Volume 43 Number 1
Clinical preventive-based best practices to reduce the risk of peristomal skin complications – an international consensus report
Gillian Down, Kimberly Bain, Birgitte Dissing Andersen, Lina Martins, Tonny Karlsmark, Gregor Jemec, Mark Bain, Lene Feldskov Nielsen, Cecilie Jaeger Leidesdorff Bechshoeft and Anne Steen Hansen
Keywords peristomal skin complications, risk factors, leakage, moisture-associated skin damage, patient quality of life
For referencing Down G et al. Clinical preventive-based best practices to reduce the risk of peristomal skin complications – an international consensus report. WCET® Journal 2023;43(1):11-19
DOI
https://doi.org/10.33235/wcet.43.1.11-19
Submitted 2 September 2022
Accepted Accepted 31 October 2022
Abstract
Evidence indicates that peristomal skin complications (PSC) are a common problem for people with an ostomy and have serious implications on their overall health and quality of life. While there is evidence and documentation on the cause and effect of PSC, there is little written on the risk factors or on how to maintain peristomal skin integrity and prevent PSC. To address this gap, a panel of ostomy experts was convened to conduct a process to reach an international consensus on PSC risk factors. A large-scale modified Delphi consensus-building process was conducted between September 2019 and October 2020. A total of 4,285 online survey responses were received from 36 countries across six continents. The result was a consensus focused on the prevention of PSC and on the individual patient risk factors healthcare providers should consider when determining the best pouching system and care plan for ostomy patients. The consensus supported the development of a PSC risk factor model. The model was subsequently ratified in October 2020. The purpose of the model is to help guide healthcare providers in assessing the risk factors for developing a PSC for each patient and ultimately guide healthcare providers to prevent skin damage, maintain healthy peristomal skin, and support the overall health, wellbeing and quality of life of ostomy patients.
Introduction
It is reported that over 700,000 people are living with a stoma in Europe1, over 1 million in the United States2 and close to 1 million in China3. The literature suggests that up to 80% of stoma patients experience peristomal skin complications (PSC)4–8. PSC negatively affect the quality of life of people with an ostomy9–11. Claessens et al12 reported that 91% of people with an ostomy surveyed said they worry about leakage, 40% said they wake up at night because of their ostomy, 33% said that they limit their physical and social activities and 12% indicated that they socially isolate. However, while the literature supports a direct correlation between quality of life and PSC, understanding the risks to peristomal skin health are not well documented13.
The peristomal skin, the skin area in circumference around the stoma, plays an important role in the effective functioning of the ostomy pouching system. The peristomal skin provides the surface that the pouching system adheres to, and therefore healthy peristomal skin plays a critical role in the effective functioning of the pouching system14. The main role of the pouching system is to collect effluent that is diverted through the patient’s stoma. Effluent typically contains faecal matter, urine and mucous which is corrosive and can cause damage to skin within a short period of time15–18. This damage is often referred to as irritant contact dermatitis in the peristomal area or peristomal contact dermatitis19. Peristomal contact dermatitis can present as erosion of the peristomal skin, red, painful, itchy skin, rash, inflammation and infection. The most effective way to prevent irritant contact dermatitis is to ensure a consistent secure seal, thus preventing leakage of stoma output onto the surrounding skin20,21.
PSC are well documented as the most prevalent complication faced by people with an ostomy and the most common reason people with an ostomy seek outpatient care and specialised ostomy nursing services22. However, there is minimal evidence in the literature to help healthcare professionals to engage in early identification of the risk factors for ostomy patients in developing PSC13. This project was designed to reach consensus among both clinical experts in ostomy care and nurses and practitioners around the world working with ostomy patients regarding risk factors that may cause PSC. The purpose of reaching consensus on risk factors for PSC is to support prevention-based decision-making in ostomy care and improve peristomal skin care practices. This article will describe the process used to reach consensus on the risk factors and the results agreed to by the experts in the study.
Methods
Consensus building is the process of helping groups reach a common understanding on an issue or solution23. The concept of consensus building is based on the belief that when people think together, they can make better decisions24,25. This consensus process was informed by a systematic review of the literature on PSC risk factors and a series of consensus dialogues involving over 400 stoma nurses from across Europe and North America. This methodology ensured the model was based on literature evidence, provided by the literature review and on experiential evidence, provided through dialogues with over 400 stoma nurses and from the survey results from the modified Delphi process (Figure 1).
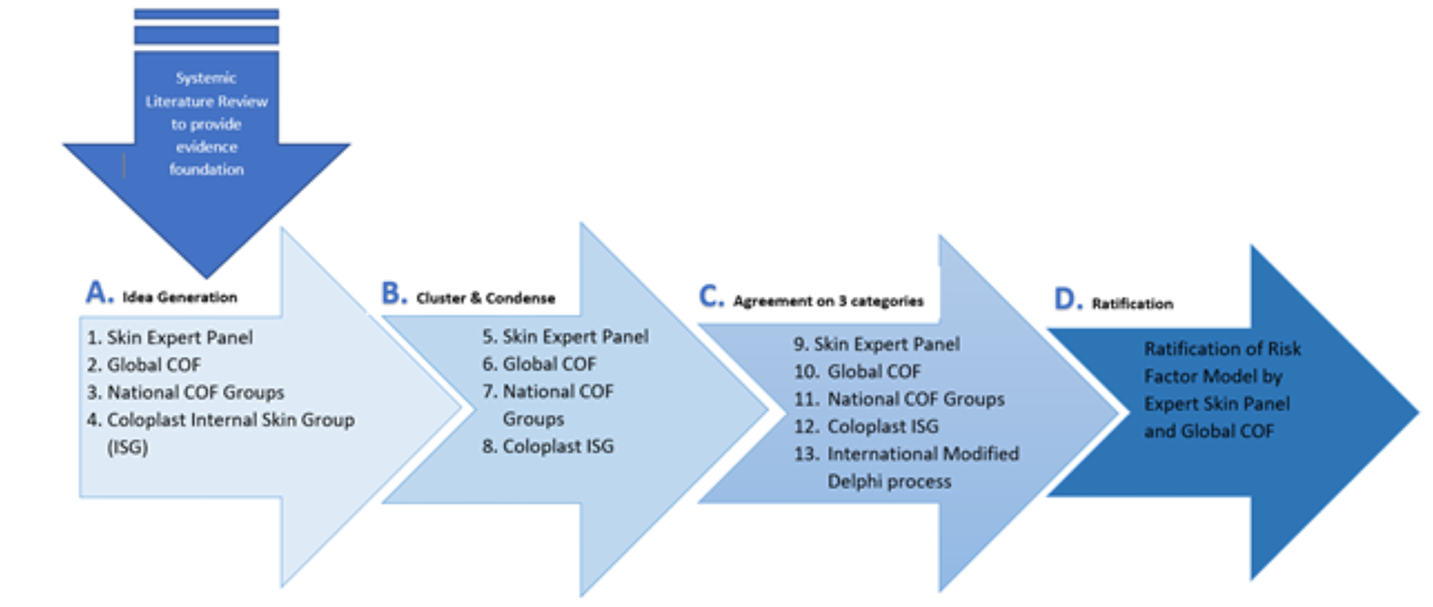
Figure 1. Method for development of the risk factor model, using both literature evidence and experiential evidence.
A. Idea generation and risk factor identification. B. Condensation of risk factors into 10 overall categories. C. Condensation of risk factors into three categories and international modified Delphi process. D. Ratification of the model. COF: Coloplast Ostomy Forum & Expert Panel
An expert panel of 15 dermatologists and ostomy care nurse specialists from eight countries provided stewardship for the project: Birgitte Dissing Andersen (Denmark); Janice Colwell (USA); Gill Down (UK); Tracy Virgin-Elliston (UK); Jane Fellow (USA); Louise Forest-Lalande (Canada); Gregor Jemec (Denmark); Tonny Karlsmark (Denmark); Doris Kost (Germany); Lina Martins (Canada); Svatava Nováková (Czech Republic); Rosalind Probert (Australia); Oirda Samai (France); Emilie Trividic (France); Chantal Tielemans (Belgium). Coloplast A/S funded the project. A modified Delphi process was utilised to help develop the consensus which led to ratification of the model and included elements of Delphi survey methodology, nominal group techniques (NGT-R) and process facilitation26–28.
Two surveys were sent out to ostomy healthcare providers around the world. The first survey was sent out November 2019 and remained open for 30 days. The survey invitation was emailed to healthcare professionals in 17 different languages, across 36 countries, spanning six continents, through industry and professional association mailing lists. The survey was anonymous and was conducted virtually. A total of 2262 responses were received. The first survey was designed to identify current practices, tools and methodologies, and to explore respondents’ views on risk factors for PSC, as well as identify the strategies used to prevent and treat PSC. The results of the survey were analysed by the expert panel and assessed against the literature review findings.
The second survey opened in late January 2020. Survey invitations were emailed to the same invitees as the first survey, this time in 16 languages (the second survey was not sent out in Italian as Italy was under lockdown due to COVID-19 at the time) and across 35 countries. The second survey was designed to confirm the risk factors identified in the first survey and the literature findings, the results of which were again reviewed by the expert panel. Due to the COVID-19 global pandemic, the second survey remained open for 90 days, in recognition that healthcare professionals’ time was focused on pandemic response not responding to research surveys. A total of 2023 responses were received within the 90 days and again the results were analysed and discussed at the expert panel.
The data collected from surveys 1 and 2 were used to develop a third survey which was sent to the expert panel (n=15). The expert panel members ratified the list of risk factors based on the results of the literature review, the two global surveys, and in person (September 2019) and virtually (throughout 2020) facilitated dialogues.
Participants
The first survey was responded to by 2262 healthcare professionals. The response breakdown by region can be seen in Figure 2. The majority, 79%, of respondents were specialised ostomy nurses, 15% were ward or outpatient nurses, 4% were home care/community health workers; the remaining 2% included physicians, surgeons, dermatologists and healthcare managers. A total of 74% of respondents reported they had more than 10 years’ experience as a healthcare professional.
The second survey received 2023 responses and received more responses from Asia than survey 1, but less from the Middle East and Africa. The expert panel concluded this shift was due to the heavy work/time burden of the pandemic on healthcare professionals in specific regions, vis-à-vis the timing of the survey.
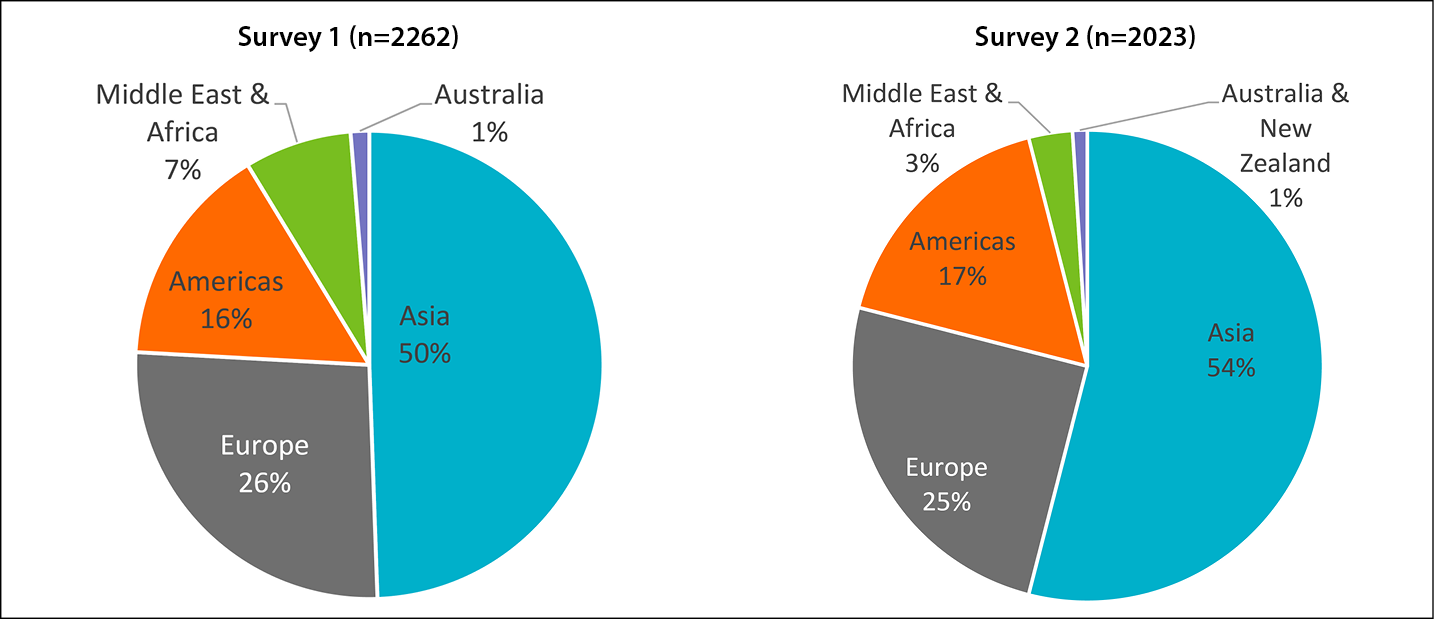
Figure 2. Survey responses by geographic region
Ethical considerations
The project received approval from the Biomedical Research Alliance of New York LLC Organizational Review Board (Study Specific #20180925) without qualifiers. All three surveys were anonymous. Demographic information gathered focused on country of residence, clinical credentials, type of clinical practice, and years of experience. No identifiable personal information was collected. Coloplast A/S funded the study, however, the research questions, project oversight and resulting consensus were the responsibility of the expert panel. Coloplast A/S products were not mentioned in the surveys nor in communication with participants. The resulting PSC risk factor model does not reference or recommend any products and focuses solely on the identification of risk factors for preventing PSC.
