Volume 42 Number 2
WHAM evidence summary: Aloe vera for treating burns
Emily Haesler
Keywords burns, acemannan, aloe vera, natural wound healing, traditional wound care
For referencing Haesler E. WHAM evidence summary: Aloe vera for treating burns. WCET® Journal 2022;42(2):36-39
DOI https://doi.org/10.33235/wcet.42.2.36-39
Clinical question
What is the best available evidence for topically applied aloe vera for promoting healing in burns?
Summary
Aloe vera is a succulent plant that has traditionally been used for natural wound healing, including to promote healing of burns.1-3 Because it has a high water content, aloe vera promotes moist wound healing and is described as soothing on application. The research identified in the literature search provided some evidence supporting the efficacy of aloe vera for promoting healing in partial thickness burns.4-13 Level 1 evidence suggested that aloe vera applied topically to partial thickness burns is associated with statistically significantly high rates of healing4-6, 8, 13 that is achieved faster4, 7-9, 12 than with comparator treatments. Level 1 evidence9, 10 also indicated that aloe vera can help relieve the pain of partial thickness wounds. Allergic reactions to the aloe vera products have been reported.6
Clinical practice recommendations
All recommendations should be applied with consideration to the wound, the person, the health professional and the clinical context.
There is some evidence that topically applied aloe vera could be used to improve healing in partial thickness burns, especially when there is limited access to contemporary dressings for moist wound healing (Grade B).
Sources of evidence: search and appraisal
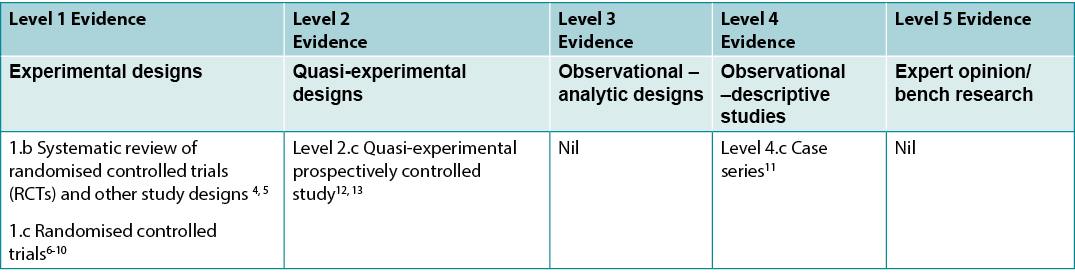
This summary was conducted using methods published by the Joanna Briggs Institute.14-16 The summary is based on a systematic literature search combining search terms related to aloe vera/acemannan and burns. This search was conducted in Medline, EMBASE, the Cochrane Library, AMED and the World Health Organisation’s Afro library, for evidence conducted in humans with burns published up to February 2017 in English. Retrieved studies were appraised for relevance and rigour using Joanna Briggs Institute critical appraisal tools. Levels of evidence for intervention studies are reported in Table 1.
Table 1: Levels of evidence for clinical studies
Background
Aloe vera (Liliaceae family) is a tropical succulent that has been used in Asian and African countries as a traditional medicine for centuries.1-3 The active component of aloe vera is a gel substance that is cultivated from the inside of the leaves. The aloe gel contains vitamins, enzymes, amino acids, sugars, minerals, anthraquinones and polysaccharides (including acemannan).1, 3, 17 It has water content of approximately 99%,1, 18 which contributes to its attributed effect in preventing wound desiccation and its soothing characteristics.19, 20
Bench research suggests that aloe vera stimulates fibroblast proliferation, promotes collagen synthesis and stimulates angiogenesis.17, 20 Aloe vera is also claimed to have antimicrobial qualities,17, 20, 21 and ability to improve microcirculation, which in turn increases wound bed oxygenation.9, 20
Aloe vera gel is produced from the leaves of the aloe vera plant. The outer layer of the washed leaf is peeled and the inner gel is pulverised. In commercial production, this gel is filtered, sterilised and pasteurised, reducing it to a slimy, gel consistency17, 21 When prepared traditionally, aloe vera leaves are washed, the outer leave rind is removed with a sterilised knife, the inner flesh is ground to a pulp with a mill and the gel substance storing it in an air tight container in a dry, cool place.22 This method produces a non-sterile product that is not recommended for use in contemporary wound care due to the risk of infection.
