Volume 41 Number 3
WHAM evidence summary: effectiveness of tea tree oil in managing chronic wounds
Emily Haesler and Keryln Carville
Keywords chronic wound, wound infection, tea tree oil, melaleuca, essential oil
For referencing Haesler E and Carville K. WHAM evidence summary: effectiveness of tea tree oil in managing chronic wounds . WCET® Journal 2021;41(3):44-47
DOI https://doi.org/10.33235/wcet.41.3.44-47
Clinical question
What is the best available evidence on the use of tea tree oil preparations in managing chronic wounds?
Summary
Tea tree oil is an essential oil traditionally used for its antibacterial and anti-inflammatory properties. Level 5 evidence from bench research1-7 has demonstrated that tea tree oil has activity against bacteria, fungi and viruses. There is minimal evidence exploring the clinical use of tea tree oil in reducing promoting healing in chronic wounds. Level 1 evidence8 demonstrated reduction of MRSA colonisation and improvement in wound assessment scores. Level 3 evidence9 reported reduction in wound size; however, MRSA colonisation did not decrease and most participants required commencement of antibiotic therapy. Level 4 evidence10, 11 reported successful wound bed granulation10 and complete healing10, 11. This limited evidence was insufficient to make a graded recommendation on the use of tea tree oil to promote healing in chronic wounds. However, the studies reported that no adverse events occurred. Tea tree oil products might be used to treat chronic wounds in clinical contexts in which there is no access to contemporary antimicrobial agents.
Clinical practice recommendations
All recommendations should be applied with consideration to the wound, the person, the health professional and the clinical context.
There is insufficient evidence on the effectiveness of topical tea tree oil products to make a graded recommendation on their use in promoting healing in chronic wounds.
Sources of evidence
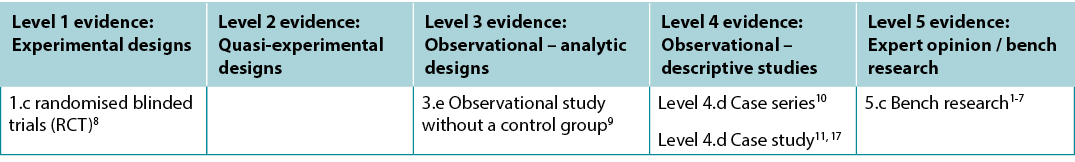
This summary was conducted using methods published by the Joanna Briggs Institute (JBI)12-16. The summary is based on a systematic literature search combining search terms related to chronic wounds with terms related to tea tree oil. Searches were conducted in Embase, Medline, Global Health, and Allied and Complementary Medicine databases, and in the Hinari database for low- and middle-income countries. Evidence published up to July 2021 in English was eligible. Studies were assigned a level of evidence (see Table one) based on JBI’s hierarchy12-16. Recommendations are made based on the body of evidence and are graded according to the system reported by JBI12-16.
Table 1. Levels of evidence
Background
Tea tree oil is an essential oil derived from an Australian native plant, Melaleuca alternifolia1, 4, 18. Essential oils are plant-based oils that contain high concentrations of plant extracts. Crushed tea tree leaves were used as a traditional remedy by Aboriginal people, prepared as a poultice for treating skin lesions4, 19. The formulation of contemporary tea tree oil, made by steam distillation of the leaves19, 20, is regulated by international standards that define its chemical composition with respect to 14 primary components7, 21. Most variations of tea tree oil contain over 100 active components.
Tea tree oil preparations are used to treat superficial skin conditions (e.g., insect bites, head lice and dandruff)4, 21 and has been shown to have some efficacy in eradicating methicillin-resistant Staphylococcus aureus (MRSA) in nasal infections22 and topical skin infections23. Topical tea tree oil preparations are also used in wound management, to achieve a range of outcomes including reduction in inflammation, control of local wound infection and to facilitate wound debridement17.
Evidence
Findings from bench research on tea tree oil
A review reported on 17 in vitro studies that demonstrated susceptibility of a wide range of bacteria, including E. coli, K. pneumoniae, S. epidermidis, S. pyogenes and MRSA to tea tree oil at 1 to 2% concentration. In vitro studies reported in the review also demonstrated that tea tree oil has anti-fungal and anti-viral activity7 (Level 5).
