Volume 43 Number 1
Fact-finding survey of pressure and shear force at the heel using a three-axis tactile sensor
Yoko Murooka and Hidemi Nemoto Ishii
Keywords heel pressure injury, decompression, shear force, elevating the head of the bed
For referencing Murooka Y and Ishii HN. Fact-finding survey of pressure and shear force at the heel using a three-axis tactile sensor. WCET® Journal 2023;43(1):20-27
DOI
https://doi.org/10.33235/wcet.43.1.20-27
Submitted 28 March 2022
Accepted 31 August 2022
Abstract
Aims We investigated changes in pressure and shear force at the heel caused by elevating the head of the bed and after offloading pressure from the heel.
Methods Data on heel pressure and shear force were collected from 26 healthy individuals aged >30 years using a three-axis tactile sensor at each angle formed as the participants’ upper bodies were raised from a supine position. Data after pressure release of either the left or right foot were collected and compared.
Results The participants’ mean age was 45.1 (±11.1) years. Pressure and anteroposterior shear force on the heel increased with elevation. These increases were especially prominent when the angle of elevation was 30˚. In the subsequent 45˚ and 60˚ tilts, body pressure and shear force increased slightly but not significantly. Pressure and shear force were released by elevating the lower extremity each time the head of the bed was elevated. However, further elevations resulted in increased pressure and shear force, particularly lateral shear force. Pressure and shear force did not change significantly when the lower limbs were elevated.
Conclusion The recommended elevation of the bed head to no more than 30˚ yielded major changes. Elevating the leg relieved the heel of continuous pressure and shear force while increasing pressure and lateral shear force. Although leg elevation is an aspect of daily nursing care, it is important to investigate such nursing interventions using objective data.
Introduction
In addition to the relationship between pressure intensity and time, it is clear that frictional and shear forces occur as external forces to the living body. Shear forces obstruct blood flow in the tissue, resulting in tissue ischemia1. In Japan, pressure injuries tend to develop frequently in bedridden older adults with bony prominences. They are especially susceptible to friction and shear forces due to dryness and reduced elasticity of the skin2,3. Therefore, regular repositioning is recommended for reducing pressure and shear force on the skin4.
Preventing pressure injuries requires not only systemic reduction of body pressure but also local depressurisation and reduction of shear force. When the head of a patient’s bed is elevated, the sacrum and coccyx are subjected to severe pressure and shear force, with particular changes in pressure and shear force reported in the sacral region5. In clinical practice, these problems are addressed via depressurisation, which includes pressure redistribution devices and providing daily nursing care. Two such forms of nursing care for depressurisation when a patient’s bed is elevated or lowered are senuki (literally ‘back omission’) and ashinuki (literally ‘leg omission’). Senuki involves the caregiver lifting the patient’s upper body and inserting their hand between the bed and the patient’s back to separate the body from the bed when it is elevated, thereby eliminating the friction and shear force between the patient’s skin and their bedclothes. Ashinuki involves the caregiver elevating the patient’s legs to eliminate the shear force that would otherwise occur from the hip to the posterior surface of the thigh and heel when the bed is elevated or lowered6.
When a bed is elevated, factors such as the concentration of pressure in the buttocks and the sliding down of the body create shear force. Therefore, when elevating a patient’s bed, nurses provide various forms of care such as elevating the legs first, positioning the patient in multiple methods, such as inserting a cushion under their knees to prevent slippage, and elevating the patient’s upper body7–9. However, these nursing interventions were reported in studies that examined the sacrum; few studies have examined changes in pressure or shear force on the heel10,11.
In the supine position, the heel is subjected to continuous pressure, making it vulnerable to tissue injury and pressure injuries. Pressure injuries in the heel are reported to account for one-fourth of all pressure injuries in American hospitals and nursing homes12–15. The effects of bed elevation and other factors make the heel susceptible to friction16. To reduce this friction, preventive dressings are applied17.
The present study examined the pressure and shear force on the heel using a three-axis tactile sensor. Additionally, the aim was to confirm changes in the pressure and shear force on the heel after elevating the heads of patients’ beds, followed by elevating the patients’ lower limbs.
Research Methods
Study design
A quasi-experimental study.
Selection of the participants and period of study
Healthy volunteers aged >30 years were recruited from the researchers’ universities and hospitals. The participants’ number of clinical experiences did not matter in this study design. Posters for research cooperation were displayed on a bulletin board at the facilities to call for participation. The primary author made verbal and e-mail announcements for the same, and used documents to explain the research specifications to individuals who wished to participate. Individuals signed a consent form to confirm participation.
Inclusion criteria required that participants had no wounds on their heels. Temporary redness was considered reactive hyperaemia and such participants were included.
Sample size
When G*Power18 was used to analyse the sample size with an effect size of 0.8, α of 0.05, and a statistical power of 0.8, the sample size was calculated to be n=15. Due to the possibility of an insufficient measurement effect in some participants, we set the sample size as 20. The target number of 20 participants was set to 15 to account for dropouts during data collection. However, no participant met the exclusion criteria and all were included.
Data collection
Data were collected between October 2018 and March 2019.
Measurement environment
Commonly used bedding was selected for the measurements. However, for the convenience of reproducibility, no pillows were used. Other equipment included:
- Electric bed: Paramount bed KA-5000 (4-split type) (Paramount Bed Corporation, Tokyo, Japan).
- Base mattress: Everfit KE-521Q (Paramount Bed Corporation, Tokyo, Japan); 10cm thick static mattress.
- Bed sheet: plain woven cotton sheet. The sheets were tucked in when the beds were made.
- Measuring device: Three-axis tactile sensor (ShokacChip™T08, Touchence Inc., Tokyo, Japan) 9mm × 9mm × 5mm. The x-, y- and z-axes of the three-axis sensor were set according to pressure, anteroposterior shear force, and lateral shear force, respectively (Figures 1a & b).
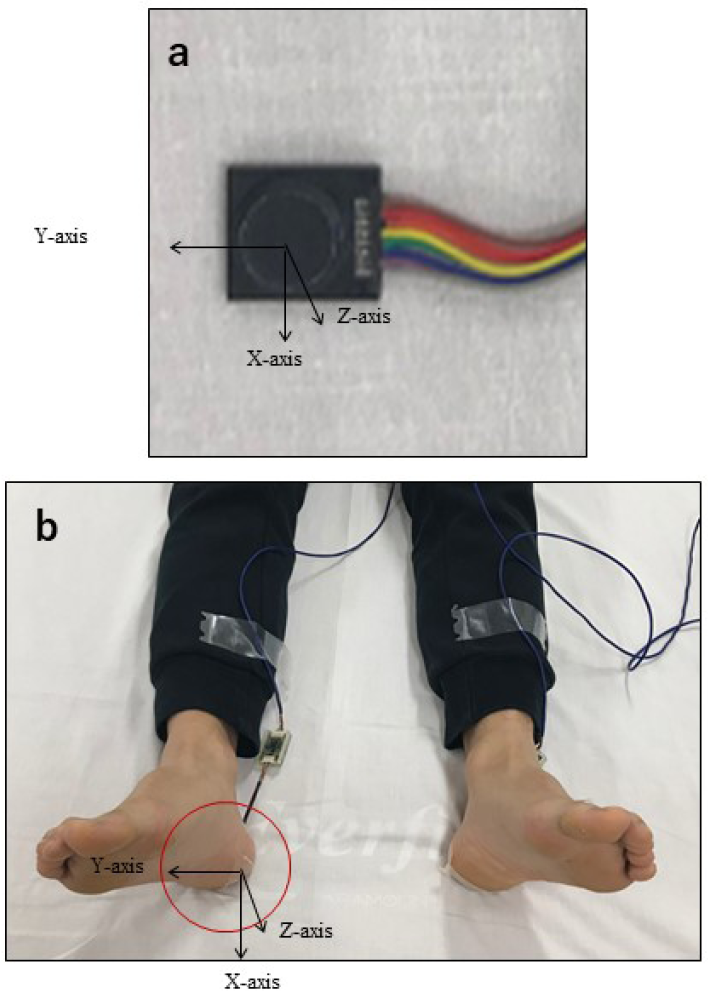
Figure 1. A tri-axial tactile sensor was attached to the skin contact area between the heel and the bed and was covered with a dressing. Three directions were measured – anteroposterior shear force (x-axis), lateral shear force (y-axis), and pressure (z-axis)
Measurement procedure
Two experiments were conducted. Experiment 1 measured the pressure and shear force on the heel. Experiment 2 measured the changes in heel pressure and shear force with and without lower limb elevation.
Experiment 1: Changes in heel pressure and shear force upon elevating the head of the bed
The participants slightly opened their lower limbs in a relaxed state and lay in a supine position with their anterior superior iliac spine aligned to the bending point of the bed. The three-axis sensor was applied to the central point of where the left or right heel touched the bed; the film dressing was applied from above (Figures 1a & b). The left or right heel was selected randomly, and the following series of data were collected:
1. After confirming that the participant’s body was still, data for the heel were collected over a 20-second period with the bed in a supine position.
2. After 20 seconds, the participant’s upper body was elevated from the bending point of the bed to a 30˚ angle measured with a goniometer (Figure 2).
3. After the participant’s upper body was elevated, data for the heel were collected while the patient lay still for 20 seconds.