Clinical evidence
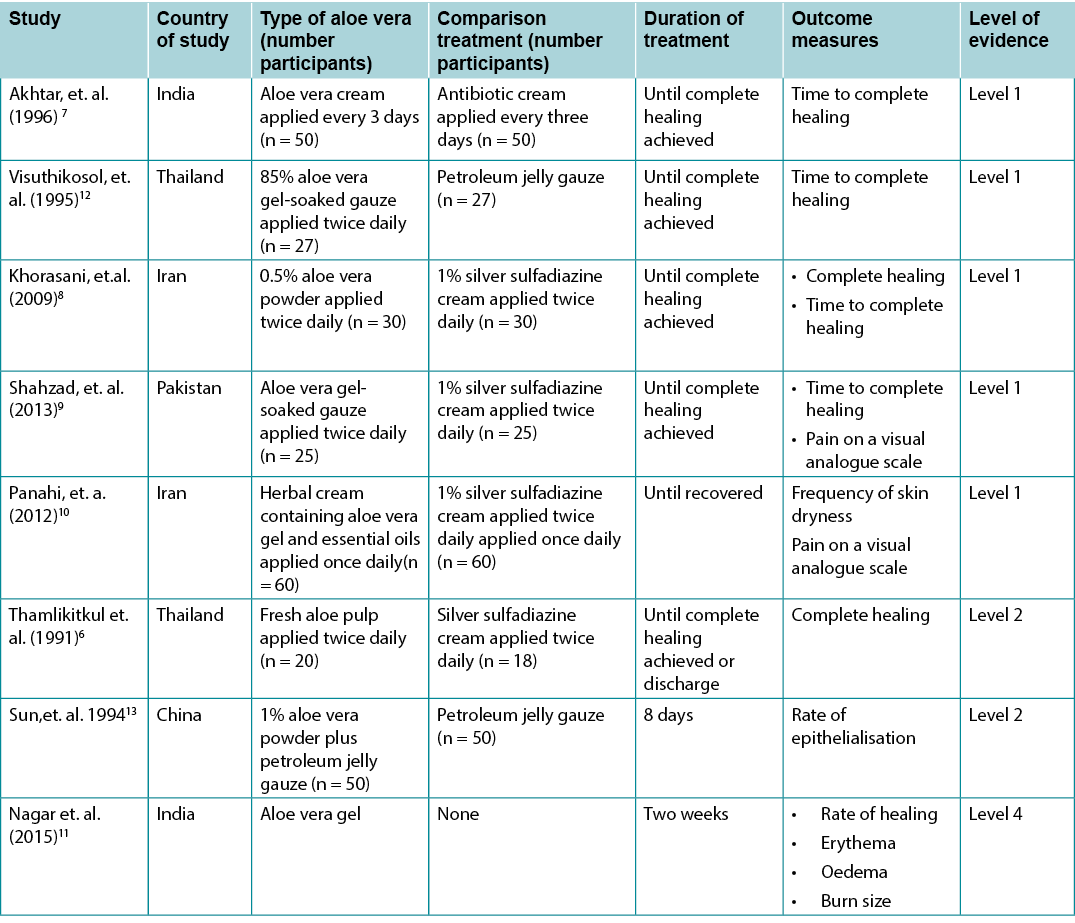
The body of evidence identified in the search included eight studies,6-13 most of which were summarised in two systematic reviews,4, 5 and all of which were at moderate or high risk of bias. All the research was conducted in people with partial thickness (second- or third-degree burns). The evidence identified in this search on aloe vera products applied topically to human burns is summarised in Table 2.