Additional bench research adds to this evidence base, reporting tea tree oil’s efficacy in eradication S. aureus1, 3, 6 and MRSA2, including in samples taken from lower limb wounds6. Minimum inhibitory concentration, which is the lowest concentration of an antimicrobial that will inhibit the growth of microorganisms, is reported as between 0.2%6 and 0.5%2. One in vitro study demonstrated that tea tree oil formulations maintained adequate antimicrobial activity when combined with alcohol and surfactants3 (Level 5).
An animal study also provided evidence that application of tea tree oil to an acute wound could improve stages of wound healing4 (Level 5).
Effectiveness in promoting chronic wound healing
The evidence on tea tree oil for promoting chronic wound healing comes from small trials that primarily used low level research designs and were at a moderate-to-high risk of bias. A summary of the studies is presented in Table two.
Table 2. Summary of clinical evidence for topical tea tree oil products
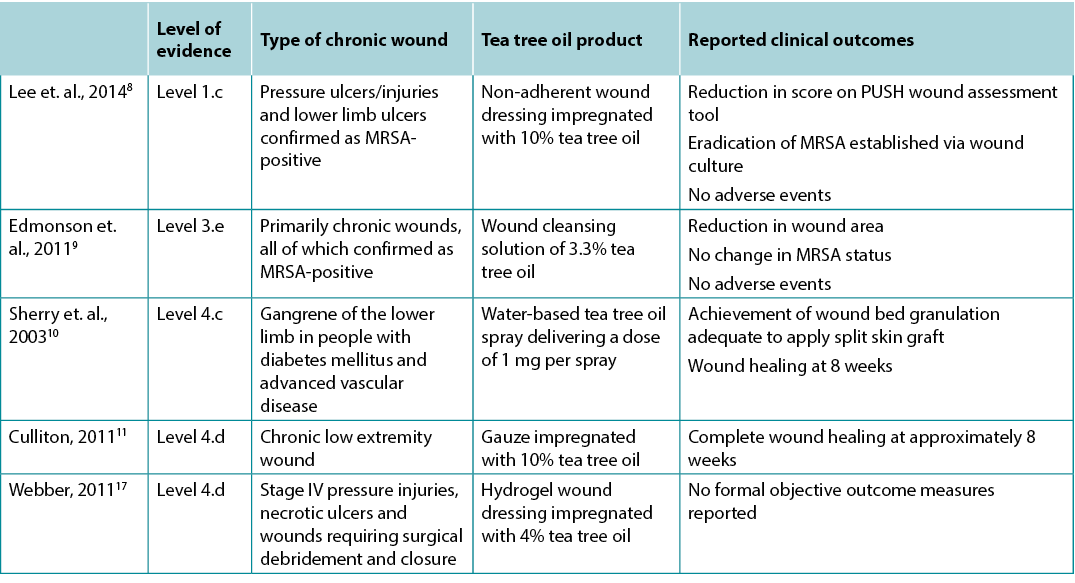
In an RCT (n = 32)8, people with chronic wounds confirmed via wound culture to be MRSA positive8 received either a wound dressing impregnated with 10% tea tree oil or a control non-adherent wound dressing. Analysis of weekly wound cultures showed statistically significantly (p < 0.01) lower viable counts of MRSA associated with tea tree oil treatment from week one to final analysis four weeks after commencing treatment. Complete eradication of MRSA was achieved by week four of treatment for 87.5% of wounds. There was also a statistically significant difference (p < 0.001) in weekly scores on the PUSH wound assessment tool, favouring the tea tree oil group8 (Level 1).
In an uncontrolled pilot trial (n = 12)9, people with wounds confirmed as being MRSA-colonised but not showing clinical signs and symptoms of local wound infection were selected for treatment with a tea tree oil wound cleansing solution. Participants were withdrawn from the study if they subsequently required antibiotic therapy. All the wounds in the study remained MRSA-colonised at the time of trial completion (n = 2) or withdrawal (n = 10). However, 66.7% of wounds had a reduction in wound area at the time of withdrawal from the study compared to baseline9 (Level 3).