4. The participant’s upper body was then elevated to 45˚ and data were collected in the same manner.
5. After the data collection for the 60˚ elevation, the bed was lowered to a supine position and data were measured for 20 seconds, concluding the experiment.
Experiment 2: Changes in heel pressure and shear force with and without lower limb elevation
As in Experiment 1, the left or right lower limb was selected randomly, and the data collection steps 1−3 in Experiment 1 were repeated. In Experiment 2, the following interventions were carried out from that state.
4. After 20 seconds, either the participant’s left or right knee and ankle were held, lifted up from the hip, and kept still in that position for 5 seconds (Figure 3).
5. After the lower limb was lowered, it was immediately elevated to a 45˚ angle and data were collected for the heel while the participant remained still for 20 seconds.
6. Similar to Step 5 in Experiment 1, after the lower limb was lowered and the head of the bed was elevated to 60˚, the same measurement was performed.
7. Finally, the head of the bed was lowered to a supine position, data were collected for 20 seconds, and the experiment was concluded.
The researcher, a certified expert nurse in wound, ostomy, and continence, conducted Experiments 1 and 2 in this study.
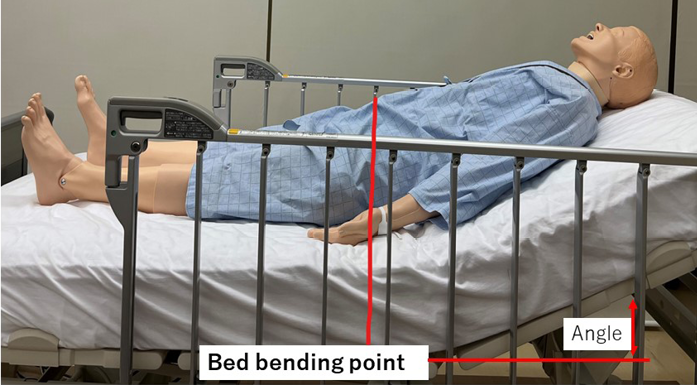
Figure 2. Lying in bed (at the time of elevating the head of the bed)

Figure 3. Lifting the lower limbs
Data analysis
Data were analysed by estimating the average of the observation points at 18 seconds without considering the seconds before and after; the influence of the anteroposterior movement data of the 20 seconds measured for each angle of elevation was also taken into account. Calculations were made by averaging the observation points without the seconds before and after. At the start of the measurement, the initial data value was calibrated to zero and measured twice. The data obtained from the sensors were analysed along the x-axis (anteroposterior shear force), y-axis (lateral shear force), and z-axis (pressure). The pressure and shear force, with and without offloading pressure from the heel at each angle, were analysed using dedicated data software and two-way ANOVA was performed. All statistical analyses were performed using SPSS 23.0 for Windows (IBM Corp. Armonk, N.Y., USA), and the significance level was set at 5%.
Ethical considerations
The study was approved by the Ethical Review Committee of the Jikei University School of Medicine, Tokyo (9212). The participants were informed of the study orally and in writing, including instructions for the study. The participants’ health status was always observed during the data measurement. They were informed that the procedure would be stopped if they experienced distress. After data collection, we looked for any adverse conditions, such as skin indentation caused by the sensor being applied to the subject’s heel or epidermal peeling caused by the application of the dressing material.
Results
Subject attributes
The study was conducted with 26 participants (11 men and 15 women) with a mean age of 45.1 (±11.1) years and mean BMI of 22.2 (±3.2). No participant met the exclusion criteria, and no adverse events occurred.
Experiment 1: Changes in heel pressure and shear force upon elevating the head of the bed
The change in pressure at the heel tended to increase and maintain its value as the head of the bed was raised (Figure 4a). In particular, the pressure increased significantly when the head of the bed was raised from the supine position to 30˚. Subsequently, the pressure values were maintained for the elevation angles of 45˚ and 60˚; no significant increase was observed. However, a significant difference was observed when the angle was changed from 60˚ to the supine position. The pressure initially dropped, but did not return to the starting pressure, which further decreased.
The shear force in the front–back direction tended to increase with the elevation angle. Similar to the pressure values found, the value increased significantly at the 30˚ angle of elevation, and a significant difference was observed. After 45˚, the anteroposterior shear force was maintained but did not increase significantly when the angle was raised from the supine position to 60˚. However, when the angle was changed from 60˚ to the supine position, shear force in the opposite direction was added and a significant difference was observed (Figure 4b).
Although the lateral shear force increased as the head of the bed was elevated, it did not change as greatly as the anteroposterior shear force. A significant difference was observed when the bed was lowered from a 60˚ angle to a supine position. However, the large changes that occurred in the anteroposterior shear force did not occur in the case of lateral shear force (Figure 4c).
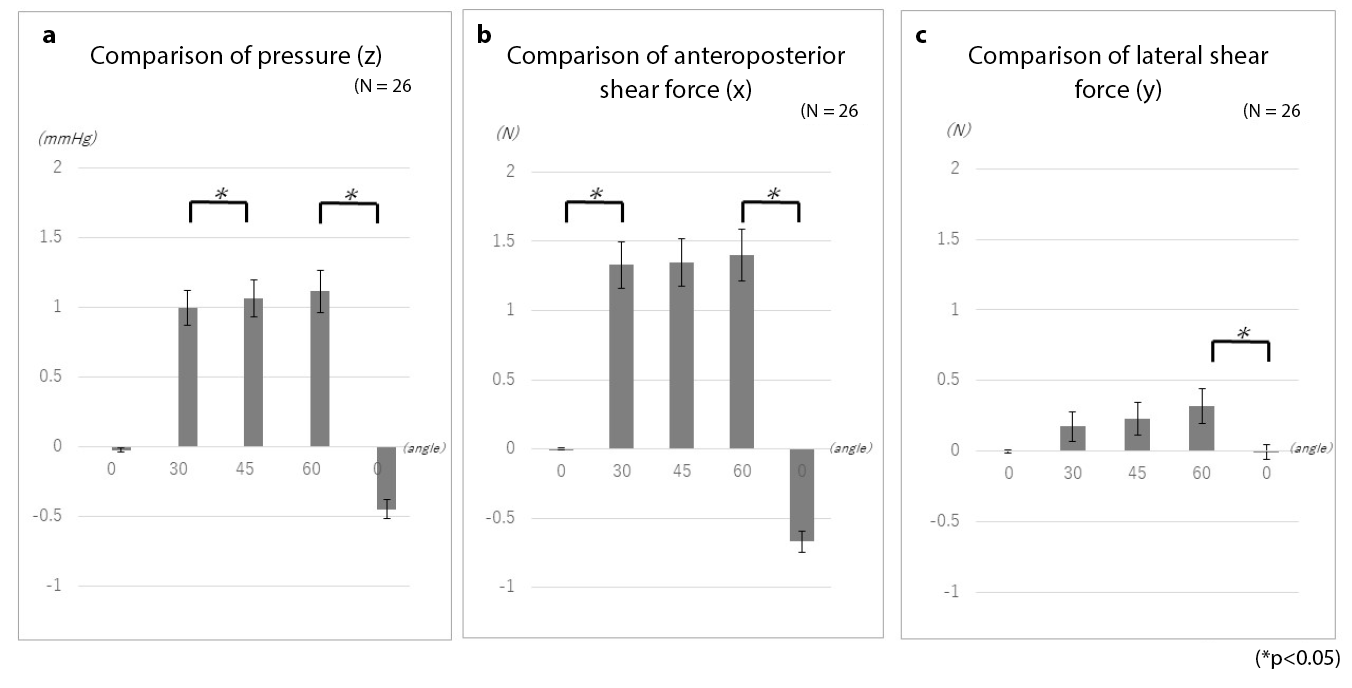
Figure 4. Changes in heel pressure and shear force while elevating the head of the bed
Experiment 2: Changes in heel pressure and shear force with and without lower limb elevation
Examinations of the changes in pressure with and without elevation of the lower limbs showed no significant differences in pressure, anteroposterior shear force, or lateral shear force (Figure 5). However, as with the measurements taken with simple elevation of the head of the bed, even when pressure and shear force were offloaded, elevating the head of the bed led to the reapplication of external force. Moreover, while the anteroposterior shear force was large when only the head of the bed was elevated, the lateral shear force increased upon lower limb elevation. An example of elevating the head of the bed is presented here to explain these changes.