Table 2: Summary of the evidence
A systematic review4 at moderate risk of bias reported four studies,6, 7, 12, 13 all of which were at a high risk of bias and two of which were randomised.6, 7 Participants had deep partial thickness (second- or third-degree) burns to up to 40% of total body surface area.4 The pooled results for two studies7, 12 reporting time to complete healing showed that aloe vera products were associated with superior outcomes compared to control treatments. Time to complete healing was statistically significantly shorter for topical aloe vera compared to the comparator treatments (weighted mean difference [WMD] 8.79 days, 95% confidence interval [CI] 2.51 to 15.07, p = 0.006). The third trial6 in the review4 reported higher rates of complete healing with fresh aloe vera pulp compared to 1% silver sulfadiazine cream (95% versus 83%). The last trial13 reported that an aloe vera powder was associated with an improved rate of epithelisation in burns following skin grafting compared to no aloe vera treatment (5.84±0.27mm versus 3.95±0.33 mm) (Level 1).4
A Cochrane review5 included three studies6-8 reporting aloe vera treatments for people with burns, two of which are reported above.6, 7 In the third study (also at high risk of bias),8 0.5% aloe vera powder was associated with a higher rate of achieving complete healing for partial thickness burns compared to 1% silver sulfadiazine cream (100% versus 80%, risk ratio [RR] 1.41, 95% CI 0.70 to 2.85, p>0.05). In this study 100% of the aloe vera treated burns healed by 15.9 ± 2 days, compared with 18.73 ± 2.65 days for the burns treated with silver sulfadiazine cream5, 8 (Level 1).
Efficacy of aloe vera gel for deep partial thickness burns was demonstrated in an RCT conducted in individuals with second degree burns covering less than 25% total body surface area. Patients were randomised to receive either gauze soaked in aloe vera gel (n = 25) or 1% silver sulfadiazine cream (n = 25). The mean healing time was significantly faster in the aloe vera group (mean 11 ± 4.18 days versus mean 24.24 ± 11.16 days, p<0.00001)9 (Level 1).
One RCT10 (n = 120) that was at high risk of bias reported skin dryness as the main evaluation of aloe vera treatment for second-degree burns. At 14-day follow-up, there was no significant difference in skin dryness between a group treated with an aloe vera herbal cream and a group receiving silver sulfadiazine cream (7.1% versus 10.9%, p>0.05)10 (Level 1).
A case series that was at high risk of bias reported outcomes for people with burns (n = 4) who were treated with aloe vera gel. After two weeks, 50% of the burns were completely healed and the other 50% were evaluated as having achieved 80 to 90% improvement in size, oedema and erythema11 (Level 4).
Considerations for use
- Aloe vera has been associated with allergic responses including uriticaria and contact allergic dermatitis.1, 4 Its application should be avoided in people with an allergy to plants in the Liliaceae family(e.g., onions and garlic). In one trial, approximately 40% of participants reported irritation or itching, but this was not different from individuals treated with a silver sulfadiazine dressing.6 Allergic response may be greater when the aloe gel is harvested from the centre component of the leaf, because the active ingredients are more condensed in this part of the plant.4 Applying the aloe gel to a small area of skin as a test prior to application to a burn is recommended.23
- Aloe vera gel appears to be an effective treatment for reducing pain in people with burns.9, 10 In RCTs, people with second and third degree burns who received aloe vera gel reported statistically significantly lower rating of pain measured on a on visual analogue scale than people who were treated with 1% silver sulfadiazine cream. Aloe vera gel was superior for pain management after seven days of treatment (n=120 people, p = 0.014) and after 14 days of treatment (n = 120 people, p =0.05).10 Aloe vera was also associated with faster achievement of a pain-free status in people with second degree burns (n = 50 people, p = 0.01).9 The soothing characteristics of aloe vera are potentially related to its high water content.1, 18-20
- In countries with limited access to contemporary moist wound dressings, aloe vera presents a cost-effective management option. A cost analysis conducted in India reported that a 5ml aloe vera gel dressing was 2.40 Indian rupee. This was about half the price of using a 2g silver sulfadiazine dressing at the cost of 4.92 Indian rupee.9
Conflicts of interest
The author declares no conflicts of interest in accordance with International Committee of Medical Journal Editors (ICMJE) standards.