In a case series analysis (n = 10)10, gangrenous lower limb wounds were treated with tea tree oil applied as a spray three times daily. Treatment was initially administered until the wound bed was granulating and appropriate for application of a split skin graft. In 100% of wounds, granulation occurred within 2 to 3 weeks, achieving a clinical condition appropriate for grafting. Tea tree oil treatment continued for 1 to 2 weeks following grafting. Complete wound healing was achieved within eight weeks for 100% of wounds10 (Level 4).
In a report of three case studies17, a hydrogel dressing impregnated with 4% tea tree oil was used to treat chronic wounds. Wound dressings were changed every 1—5 days based on wound depth. All wounds were described as healing well when the patient was discharged. The lack of formal outcome measure reporting and the use of a range of concurrent wound treatments prevented conclusions being made about the efficacy of tea tree oil in this report17 (Level 4). Another report on a single case study11 described progression to complete wound healing over a period of approximately eight weeks for a lower limb wound that had been assessed as requiring amputation. Tea tree oil-soaked gauze dressings were applied daily until complete epithelialisation was achieved11 (Level 4).
Considerations for use
- Use tea tree oil with composition that meets the relevant international standard (ISO4730)20 that dictates the composition of the product. Tea tree oil can be prepared for use in a variety of different formulations. The product reported in the Level 1 study8 above was prepared in the laboratory by diluting 100% tea tree oil to a concentration of 10% tea tree oil and 90% paraffin oil. In other studies, tea tree oil was been impregnated in a wound dressing8, 17, applied as a spray10, and used as a cleansing agent9.
- In clinical studies in which tea tree oil was applied directly to chronic wounds, adverse events were not observed8, 10, 11, 17. However, in other contexts mild adverse effects have been associated with topical application of tea tree oil. From ten clinical studies in which a tea tree oil product was applied to broken skin (e.g., dermatitis, acne and tinea), five reported mild irritation as an adverse effect7. In studies reporting application of tea tree oil to intact skin, mild sensitivity reactions were reported in a small proportion of people,7, 21 with sensitivity rates higher for products with higher tea tree oil concentrations21.
- Tea tree oil is reported to have a pleasant odour when used in wound products17 and a laboratory study demonstrated the oil is effective in reducing general malodour5.
- Clinical studies conducted in Australian tertiary hospitals reported that tea tree oil products were a cost effective treatment option for chronic wound management10, 17.
Conflicts of interest
The author declares no conflicts of interest in accordance with International Committee of Medical Journal Editors (ICMJE) standards.
About WHAM evidence summaries
WHAM evidence summaries are consistent with methodology published in:
Munn Z, Lockwood C, Moola S. The development and use of evidence summaries for point of care information systems: A streamlined rapid review approach, Worldviews Evid Based Nurs. 2015;12(3):131-8.
Methods are outlined in detail in resources published by the Joanna Briggs Institute as cited in this evidence summary. WHAM evidence summaries undergo peer-review by an international multidisciplinary Expert Reference Group. More information: https://healthsciences.curtin.edu.au/health-sciences-research/research-institutes-centres/wceihp/ .
WHAM evidence summaries provide a summary of the best available evidence on specific topics and make suggestions that can be used to inform clinical practice. Evidence contained within this summary should be evaluated by appropriately trained professionals with expertise in wound prevention and management, and the evidence should be considered in the context of the individual, the professional, the clinical setting and other relevant clinical information.
Copyright © 2021 Wound Healing and Management Unit, Curtin University.
![]()
WHAM证据总结:茶树油治疗慢性伤口的有效性
Emily Haesler and Keryln Carville
DOI: https://doi.org/10.33235/wcet.41.3.44-47
临床问题
使用茶树油制剂治疗慢性伤口的最佳证据是什么?