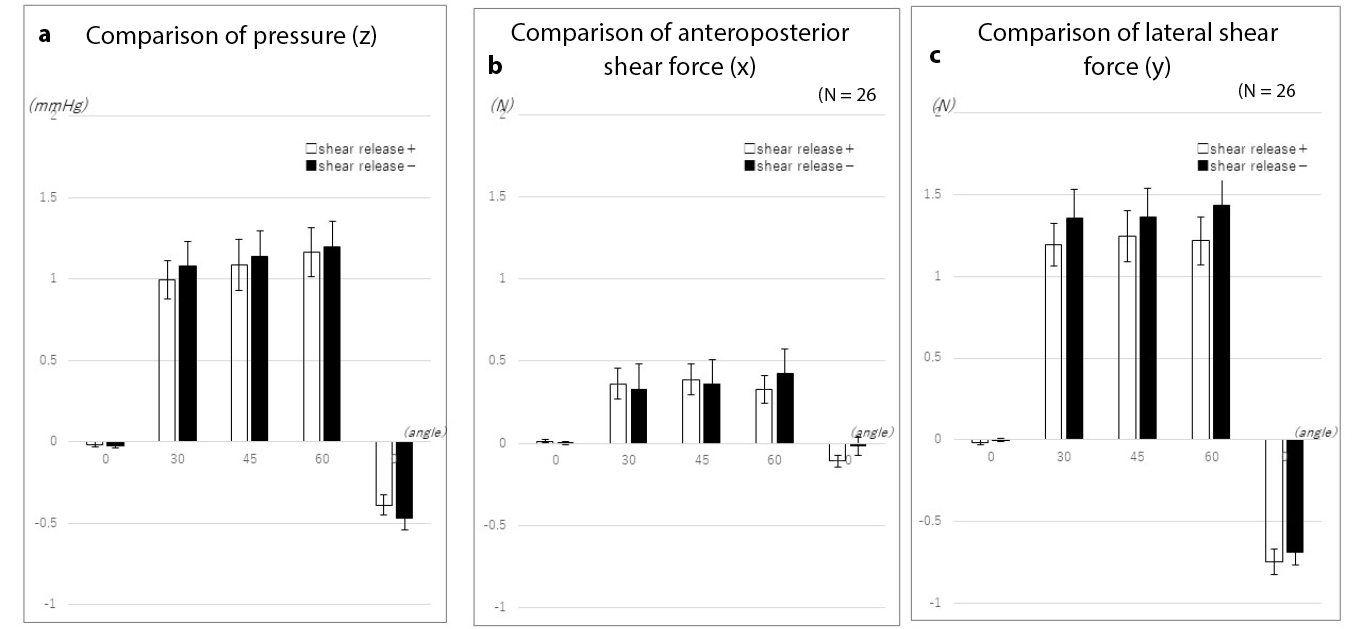
Figure 5. Changes in heel pressure and shear force with and without lower limb elevation
When the head of the bed was elevated to 30˚, elevation of the lower limbs temporarily offloaded the pressure on the heel. While further bed elevation once again increased pressure on the heel, lower limb elevation tended to inhibit subsequent increases in pressure (Figure 6a).
When the lower limbs were not elevated, the anteroposterior shear force increased slightly when the bed head was elevated to 30˚. On the other hand, when the lower limbs were elevated, no significant change occurred (Figure 6b).
Similarly, the lateral shear force increased without elevation of the lower limb when the head of the bed was elevated to 30˚. On further elevation of the head of the bed, the lateral shear force increased in the absence of lower limb elevation. The greatest change occurred when the bed returned to the supine position. When the lower limb was elevated, the lateral shear force was temporarily offloaded. However, elevating the head of the bed again created lateral shear force. Although the difference in lateral shear force when the bed returned to the supine position was smaller than the difference observed without elevation of the lower limb, the results demonstrated the occurrence of lateral shear force associated with temporary offloading of force (Figure 6c).
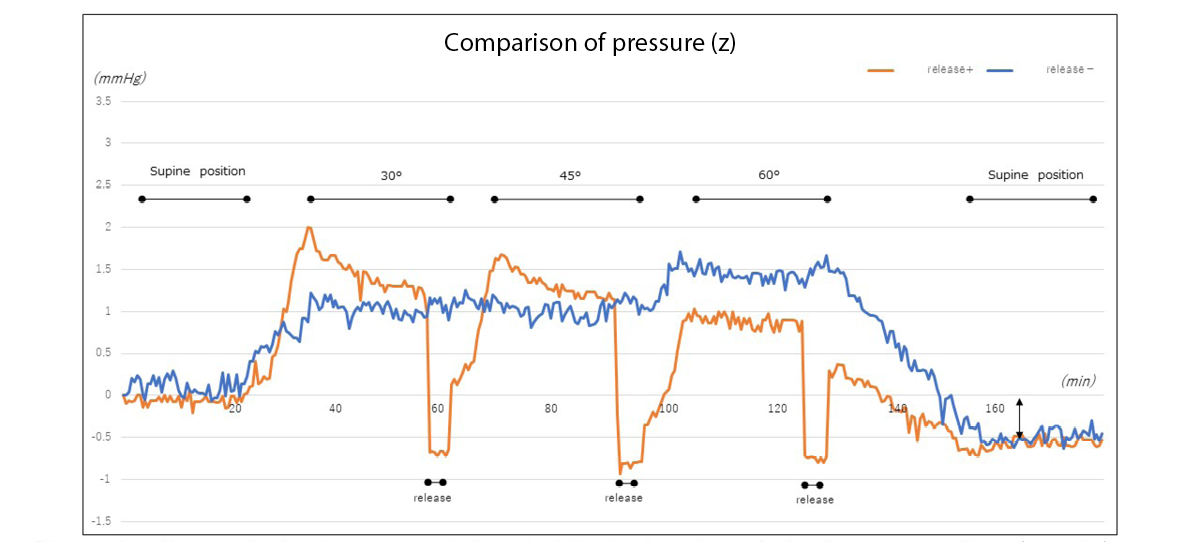
Figure 6a. Changes in heel pressure with and without elevation of the lower extremity (example)
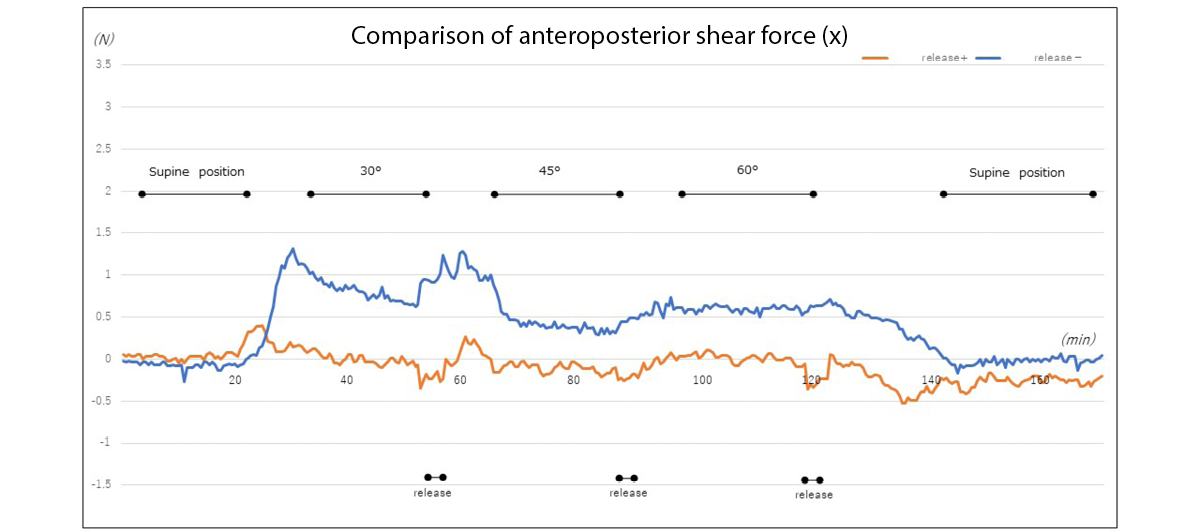
Figure 6b. Changes in anteroposterior shear force at the heel with and without elevation of the lower limb (example)
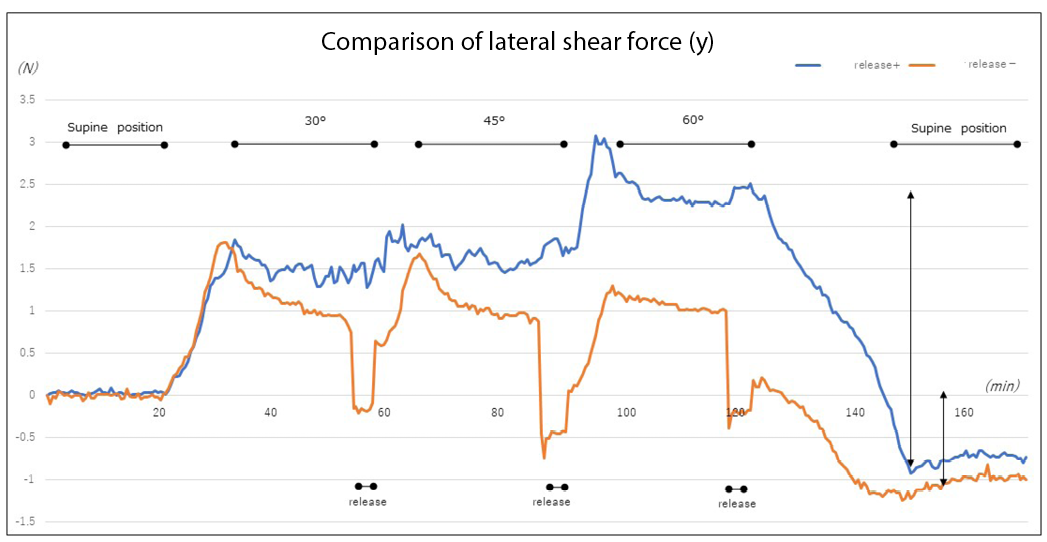
Figure 6c. Changes in lateral shear force at the heel with and without elevation of the lower limb (example)
Discussion
The experimental results revealed that the pressure and shear force at the heel increased with elevating the head of the bed. In particular, the rate of change in the values was large at the 30˚ angle of elevation. As previously reported, this is attributed to the effect of the centre of gravity shifting and upper body sliding down due to head elevation17–19. From the viewpoint of preventing pressure injury in the buttocks, it is desirable that the angle of elevating the head of the bed be 30˚ or less20. Although the 30˚ rule”(30˚ lateral supine, elevating the head of the bed by 30˚) has been widely used in positioning to prevent pressure injury, it has also been reported to delay healing in patients with pressure injury in the buttocks21. Therefore, the 4th edition of the Guidelines for the Prevention and Management of Pressure Ulcers states that positioning other than the 30˚ side-lying and 30˚ supine positions may be performed22.
