于最小重要性差值的预定义下限。
结论 数据证明,渗漏和PSC对造口患者的生理和心理具有显著影响。
引言
渗漏是造口患者的一个大问题。多达87%的患者经历了底盘下方造口渗出液(排出物)渗漏1,2。渗漏的后果是两方面的,会在心理和生理方面均对日常生活造成影响。心理影响表现在大多数造口患者(91%)担心渗漏2。生理负担包括刺激性接触性皮炎(ICD),这是一种造口周围皮肤并发症(PSC)3。PSC会造成全身性不适感4。英国的造口护理护士报告称,超过60%的患者显示了PSC征象,而这些病例中有86%是由于渗漏问题4。有研究认为造口渗出液接触造口周围皮肤导致了ICD3。最近的一项调查显示,ICD在造口患者中是一个非常普遍的问题,其中49%报告了ICD事件5。
观察发现,减少渗漏和改善造口周围皮肤健康可提高遭受渗漏导致的PSC的造口患者的生活质量(QoL)6。而对于与QoL直接相关的基本参数,仍有待进一步深入了解。本研究旨在了解排出物渗漏、PSC和QoL之间的关系并探索造口相关的QoL领域(信心、舒适度、自主性和社交)是否对这些关系产生了影响。
方法
Voegeli等人5 描述了调查方法。简而言之,向来自四大洲13个国家的19,555例造口患者发送了一份回顾性自评在线问卷。收集了2016年8月30日至10月3日的数据。纳入标准如下:18岁以上,且至少拥有一个任意类型的造口。未完成调查、对超过30%的问题回答“不知道”或很快(在15分钟内)完成所有问题的受访者被排除在人群之外。除了人口统计学数据和有关PSC发生率的数据(由Voegeli等人5报告),该调查还包含有关以下方面的问题:QoL、渗漏频率(受访者最近十次底盘更换内的渗漏发生率)和先前未报告过的对于渗漏的担忧(使用五点李克特量表)。使用造口患者生活质量量表估计产品相关的QoL,这是一种由四个领域(信心、舒适度、自主性和社交)组成的量表7。在调查纳入的4,235名研究人群中(22%的应答率),3,638名受访者完成了造口患者生活质量问卷(19%的最终应答率)。
对于统计分析,使用了JMP®(版本13.1. SAS Institute Inc.,北卡罗来纳州凯里,1989-2019)。在分析不同水平之间的统计学差异时,渗漏采用Tukey-Kramer HSD检验,PSC采用 Student t检验。除了统计学差异(p<0.05),还定义了临床相关性阈值,即所谓的最小重要性差值(MID),所以两个水平之间总QoL的任何差异必须>5.75;且,对于领域而言,舒适度领域必须>2.75,信心领域必须>2.51,自主性领域必须>2.54,社交生活领域必须>2.607。
伦理事宜
本调查为一项经内部审查委员会批准的市场调查研究。以自愿参与为基础,并签署了知情同意书。根据欧盟《通用数据保护条例》,对患者数据进行保密处理,并对汇总的匿名数据进行数据分析。治疗中无干预和改变。
结果
调查人群包括46%的女性,且66%的受访者为60岁或60岁以上(表1)。报告的造口中最常见的类型是结肠造口(44%),其次是回肠造口(38%)和尿道造口(15%)(表1)。83%的受访者报告称,在最近十次底盘更换过程中观察到了底盘下方存在排出物(即渗漏),26%报告在其最近七次底盘更换过程中出现渗漏(表1)。此外,73%的受访者报告在最近6个月内经历了PSC(表1;Voegeli等人5也报告了这一点)。
表1.参与者人口统计学数据
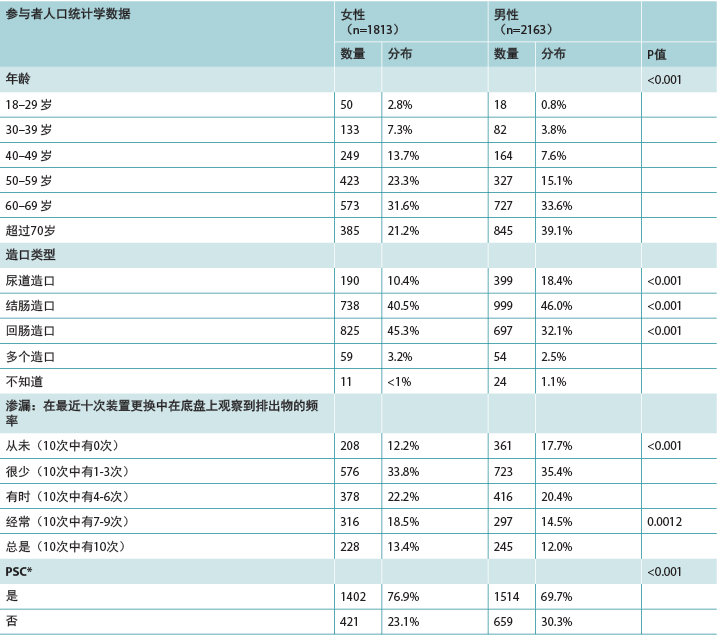
* 基于回想到最近6个月内的至少一次PSC经历5
渗漏和QoL
总体而言,观察发现,总QoL随着渗漏频率的每次增加而逐步下降,直至达到平稳状态,即对于那些经常或总是经历渗漏的人(最近十次底盘更换中有七次或更多次)(图1)。尽管渗漏频率增加造成的QoL下降具有统计学意义,但是仅当十次底盘更换中有四次或更多次显示出渗漏征象时,QoL的下降才具有临床相关性(图1)。