Data management and analysis
Survey data was comprised of a total of 4285 anonymous survey responses and was analysed using descriptive statistics utilising Excel Pivot Tables (Excel 365 v 2109). All data was analysed and reported in aggregate and by basic demographic data – type of respondent (nurse, physician, etc) and location of practice (region or country). Data were analysed using descriptive statistics using mean, median, mode and standard deviation, as well as comparative analysis between regions and between professional groups. Significance was defined as p<0.050.
Results
The results clearly indicate that survey respondents believe it is important to maintain peristomal skin integrity for positive patient outcomes. A total of 93% of respondents agreed that peristomal skin health is very important to patient overall health and wellbeing; 99% of respondents agreed that preventing PSC should be the aim of healthcare providers and 97% agreed that PSC risk factors should always be considered when determining the most effective pouching system for a patient. However, when asked to estimate the percentage of their patients who experienced PSC in the last 6 months, the average response was 42%, with a standard deviation of +22.47% (Table 1). The high degree of variability in responses (+22.47%) was consistent across all regions (Table 2). There were no significant statistical differences between responses from experienced healthcare professionals and respondents with less than 5 years of healthcare experience. The results indicate that neither geography nor experience of the healthcare provider impacts the probability of a patient experiencing PSC.
Table 1. Percentage of their ostomy patients that experienced PSC in the last 6 months, as reported by survey respondents
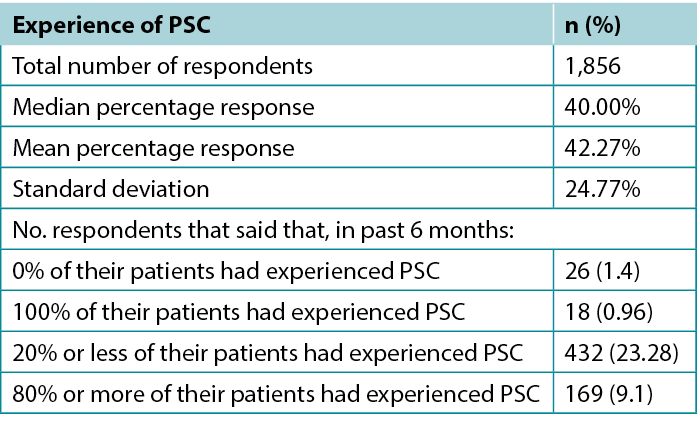
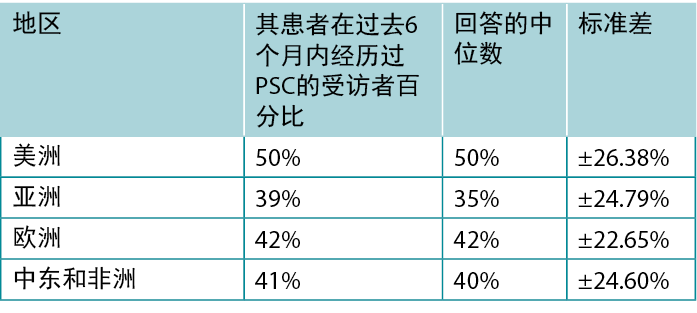
Table 2. Percentage of patients who experienced PSC in the last 6 months by region
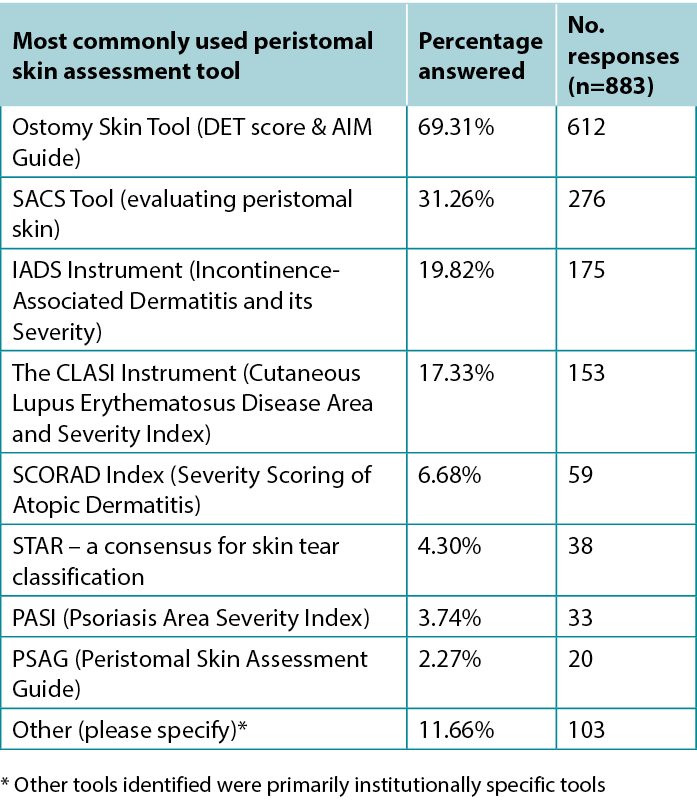
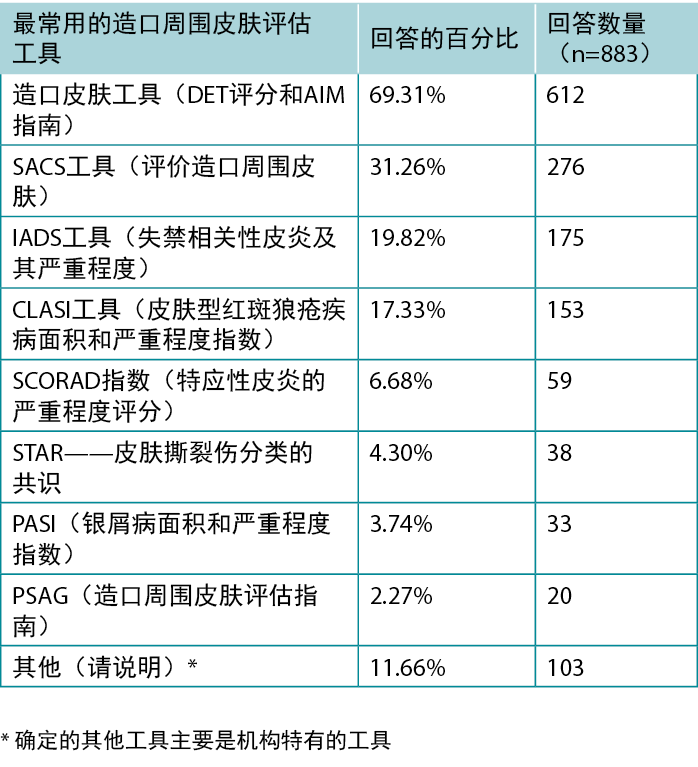
When asked about peristomal skin health, 85% of respondents agreed that it is a realistic goal for peristomal skin to look and feel exactly like skin outside the peristomal area, with 11% neither agreeing nor disagreeing and only 4% disagreeing. However, only 47% (n=883) of respondents reported consistently using a peristomal skin assessment tool in their practice. Of the tools identified, the most frequently used tool was the ostomy skin tool that uses DET scores (Table 3)29.
Table 3. Most commonly used peristomal skin assessment tool
The main health indicators observed in patients with PSC were identified, in descending order, as (Figure 3):
- Moisture-associated skin damage (MASD).
- Contact dermatitis.
- Mucocutaneous separation.
- Bacterial, fungal or yeast infections.
- Skin stripping.
- Medical adhesive-related skin injuries (MARSI).
- Suture granulomas.
- Hyperplasia/tissue overgrowth.
- Folliculitis.
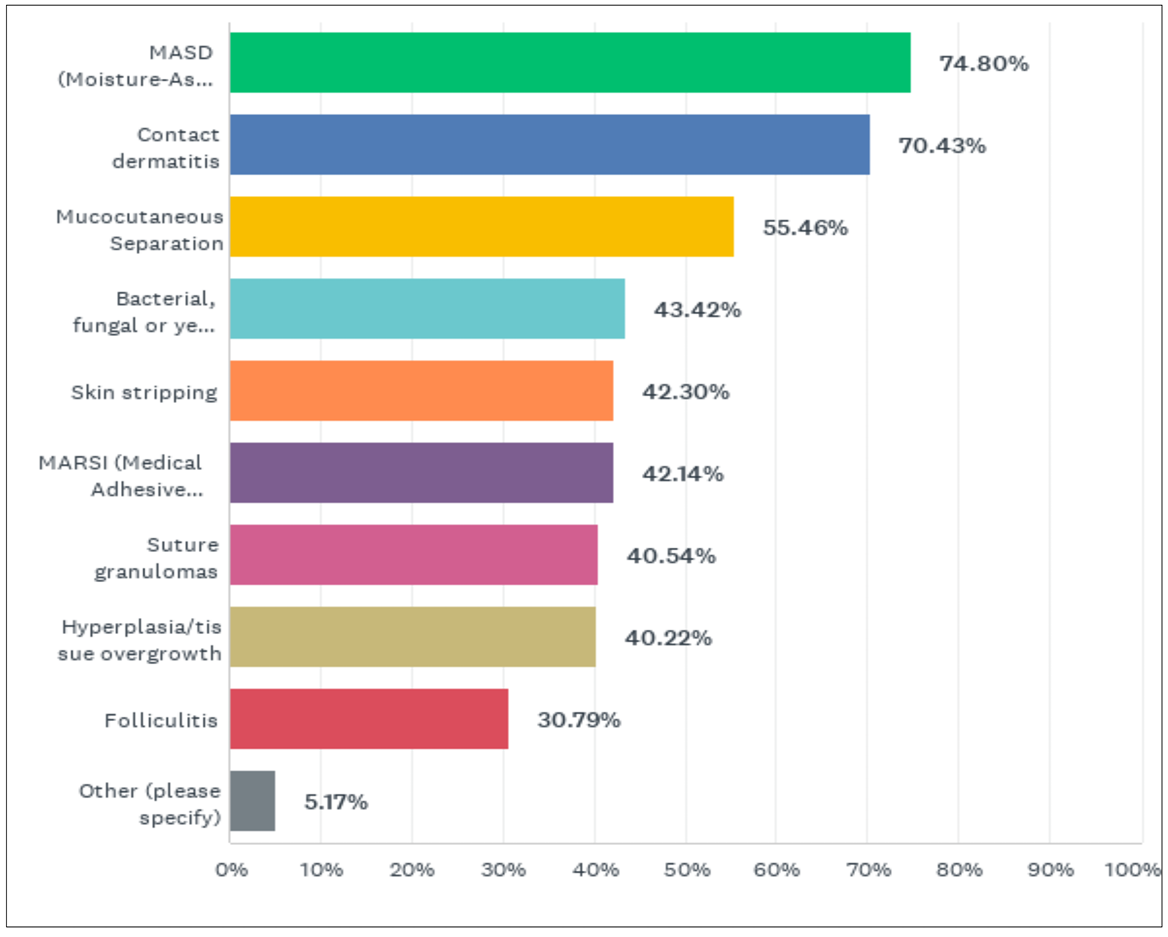
Figure 3. What have you observed are the main health indications of PSC in your patients? (answered by 1877 survey respondents)
The main effects of PSC on patients’ quality of life were: increased worry about leakage, identified by 90% of respondents; decreased social activities/social isolation, identified by 88% of respondents; decreased confidence in the pouching system by patients, identified by 82% of respondents; increased pain and itching, also identified by 82% of respondents; decreased feelings of security and confidence, identified by 77% of respondents; negative affect on sleep patterns, identified by 76% of respondents; and decreased productivity of patient, identified by 60% of respondents.