The heel is a common site of pressure injuries. Even if a visual assessment identifies no problems, tissue injury occurs, leading to deep tissue injury (DTI) due to changes inside the tissue. When pressure injuries are detected by a physician, the skin is often discoloured and injured, with DTI having already occurred16. As the heel is known to have a lower concentration of melanocytes, tissue response to stress and tissue injury are difficult to detect based on changes in skin colour23. In addition, while the epidermis may be thick in the lateral aspect of the sole of the heel, the skin of the posterior heel is relatively thin. In older adults and patients with fragile skin, capillary density is low and mass is reduced throughout the soft tissue in the posterior heel, adversely affecting the linkage between the epidermis and skin junctions24, conceivably increasing the risk of pressure injuries. Similar results were observed among the present study’s participants, despite having a mean BMI of 22.2 (±3.2) and standard body type. The participants’ BMI led to changes in mass throughout the soft tissue in the posterior heel. Conceivably, BMI and heel bone geometry also affected the linkage between the epidermis and skin junctions, suggesting an effect on pressure and shear force as well.
The present experiments demonstrated that powerful pressure and shear force occur when the head of a hospital bed is elevated to the recommended angle of 30˚. In the initial measurement, the head of the bed was elevated with the participant’s superior anterior iliac spine aligned with the bending point of the bed to prevent the body from sliding down. However, because the knees are not elevated and the heels are not supported, continuous strain on soft tissue leads to tissue injury25 and multiple thrombosis26, often causing DTI. In fact, this strain was shown to act as the anteroposterior and lateral shear forces due to elevation of the head of the hospital bed, elevation of the lower limbs, and other acts of nursing care. Although the lower limbs are elevated as a form of preventive care, we learned that this elevation does not entirely eliminate external force. This finding suggests the need for further preventive measures based on objective data.
The application of polyurethane foam/soft silicon foam to the heel has been reported to reduce friction and shear force on the heel, resulting in prevention of pressure injuries27,28. The skin of elder adults is dry, resulting in friction even when they sleep on bedsheets. The application of moisturiser, particularly the use of ceramide-containing formulations, to moisturise dry skin daily is reported to be an effective nursing intervention29; therefore, this intervention is also important to incorporate. European Pressure Ulcer Advisory Panel guidelines also recommend the use of sheets made of silk or other similar material instead of cotton or cotton blends to reduce friction and shear force30.
Considering the advancements in body pressure redistribution devices, repositioning at conventional 2-hour intervals is reported to not differ from repositioning at 3- or 4-hour intervals31. When a patient’s body is repositioned (or their posture is maintained), it is supported with cushions and pillows. Although this study used four-section hospital beds, data in the present experiments were collected for the heel with only participants’ upper bodies being elevated and without elevation of the lower limb. However, with a bed that permits elevation of the lower limbs, conventional positioning requires elevation of the lower extremity side of the bed to prevent posture collapse and reduce pressure on the buttocks associated with the sliding down of the upper body; elimination of external force through means such as lower limb elevation may thus be required. Patients’ bodies are repositioned to regularly change their recumbent position and shift the external force that would otherwise continue to act on the same site.