总结
茶树油是一种传统上用于抗菌和抗炎的精油。来自实验室研究1-7的5级证据表明,茶树油具有抗细菌、真菌和病毒的活性。探索茶树油在促进慢性伤口愈合方面的临床用途证据很少。1级证据8证明MRSA定植减少,伤口评估评分提高。3级证据9报告伤口尺寸变小;然而,MRSA定植并没有减少,大多数受试者需要开始抗生素治疗。4级证据10,11报告了成功的伤口床肉芽形成10和完全愈合10,11。证据有限,无法就茶树油在促进慢性伤口愈合方面的作用明确推荐等级。不过,研究均报告无不良事件发生。茶树油产品可用于治疗临床环境中无法获得现代抗菌剂的慢性伤口。
临床实践建议
采用所有建议时,应考虑伤口、患者、专业医护人员和临床环境。
外用茶树油产品的有效性证据不足,无法就茶树油在促进慢性伤口愈合方面的作用明确推荐等级。
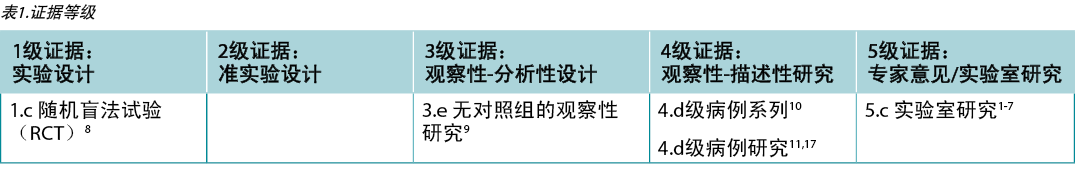
证据来源
本总结是采用乔安娜·布里格斯研究所(JBI)公布的方法进行的12-16。本总结以系统性的文献检索为基础,将与慢性伤口相关的检索术语与与茶树油相关的术语相结合。在Embase、Medline、Global Health、补充医学文献数据库(Allied and Complementary Medicine)以及Hinari数据库等数据库中对中低收入国家进行了检索。截至2021年7月以英文发表的证据符合条件。根据JBI的等级划分,对研究进行了证据水平(表1)的划分12-16。根据大量证据提出建议,并根据JBI报告的系统进行评分12-16。
背景
茶树油是一种源自澳大利亚本土植物互叶白千层1,4,18的精油。精油是植物油,含有高浓度的植物提取物。原住民使用压碎的茶树叶作为传统药物,制成膏药来治疗皮肤损伤4, 19。现代茶树油的配方是通过叶子的蒸汽蒸馏制成的19,20,受国际标准监管,该标准定义了其化学成分的14种主要成分7,21。大多数茶树油都含有超过100种活性成分。
茶树油制剂用于治疗浅表皮肤病(例如,昆虫叮咬、头虱和头皮屑)4, 21,并且已被证明在根除鼻部感染22和局部皮肤感染中的耐甲氧西林金黄色葡萄球菌(MRSA)方面具有一定功效23。外用茶树油制剂也用于伤口管理,以减少炎症、控制局部伤口感染和促进伤口清创等17。
证据
茶树油的实验室研究结果
一项评价报告了17项体外研究,这些研究证明了多种细菌(包括大肠杆菌、肺炎克雷伯菌、表皮葡萄球菌、化脓性链球菌和MRSA)对浓度为1%至2%的茶树油的敏感性。评价中报告的体外研究还表明,茶树油具有抗真菌和抗病毒活性作用7(5级)。
另有长期实验室研究丰富了这一证据,报告了茶树油在根除金黄色葡萄球菌1,3,6和MRSA2方面的功效,包括从下肢伤口采集的样本6。最小抑制浓度,即抑制微生物生长的抗微生物剂的最低浓度,据报告介于 0.2%6和0.5%2之间。一项体外研究表明,茶树油配方与酒精和表面活性剂结合使用时,仍能保持足够的抗菌活性3(5级)。
一项动物研究还提供证据表明,将茶树油涂抹于急性伤口可以改善伤口愈合阶段4(5级)。
促进慢性伤口愈合的有效性
茶树油促进慢性伤口愈合的证据来自小型试验,这些试验主要使用低水平的研究设计,并且存在中到高的偏倚风险。研究总结见表2。
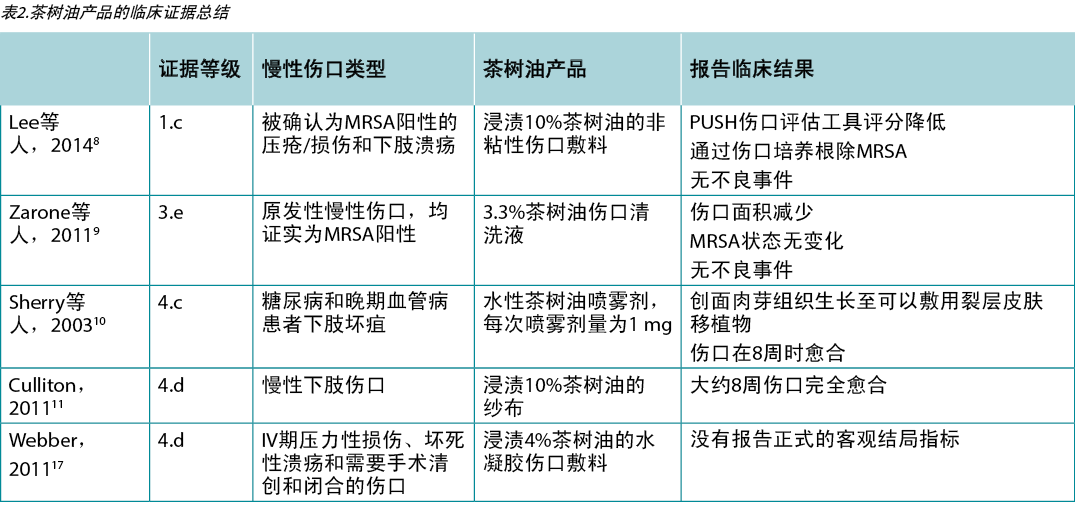
在一项RCT(n=32)8中,通过伤口培养确认为MRSA阳性8的一些慢性伤口患者接受了浸渍10%茶树油的伤口敷料,另一些则接受了作为对照的非粘附性伤口敷料。每周伤口培养的分析显示,从第一周到开始治疗后4周的最终分析,与茶树油治疗相关的MRSA存活数量在统计学上显著降低(p<0.01)。87.5%的伤口在治疗第4周时MRSA被完全根除。PUSH伤口评估工具的每周评分也存在统计学显著差异(p<0.001),茶树油组评分更高8(1级)。