About WHAM evidence summaries
WHAM evidence summaries are consistent with methodology published in Munn Z, Lockwood C, Moola S. The development and use of evidence summaries for point of care information systems: A streamlined rapid review approach, Worldviews Evid Based Nurs. 2015;12(3):131-8.
Methods are outlined in resources published by the Joanna Briggs Institute14-16 and on the WHAM Collaborative website: http://WHAMwounds.com. WHAM evidence summaries undergo peer-review by an international, multidisciplinary Expert Reference Group. WHAM evidence summaries provide a summary of the best available evidence on specific topics and make suggestions that can be used to inform clinical practice. Evidence contained within this summary should be evaluated by appropriately trained professionals with expertise in wound prevention and management, and the evidence should be considered in the context of the individual, the professional, the clinical setting and other relevant clinical information.
Copyright © 2021 Wound Healing and Management Collaboration, Curtin Health Innovations Research Institute, Curtin University

WHAM证据总结:芦荟治疗烧伤
Emily Haesler
DOI: https://doi.org/10.33235/wcet.42.2.36-39
临床问题
局部应用芦荟促进烧伤愈合的现有最佳证据是什么?
摘要
芦荟是一种肉质植物,传统上用于自然伤口愈合,包括促进烧伤愈合。1-3芦荟因含水量高,遂能促进湿润的伤口愈合,在使用中被描述为具有舒缓作用。文献检索中发现的研究提供了一些证据,支持芦荟促进部分皮层烧伤愈合的功效。4-131级证据表明,局部应用芦荟治疗部分皮层烧伤与统计学上显著的高治愈率4-6,8,13相关,比对照治疗愈合更快4,7-9,12。1级证据9,10还表明,芦荟有助于缓解部分皮层伤口的疼痛。但有报告称对芦荟产品存在过敏反应。6
