Volume 42 Number 2
Editorial
Iben Plate
For referencing Plate I. Editorial. WCET® Journal Supplement 2022;42(1)Sup:s3-4
DOI https://doi.org/10.33235/wcet.42.1.sup.s3-4
The presence and persistence of stoma-related complications following ostomy surgery constitute a major burden for individuals living with an ostomy, a burden comprising physical as well as mental components. The physical component includes leakage of stomal effluent and peristomal skin complications, which may range from mild peristomal dermatitis to full thickness painful skin ulcerations1,2. Additionally, the profound bodily changes following surgery, along with the risk and worry of leakage and complications, may lead to psychosocial problems, including depression, anxiety, low self-esteem and social withdrawal3. These may adversely affect the individual’s adaptation to the stoma and quality of life. Therefore, critical components of ostomy care comprise prevention and management of leakage and skin complications, while helping patients adjust to their changed body and re-engage with their social environment (Figure 1). An insight into these issues is provided in two articles included in the following pages of this WCET supplement.
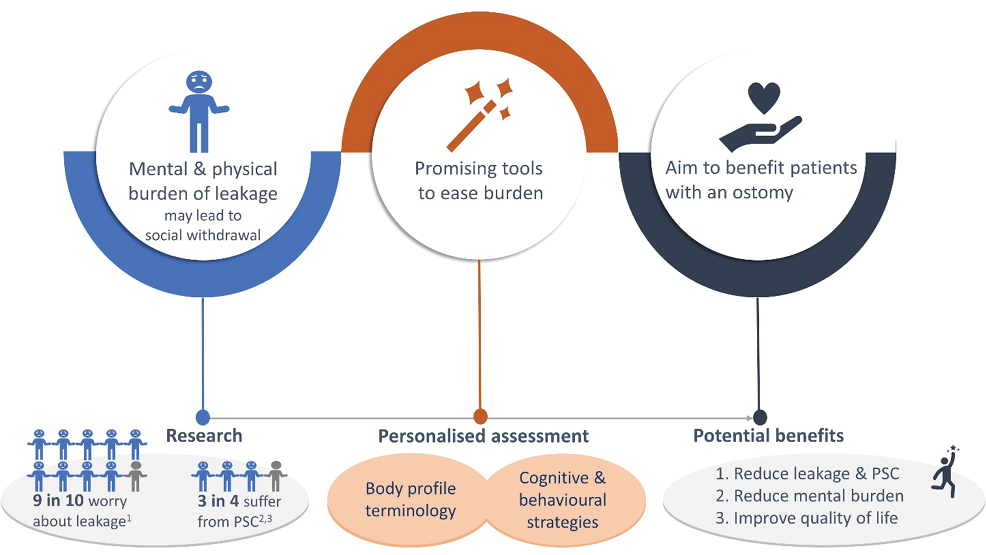
Figure 1. An overview of the problem of peristomal leakage and skin complications faced by individuals living with an ostomy, and approaches to help mitigate these problems
PSC = peristomal skin complication
1. Claessens I, Probert R, Tielemans C, et al. The Ostomy Life Study: the everyday challenges faced by people living with a stoma in a snapshot. Gastrointest Nurs 2015;13(5):18–25.
2. Salvadalena G, Colwell JC, Skountrianos G, et al. Lessons learned about peristomal skin complications: secondary analysis of the ADVOCATE trial. J Wound Ostomy Continence Nurs 2020;47(4):357–63.
3. Herlufsen P, Olsen AG, Carlsen B, et al. Study of peristomal skin disorders in patients with permanent stomas. Br J Nurs 2006;15(16):854–62.
In the first article, author Janice Colwell argues that one of the most important contributions ostomy care specialists can make to their patients is to help them find the best pouching system in terms of the right size of the skin barrier opening and the best shape (flat or convex) of the skin barrier. While the size of the barrier opening depends on the size of the stoma, the shape of the barrier should be based on a thorough assessment of the patient’s peristomal body profile, the stoma, and the output volume and consistency. The author recommends using a convex solution, particularly if the peristomal area is soft, if there are skin creases/folds, or if the stoma lumen is at or below the skin level4. The importance of reassessing patients on an ongoing basis is emphasised to ensure continued use of the optimal pouching system.
The second article by Anne Steen Hansen and colleagues further discusses the importance of a good fit of the ostomy product to reduce leakage and skin complications. It alludes to a modified Delphi consensus building process involving over 1200 stoma care nurses from 27 countries; this helped to create practical guidelines on how to accurately assess body and stoma profiles. The process was facilitated by Coloplast. The standardised Body Profile Terminology5,6 was recommended for characterising the peristomal body profile of patients. Further highlighted in the second article are results from a scoping review undertaken by a group of ostomy care nurses and physicians; these results indicate that convexity should be considered at all times after ostomy surgery, including in the immediate postoperative period, to secure pouch seal and prevent leakage4.
Overall, the articles emphasise the importance of tailoring ostomy care to include individual preferences and peristomal body profiles to obtain the optimal ostomy solution to prevent leakage and skin complications. By implementing such individualised approaches, ostomy care professionals can considerably improve the lives of the millions of individuals around the world living with an ostomy.