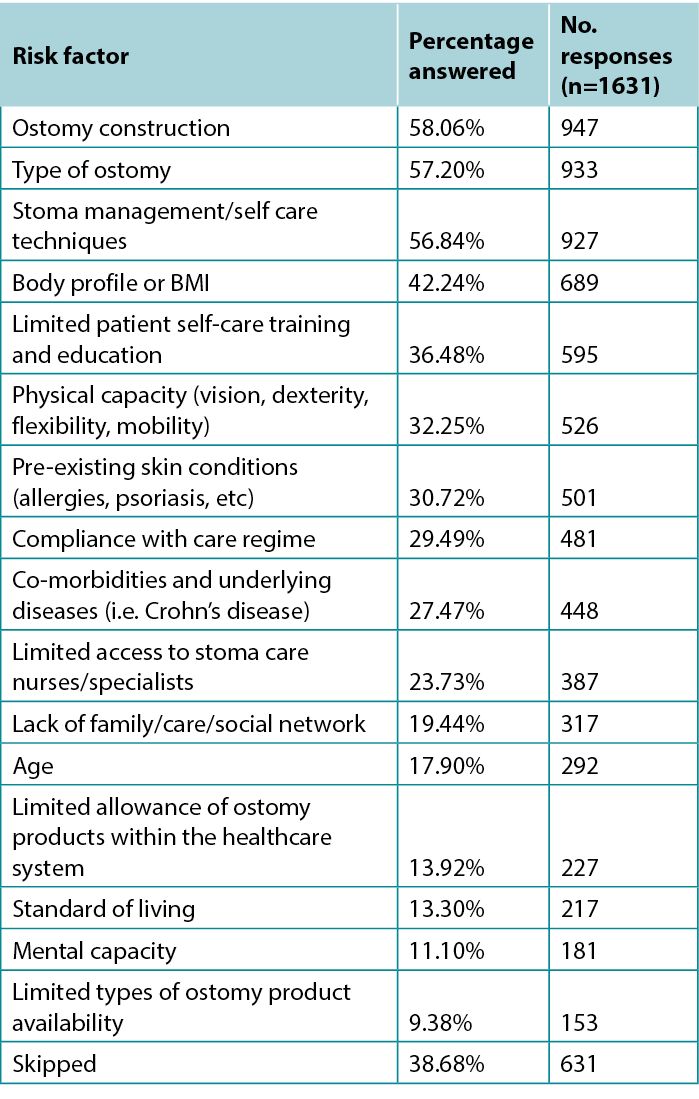
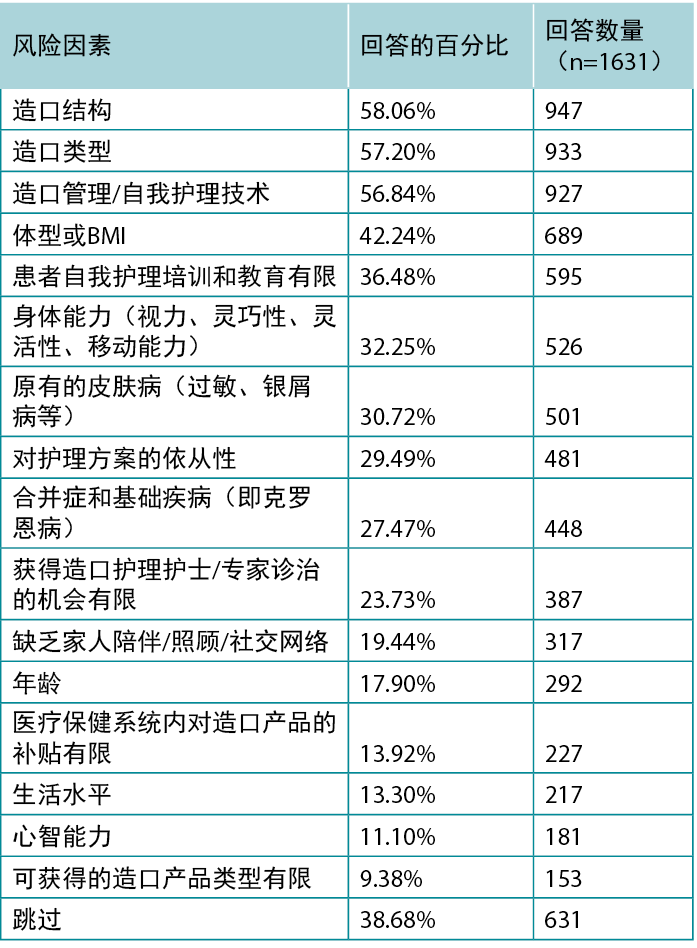
The most often identified risks, for patients developing PSC, are presented below in descending order, starting with those factors most often identified by respondents (Table 4):
- Ostomy construction.
- Type of ostomy.
- Stoma management/self care techniques.
- Body profile/BMI.
- Limited patient self-care training and education.
- Physical capacity (vision, dexterity, flexibility, mobility).
- Pre-existing skin conditions (allergies, psoriasis, etc).
- Compliance with care regime.
- Co-morbidities and underlying diseases (i.e., Crohn’s disease).
- Limited access to stoma care nurses/specialists.
- Lack of family/care/social network.
- Age.
- Limited allowance of ostomy products within the healthcare system.
- Standard of living.
- Mental capacity.
- Limited types of ostomy product availability.
Table 4. Main risk factors identified by respondents for developing PSC
Respondents identified the following as the most common reasons patients develop PSC (Figure 4):
- Leakage of stoma effluent (poor pouching seal).
- Scars, creases and folds in the peristomal skin.
- Ostomy construction/height & location.
- Not dealing with minor skin irritations in a timely fashion, allowing the condition to worsen.
- Patient compliance with care regime, including proper cleaning of peristomal skin.
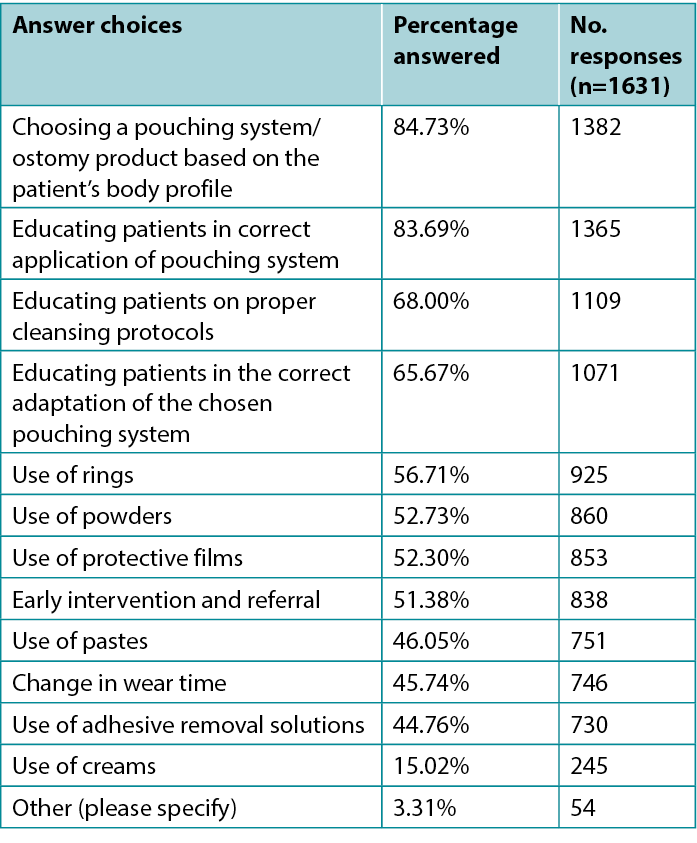
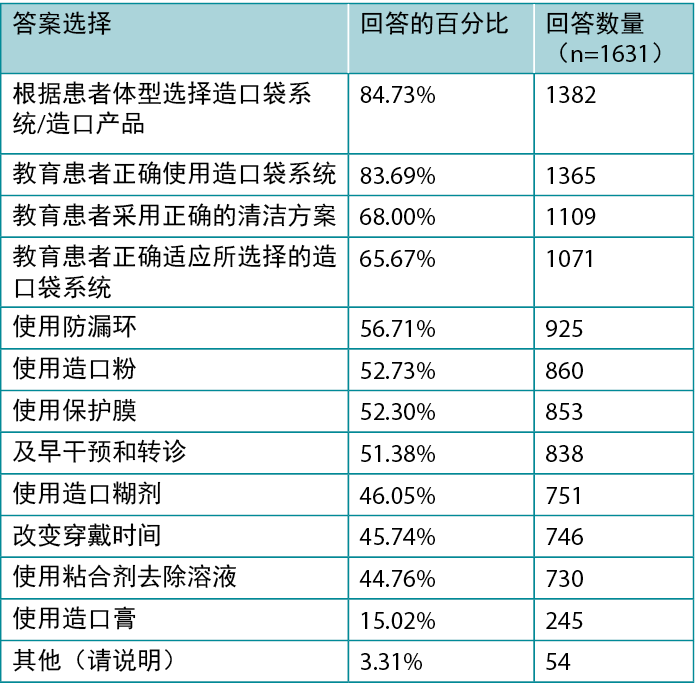
When asked to identify the main prevention strategies they currently use to maintain optimal peristomal skin health, respondents indicated choosing a pouching system based on the patient’s body profile and patient education as the top two strategies (Table 5).
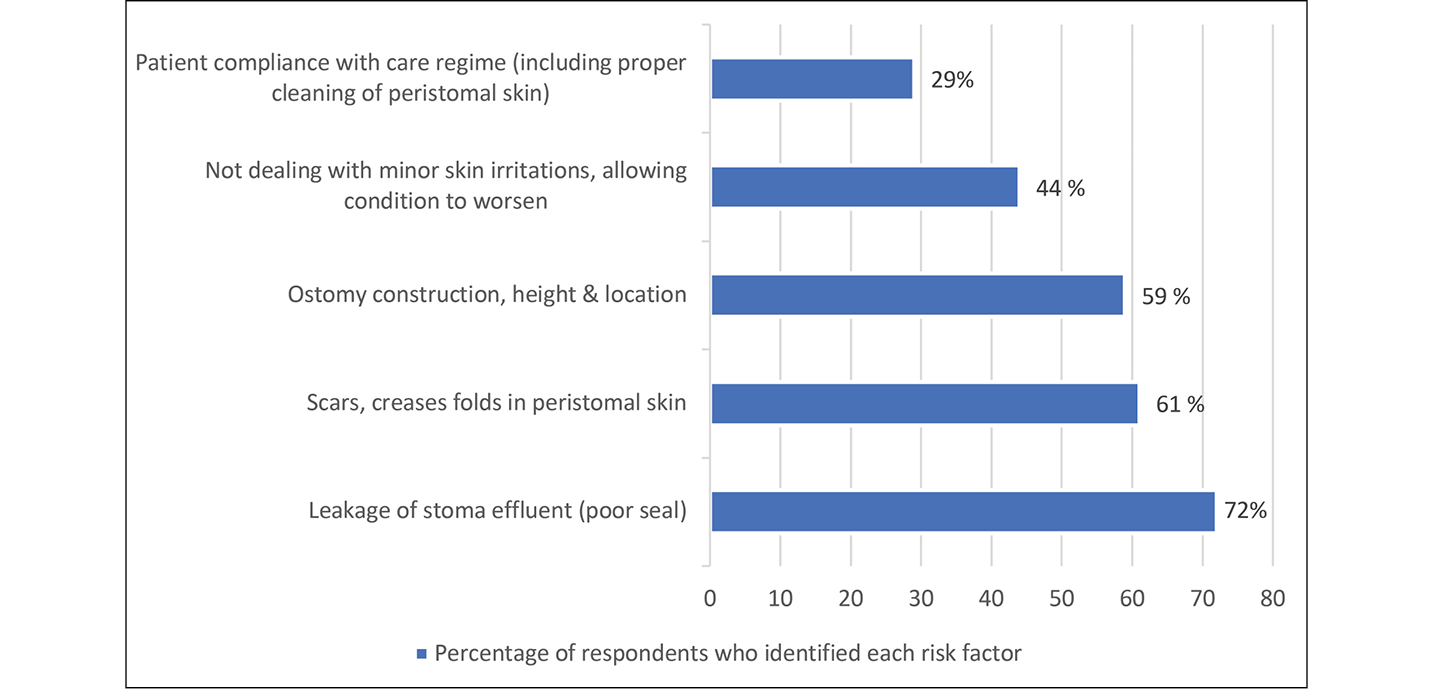
Figure 4. Five most common risk factors leading to PSC in respondents’ patient population
Table 5. Main prevention strategies respondents reported using to maintain optimal peristomal skin health
Respondents were also asked about their healthcare systems. To determine the effects of delivery and affordability of care, respondents were asked how often the issue of cost influences decision-making when determining the best pouching system for patients. The responses varied across regions but not across system types (i.e., public- vs private-based systems). Respondents from Asia, USA and Canada tend to take costs into consideration more often, while respondents from Europe, the Middle East and Africa do not consider costs as often (Figure 5). When asked about post-discharge programs for people who go through stoma surgery, overall, only 56% of respondents indicated that all of their ostomy patients have access to post-discharge programs, with the Americas being the lowest at 43% and Europe being highest at 72%. The length of post-discharge programs also varied greatly across regions, with Europe being the longest, 51% reporting their post-discharge programs are longer than 12 months; in the Americas, 55% reported their post-discharge programs are 2 months or less.