However, while voluntary movement is also important, it is sometimes difficult for patients who have trouble moving on their own. In Japan, studies are being conducted on ‘small changes’, a body pressure dispersal method involving the use of a small pillow. ‘Small changes’ refers to a method in which a small pillow is moved at regular intervals to the shoulder, hip or lower extremity on one side of the body to change the site on which pressure acts and thus redistribute pressure. This method has been reported to reduce the incidence of pressure injuries32,33. Furthermore, an air mattress equipped with such a small change system has been developed, with a study having reported on its efficacy in preventing pressure injuries34.
Along with the measures described above to prevent pressure injuries in the heel, ultrasonography is also being used to detect pressure injuries at an early stage without relying on visual assessment35. Acquiring more basic data, such as that obtained in the present experiment, may be necessary.
More comments are needed on what is currently known about nursing interventions such as repositioning, frequency of repositioning to reduce pressure, shear force and friction, and the use of a knee-break or knee elevation capability of beds or simple devices such as pillows, etc to alleviate heel pressure shear and friction.
Limitations of the study and future challenges
In this study, the target age group was relatively young. Their skin structure in the heel region differs from that of older adults, who are more prone to pressure injury, and there are limitations when comparing with patients who are more prone to pressure injury. The mattress used was a urethane mattress, which is used to prevent pressure injury; hence, the effects of using other materials, such as an air mattress, need to be examined in the future.
Based on these results, we intend to consider more clinically-relevant positioning and pressure redistribution methods in the future. Additionally, we would like to check the changes occurring in not only the heel region but also the sacral region and other bone protrusion sites and collect data to provide evidence for nursing practice.
Conclusions
When elevation was performed, the pressure and shear force on the heel increased significantly at 30˚. The elevation of the lower limbs led to an offloading of continuous pressure and shear force on the heel, although the differences were not significant. However, we noted the pressure and shear force that occurred while elevating the head of the bed and determined that elevation of the lower limbs, a typical act of nursing care, does not prevent the application of shear force. Further examination with more objective data will be conducted to examine preventive nursing interventions.
Acknowledgements
We would like to thank all the study participants for their cooperation. We would also like to thank Editage (www.editage.com) for English language editing.
Conflict of interest
There are no conflicts of interest to declare.
Ethics statement
The study was approved by the Ethical Review Committee of the Jikei University School of Medicine, Tokyo (9212).
Funding
This study received a research grant from the School of Nursing, the Jikei University School of Medicine. However, they were not involved in any aspect of the study content, including study design, data collection, analysis, or interpretation of data; they only provided funding.