This supplement has been supported by

June 2022
补充社论
Iben Plate
DOI: https://doi.org/10.33235/wcet.42.1.sup.s3-4
造口术后造口相关并发症的存在和持续存在给造口患者造成了重大负担,包括生理和心理负担。生理负担包括造口流出物渗漏和造口周围皮肤并发症,其范围可能从轻度造口周围皮炎到全层疼痛性皮肤溃疡1,2。此外,术后身体的重大变化以及出现渗漏和并发症的风险和担忧,可能导致社会心理问题,包括抑郁、焦虑、自卑和社交回避3。这些可能会对患者对造口的适应和患者生活质量产生不利影响。因此,造口护理的关键在于预防和管理渗漏和皮肤并发症,同时帮助患者适应身体变化并重新融入社会环境(图1)。本WCET增刊的以下几页中包含了两篇文章,对这些问题进行了深入的分析。
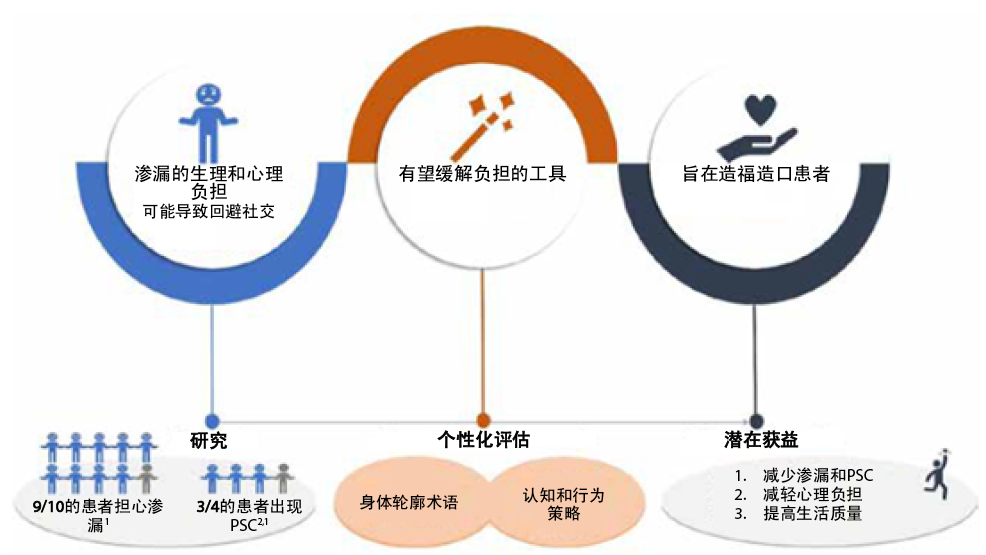
图1.造口患者面临的造口周围渗漏和皮肤并发症问题以及帮助缓解这些问题的方法的概览
PSC=造口周围皮肤并发症1. Claessens I, Probert R, Tielemans C, et al. The Ostomy Life Study: the everyday challenges faced by people living with a stoma in a snapshot. Gastrointest Nurs 2015;13(5):18–25.2. Salvadalena G, Colwell JC, Skountrianos G, et al. Lessons learned about peristomal skin complications: secondary analysis of the ADVOCATE trial. J Wound Ostomy Continence Nurs 2020;47(4):357–63.3. Herlufsen P, Olsen AG, Carlsen B, et al. Study of peristomal skin disorders in patients with permanent stomas. Br J Nurs 2006;15(16):854–62.
在第一篇文章中,作者Janice Colwell认为造口医护人员能够给予患者的最重要帮助之一是帮助他们寻找最佳的造口袋系统,即具有皮肤屏障开口的最佳尺寸和皮肤屏障的最佳形状(平面或凸面)。虽然屏障开口的尺寸取决于造口的尺寸,但屏障的形状应基于对患者造口周围身体轮廓、造口以及输出量和一致性的全面评估。作者建议使用凸面系统,特别是如果造口周围区域较软,存在皮肤皱纹/皱褶,或者造口腔位于或低于皮肤水平4。作者强调了持续重新评估患者的重要性,以确保持续使用最佳的造口袋系统。
Anne Steen Hansen及其同事的第二篇文章进一步讨论了造口产品良好贴合对于减少渗漏和皮肤并发症的重要性。该篇文章略加提及了一个改良后的Delphi共识建立过程,涉及来自27个国家的1200多名造口护理护士;这有助于制定如何准确评估身体和造口轮廓的实用指南。Coloplast促进了这一过程。推荐使用标准化的身体轮廓术语5、6来描述患者的造口周围身体轮廓。第二篇文章进一步强调了一组造口护理护士和医生进行的概况性评价的结果;这些结果表明,造口术后任何时候(包括术后即刻)都应考虑采用凸面系统,以确保造口袋密封并防止渗漏4。
总体而言,两篇文章强调了量身定制造口护理实践的重要性,包括考虑个人偏好和造口周围身体轮廓,以获得最佳的造口解决方案,从而防止渗漏和皮肤并发症。通过实施这种个性化的方法,造口护理专业人员可以显著改善全世界数以百万计的造口患者的生活。

Author(s)
Iben Plate
Director of Evidence & Adoption, Coloplast A/S
References
- Meisner S, Lehur PA, Moran B et al. Peristomal skin complications are common, expensive, and difficult to manage: a population based cost modeling study. PloS One 2012;7(5):e37813.
- Kwiatt M, Kawata M. Avoidance and management of stomal complications. Clin Colon Rectal Surg 2013;26(2):112–21.
- Ayaz-Alkaya S. Overview of psychosocial problems in individuals with stoma: a review of literature. Int Wound J 2019;16(1):243–9.
- Colwell JC, Davis JS, Emodi K, et al. Use of a convex pouching system in the post-operative period – a national consensus. In press. 2022.
- Global Coloplast Ostomy Forum. Ostomy life study review 2016/17. Coloplast A/S;2017:1–23. Available at: https://www.coloplast.com/Documents/Stoma/CP_MM_OstomyLifeStudy_2016.pdf.
- Colwell JC, Bain KA, Hansen AS et al. International consensus results: development of practice guidelines for assessment of peristomal body and stoma profiles, patient engagement, and patient follow-up. J Wound Ostomy Continence Nurs 2019;46(6):497–504.