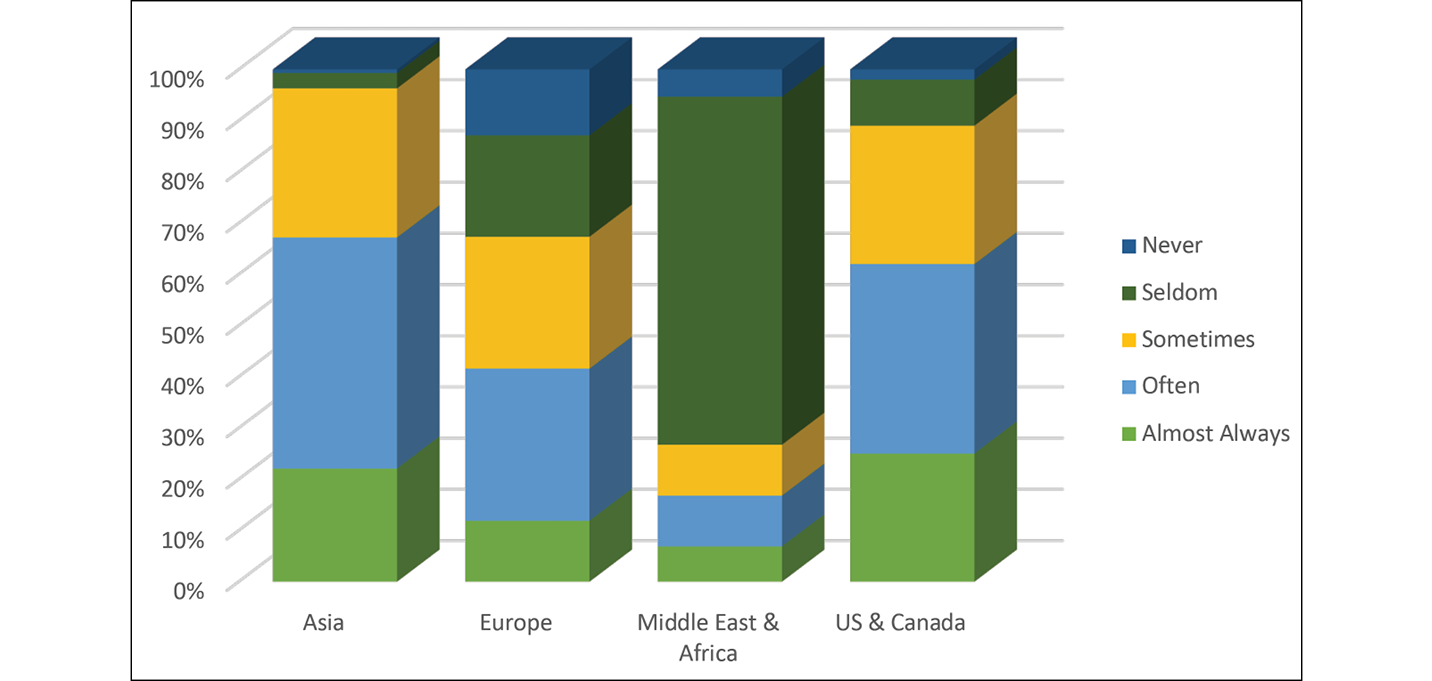
Figure 5. How often the issue of costs influences decision-making when determining the best pouching system for patients, reported by region
The survey results also offer insights on respondents’ experience regarding ostomy pouching systems. A total of 97% of respondents indicated that it is important or very important to have a range of products available to meet individual ostomate needs and enable adaption to each individual patient’s body profile. Overall, 99% of respondents indicated that product considerations were important in assessing a patient’s risk of developing PSC. Finally, respondents identified those considerations seen as most important regarding the adhesive properties of products in the prevention of PSC, in order of prevalence:
- The ease of application and removal.
- The ability to follow body movements.
- The erosion resistance of adhesive.
- The need to add accessories to aid in the product effectiveness.
- The potential for skin stripping.
- The speed with which the product attaches to the skin (immediate adherence to the skin).
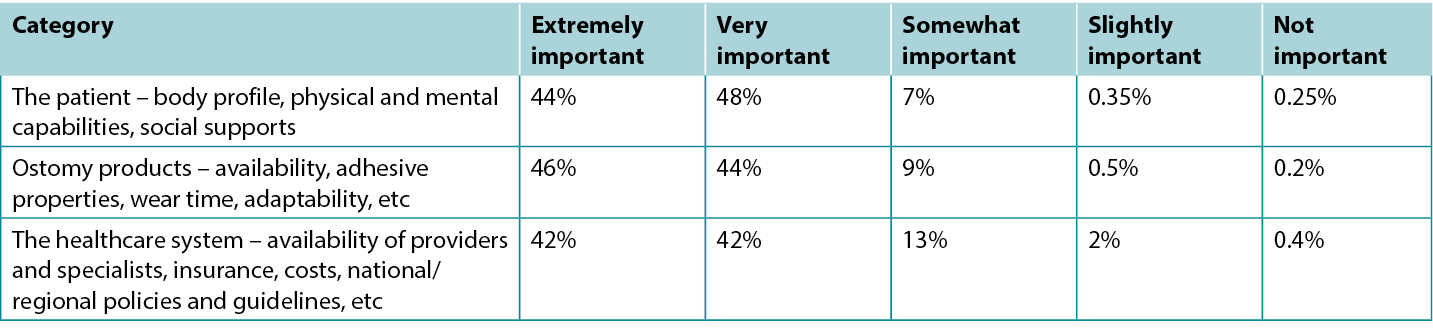
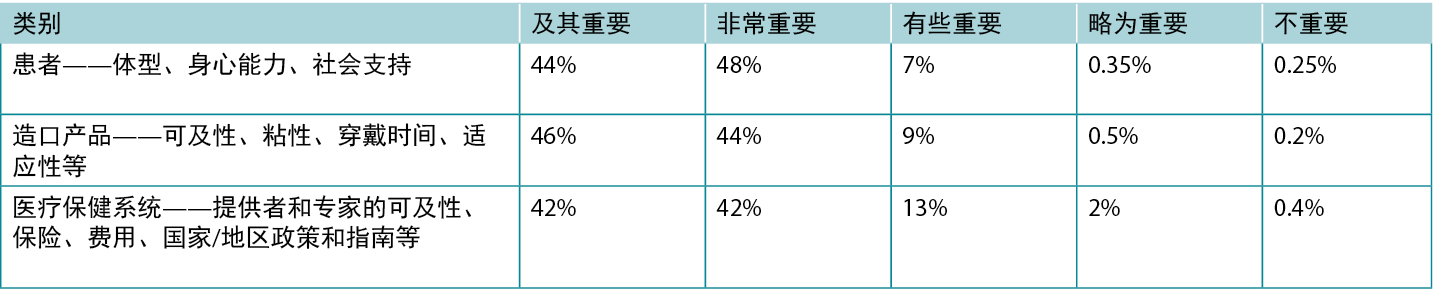
Table 6 indicates the factors that respondents identified as necessary to determine the optimal pouching system for patients. Three risk factor categories were supported by the survey respondents: the patient (body profile, physical and mental capabilities and social supports); ostomy products (availability, wear time, adhesive properties, adaptability, etc); and the healthcare system (costs, availability of healthcare providers and specialists, guidelines and limitations, insurance provisions, etc) (Table 7).
Table 6. Factor respondents always consider when determining the best pouching system for patients
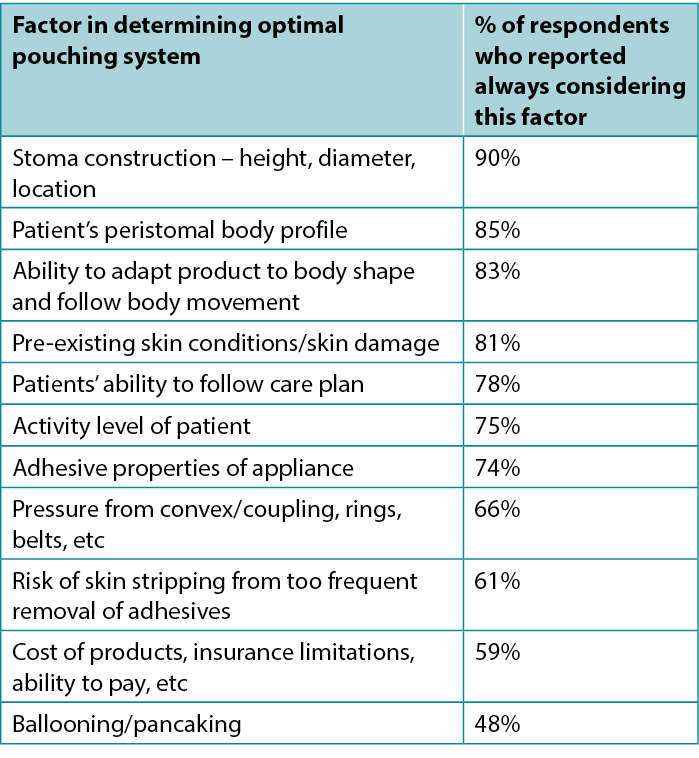
Table 7. Support for risk factor categories, asked in survey 2 (n=2023)
Discussion
The survey results show there is strong clinician support for prevention of PSC among respondents. Reacting once peristomal skin issues arise is difficult because once the peristomal skin is compromised, a secure seal is harder to obtain, resulting in leakage and further deterioration of the peristomal skin5,8,21. When skin integrity around the stoma site is compromised, appliance adherence problems are compounded; therefore, preventing PSC is paramount14,19,22.
Respondents agreed that peristomal skin health is important to people with an ostomy’s overall health, wellbeing and quality of life and that it is a realistic goal for peristomal skin to look and feel like the skin outside of the peristomal area30. To maintain healthy peristomal skin for the life of the person with an ostomy, healthcare providers should identify the risk factors for developing PSC of each patient periodically throughout the patient journey22,29. Identifying the risks will allow healthcare providers, in partnership with patients, to choose the appropriate pouching system and develop the best care plan to mitigate the identified risks and maintain/promote peristomal skin health20.
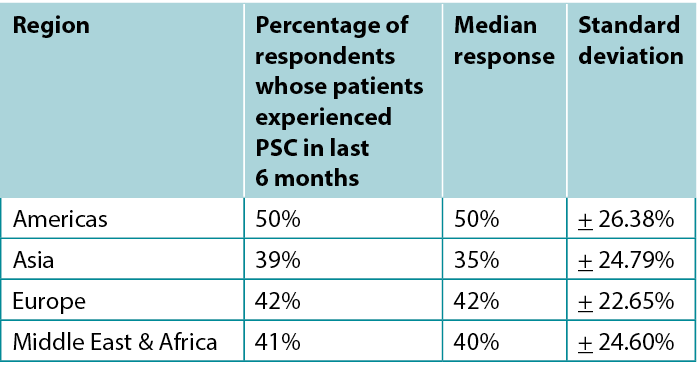
The Modified Delphi Process resulted in a strong consensus around the importance of maintaining peristomal integrity and the risk factors that must be considered in the prevention of PSC. The evidence identified in the literature review13 and the experiential evidence gathered through the surveys and the facilitated dialogues led to the development and ratification of the PSC risk factor model (Figure 6).