临床实践建议
采用所有建议时,应考虑伤口、患者、专业医护人员和临床环境。
有一些证据表明,局部应用芦荟可以改善部分皮层烧伤的愈合,特别是用于湿润伤口愈合(B级)的当代敷料获取途径有限时。
证据来源搜索和评价
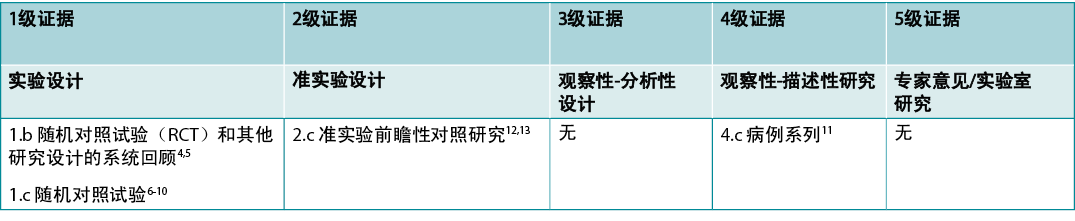
本摘要采用Joanna Briggs Institute公布的方法进行。14-16本摘要基于系统的文献检索,结合了与芦荟/乙酰化甘露聚糖和烧伤相关的检索词。本项检索在Medline、EMBASE、Cochrane图书馆、AMED和世界卫生组织的Afro图书馆进行,检索截至2017年2月以英文发表的针对烧伤患者的证据。使用Joanna Briggs Institute的关键评价工具,评价检索到的研究的相关性和严谨性。干预性研究的证据水平见表1。
表1:临床研究的证据水平
背景
芦荟(百合科)是一种热带肉质植物,数百年来一直在亚洲和非洲国家作为传统药物使用。1-3芦荟的活性成分是一种从叶子内部培养的凝胶物质。芦荟凝胶含有维生素、酶、氨基酸、糖、矿物质、蒽醌和多糖(包括乙酰甘露聚糖)。1,3,17其含水量约为99%,1,18这造就了其防止伤口干燥的功效和舒缓的特性。19,20
实验室研究表明,芦荟能刺激成纤维细胞增殖,促进胶原蛋白合成,并刺激血管生成。17,20芦荟还据称具有抗菌特性17,20,21和改善微循环的能力,从而提高伤口床的氧合。9,20
芦荟凝胶是由芦荟植物的叶子制成的。将清洗过的叶子的外层去皮,捣碎内层凝胶。在商业生产中,这种凝胶经过过滤、消毒和巴氏杀菌,使其成为粘稠的凝胶稠度17,21。传统制备方法是,清洗芦荟叶,用消毒过的刀去除外层叶皮,用研磨机将内层芦荟叶肉研磨成浆,并将凝胶物质储存在密封容器中,放置于干燥阴凉处。22这种方法生产的不是无菌产品,由于有感染的风险,不建议在当代伤口护理中使用。
临床证据
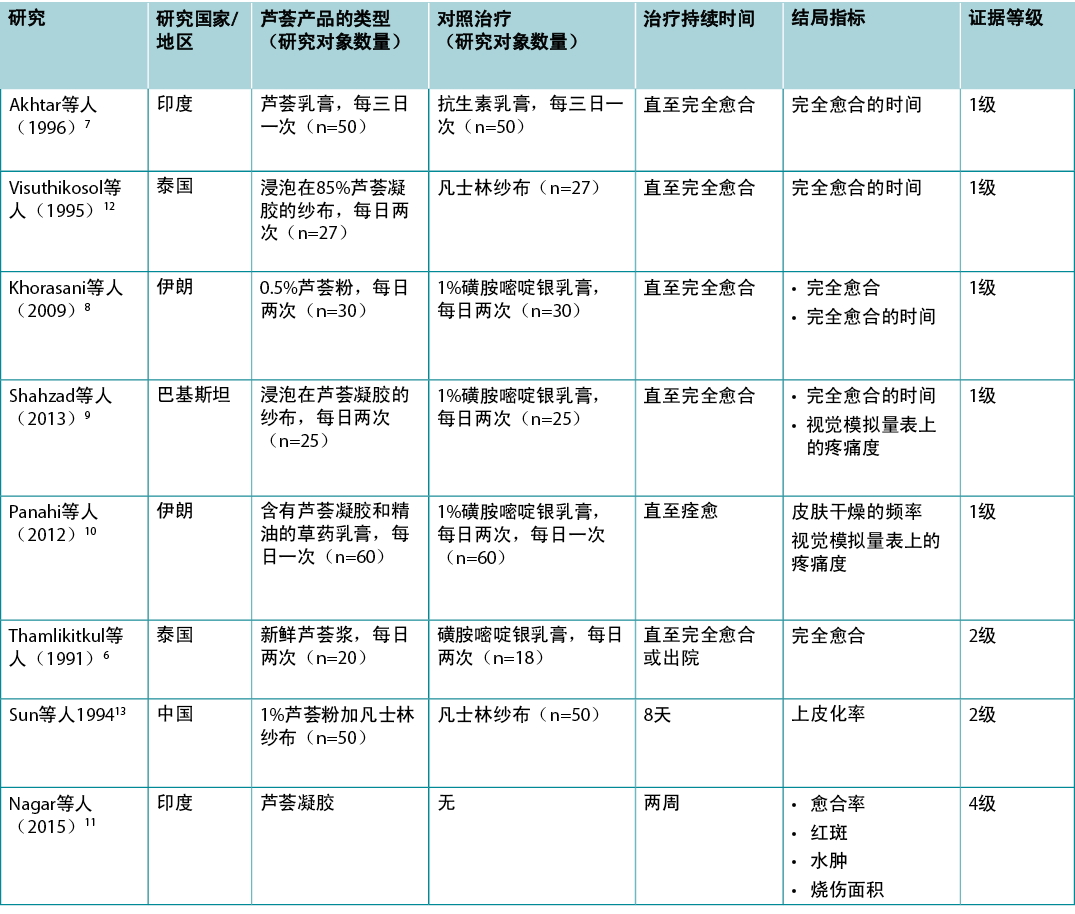
搜索中发现的证据包括8项研究,6-13其中的大部分都总结在两项系统综述中,4,5且所有这些研究都有中度或高度的偏倚风险。所有的研究都是在有部分皮层烧伤(二度或三度烧伤)的人群中进行的。表2总结了此次检索中发现的关于将芦荟产品局部应用于人体烧伤的证据。
表2:证据总结
一项中等偏倚风险的系统综述4报告了四项研究(均为高偏倚风险研究),6,7,12,13其中两项为随机研究。6,7研究对象的深部部分皮层(二度或三度)烧伤高达体表总面积的40%。4两项研究7,12报告完全愈合时间的汇总结果表明,与对照治疗相比,芦荟产品与更好的结局相关。与对照治疗相比,局部使用芦荟的完全愈合时间在统计学上显著缩短(加权平均差[WMD]为8.79天,95%置信区间[CI]为2.51至15.07,p=0.006)。综述4的第三次试验6报告,与1%磺胺嘧啶银乳膏相比,新鲜芦荟浆的完全愈合率更高(95%对83%)。最后一项试验13报告称,使用芦荟粉与未使用芦荟治疗相比,使用芦荟粉与烧伤后皮肤移植的上皮化率的提高相关(5.84±0.27 mm对比3.95±0.33 mm)(1级)。4