使用三轴触觉传感器对足跟压力和剪切力进行的实情调查
Yoko Murooka and Hidemi Nemoto Ishii
DOI: https://doi.org/10.33235/wcet.43.1.20-27
摘要
目的 我们研究了抬高床头和足跟减压后引起的足跟压力和剪切力的变化。
方法 从26名年龄30岁以上的健康受试者中收集足跟压力和剪切力的数据,在受试者的上半身以不同角度从仰卧位抬起时,使用三轴触觉传感器测量每个角度下的数据。收集左、右足压力释放后的数据并进行比较。
结果 受试者的平均年龄为45.1(Å}11.1)岁。足跟压力和前后向剪切力随着床头抬高而増加。当抬高角度为30Åã时,上述变化尤为明显。在随后将床倾斜至45Åã和60Åã角时,身体压力和剪切力略有増加,但不显著。每次抬高床头时,通过抬高下肢来释放压力和剪切力。然而,进一步抬高会导致压力和剪切力増加,特别是横向剪切力。当下肢被抬高时,压力和剪切力无显著变化。
结论 建议将床头抬高到不超过30Åã,可产生重要变化。抬高腿部缓解了足跟的持续压力和剪切力,同时増加了压力和横向剪切力。虽然抬高腿部是日常护理的一个方面,但使用客观数据研究此类护理干预措施很重要。
引言
除了压力强度和时间之间的关系外,很明显摩擦力和剪切力是作为外力作用于生命体的。剪切力阻碍组织内的血流,导致组织缺血1。在日本,压力性损伤往往经常发生在有骨质突出的卧床老人身上。由于皮肤干燥和弹性降低,他们特别容易受到摩擦力和剪切力的影响2,3。因此,建议定期改变体位以减少对皮肤的压力和剪切力4。
预防压力性损伤不仅需要降低全身压力,还需要局部减压和减少剪切力。当患者的床头被抬高时,骶骨和尾骨会承受严重的压力和剪切力,据报告,骶骨区域的压力和剪切力变化尤为明显5。在临床实践中,这些问题可以通过减压来解决,包括使用压力再分配装置和提供日常护理。当患者的床头被抬高或降低时,有两种减压护理形式,即senuki(字面意思是“背部省略”)和ashinuki(字面意思是“腿部省略”)。 Senuki是指护理人员将患者的上半身抬起,将手插入床与患者的背部之间,以便在床头被抬高时使身体与床分离,从而消除患者皮肤与被褥之间的摩擦力和剪切力。Ashinuki是指护理人员将患者双腿抬高,以消除在抬高或降低床头时从臀部到大腿后表面和足跟的剪切力6。
当床头被抬高时,臀部压力集中和身体向下滑落等因素会产生剪切力。因此,在抬高患者床头时,护士会提供各种形式的护理,例如先抬高双腿,采取在膝下插入垫子防止打滑、抬高患者上半身等多种方法安置患者体位7-9。然而,这些护理干预措施是在检查骶骨的研究中报告的;很少有研究检查足跟压力或剪切力的变化10,11。
在仰卧位时,足跟承受持续的压力,容易受到组织损伤和压力性损伤。据报告,在美国医院和疗养院的全部压力性损伤中,足跟压力性损伤占四分之一12-15。床头抬高和其他因素的影响使足跟容易受到摩擦的影响16。为了减少这种摩擦,使用了预防性敷料17。
本研究使用三轴触觉传感器检查了足跟的压力和剪切力。此外,研究目的是确认在抬高患者床头然后再抬高患者的下肢后,足跟压力和剪切力的变化。
研究方法
研究设计
一项准实验研究。
受试者和研究期的选择
从研究人员所在的大学和医院招募了年龄30岁以上的健康志愿者。在这项研究设计中,受试者的临床经验数量并不重要。研究合作的海报被张贴在机构的公告板上,呼吁人们参与。主要作者以口头和电子邮件的方式发布了同样的公告,并使用文件向希望参与的个人解释研究规范。每个人签署一份知情同意书以确认参与。
纳入标准要求受试者的足跟没有伤口。暂时性的发红被认为是反应性充血,有此情况的受试者被纳入。
样本量
采用G*Power18分析样本量时,效应量为0.8,Éø为0.05,统计功效为0.8,计算出样本量为n=15。由于部分受试者可能存在测量效应不足的问题,我们将样本量定为20个。考虑到数据收集期间的退出情况,20名受试者的目标人数被设定为15人。然而,没有受试者符合排除标准,所有受试者均被纳入。
数据收集
数据收集时间为2018年10月至2019年3月。
测量环境
选择常用的床上用品进行测量。然而,为了便于进行再现性测量,未使用枕头。其他设备包括:
- 电动床:Paramount电动床KA-5000(四分体式)(Paramount Bed Corporation,日本东京)。
- 底垫:Everfit KE-521Q(Paramount Bed Corporation,日本东京);10 cm厚静态床垫。
- 床单:平纹棉布床单。铺床时,将床单塞进去。
- 测量设备:三轴触觉传感器(ShokacChip˛ T08, Touchence Inc.,日本东京)9 mmÅ~9 mmÅ~5 mm。三轴传感器的x轴、y轴和z轴分别根据压力、前后向剪切力和横向剪切力进行设置(图1a和b)。
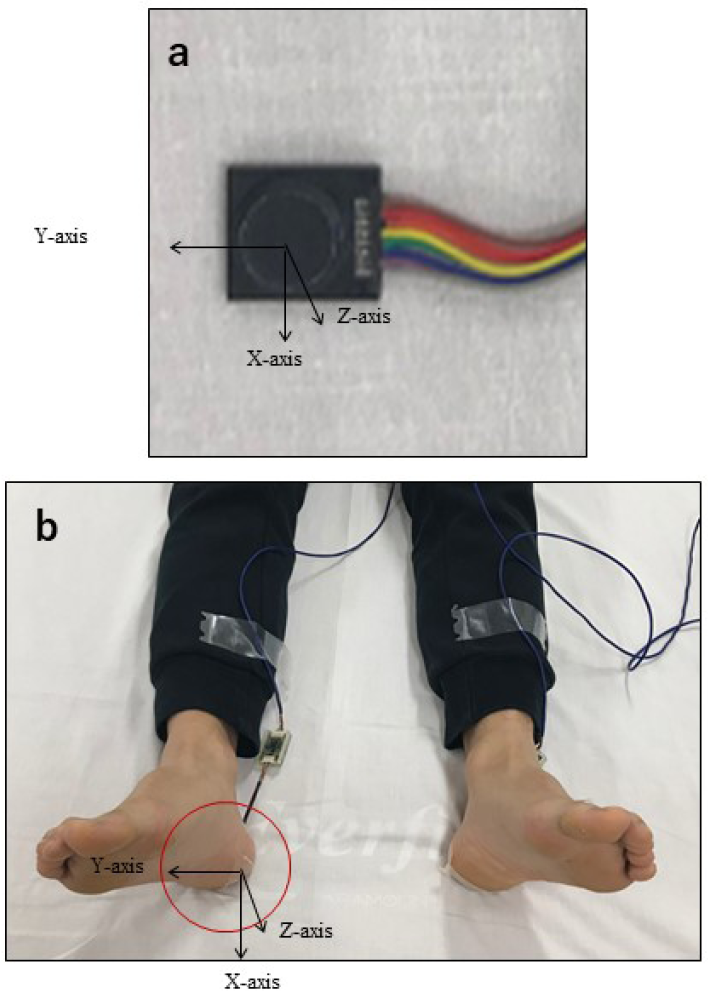
图1.将一个三轴触觉传感器连接到足跟和床之间的皮肤接触区域,并用敷料覆盖。测量了三个方向Å\Å\前后向剪切力(X轴)、横向剪切力(Y轴)和压力(Z轴)。
测量过程
进行了两项实验。实验1测量了足跟压力和剪切力。实验2测量了在下肢抬高和不抬高的情况下足跟压力和剪切力的变化。
实验1:抬高床头时足跟压力和剪切力的变化
受试者在放松状态下微微张开下肢,以仰卧位躺下,髂前上棘对准床的弯曲点。将三轴传感器置于左足跟或右足跟接触床面的中心点;从上方施用薄膜敷料(图1a和b)。随机选择左足跟或右足跟,收集以下一系列数据:
1. 确认受试者身体处于静止状态后,在床处于仰卧位的情况下,在20秒内收集足跟数据。
2. 20秒后,将受试者的上半身从床的弯曲点抬高至用测角仪测量的30Åã角(图2)。
3. 在受试者的上半身被抬高后,保持患者静止不动,收集20秒的足跟数据。
4. 然后将受试者的上半身抬高至45Åã,以同样的方式收集数据。
5. 收集完抬高至60Åã的数据后,将床降至仰卧位,进行20秒的数据测量,结束实验。
实验2:在下肢抬高和不抬高的情况下,足跟压力和剪切力的变化
与实验1一样,随机选择左下肢或右下肢,并重复实验1中的数据收集步骤1-3。在实验2中,从该状态开始进行以下干预。
4. 20秒后,握住受试者的左膝或右膝以及脚踝,从臀部抬起,并保持该姿势5秒(图3)。
5. 将下肢放下,然后立即将床头抬高至45Åã角,在受试者保持静止的情况下收集足跟数据,持续20秒。
6. 与实验1中的步骤5类似,在下肢放下后,将床头抬高至60Åã,进行同样的测量。
7. 最后,将床头降至仰卧位,收集数据20秒,实验结束。
研究人员是一名伤口、造口、失禁方面的认证专家护士,在本研究中执行了实验1和实验2。
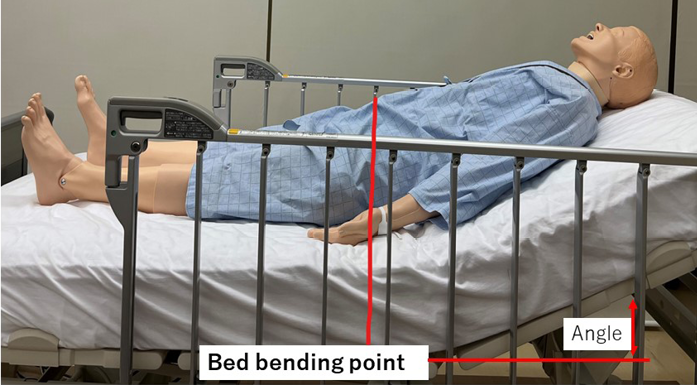
图2.躺在床上(抬高床头时)

图3.抬起下肢
数据分析
通过估计18秒时的观察点平均值来分析数据,不考虑之前和之后的秒数;还考虑了每个抬高角度进行的20秒测量的前后向运动数据的影响。计算方法是计算观察点的平均值,而不考虑观察点之前和之后的秒数。在测量开始时,将初始数据值校准为零并测量两次。从传感器获得的数据沿x轴(前后向剪切力)、 y轴(横向剪切力)和z轴(压力)进行分析。使用专门的数据软件分析了每个角度的压力和剪切力(在足跟减压和不减压的情况下),并进行了双因素方差分析(ANOVA)。所有的统计分析均使用SPSS 23.0 Windows版(IBM Corp.,Armonk,N.Y.,USA)进行,显著性水平被设定为5%。
伦理事宜
研究获得了东京慈惠会医科大学伦理审查委员会的批准(9212)。受试者被口头和书面告知本研究,包括研究说明。在数据测量过程中,始终对参与者的健康状况进行观察。他们被告知,如果他们感到痛苦,测量过程将会停止。在收集数据后,我们检查了是否存在任何不良情况,例如传感器应用于受试者的足跟而造成的皮肤压痕或应用敷料造成的表皮剥脱。
结果
受试者特征
研究有26名受试者(11名男性和15名女性)参与,平均年龄为45.1(Å}11.1)岁,平均BMI为22.2(Å}3.2)。无受试者符合排除标准,也未发生不良事件。
实验1:抬高床头时足跟压力和剪切力的变化
随着床头抬高,足跟的压力变化趋于増加,并维持在一个压力值(图4a)。特别是当床头从仰卧位抬高至30Åã时,压力显著増加。随后,抬高至45Åã和60Åã角时,压力值保持稳定;未观察到显著増加。然而,当角度从60Åã变为仰卧位时,观察到显著差异。压力最初下降,但未恢复到起始压力,而是进一步下降。
前后方向的剪切力随着抬高角度的増加而趋于増加。与压力值结果相似,在30Åã的抬高角度下,剪切力值显著増加,并观察到显著差异。抬高至45Åã后,前后向剪切力保持稳定,当角度从仰卧位抬高至60Åã时,无显著増加。然而,当角度从60Åã变为仰卧位时,相反方向的剪切力増加,并观察到显著差异(图4b)。