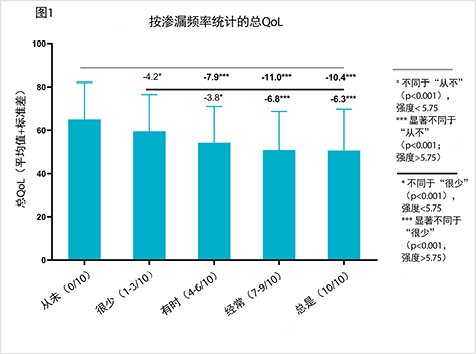
图1.底盘下方存在排出物(渗漏)对总QoL的影响
受访者报告他们在最近十次底盘更换过程中是否经历了底盘下方存在排出物的情况,并完成了造口患者生活质量问卷(n=3,638)。
(–) 与“从未”观察到渗漏相比的水平。
(–)与“很少”观察到渗漏相比的水平。
*观察到的差异具有统计学意义(p<0.001),但是强度小于临床相关性MID(<5.75)
***观察到的差异具有统计学意义(p<0.001)且大于临床相关性MID(>5.75)。
在造口患者生活质量量表的四个领域中,当与“从未”比较,底盘渗漏频率高于十次底盘更换中有三次时,对造口装置的信心这一领域受到了显著影响(p<0.0001;图2A)。渗漏还影响了造口患者生活质量的舒适度、自主性和社交领域;当受访者在最近十次底盘更换过程中经历了六次以上的渗漏时,舒适度和自主性领域受到影响(图2B&C)。渗漏还影响社交生活,但仅在报告最近所有(最近十次底盘更换中有十次)底盘更换中均有渗漏的受访者中(图2D)。
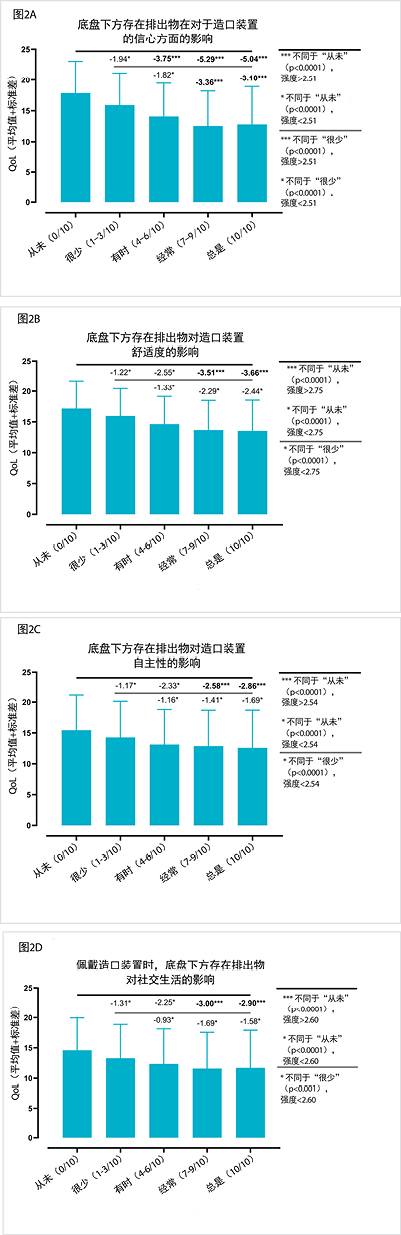
图2.底盘下方存在排出物(渗漏)对造口患者生活质量各个领域的影响:(A)信心、(B)舒适度、(C)自主性和(D)社交
受访者报告他们在最近十次底盘更换过程中是否经历了底盘下方存在排出物的情况,并完成了造口患者生活质量问卷(n=3,638)。
(–) 与“从未”观察到渗漏相比的水平。
(–) 与“很少”观察到渗漏相比的水平。
* 观察到的差异具有统计学意义(p<0.001),但是强度小于临床相关性MID
*** 观察到的差异具有统计学意义(p<0.001)且大于临床相关性MID。
PSC和QoL
报告皮肤问题的受访者的QoL显著低于那些在调查前6个月期间未经历皮肤问题的受访者(p<0.001;图3)。
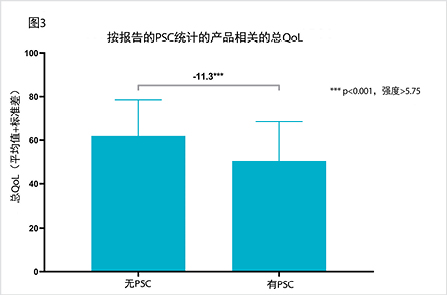
图3.PSC对总QoL的影响
受访者报告他们在完成造口患者生活质量问卷前6个月期间是否经历了PSC(n=3,638)。
(–) 相互比较的水平(有/无PSC)。
*** 观察到的差异具有统计学意义(p<0.001)且大于临床相关性MID(>5.75)。
PSC对信心和舒适度领域有显著影响(p<0.001;图4A&B)。同样,PSC对自主性和社交领域有显著影响(p<0.001),不过差异低于最小重要性差值的预定义下限(图4C&D)。
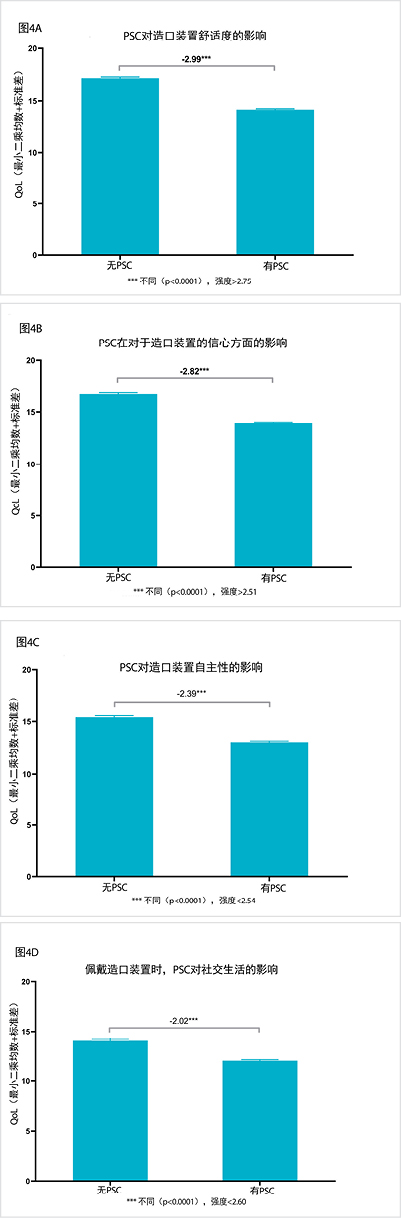
图4.PSC对造口患者生活质量各个领域的影响:(A)舒适度、(B)信心、(C)自主性和(D)社交
受访者报告他们在完成造口患者生活质量问卷前6个月期间是否经历了PSC(n=3,638)。
(–) 相互比较的水平(有/无PSC)。
*** 观察到的差异具有统计学意义(p<0.001)且大于临床相关性MID(>5.75)。
讨论
我们的数据表明,渗漏发生率与报告的QoL之间存在明确的关系;在最近十次底盘更换中经历四次或更多次渗漏至底盘问题的受试者具有显著更低的总QoL。先前有报告称,渗漏具有心理和生理的双重影响(Nafees等人8记录了心理影响,其中,作者制定了一种用于测量渗漏对心理、社交以及应对和控制等领域的影响的量表),但是未充分了解人们的经历及其影响。
本研究旨在通过临床和用户输入确定渗漏的定义。进而使用此信息来开发和确认一种新的测量工具,用于理解渗漏对英国、美国、法国和丹麦使用造口装置的人群的影响。参与者从一组用户中招募,其中包括目前使用康乐保产品的人群,该活动由康乐保组织。六位临床医生和41名用户参加了概念启发访谈。使用此访谈的定性结果起草项目。组织一组临床专家来开发和确认项目(n=6)。当造口排出物流到底盘区域外并流到参与者衣服上时,渗漏的影响变得明显更为重大8。我们的数据表明,即使排出物停留在底盘区域内,由于用户对自己的造口装置失去了信心,这似乎也会对QoL产生影响。