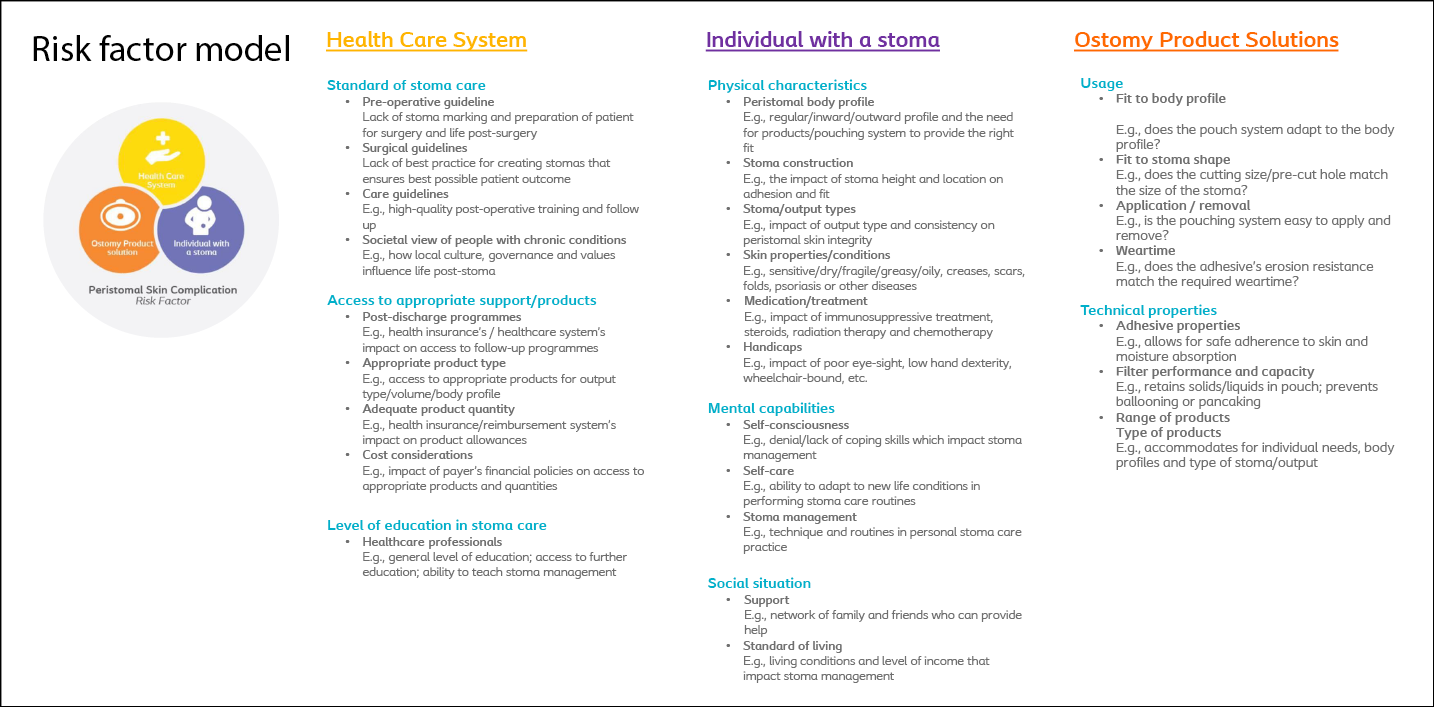
Figure 6. PSC risk factor model13
The model categorises peristomal risk factors into three categories – the individual with a stoma, the ostomy product solutions, and the healthcare system in which the patient lives. Each of these categories encompass a list of risk factors that should be considered by healthcare providers when assessing a patient’s risk of developing PSC. The PSC risk factor model was designed to guide healthcare providers in identifying the risks for each patient so that an individualised care plan can be developed to support the peristomal skin health and overall wellbeing of the ostomate. The international nature of the survey results supports the model as a global framework that can provide an evidence-based foundation for regional decision-making on preventing PSC.
Strengths and limitations
The strength of this project stems from the large number and geographic diversity of the participants. Close to 4,300 survey responses were received from experienced ostomy care providers spread across six continents. The multinational, multicultural and multilinguistic nature of the study makes the model uniquely positioned to allow for regionally appropriate emphasis and implementation variations based on system requirements and patient expectations.
Another strength was the depth and breadth of experience of the expert panel members who acted as stewards for the process. The skin expert panel consisted of highly experienced ostomy nurses and dermatologists who have impressive research resumes and are highly regarded in the field.
A limitation of the study was the inability, due to the anonymity of survey respondents, to know how many of the respondents who responded to the first survey also responded to the second survey. Therefore, the authors are unable to calculate a definitive number of overall participants. Finally, industry sponsorship of this study could lead respondents to bias towards Coloplast A/S products; however, no survey questions, nor any of the communication with respondents, included product names, types or descriptions. Survey respondents were not in any way compensated or incentivised to respond to the surveys. Additionally, respondents were anonymous to both the research team and industry sponsorship partner. It is the opinion of the authors that this decreased bias in the survey results.
Conclusion
Peristomal skin integrity is necessary to obtain a secure seal for an ostomy pouching system. If the ostomy pouching system is not secure, effluent can leak onto the peristomal skin, causing PSC such as skin damage and erosion. Preventing leakage and PSC is paramount to an ostomate’s health and quality of life. This study was designed to identify the risk factors in preventing PSC. The risk factors were categorised under three headings: the individual with a stoma (body profile, capabilities, social situation); the healthcare system (standard of care, access and education); and ostomy products (usage and technical properties). An international consensus was reached on the risk factor model and its importance in focusing on prevention of PSC. Agreement was also achieved in that the goal for all healthcare providers should be to maintain peristomal skin to the same condition/health of skin outside the peristomal area. The resulting PSC risk factor model was unanimously ratified by the expert panel, and they, along with the research authors, advocate its use by healthcare providers as a first line of defence to identify risks and guard against PSC.
Conflict of Interest