尽管横向剪切力也随着床头抬高而増加,但变化幅度没有前后向剪切力大。当床体角度从60Åã角降至仰卧位时,观察到显著差异。然而,横向剪切力并未发生在前后向剪切力中观察到的巨大变化(图4c)。
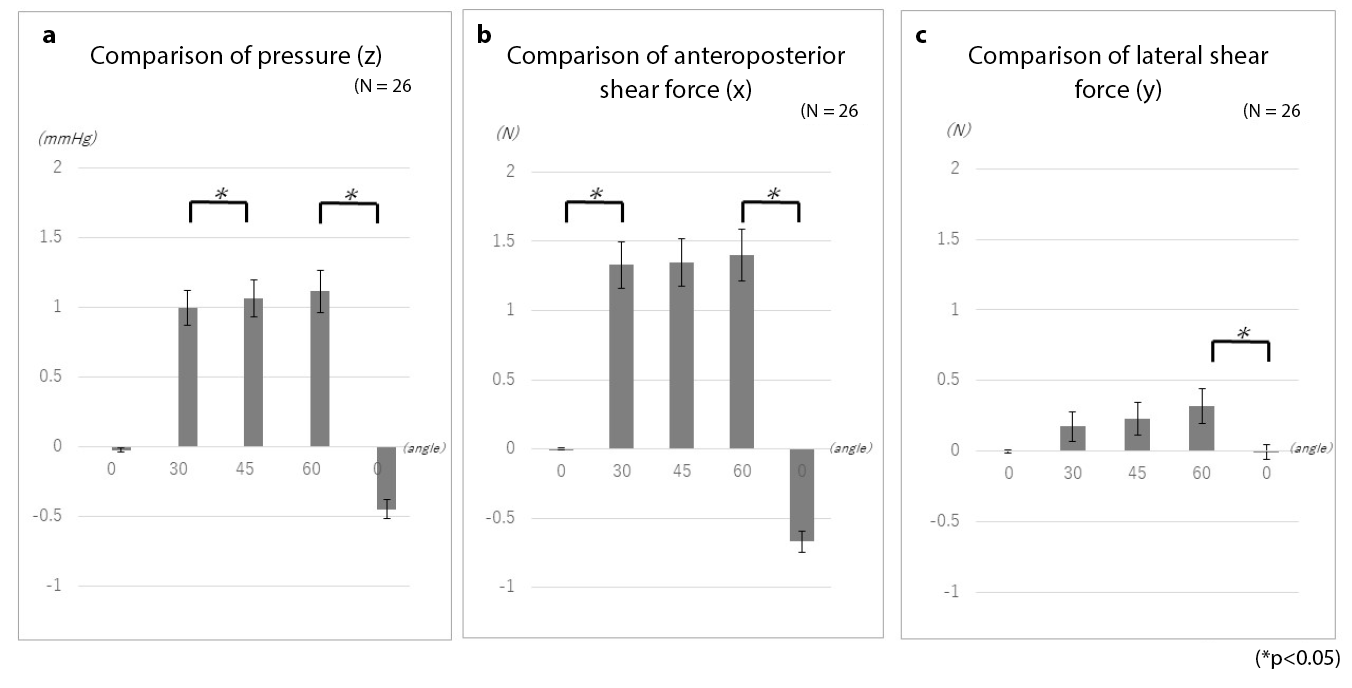
图4.抬高床头时足跟压力和剪切力的变化
实验2:在下肢抬高和不抬高的情况下,足跟压力和剪切力的变化
对下肢抬高和不抬高情况下的压力变化进行检查,结果显示压力、前后向剪切力和横向剪切力无显著差异(图5)。然而,与通过简单抬高床头进行的测量一样,即使暂时将压力和剪切力减轻,抬高床头也会导致重新施加外力。此外,当仅抬高床头时,前后向剪切力较大,而下肢抬高时,横向剪切力増加。这里举一个抬高床头的例子来解释这些变化。
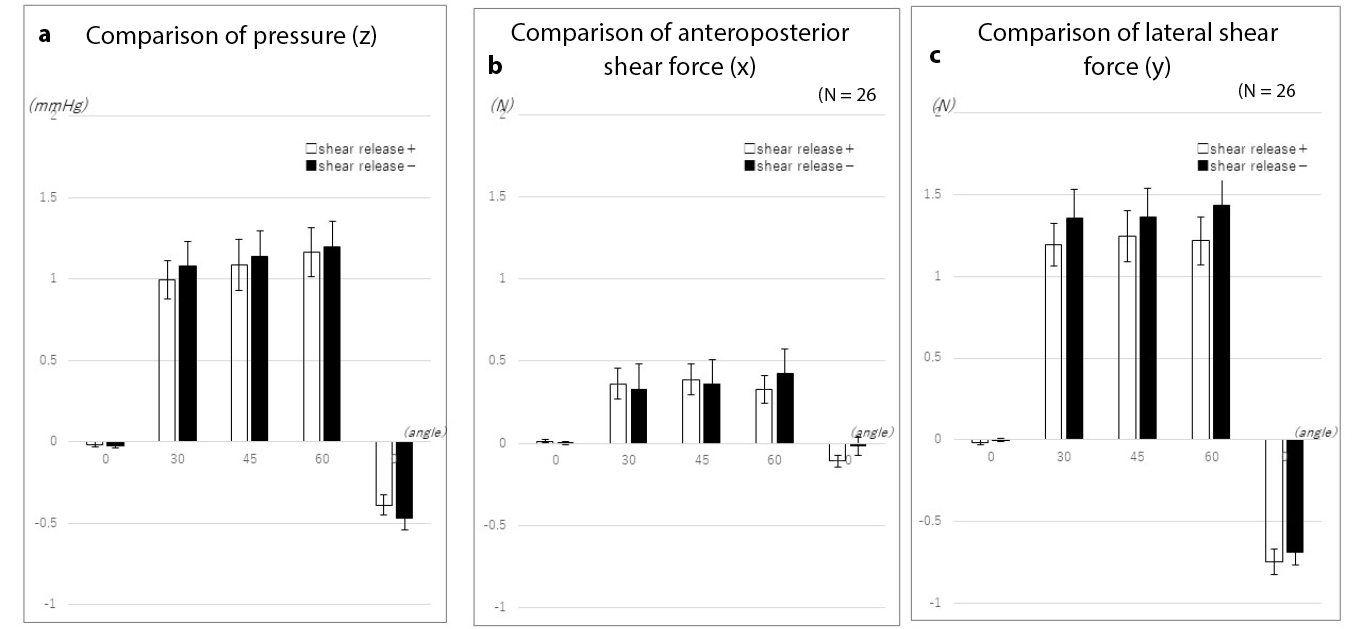
图5.在下肢抬高和不抬高的情况下,足跟压力和剪切力的变化
当床头抬高至30Åã时,抬高下肢暂时减轻了足跟的压力。虽然进一步抬高床头会再次増加足跟压力,但抬高下肢往往会抑制随后的压力増加(图6a)。
当下肢未被抬高,床头抬高至30Åã时前后向剪切力略有増加。另一方面,当下肢被抬高时,未发生显著变化(图6b)。
同样,当床头抬高至30Åã时,横向剪切力在下肢不抬高的情况下増加。当床头进一步抬高时,在未抬高下肢的情况下,横向剪切力増加。最大的变化发生在床位恢复至仰卧位时。当下肢被抬高时,横向剪切力暂时减轻。然而,抬高床头又产生了横向剪切力。尽管当床位恢复到仰卧位时,横向剪切力的差异比不抬高下肢时观察到的差异要小,但结果表明,横向剪切力的发生与临时减压有关(图6c)。
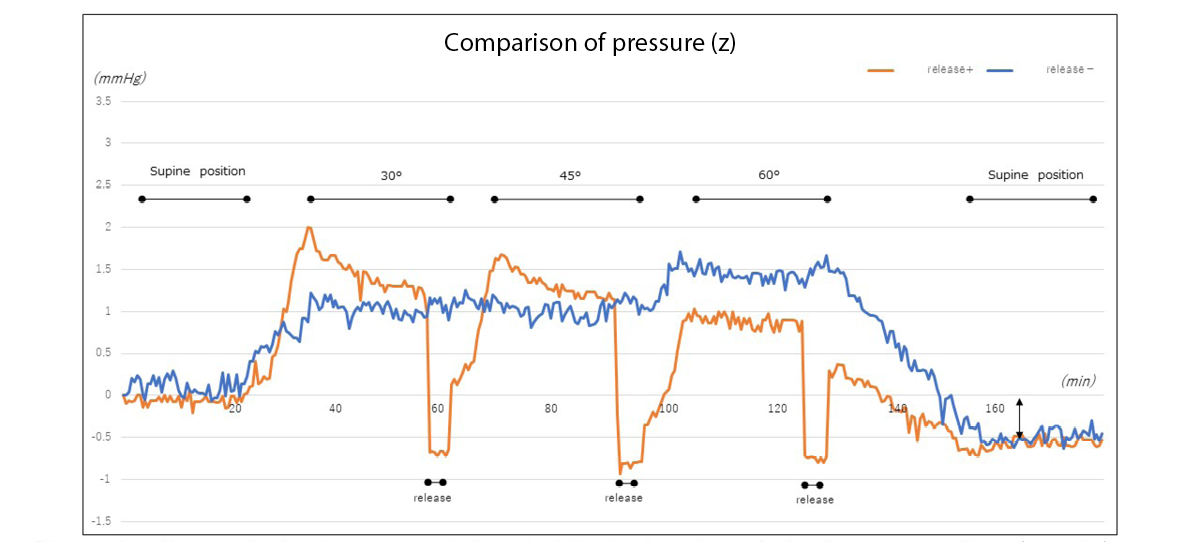
图6a.在下肢抬高和不抬高的情况下,足跟压力的变化(示例)
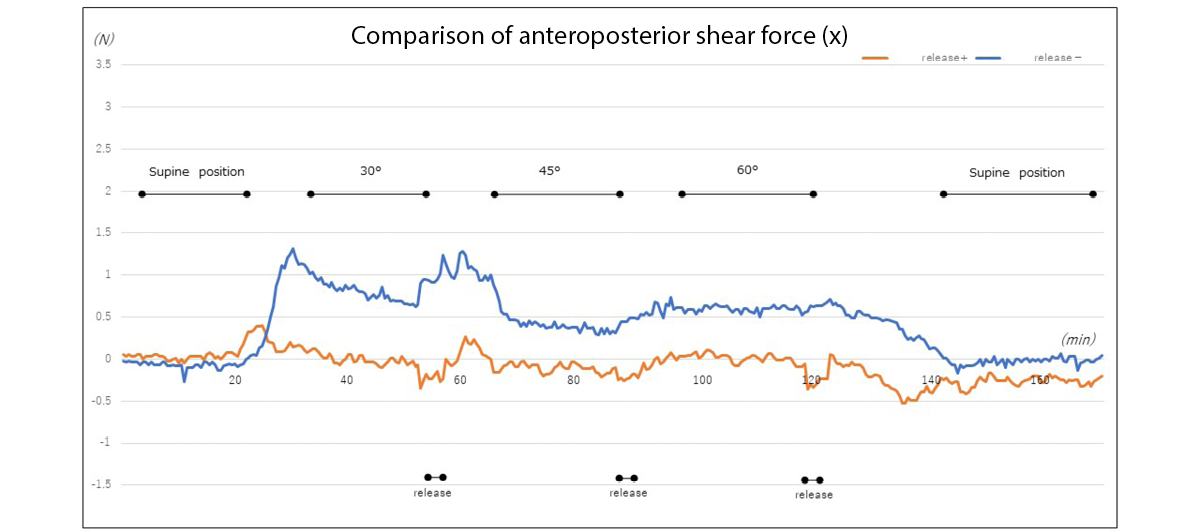
图6b.在下肢抬高和不抬高的情况下,足跟前后向剪切力的变化(示例)
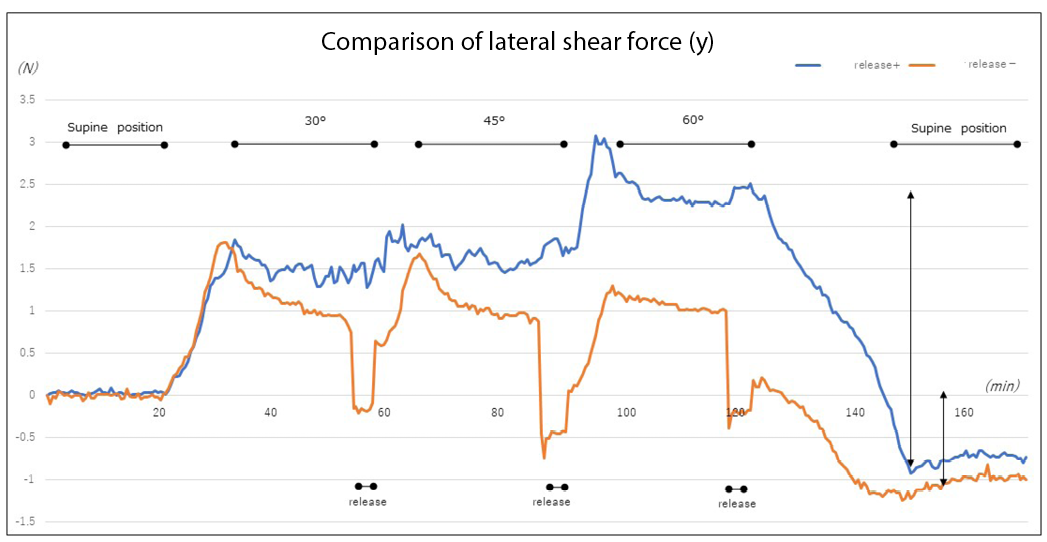
图6c.在下肢抬高和不抬高的情况下,足跟横向剪切力的变化(示例)
讨论
实验结果显示,足跟的压力和剪切力随床头抬高而増加。特别是当抬高角度为30Åã时,数值变化率很大。根据既往文献报告,这是由于重心转移和上半身因床头抬高而向下滑动17-19。从预防臀部压力性损伤的角度来看,床头抬高角度最好是30Åã或更低20。尽管“30Åã规则”(30Åã侧卧,将床头抬高至30Åã)已广泛用于预防压力性损伤的体位安置,但也有报告称该规则会延迟臀部压力性损伤患者的愈合21。因此,第四版《压疮防治指南》指出,可以采取30Åã侧卧位和30Åã仰卧位以外的体位22。
足跟是发生压力性损伤的常见部位。即使视觉评估没有发现问题,也会发生组织损伤,导致因组织内部变化而产生的深部组织损伤(DTI)。当医生检查发现压力性损伤时,皮肤往往已变色和损伤,DTI已经发生16。由于足跟的黒素细胞浓度较低,因此很难根据皮肤颜色的变化来检测组织对压力的反应和组织损伤23。此外,虽然足跟底部外侧的表皮可能很厚,但足跟后部的皮肤相对较薄。对于老年人和皮肤脆弱的患者,其毛细血管密度低,整个足跟后部的软组织质量减少,对表皮和皮肤连接处之间的连接产生不利影响24,可以想象会増加压力性损伤的风险。在本研究的受试者中也观察到类似的结果,尽管他们的平均BMI为22.2(Å}3.2),而且是标准体型。受试者的BMI导致整个足跟后部软组织的质量变化。可以想象,BMI和足跟骨的几何形状也会影响表皮和皮肤连接处之间的连接,这表明对压力和剪切力也有影响。
本实验表明,当医院的床头被抬高至建议的30Åã角时,会产生强大的压力和剪切力。在最初的测量中,床头被抬高时,将受试者的髂前上棘与床的弯曲点对齐,以防止身体下滑。然而,由于膝盖未被抬高,足跟未得到支撑,软组织持续受力导致组织损伤25和多发性血栓形成26,通常会导致DTI。事实上,这种应变被证明是由于抬高医院床头、抬高下肢以及其他护理行为而产生的前后向和横向剪切力。虽然将抬高下肢作为一种预防性护理,但我们了解到,这种抬高并不能完全消除外力。这一发现表明,需要根据客观数据采取进一步的预防措施。
据报告,在足跟处使用聚氨酯泡沫/软硅泡沫可以减少足跟的摩擦和剪切力,从而预防压力性损伤27,28。老年人皮肤干燥,因此即使睡在床单上也会产生摩擦。据报告,每天使用润肤霜,特别是使用含神经酰胺配方的润肤霜来滋润干燥的皮肤,是一种有效的护理干预措施29;因此,纳入这种干预措施也很重要。欧洲压疮咨询委员会的指南还建议使用丝绸或其他类似材料制成的床单,而非棉或棉混纺床单,以减少摩擦和剪切力30。
考虑到身体压力再分配装置的进步,据报告,以传统的2小时间隔改变体位与以3或4小时间隔改变体位没有区别31。当改变患者体位(或保持他们的姿势)时,要用垫子和枕头来支撑。虽然本研究使用了四节病床,但本实验中的数据是在仅将受试者上半身抬高而不抬高下肢的情况下收集的足跟数据。然而,对于允许抬高下肢的床来说,传统体位需要将床的下肢侧抬高,以防止姿势塌陷并减轻因上半身下滑对臀部产生的压力;因此可能需要通过抬高下肢等方式来消除外力。通过更换患者体位来定期改变其卧位,并转移原本将继续作用于同一部位的外力。
然而,虽然自主运动也很重要,但对于自己行动有困难的患者来说,有时很难做到自主运动。在日本,研究人员正在对“小幅调整”进行研究,这是一种包括使用一个小枕头来分散身体压力的方法。“小幅调整”指的是将一个小枕头定期移动到身体一侧的肩部、臀部或下肢,改变压力作用的部位,从而重新分配压力的方法。据报告,这种方法可以减少压力性损伤的发生率32,33。此外,还开发了一种配备这种小幅调整系统的气垫,一项研究报告了其在预防压力性损伤方面的效果34。
除了上述预防足跟压力性损伤的措施外,超声检查也被用于在早期检查压力性损伤,不再仅依赖于视觉评估35。可能需要获得更多的基本数据,例如本实验中获得的数据。
对于目前已知的护理干预措施也需要了解更多的评论,例如改变体位、采取适当的体位改变频率来减少压力、剪切力和摩擦力,以及使用具备弯折膝盖或抬高膝盖功能的床或枕头等简单设备来减轻足跟压力、剪切力和摩擦力。
研究的局限性和未来的挑战
在本研究中,目标年龄组相对年轻。其足跟区域的皮肤结构与老年人不同,老年人更容易发生压力性损伤。因此与更容易发生压力性损伤的患者相比,存在局限性。使用了聚氨酯床垫来预防压力性损伤;因此,未来需要研究使用其他材料(例如气垫)的效果。
基于这些结果,我们打算在未来考虑更多与临床相关的体位放置和压力再分配方法。此外,我们希望不仅要检查发生在足跟区域的变化,还要检查发生在骶骨区和其他骨突起部位的变化,并收集数据,为护理实践提供证据。
结论
当床头抬高角度为30Åã时,足跟的压力和剪切力显著増加。抬高下肢减轻了足跟受到的持续压力和剪切力,尽管差异并不显著。然而,我们注意到在抬高床头时产生的压力和剪切力,并确定抬高下肢这一典型的护理行为并不能阻止剪切力的施加。将使用更多客观数据进行进一步考察,以研究预防性护理干预措施。
致谢
我们要感谢所有研究受试者的配合。我们还要感谢Editage(www.editage.com)的英文编辑工作。
利益冲突声明
本研究无任何利益冲突需要声明。
伦理声明
研究获得了东京慈惠会医科大学伦理审查委员会的批准(9212)。
资金支持
本研究获得了慈惠会医科大学护理学院的研究资助。但是他们不涉及研究内容的任何方面,包括研究设计、数据收集、数据分析或数据解释;他们只提供资金。
Author(s)
Yoko Murooka*
RN, PhD, WOCN
Faculty of Nursing, Tokyo University of Information Sciences,
4–1 Onaridai, Wakaba-ku, Chiba, 265–8501 Japan
Email myoko0913@gmail.com
Hidemi Nemoto Ishii
RN, MSN, ET/WOCN
Wound & Ostomy Care Division, ALCARE Co. Ltd., Sumida-ku,
Tokyo, Japan
* Corresponding author
References
- Manorama A, Meyer R, Wiseman R, Bush T. Quantifying the effects of external shear loads on arterial and venous blood flow: implications for pressure ulcer development. Clin Biomech 2013;28(5):574–78.