在一项无对照的先导试验(n=12)9中,选择了伤口确认为MRSA定植,但未显示局部伤口感染的临床体征和症状的患者使用茶树油伤口清洁液进行治疗。如果受试者随后需要抗生素治疗,将退出研究。研究中的所有伤口在试验完成(n=2)或患者退出(n=10)时均有MRSA定植。然而,与基线9相比,66.7%的伤口在退出研究时面积减少(3级)。
在一个病例系列分析(n=10)10中,使用茶树油每天喷洒3次来治疗坏疽下肢伤口。初期使用茶树油进行治疗,直到伤口床形成肉芽并适合进行裂层皮肤移植。在100%的伤口中,肉芽在2至3周内出现,达到适合移植的临床条件。茶树油处理在移植后持续使用1至2周。8周内100%的伤口完全愈合10(4级)。
在一份包含三个病例研究的报告17中,用浸渍了4%茶树油的水凝胶敷料治疗慢性伤口。根据伤口深度,每1-5天更换一次伤口敷料。患者出院时,所有伤口都被描述为愈合良好。由于缺乏正式的结果测量报告,且同时进行了一系列的伤口治疗,无法在本报告中得出关于茶树油功效的结论17(4级)。另一项关于单个病例研究的报告11描述了下肢伤口在大约八周的时间内完成愈合的进程,该伤口已评估为需要截肢。每天使用茶树油浸纱布敷料,直至达到完全上皮形成11(4级)。
使用注意事项
· 使用成分符合规定产品成分的相关国际标准(ISO4730)20的茶树油。茶树油可以制备用于各种不同的配方。上述1级研究8中报告的产品是在实验室中通过将100%茶树油稀释至10%茶树油和90%石蜡油的浓度而制备。在其他研究中,茶树油浸渍在伤口敷料中8,17,以喷雾形式10,用作清洁剂9。
· 在将茶树油直接涂抹于慢性伤口的临床研究中,未观察到不良事件8,10,11,17。不过,在其他条件下,出现了与茶树油局部应用有关的轻微副作用。在十项将茶树油产品应用于破损皮肤(例如皮炎、痤疮和癣)的临床研究中,五项报告称其副作用为轻度刺激7。在报告将茶树油应用于完整皮肤的研究中,一小部分人报告了轻微的敏感反应,7,21 茶树油浓度较高的产品的敏感率更高21。
· 据报告,茶树油在用于伤口产品时具有令人愉悦的气味17,实验室研究表明该油可有效减轻普通恶臭5。
· 在澳大利亚三级医院进行的临床研究表明,茶树油产品是慢性伤口管理的一种具有成本效益的治疗选择10,17。
利益冲突
根据国际医学期刊编辑委员会(ICMJE)的标准,作者声明没有利益冲突。
WHAM证据总结
WHAM证据总结的方法与Munn Z, Lockwood C, Moola S发表的现场医护信息系统(一种简化的快速审查方法)证据总结的开发和使用,Worldviews Evid Based Nurs 2015; 12 (3):131-8的方法一致。
方法在本证据总结中引用的Joanna Briggs研究所出版的资源中有详细概述。WHAM证据总结经过国际多学科专家参考小组的同行评审。更多信息:https://healthsciences.curtin.edu.au/health-sciences-research/research-institutes-centres/wceihp/
WHAM证据总结提供了关于特定主题的最佳可用证据的总结,并提出了可用于指导临床实践的建议。本总结中包含的证据应由经过适当培训的具有伤口预防和管理专业知识的专业人士员进行评价,并应根据个人、专业人士、临床环境以及其他相关临床信息考虑证据。
版权所有© 2021 科廷大学伤口愈合和管理课程。
![]()
Author(s)
Emily Haesler* PhD, P Grad Dip Adv Nurs (Gerontics), BN