Cochrane综述5包括三项研究6-8,报告了芦荟对烧伤患者的治疗,其中两项已在上文中报告。6,7在第三项研究中(也有较高的偏倚风险),80.5%芦荟粉与1%磺胺嘧啶银乳膏相比,0.5%芦荟粉与部分皮层烧伤的完全愈合率更高相关(100%对比80%,风险比[RR]1.41,95%CI为0.70至2.85,p>0.05)。在本研究中,100%的芦荟治疗的烧伤在15.9±2天痊愈,而使用磺胺嘧啶银乳膏治疗的烧伤则需要18.73±2.65天5,8(1级)。
芦荟凝胶对深部部分皮层烧伤的疗效在一项针对二度烧伤患者(烧伤面积少于总体表面积的25%)的随机对照试验(RCT)中得到证实。患者随机接受浸泡在芦荟凝胶中的纱布(n=25)或1%磺胺嘧啶银乳膏(n=25)。芦荟组的平均愈合时间明显更快(平均11±4.18天对比平均24.24±11.16天,p<0.00001)9(1级)。
一项具有高偏倚风险的RCT10(n=120)报告称,皮肤干燥度是对芦荟治疗二度烧伤的主要评价指标。在14天的随访中,芦荟草药乳膏治疗组和磺胺嘧啶银乳膏治疗组的皮肤干燥度无显著差异(7.1%对10.9%,p>0.05)10(1级)。
一组具有高偏倚风险的病例报告了使用芦荟凝胶治疗的烧伤患者(n=4)的结局。两周后,50%的烧伤完全愈合,另外50%的烧伤在面积、水肿和红斑方面改善了80%-90%(4级)。
使用注意事项
- 芦荟与过敏反应有关,包括荨麻疹和接触性过敏性皮炎。1,4对百合科植物(如洋葱和大蒜)过敏的人应避免使用芦荟。在一项试验中,约40%的研究对象报告有刺激或瘙痒,但这与使用磺胺嘧啶银敷料治疗的研究对象并无不同。6从叶子的中心部分提取芦荟凝胶时,过敏反应可能更大,因为植物的这一部分中活性成分更为浓缩。4建议在用于烧伤之前将芦荟凝胶涂抹在一小块皮肤上作为测试。23
- 芦荟凝胶似乎是缓解烧伤患者疼痛的有效疗法。9,10在RCT中,接受芦荟凝胶治疗的二度和三度烧伤患者在视觉模拟量表上的疼痛评分明显低于接受1%磺胺嘧啶银乳膏治疗的患者。芦荟凝胶在治疗7天后(n=120人,p=0.014)和治疗14天后(n=120人,p=0.05)的疼痛管理方面效果更佳。10芦荟还与使二度烧伤患者更快达到无痛状态有关(n=50人,p=0.01)。9而芦荟的舒缓特性可能与其高含水量有关。1,18-20
- 在现代湿润伤口敷料资源有限的国家,芦荟是一种具有成本效益的伤口管理选择。在印度进行的一项成本分析报告表明,5 ml芦荟凝胶敷料的价格为2.40印度卢比,大约是使用2 g磺胺嘧啶银敷料价格的一半(成本为4.92卢比)。9
利益冲突
根据国际医学期刊编辑委员会(ICMJE)的标准,作者声明无利益冲突。
关于WHAM证据总结
WHAM证据总结的方法与Munn Z等人(Munn Z, Lockwood C, Moola S. The development and use of evidence summaries for point of care information systems:A streamlined rapid review approach, Worldviews Evid Based Nurs.2015;12(3):131-8.)发表的方法一致。
Joanna Briggs Institute14-16和WHAM合作网站(http://WHAMwounds.com)发布的资源列出了这些方法。WHAM证据总结经过国际多学科专家参考小组的同行评审。WHAM证据总结提供了关于特定主题的最佳可用证据的总结,并提出了可用于指导临床实践的建议。本总结中包含的证据应由经过适当培训的具有伤口预防和管理专业知识的专业人士进行评价,并应根据个人、专业人士、临床环境以及其他相关临床信息考虑证据。