- Leyva-Mendivil MF, Lengiewicz J, Page A, et al. Skin microstructure is a key contributor to its friction behaviour. Tribol Lett 2017;65(1):12.
- Vianna V, Broderick L, Cowan L. Pressure injury related to friction and shearing forces in older adults. J Dermatol & Skin Sci 2021;3(2):9–12.
- European Pressure Ulcer Advisory Panel, National Pressure Injury Advisory Panel, Pan Pacific Pressure Injury Alliance. Prevention and treatment of pressure ulcers/injuries: clinical practice guideline. The International Guideline. Emily Heasler, editor. EPUAP/NPIAP/PPPIA 2019.
- Mimura M, Okazaki H, Kajiwara T, et al. Variation of body pressure and shear force during bed manipulation (Part 1): effect of body shape and bed manipulation. J Jap Soc Bedsores 2007;9:11–20 (in Japanese).
- Ishikawa H, Hata M, Kondo Y. The effect of back-pulling during head-up and head-down. Asahikawa Red Cross Hosp Med J 2011;31–33 (in Japanese).
- Mori M, Endo A, Oshimoto Y. Fabrication of a cushion to reduce pressure on the buttocks during back elevation and a study of its effectiveness. J Jap Soc Bedsores 2010;12:509–12 (in Japanese).
- Y, Otsuka N, Ibe F, et al. Relationship of 45˚ head-side up and knee elevation and local pressure at the sacral region. Jap J PU 2009;11(1):40–6.
- Harada C, Shigematsu T, Hagisawa S. The effect of 10-degree leg elevation and 30-degree head elevation on body displacement and sacral interface pressures over a 2-hour period. J WOCN 2002:29(3):143–48.
- Lippoldt J, Pernicka E, Staudinger T. Interface pressure at different degrees of backrest elevation with various type of pressure-redistribution surfaces. Am J Crit Care 2014;23(2):119–26.
- Defloor T. The effect of position and mattress on interface pressure. Appl Nurs Res 2000;13(1):2–11.
- Anderwee K, Clark M, Dealey C, et al. Pressure ulcer prevalence in Europe: a pilot study. J Eval Clin Pract 2007;13(2):227–35.
- VanGilder C, Macfarlane GD, Meyer S. Results of nine international pressure ulcer prevalence surveys: 1989 to 2005. Ostomy Wound Manage 2008;54(2):40–54.
- VanGilder C, Amlung S, Harrison P, Meyer S. Results of the 2008–2009 International Pressure Ulcer Prevalence Survey and a 3-year, acute care, unit specific analysis. Ostomy Wound Manage 2009;55(11):39–45.
- VanGilder C, Lachenbruch C, Algrim-Boyle C, Meyer S. The International Pressure Ulcer Prevalence Survey 2006–2015: a 10-year pressure injury prevalence and demographic trend analysis by care setting. J WOCN 2017;44(1):20–8.
- Gefen A. Why is the heel particularly vulnerable to pressure ulcers? Br J Nurs 2017;26(Sup20):S62–S74.
- Nakagami G, Sanada H, Konya C, et al. Comparison of two pressure ulcer preventive dressings for reducing shear force on the heel. J WOCN 2006;33(3):267–72.
- Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 2007;39:175–91.
- Okubo Y, Kohase M, Ogawa KI. Influence of raising and lowering the back of the bed on the body. J Jap Soc Bedsores 2000;2:45–50 (in Japanese).
- Grey JE, Harding KG, Enoch S. Pressure ulcers. BMJ 2006;332:472–75.
- Okuwa M, Sugama J, Sanada H, et al. Measuring the pressure applied to the skin surrounding pressure ulcers while patients are nursed in the 30 degree Position. J Tissue Viab 2005;15(1):3–8.
- The Japanese Society of Pressure Ulcers Guideline Revision Committee. JSPU guidelines for the prevention and management of pressure ulcers (4th ed.). Jpn J PU 2015;17(4):487–557.
- McCreath HE, Bates-Jensen BM, Nakagami G, et al. Use of Munsell Color Charts to objectively measure skin color in nursing home residents at risk for pressure ulcer development. J Adv Nurs 2016;72(9):2077–85.
- Gefen A. Tissue changes in patients following spinal cord injury and implications for wheelchair cushions and tissue loading: a literature review. Ostomy Wound Manage 2014;60(2):34–45.
- Takahashi M, Shimomichi M, Ohura T. Effects of pressure and shear force on blood flow in the radial artery and skin capillaries. J Jap Soc Bedsores 2012;14:547–52 (in Japanese).
- Takeda T. An experimental study on the effects of friction and displacement on the occurrence of bedsore. J Jap Soc Bedsores 2001;3:38–43 (in Japanese).
- Santamaria N, Gerdtz M, Sage S, et al. A randomised controlled trial of the effectiveness of soft silicone multi-layered foam dressings in the prevention of sacral and heel pressure ulcers in trauma and critically ill patients: the border trial. Int Wound J 2013;12(3):302–8.
- Ferrer Solà M, Espaulella Panicot J, Altimires Roset J, et al. Comparison of efficacy of heel ulcer prevention between classic padded bandage and polyurethane heel in a medium-stay hospital: randomized controlled trial. Rev Esp Geriatr Gerontol 2013;48(1):3–8.
- Takeshi K, Yoshiki M, Makoto K. Clinical significance of the water retention and barrier function: improving capabilities of ceramide-containing formulations: a qualitative review. J Dermatol 2021;48(12):1807–16.
- European Pressure Ulcer Advisory Panel, National Pressure Ulcer Advisory Panel, Pan Pacific Pressure Injury Alliance. Prevention and treatment of pressure ulcers: quick reference guide. Available from: http://tinyurl.com/yck2mmr6
- Moore Z, Cowman S, Conroy RM. A randomized controlled clinical trial of repositioning, using the 30˚ tilt, for the prevention of pressure ulcers. J Clin Nurs 2011;20(17–18):2633–44.
- Brown MM, Boosinger J, Black J, et al. Nursing innovation for prevention of decubitus ulcers in long term care facilities. Plast Surg Nurs 1985;5:57–64.
- Smith AM, Malone JA. Preventing pressure ulcers in institutionalized elders: assessing the effects of small, unscheduled shifts in body position. Decubitus 1990;3:20–4.
- Dai M, Yamanaka T, Matsumoto M, et al. Effectiveness of the air mattress with small change system on pressure ulcer prevention: a pilot study in a long-term care facility. J Jap WOCM 2018;22(4):357–62.
- Nagase T, Koshima I, Maekawa T, et al. Ultrasonographic evaluation of an unusual peri-anal induration: a possible case of deep tissue injury. J Wound Care 2007;16(8):365–7.