The project was supported by Coloplast A/S. G Down, B Andersen, L Martins, T Karlsmark and G Jemec are all members of the Coloplast Skin Expert Panel. K Bain has conducted facilitation contracts for Coloplast A/S in the past. M Bain has provided data analysis services for Coloplast A/S in the past. A Steen Hansen, L Feldskov and C Bechshoeft all work for Coloplast A/S.
Funding
This project was funded by Coloplast A/S.
基于临床预防的降低造口周围皮肤并发症风险的最佳实践——一份国际共识报告
Gillian Down, Kimberly Bain, Birgitte Dissing Andersen, Lina Martins, Tonny Karlsmark, Gregor Jemec, Mark Bain, Lene Feldskov Nielsen, Cecilie Jaeger Leidesdorff Bechshoeft and Anne Steen Hansen
DOI: https://doi.org/10.33235/wcet.43.1.11-19
摘要
证据表明,造口周围皮肤并发症(PSC)是造口患者的常见问题,对他们的整体健康和生活质量都有严重影响。虽然已有关于PSC的因果关系的证据和文献,但关于风险因素或如何保持造口周围皮肤的完整性和预防PSC的内容却很少。为了弥补这一差距,我们召集了一个造口专家小组,通过共识建立过程来达成PSC风险因素的国际共识。在2019年9月至2020年10月期间,开展了大规模的改良徳尔菲法共识建立调查,共收到来自六大洲36个国家的4,285份在线调查回复。结果形成了一项共识,重点是预防PSC以及医疗服务提供者在确定造口患者的最佳造口袋系统和护理计划时应考虑的个体患者风险因素。该共识支持了PSC风险因素模型的开发,随后该模型于2020年10月获得批准。该模型的目的是帮助指导医疗服务提供者评估每位患者发生PSC的风险因素,并最终指导医疗服务提供者预防皮肤损伤,保持造口周围皮肤的健康,并为造口患者的整体健康、幸福和生活质量提供支持。
引言
据报告,欧洲1有70多万造口患者,美国2有100多万,中国3有近100万。文献表明,高达80%的造口患者会出现造口周围皮肤并发症(PSC)4-8。PSC会对造口患者的生活质量产生负面影响9-11。Claessens等人12报告说,接受调查的造口患者中有91%表示他们担心渗漏,40%表示他们因为造口而在夜间醒来,33%表示造口对他们的身体和社会活动造成限制,12%表示他们在社交上被孤立。然而,虽然文献支持生活质量与PSC之间存在直接相关性,但对造口周围皮肤健康风险的理解并没有得到很好的记录13。
造口周围皮肤,即造口周围的皮肤区域,在造口袋系统的有效运作中起着重要作用。造口周围皮肤提供了造口袋系统附着的表面,因此健康的造口周围皮肤在造口袋系统的有效运作中起着关键作用14。造口袋系统的主要作用是收集通过患者造口转移的流出物。流出物通常含有粪便、尿液和粘液,具有腐蚀性,可在短时间内对皮肤造成损
害15-18。这种损害通常被称为造口周围区域的刺激性接触性皮炎或造口周围接触性皮炎19。造口周围接触性皮炎可表现为造口周围皮肤糜烂、皮肤发红、疼痛、发痒、皮疹、炎症和感染。预防刺激性接触性皮炎最有效的方法是始终确保安全密封,从而防止造口输出物渗漏到周围皮肤上20,21。
有资料显示,PSC是造口患者面临的最普遍的并发症,也是造口患者寻求门诊护理和专业造口护理服务的最常见原因22。然而,文献中很少有证据可以帮助医疗保健专业人员及早识别造口患者发生PSC的风险因素13。本项目旨在就可能导致PSC的风险因素在世界各地的造口护理临床专家和从事造口患者工作的护士和从业人员之间达成共识。就PSC的风险因素达成共识的目的是支持以预防为基础的造口护理决策并改善造口周围皮肤护理实践。本文将介绍用于就风险因素达成共识的过程以及研究中专家们同意的结果。
方法
建立共识是帮助团体就某一问题或解决方案达成共识的过程23。建立共识的概念基于这样一种信念:当大家共同思考,就可以做出更好的决定24,25。这一共识过程参考了对PSC风险因素文献的系统综述以及来自欧洲和北美的400多名造口护士参与的一系列共识对话。这种方法确保了该模型以文献综述提供的文献证据和通过与400多名造口护士的对话以及改良徳尔菲法的调查结果提供的经验证据为基础(图1)。
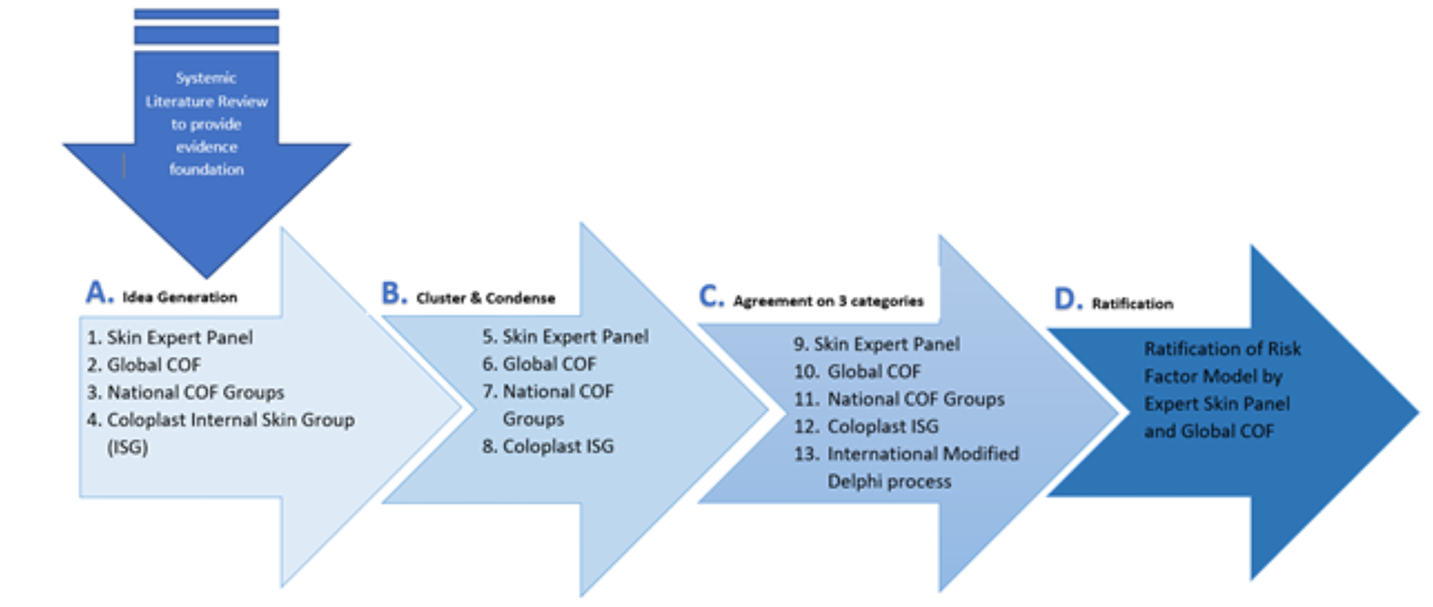
图1.利用文献证据和经验证据开发风险因素模型的方法。
A.想法的产生和风险因素的确定。B.将风险因素浓缩为10个总体类别。C.将风险因素缩减为三类,并在国际上采用改良的徳尔菲法。D.模型的批准。COF:Coloplast造口论坛和专家小组
由来自八个国家的15名皮肤科医生和造口护理护士专家组成的专家小组为该项目提供了指导:Birgitte Dissing Andersen(丹麦);Janice Colwell(美国);
Gill Down(英国);Tracy Virgin-Elliston(英国);
Jane Fellow(美国);Louise Forest-Lalande(加拿大);Gregor Jemec(丹麦);Tonny Karlsmark
(丹麦);Doris Kost(徳国);Lina Martins(加拿大);Svatava Nováková(捷克共和国);Rosalind Probert(澳大利亚);Oirda Samai(法国);Emilie Trividic(法国);Chantal Tielemans(比利时)。
Coloplast A/S资助了该项目。采用改良的徳尔菲法帮助形成共识,从而使模型得到批准,该方法包括徳尔菲调查方法、名义小组法(NGT-R)和过程促进等要素26-28。
我们向世界各地的造口医疗服务提供者发送了两项调查。第一次调查于2019年11月发出,开放了30天。调查邀请函通过行业和专业协会的邮件列表以17种不同的语言发送至横跨六大洲36个国家的医疗保健专业人员。该调查是匿名的,并且是以虚拟方式进行的。共收到2262份回复。第一次调查旨在确定目前的做法、工具和方法,并探讨受访者对PSC风险因素的看法,以及确定用于预防和治疗PSC的策略。专家小组对调查结果进行了分析,并根据文献综述结果进行了评估。
第二次调查于2020年1月下旬开始。调查邀请函通过电子邮件发给了与第一次调查相同的受邀者,这次用了16种语言(第二次调查没有用意大利语发送,因为当时意大利因COVID-19疫情而处于封锁状态),覆盖35个国家和地区。第二次调查的目的是确认第一次调查中确定的风险因素和文献综述的结论,其结果再次由专家小组审查。由于COVID-19的全球大流行,第二次调查开放了90天,因为认识到医疗保健专业人员的时间都重点放在抗击疫情上,而不是回复研究调查。在90天内共收到2023份回复,专家小组再次对结果进行了分析和讨论。
从调查1和2中收集的数据用于制定第三次调查,并发送给专家小组(n=15)。专家小组成员根据文献综述、两次全球调查以及线下(2019年9月)和线上(2020年全年)促进对话的结果,批准了风险因素列表。
参与者
第一次调查得到了2262名医疗保健专业人员的回复。图2显示了按地区对回复进行的细分。大部分受访者(79%)是专业造口护士,15%是病房或门诊护士,4%是家庭护理/社区卫生工作者;其余2%包括内科医生、外科医生、皮肤科医生和医疗保健管理人员。共有74%的受访者表示他们拥有超过10年的医疗保健专业经验。
第二次调查收到了2023份回复,相较于调查1,来自亚洲的回复数量増多,但来自中东和非洲的回复有所减少。专家小组得出的结论是,这种转变是由于相对于调查的时间而言,疫情给特定地区的医疗保健专业人员带来了沉重的工作/时间负担。
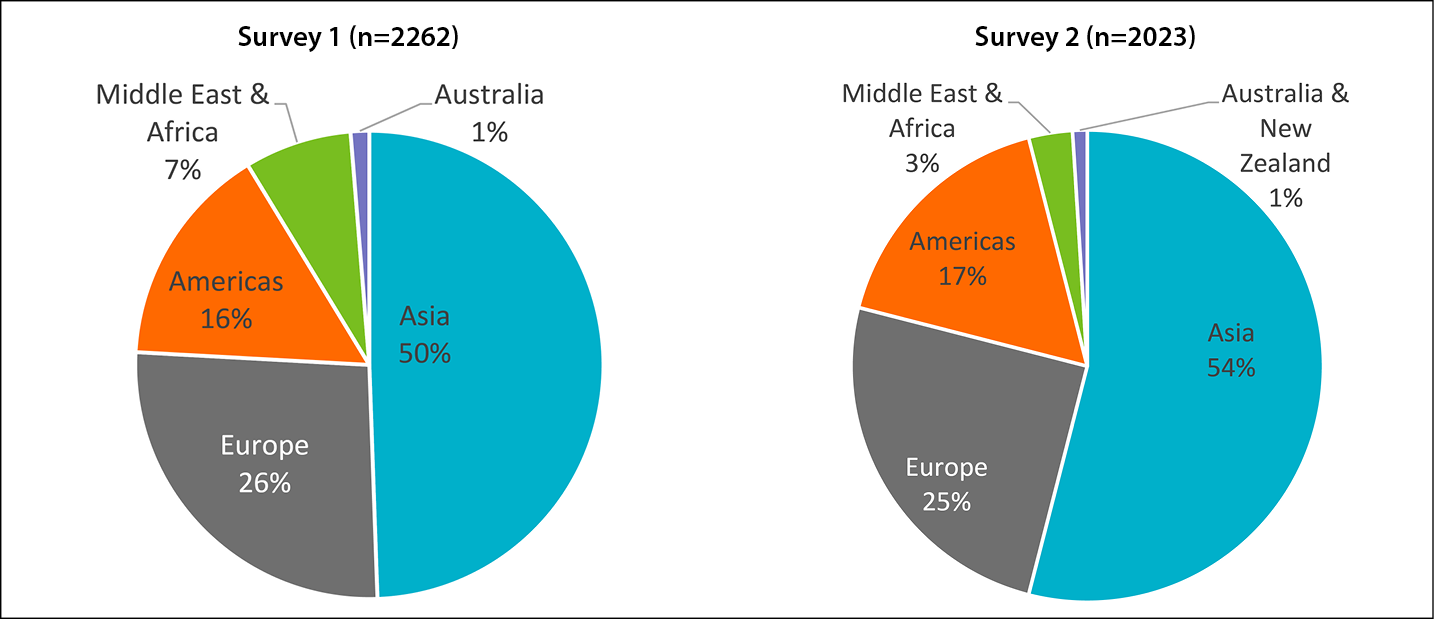
图2.按地理区域划分的调查回复
伦理事宜