Fellow Wounds Australia
Adjunct Professor, Curtin University, Wound Healing and Management (WHAM) Unit.
Email Emily.haesler@curtin.edu.au
Keryln Carville PhD, RN, Fellow Wounds Australia
Professor, Silver Chain Group and Curtin University.
* Corresponding author
References
- Bearden DT, Allen GP, Christensen JM. Comparative in vitro activities of topical wound care products against community-associated methicillin-resistant Staphylococcus aureus. J Antimicrob Chemother, 2008;62(4):769-72.
- Kwieciński J, Eick S, Wójcik K. Effects of tea tree (Melaleuca alternifolia) oil on Staphylococcus aureus in biofilms and stationary growth phase. Int J Antimicrob Agents, 2009;33(4):343-7.
- Thomsen PS, Jensen TM, Hammer KA, Carson CF, Mølgaard P, Riley TV. Survey of the antimicrobial activity of commercially available Australian tea tree (Melaleuca alternifolia) essential oil products in vitro. J Altern Complement Med, 2011;17(9):835-41.
- Labib RM, Ayoub IM, Michel HE, Mehanny M, Kamil V, Hany M, Magdy M, Moataz A, Maged B, Mohamed A. Appraisal on the wound healing potential of Melaleuca alternifolia and Rosmarinus officinalis L. essential oil-loaded chitosan topical preparations. PloS one, 2019;14(9):e0219561-e.
- Lee G, Anand SC, Rajendran S. Are biopolymers potential deodourising agents in wound management? J Wound Care, 2009;18(7):290, 2-5.
- Falci SP, Teixeira MA, Chagas PF, Martinez BB, Loyola AB, Ferreira LM, Veiga DF. Antimicrobial activity of Melaleuca sp. oil against clinical isolates of antibiotics resistant Staphylococcus aureus. Acta Cir Bras, 2015;30(7):491-6.