版权所有©2021科廷大学科廷健康创新研究所伤口愈合和管理协作组织

Author(s)
Emily Haesler
PhD Post Grad Sip Adv Nurs (Gerontics) BNurs Fellow Wounds Australia
Wound Healing and Management Collaborative, Curtin Health Innovation Research Institute, Curtin University
References
- Ulbricht C, Armstrong J, Basch E, Basch S, Bent S, Dacey C, Dalton S, Foppa I, Giese N, Hammerness P, Kirkwood C, Sollars D, Tanguay-Colucci S, Weissner W. An evidence-based systematic review of aloe vera by the natural standard research collaboration. J Herb Pharmacother, 2007;7(3-4):279-323.
- Manvitha K, Bidya B. Aloe vera: A wonder plant its history, cultivation and medicinal uses. J Pharmacogn Phytochem, 2014;2(5):85-8.
- Pazyar N, Yaghoobi R, Rafiee E, Mehrabian A, Feily A. Skin wound healing and phytomedicine: A review. Skin Pharmacol Physiol, 2014;27(6):303-10.
- Maenthaisong R, Chaiyakunapruk N, Niruntraporn S, Kongkaew C. The efficacy of aloe vera used for burn wound healing: A systematic review. Burns, 2007;33(6):713-8.
- Dat AD, Poon F, Pham KB, Doust J. Aloe vera for treating acute and chronic wounds. Cochrane Database Syst Rev, 2012;2:CD008762.
- Thamlikitkul V, Bunyapraphatsara N, Riewpaiboon W, Theerapong S, Chantrakul C, Thanaveerasuwan T, Nimitnon S, Wongkonkatape S, Riewpaiboon A, Tenambergen ED. Clinical trial of aloe vera Linn. for treatment of minor burns. Siriraj Hosp Gaz, 1991;43(5):313–6.