项目获得了纽约生物医学研究联盟有限责任公司组织审查委员会的批准(特定研究编号20180925),无限定条件。三次调查均匿名进行。收集的人口统计信息主要集中在居住国、临床证书、临床实践类型和经验年限。未收集可识别的个人信息。Coloplast A/S资助了这项研究,然而,研究问题、项目监督和由此产生的共识是由专家小组负责。在调查中以及与参与者的交流中均未提及Coloplast A/S的产品。由此建立的PSC风险因素模型不参考或推荐任何产品,仅侧重于识别预防PSC的风险因素。
数据管理和分析
调查数据由总计4285份匿名调查回复组成,使用Excel数据透视表(Excel 365,版本2109)进行描述性统计分析。所有数据均按基本人口统计数据Å\Å\受访者类型(护士、医生等)和执业地点(地区或国家)进行汇总分析和报告。采用平均值、中位数、众数和标准差等描述性统计对数据进行分析,并进行地区之间和专业组之间的比较分析。P<0.050时视为具有统计学显著性。
结果
结果清楚地表明,调查受访者认为保持造口周围皮肤的完整性对获得积极的患者治疗效果非常重要。共有93%的受访者同意造口周围皮肤健康对患者的整体健康和幸福非常重要;99%的受访者同意预防PSC应该是医疗服务提供者的目标,97%的受访者同意在为患者确定最有效的造口袋系统时,应始终考虑PSC风险因素。然而,当被要求估计过去6个月内经历过PSC的患者百分比时,平均回答为42%,标准差为Å}22.47%(表1)。回答的高度差异性(Å}22.47%)在所有地区均一致(表2)。经验丰富的医疗保健专业人员的回答与医疗保健经验不足5年的受访者之间没有显著的统计差异。结果表明,无论是地理位置还是医疗服务提供者的经验,均不会影响患者发生PSC的可能性。
表1.根据调查受访者的报告,他们的造口患者在过去6个月内经历过PSC的百分比
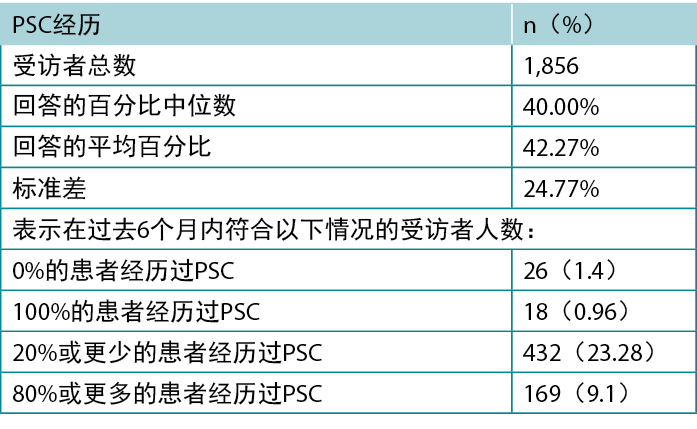
表2.按地区划分的过去6个月内经历过PSC的患者百分比
当被问及造口周围皮肤健康情况时,85%的受访者同意,使造口周围皮肤看起来和感觉起来与造口周围区域外的皮肤完全一致是一个现实的目标,11%的受访者既不同意也不反对,仅4%的受访者不同意。然而,只有47%(n=883)的受访者表示他们在实践中始终使用造口周围皮肤评估工具。在确定的工具中,最常使用的工具是采用DET评分的造口皮肤工具(表3)29。
表3.最常用的造口周围皮肤评估工具
在PSC患者中观察到的主要健康指标由高到低依次为(图3):
1. 潮湿相关性皮肤损伤(MASD)。
2. 接触性皮炎。
3. 黏膜分离。
4. 细菌、真菌或酵母菌感染。
5. 皮肤剥脱。
6. 医用粘胶相关性皮肤损伤(MARSI)。
7. 缝合肉芽肿。
8. 増生/组织过度生长。
9. 毛嚢炎。
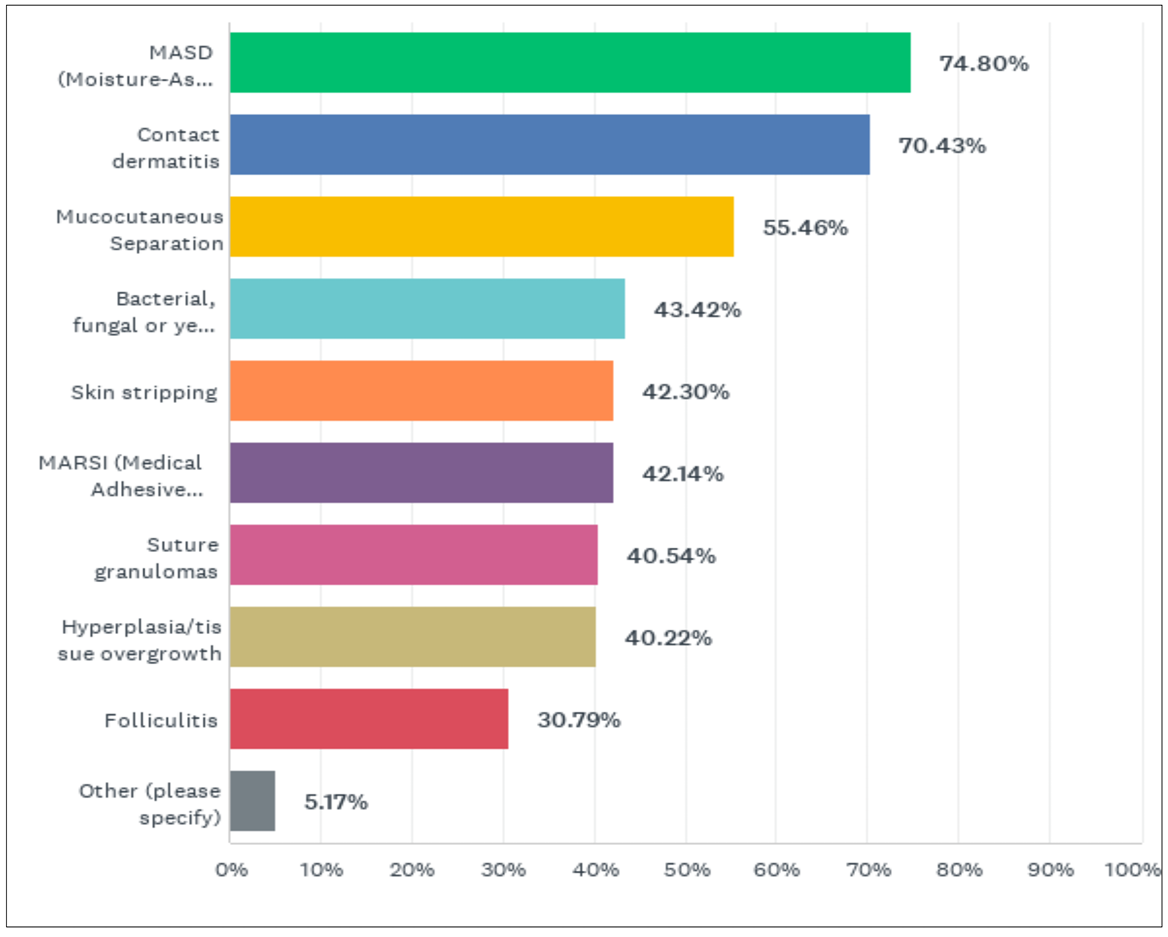
图3.据您观察,您的患者中PSC的主要健康指征是什么?(由1877名调查受访者回答)
PSC对患者生活质量的主要影响是:90%的受访者认为増加了对渗漏的担忧;88%的受访者认为社会活动减少/社交孤立;82%的受访者认为患者对造口袋系统的信心下降;82%的受访者认为疼痛和瘙痒加重;77%的受访者认为安全感和信心下降;76%的受访者认为对睡眠模式产生负面影响;60%的受访者认为患者的工作效率下降。
对于发生PSC的患者,最常识别出的风险按降序排列如下,从受访者最常识别出的因素开始(表4):
1. 造口结构。
2. 造口类型。
3. 造口管理/自我护理技术。
4. 体型/BMI。
5. 患者自我护理培训和教育有限。
6. 身体能力(视力、灵巧性、灵活性、移动能力)。
7. 原有的皮肤病(过敏、银屑病等)。
8. 对护理方案的依从性。
9. 合并症和基础疾病(即克罗恩病)。
10. 获得造口护理护士/专家诊治的机会有限。
11. 缺乏家人陪伴/照顾/社交网络。
12. 年龄。
13. 医疗保健系统内对造口产品的补贴有限。
14. 生活水平。
15. 心智能力。
16. 可获得的造口产品类型有限。
表4.受访者确定的发生PSC的主要风险因素
受访者认为以下是患者发生PSC的最常见原因( 图4):
造口流出物渗漏(造口袋密封不良)。
造口周围皮肤的疤痕、皱纹和褶皱。
造口结构/高度和位置。
未及时处理轻微的皮肤刺激,导致病情恶化。
患者对护理方案的依从性,包括正确清洁造口周围皮肤。
当被要求确定他们目前用于维持最佳造口周围皮肤健康的主要预防策略时,受访者表示根据患者体型选择造口袋系统和进行患者教育是最重要的两个策略(表5)。
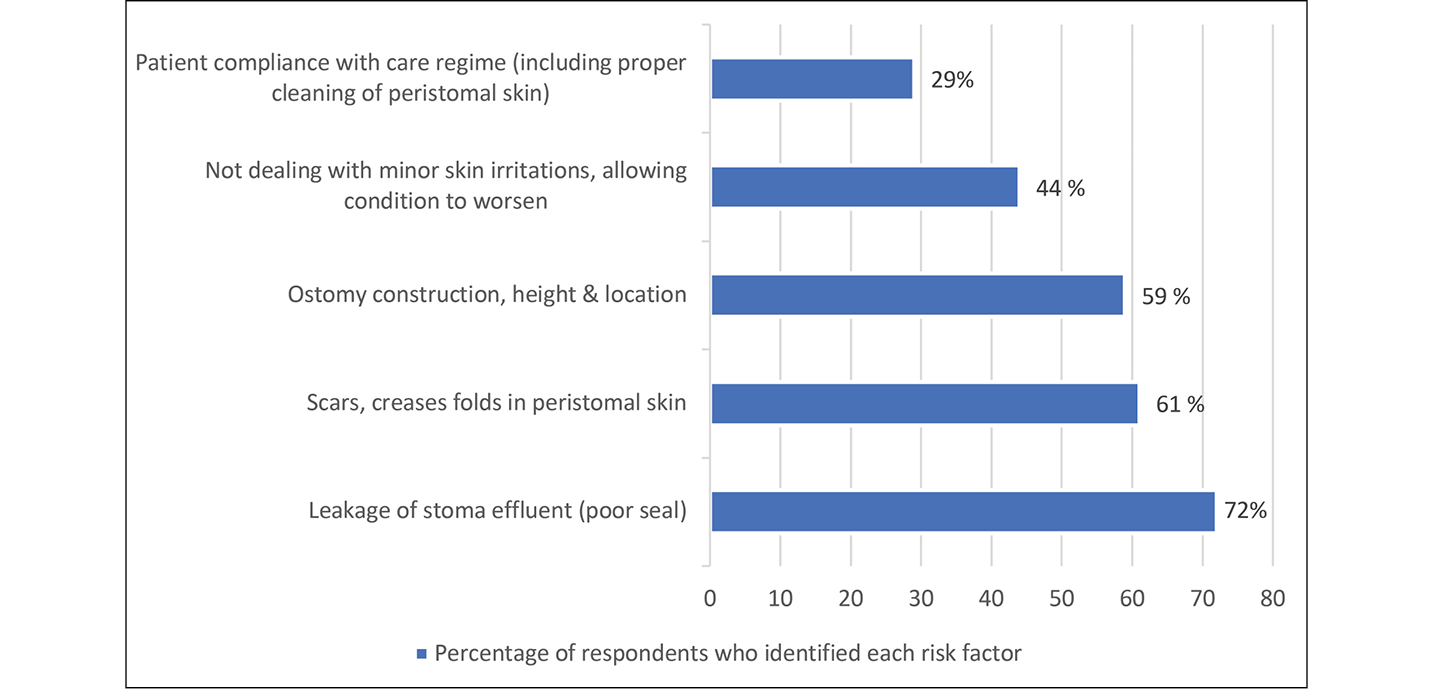
图4.在受访者的患者人群中五个最常见的导致PSC的风险因素
表5.受访者报告用于保持最佳造口周围皮肤健康的主要预防策略
受访者还被问及他们的医疗保健系统。为了确定护理服务的效果和可负担性的影响,受访者被问及在为患者确定最佳造口袋系统时,费用问题对决策的影响有多大。回答因地区而异,但不因系统类型(即公共系统与私人系统)而异。来自亚洲、美国和加拿大的受访者往往更经常考虑费用,而来自欧洲、中东和非洲的受访者则不经常考虑费用(图5)。当被问及为造口手术患者提供的出院后计划时,总体而言,只有56%的受访者表示他们所有的造口患者都能获得出院后计划,美洲最低,为43%,欧洲最高,为72%。出院后计划的时长也因地区而异,欧洲最长,51%的受访者表示他们的出院后计划超过12个月;美洲的受访者中,55%表示他们的出院后计划是2个月或更短。
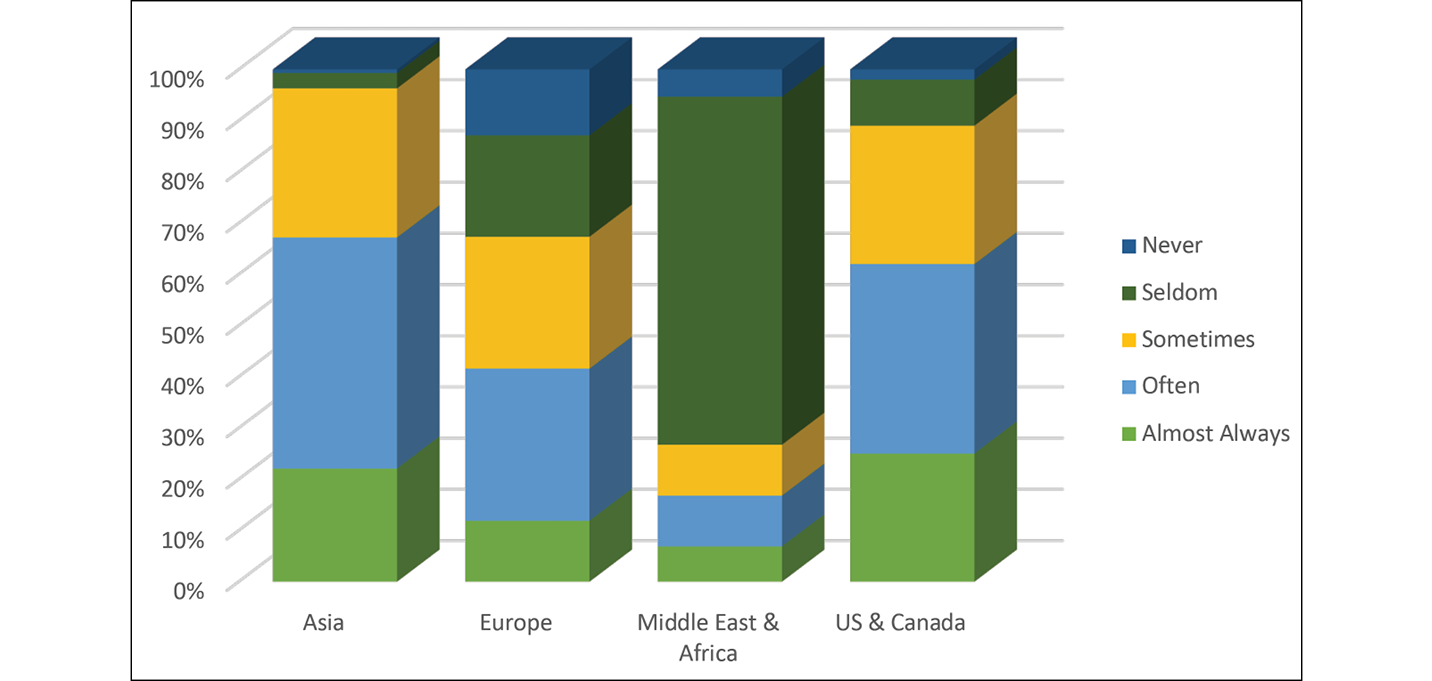
图5.在为患者确定最佳造口袋系统时,费用问题对决策的影响有多大(按地区报告)
调查结果还提供了关于受访者对造口袋系统的经验的见解。共有97%的受访者表示,提供一系列产品以满足个人造口需求并能适应每个患者的体型是重要或非常重要的。总体而言,99%的受访者表示,在评估患者发生PSC的风险时,产品因素很重要。最后,受访者确定了在预防PSC方面被视为最重要的产品粘合性能方面的考虑因素,按普遍性排序:
应用和拆除的便利性。
跟随身体动作的能力。
粘合剂的耐侵蚀性。
是否需要増加配件来帮助提高产品的有效性。
皮肤剥脱的可能性。
产品附着在皮肤上的速度(立即粘附在皮肤上)。
表6显示了受访者认为确定患者的最佳造口袋系统的必要因素。三类风险因素得到了调查受访者的支持:患者(体型、身心能力以及社会支持);造口产品(可用性、穿戴时间、粘合性能、适应性等);以及医疗保健系统(费用、医疗服务提供者和专家的可及性、指南和限制、保险条款等)(表7)。
表6.受访者在为患者确定最佳造口袋系统时始终考虑的因素
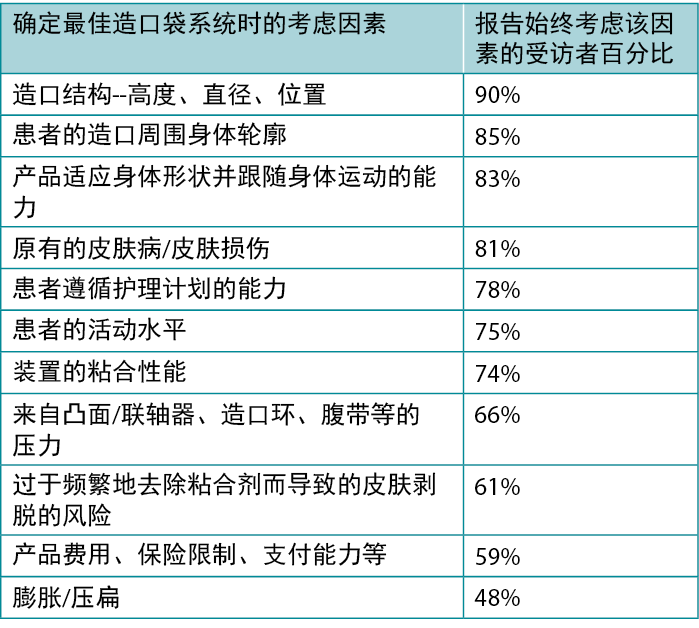
表7.在调查2(n=2023)中询问的对风险因素分类的支持程度
讨论
对受访者的调查结果显示,临床医生强烈支持预防PSC。一旦出现造口周围皮肤问题,就很难做出反应,因为一旦造口周围皮肤受损,就更难获得安全的密封,从而导致渗漏和造口周围皮肤进一步恶化5,8,21。当造口部位周围的皮肤完整性受损时,就会加剧造口装置的粘附问题;因此,预防PSC至关重要14,19,22。
受访者同意,造口周围皮肤健康对造口患者的整体健康、幸福和生活质量很重要,使造口周围皮肤看起来和感觉起来与造口周围区域外的皮肤一样是一个现实的目标30。为了让造口患者在其一生中保持健康的造口周围皮肤,医疗服务提供者应该在患者的整个病程定期识别每位患者发生PSC的风险因素22,29。识别风险使医疗服务提供者可以与患者合作,选择合适的造口袋系统,并制定最佳的护理计划,以缓解已识别的风险,并保持/促进造口周围皮肤健康20。
使用改良的徳尔菲法,就保持造口周围皮肤完整性的重要性和预防PSC必须考虑的风险因素达成了强烈的共识。通过文献综述中确定的证据13以及从调查和促进对话中收集的经验证据,最终开发了PSC风险因素模型并得到批准(图6)。
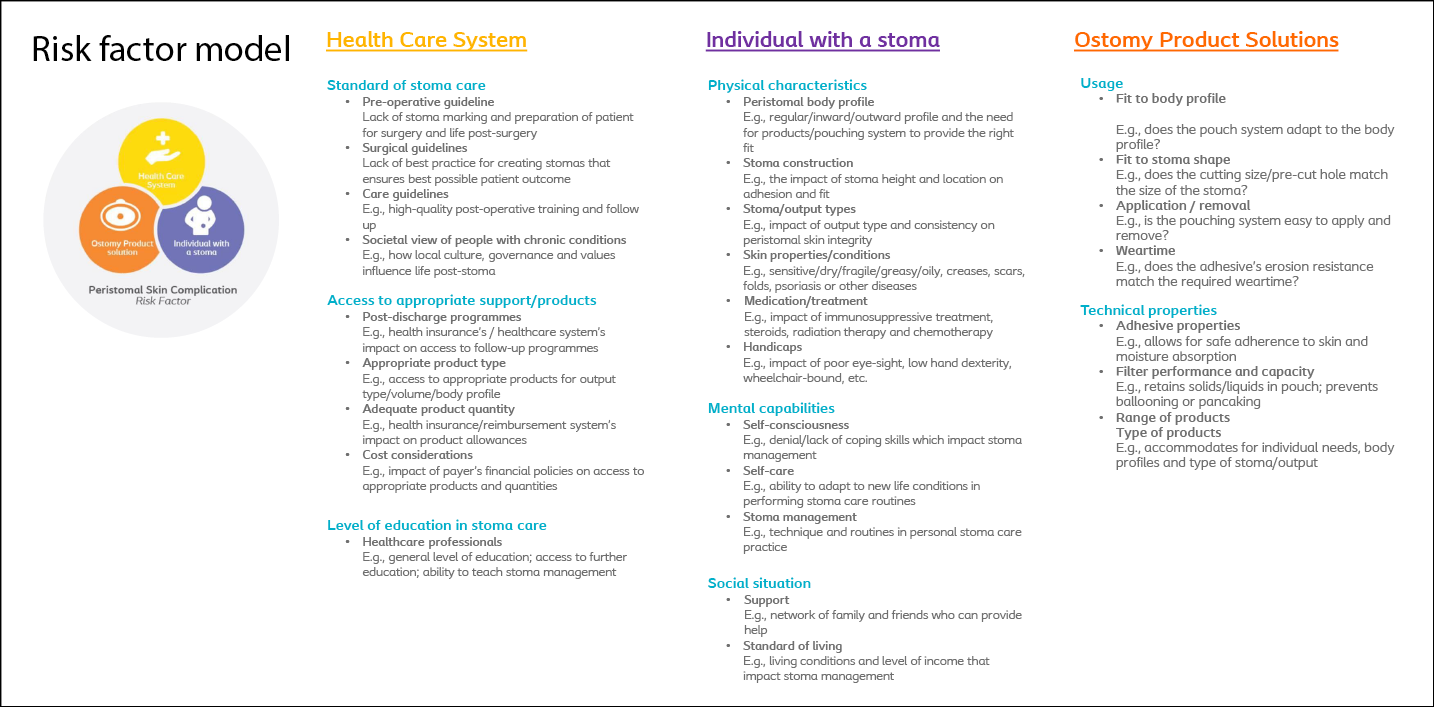
图6.PSC风险因素模型13
该模型将造口周围风险因素分为三类Å\Å\造口患者、造口产品解决方案和患者所处的医疗保健系统。其中每个类别都包含一系列风险因素,医疗服务提供者在评估患者发生PSC的风险时应考虑这些因素。PSC风险因素模型旨在指导医疗服务提供者识别每个患者的风险,以便制定个性化的护理计划,为造口患者的造口周围皮肤健康和整体幸福感提供支持。调查结果具有国际性质,支持该模型可作为一个全球性框架,为预防PSC的区域决策提供循证基础。
优势和局限性
本项目的优势在于参与者数量众多且具有地域多样性。共收到近4300份调查回复,来自遍布六大洲的经验丰富的造口护理提供者。该研究的跨国、多文化和多语言性质使得该模型具有独特的地位,可以根据系统需求和患者期望,在区域内进行重点和实施方面的适当变化。