- Carson C, Hammer K, Riley T. Melaleuca alternifolia (tea tree) oil: a review of antimicrobial and other medicinal properties Clin Microbiol Rev, 2006;19(1):50-62.
- Lee RLP, Leung PHM, Wong TKS. A randomized controlled trial of topical tea tree preparation for MRSA colonized wounds. Int J Nurs Sci, 2014;1(1):7-14.
- Edmondson M, Newall N, Carville K, Smith J, Riley TV, Carson CF. Uncontrolled, open-label, pilot study of tea tree (Melaleuca alternifolia) oil solution in the decolonisation of methicillin-resistant Staphylococcus aureus positive wounds and its influence on wound healing. Int Wound J, 2011;8(4):375-84.
- Sherry E, Sivananthan S, Warnke PH, Eslick GD. Topical phytochemicals used to salvage the gangrenous lower limbs of type 1 diabetic patients. Diabetes Res Clin Pract, 2003;62(1):65-6.
- Culliton P. Chronic Wound Treatment With Topical Tea Tree Oil. Altern Ther Health Med, 2011;17(2):46-7.
- Munn Z, Lockwood C, S. M. The development and use of evidence summaries for point of care information systems: A streamlined rapid review approach. Worldviews Evid Based Nurs, 2015;12(3):131-8.
- Aromataris E, Munn Z, editors. (2021). JBI Manual for Evidence Synthesis. https://synthesismanual.jbi.global: Joanna Briggs Institute.
- Joanna Briggs Institute. (2013). Levels of Evidence and Grades of Recommendation Working Party. New JBI Grades of Recommendation. Joanna Briggs Institute: https://jbi.global/sites/default/files/2019-05/JBI-grades-of-recommendation_2014.pdf.
- Joanna Briggs Institute. (2014). Levels of Evidence and Grades of Recommendation Working Party. Supporting Document for the Joanna Briggs Institute Levels of Evidence and Grades of Recommendation. Joanna Briggs Institute: https://jbi.global/sites/default/files/2019-05/JBI%20Levels%20of%20Evidence%20Supporting%20Documents-v2.pdf.
- Joanna Briggs Institute. (2013). Levels of Evidence and Grades of Recommendation Working Party. JBI Levels of Evidence. Joanna Briggs Institute: https://jbi.global/sites/default/files/2019-05/JBI-Levels-of-evidence_2014_0.pdf:
- Webber L. Managing bio-burden and devitalised tissue: an early intervention using Woundaid® Wound Practice and Research, 2011;19(3):174-279.
- Baars EW, Zoen EBV, Breitkreuz T, Martin D, Matthes H, Schoen-Angerer TV, Soldner G, Vagedes J, Wietmarschen HV, Patijn O, Willcox M, Flotow PV, Teut M, Ammon KV, Thangavelu M, Wolf U, Hummelsberger J, Nicolai T, Hartemann P, Szoke H, McIntyre M, Werf ETVD, Huber R. The contribution of complementary and alternative medicine to reduce antibiotic use: A narrative review of health concepts, prevention, and treatment strategies. Evid Based Complement Alternat Med, 2019; (no pagination).
- Low WL, Kenward K, Britland ST, Amin MC, Martin C. Essential oils and metal ions as alternative antimicrobial agents: a focus on tea tree oil and silver. Int Wound J, 2017;14(2):369-84.
- International Standards Organisation. (2017). ISO 4730:2017 Essential oil of Melaleuca, terpinen-4-ol type (Tea Tree oil). International Standards Organisation:https://www.iso.org/standard/69082.html.
- Halcón L, Milkus K. Staphylococcus aureus and wounds: a review of tea tree oil as a promising antimicrobial. Am J Infect Control, 2004;32(7):402-8.
- Caelli M, Porteous J, Carson CF, Heller R, Riley TV. Tea tree oil as an alternative topical decolonization agent for methicillin-resistant Staphylococcus aureus. J Hosp Infect, 2000;46(3):236-7.
- Dryden MS, Dailly S, Crouch M. A randomized, controlled trial of tea tree topical preparations versus a standard topical regimen for the clearance of MRSA colonization. J Hosp Infect, 2004;56(4):283-6.