不清楚渗漏事件的高报告率是否受到了用户缺乏依从性或者缺乏关于如何避免渗漏的知识的影响。但是,如果这些数据确实反映出用户在管理自己的造口装置方面存在困难,则可以通过向用户提供有关良好造口护理实践的建议来防止不良QoL。缺乏舒适度和信心也可能受到了渗漏产生的生理影响的影响。由于造口排出物包含消化酶9–11,排泄物可能导致ICD,这是最常见的PSC类型5,12。因此,渗漏和PSC似乎影响了对造口装置的信心和造口装置的舒适度领域,进而给总QoL带来了负面影响。在本研究中,要求用户回想在最近6个月期间出现的所有皮肤问题,以确保记录了所有不时需要努力克服皮肤问题的用户,而且本研究仅测量一个时间点的QoL。因此,由于本研究在横断面数据收集方面的局限性,无法表明PCS和QoL之间的因果关系。但是,在先前的一项前瞻性研究中,在遭受PSC的患者中也观察到了较低的QoL6。
结论
数据证明,渗漏对造口患者的生理和心理具有显著影响。因此,预防渗漏事件有可能改善QoL(包括舒适度和信心领域),以及减少PSC。此外,由于几乎所有受访者均对渗漏表示担忧,并且渗漏影响了人们对造口装置的信心,这些结果表明,需要能通过减少对于渗漏的担忧增强信心的解决方案。
伦理
本调查作为一项市场研究来执行并获得了内部审查委员会的批准。
致谢
我们感谢高级生物统计师Helle Doré Hansen以及证据和教育主管Anni Rønfeldt Thomsen的协助。
利益冲突
所有作者皆为康乐保集团的雇员。
资助
本文章完全由康乐保集团资助。
Author(s)
Chris Juul Hedegaard
PhD, MSc, BSc
Evidence Manager, Coloplast A/S, Humlebaek, Denmark
Teresa Adeltoft Ajslev
Senior Scientific Manager, Coloplast A/S, Humlebaek, Denmark
Rikke Zeeberg
MSc
Senior Insights Manager, Coloplast A/S, Humlebaek, Denmark
Anne Steen Hansen*
RN, ET, BSc, PMI
Lead Medical Specialist, Coloplast A/S, Humlebaek, Denmark
Email dkasn@coloplast.com
* Corresponding author
References
- Porrett T, Nováková S, Schmitz K, Klimekova E, Aaes H. Leakage and ostomy appliances: results from a large-scale, open-label study in clinical practice. Gastrointest Nurs 2014;9(Sup2):19–23.
- Claessens I, Probert R, Tielemans C, Steen A, Nilsson C, Andersen BD, et al. The Ostomy Life Study: the everyday challenges faced by people living with a stoma in a snapshot. Gastrointest Nurs 2015;13(5):18–25.
- Nybaek H, Jemec GBE. Skin problems in stoma patients. J Eur Acad Dermatology Venereol 2010;24(3):249–57.