- Akhtar MA, Hatwar SK. Efficacy of aloe vera extract cream in management of burn wound. J Clin Epidemiol, 1996;49(Suppl. 1):24.
- Khorasani G, Hosseinimehr SJ, Azadbakht M, Zamani A, Mahdavi MR. Aloe versus silver sulfadiazine creams for second-degree burns: A randomized controlled study. Surg Today, 2009;39(7):587-91.
- Shahzad MN, Ahmed N. Effectiveness of aloe vera gel compared with 1% silver sulphadiazine cream as burn wound dressing in second degree burns. J Pak Med Assoc, 2013;63(2):225-30.
- Panahi Y, Beiraghdar F, Akbari H, Bekhradi H, Taghizadeh M, Sahebkar A. A herbal cream consisting of Aloe vera, Lavandulastoechas, and Pelargonium roseum as an alternative for silver sulfadiazine in burn management. Asian Biomedicine, 2012;6(2):273-8.
- Nagar P, Magesh Kumar J, Vardharajan P. Efficacy of aloe vera gel dressing in chronic leg ulcer of diabetic, traumatic and burns origin. Res J Pharm Biol Chem Sci, 2015;6(6):482-4.
- Visuthikosol V, Sukwanara tY, Chowchuen B, Sriurairatana S, Boonpucknavig V. Effect of aloe vera gel to healing of burn wound a clinical and histologic study. J Med Assoc Thai 1995;78(8):403–8.
- Sun JH, Chen XG, Jin RT, Li TN, Bian YX. People’s Liberation Army medicine information. Med J Chin Army, 1994;8(4):191–2.
- Aromataris E, Munn Z, editors. Joanna Briggs Institute Reviewer’s Manual. 2017. https://reviewersmanual.joannabriggs.org/ The Joanna Briggs Institute.
- Joanna Briggs Institute Levels of Evidence and Grades of Recommendation Working Party. New JBI Grades of Recommendation. 2013. Adelaide: Joanna Briggs Institute.
- Joanna Briggs Institute Levels of Evidence and Grades of Recommendation Working Party. Supporting Document for the Joanna Briggs Institute Levels of Evidence and Grades of Recommendation. 2014. Adelaide: Joanna Briggs Institute.
- Andersen FA. Final report on the safety assessment of aloe andongensis extract, aloe andongensis leaf juice, aloe arborescens leaf extract, aloe arborescens leaf juice, aloe arborescens leaf protoplasts, aloe barbadensis flower extract, aloe barbadensis leaf, aloe barbadensis leaf extract, aloe barbadensis leaf juice, aloe barbadensis leaf polysaccharides, aloe barbadensis leaf water, ferox leaf extract. Int J Toxicol, 2007;26(Suppl. 2):1-50.
- Haesler E, Watts R, Rice J, Carville K. Local resource botanicals used in wound care. Wound Practice and Research, 2016;84-90.
- Lloyd ECO, Rodgers BC, Michener M, Williams MS. Outpatient burns: Prevention and care. Am Fam Physician, 2012;85(1):25-32.
- Nandal U, Bhardwaj RL. Aloe vera: A valuable wonder plant for food, medicine and cosmetic use - a review. Int J Pharm Sci Rev Res, 2012;13(1):59-67.
- Banu A, Sathyanarayana BC, Chattannavar G. Efficacy of fresh aloe vera gel against multi-drug resistant bacteria in infected leg ulcers. Australas Med J, 2012;5(6):305-9.
- Purohit SK, Solanki R, Soni M. Experimental evaluation of Aloe vera leaves pulp as topical medicament on wound. International Journal of Pharmacological Research, 2012;2(3):110-2.
- Rajeswari R, Umadevi M, Sharmila Rahale C, Pushpa R, Selvavenkadesh S, Sampath Kumar K, Bhowmik D. Aloe vera: The miracle plant its medicinal and traditional uses in India. J Pharmacogn Phytochem, 2012;1(4):118-24.