- White P, Evans M. Clinical governance for ostomates at risk of peristomal skin complications. Br J Nurs 2019;28(16):S24–32.
- Voegeli D, Karlsmark T, Eddes EH, Hansen HD, Zeeberg R, Håkan-Bloch J, et al. Factors influencing the incidence of peristomal skin complications: evidence from a multinational survey on living with a stoma. Gastrointest Nurs 2020 May 1;18(Sup4):S31–8.
- Erwin-Toth P, Thompson SJ, Davis JS. Factors impacting the quality of life of people with an ostomy in North America: results from the dialogue study. J Wound, Ostomy Cont Nurs 2012;39(4):417–22.
- Nafees B, Rasmussen M, Loyd A. The Ostomy-Q: development and psychometric validation of an instrument to evaluate outcomes associated with ostomy appliances. Ostomy Wound Manag 2017;63(1):12–22.
- Nafees B, Størling ZM, Hindsberger C, Lloyd A. The ostomy leak impact tool: development and validation of a new patient-reported tool to measure the burden of leakage in ostomy device users. Health Qual Life Outcomes 2018 Dec 14;16(1):231.
- Bohe M, Borgström A, Genell S, Ohlsson K. Determination of immunoreactive trypsin, pancreatic elastase and chymotrypsin in extracts of human feces and ileostomy drainage. Digestion 1983;27(1):8–15.
- Bohe M, Borgström A, Genell S, Ohlsson K. Metabolism of131I-labelled human pancreatic cationic trypsin after intraduodenal administration. Digestion 1986;34(2):127–35.
- Andersen PH, Bucher AP, Saeed I, Lee PC, Davis JA, Maibach HI. Faecal enzymes: in vivo human skin irritation. Contact Dermatitis 1994;30:152–158.
- Martins L, Samai O, Fernández A, Urquhart M, Hansen AS. Maintaining healthy skin around an ostomy: peristomal skin disorders and self-assessment. Gastrointest Nurs 2011;9(Sup2):9–13.