另一个优势是专家小组成员的经验深度和广度,他们担任了这个过程的监管人。皮肤专家小组由经验丰富的造口护士和皮肤科医生组成,他们的研究履历令人印象深刻,在该领域享有很高的声誉。
研究的一个局限性是,由于调查受访者是匿名的,无法知道对第一次调查作出回复的受访者中有多少人也对第二次调查作出了回复。因此,笔者无法计算出确切的参与者总人数。最后,本研究的行业赞助可能会导致受访者对Coloplast A/S的产品产生偏见;但是,无论是调查问题还是与受访者的沟通,均未包含产品名称、类型或描述。调查受访者未以任何方式得到补偿或激励来回应调查。此外,受访者对研究小组和行业赞助合作伙伴都是匿名的。笔者认为,这一做法减少了调查结果的偏倚。
结论
造口袋系统需要造口周围皮肤的完整性才能实现安全密封。如果造口袋系统未安全密封,流出物可能会渗漏到造口周围皮肤上,导致皮肤损伤、糜烂等造口周围并发症。预防渗漏和PSC对造口患者的健康和生活质量至关重要。本研究旨在确定预防PSC的风险因素。风险因素分为三个类别:造口患者(体型、身心能力、社会状况);医疗保健系统(护理标准、可及性和教育);以及造口产品(使用和技术特性)。就风险因素模型及其对PSC预防的重要性达成了国际共识。还达成了一项共识,即所有医疗服务提供者的目标应该是将造口周围皮肤保持在与造口周围区域外的皮肤相同的状况/健康状态。本研究产生的PSC风险因素模型得到了专家小组的一致批准,专家小组与研究作者共同提倡医疗服务提供者将其作为识别风险和防范PSC的第一道防线。
利益冲突声明
项目得到了Coloplast A/S的支持。G Down、B Andersen、L Martins、T Karlsmark和G Jemec都是Coloplast皮肤专家小组的成员。K Bain过去曾为Coloplast A/S执行过促进合同。M Bain过去曾为Coloplast A/S提供数据分析服务。A Steen Hansen、L Feldskov和C Bechshoeft均在Coloplast A/S工作。
资金支持
本项目由Coloplast A/S资助。
Author(s)
Gillian Down
Diploma in Cancer Nursing, EBN (continence and stoma care), Reg. Midwife, RN, NHS
North Somerset and South Gloucestershire Clinical Commissioning Group, Bristol, UK
Kimberly Bain
CPF/M MA
BainGroup Consulting, Kingston, ON, Canada
Birgitte Dissing Andersen
N, Diploma in Nursing Management, ET
The Stoma Clinic, Herlev Hospital, Herlev, Denmark
Lina Martins
RN BScN MScN WOCC(C)
London Health Sciences Centre, ON, Canada
Tonny Karlsmark
MD MDSc
University of Copenhagen, Copenhagen, Denmark
Gregor Jemec
MD MDSc
University of Copenhagen, Copenhagen, Denmark
Mark Bain
MBA
BainGroup Consulting, Kingston, ON, Canada
Lene Feldskov Nielsen
MSc
Coloplast A/S, Humlebæk, Denmark
Cecilie Jaeger Leidesdorff Bechshoeft
PhD
Coloplast A/S, Humlebæk, Denmark
Anne Steen Hansen*
RN BSN ET MA
Coloplast A/S, Holtedam 3, 3050 Humlebæk, Denmark
Email dkasn@coloplast.com
* Corresponding author
References
- European Ostomy Association. Access to ostomy supplies and innovation: guiding principles for European payers; 2012. Available from: https://www.medtecheurope.org/resource-library/access-to-ostomy-supplies-and-innovation-guiding-principles-for-european-payers-2/
- United Ostomy Associations of America. Homepage; 2014. Available from: https://www.ostomy.org/living-with-an-ostomy/
- IQVIA. 2021 OC market research by IQVIA. Available from: 齌国謾洘鶵疗师鎏袸养ㄩ现状来.doc book118.com
- Herlufsen P, Olsen AG, Carlsen B, Nybaek H, Karlsmark T, Laursen TN, Jemec GBE. Study of peristomal skin disorders in patients with permanent stomas. Br J Nurs 2006 Sep 14–27;15(16):854–62. doi:10.12968/bjon.2006.15.16.21848.
- Gray M, Colwell JC, Doughty D, Goldberg M, Hoeflok J, Manson A, McNichol L, Rao S. Peristomal moisture-associated skin damage in adults with fecal ostomies: a comprehensive review and consensus. J Wound Ostomy Continence Nurs. 2013 Jul–Aug;40(4):389–99. doi:10.1097/WON.0b013e3182944340. PMID:23652738.
- Cottam J, Richards K. National audit of stoma complications within 3 weeks of surgery. Gastrointest Nurs 2006;4(8):34–39.
- Richbourg L, Thorpe JM, Rapp CG. Difficulties experienced by the ostomate after hospital discharge. J Wound, Ostomy Continence Nurs 2007;34:70–79.
- Colwell J, Pittman J, Raizman R, Slavadalena G. A randomized controlled trial determining variances in ostomy skin conditions and the economic impact (ADVOCATE Trial). J Wound, Ostomy Continence Nurs 2018;45(1):37–42.
- Carlsson E, Fingren J, Hallén AM, Petersén C, Lindholm E. The prevalence of ostomy-related complications 1 year after ostomy surgery: a prospective, descriptive, clinical study. Ostomy Wound Manage 2016 Oct;62(10):34–48.
- Maydick-Youngberg D. A descriptive study to explore the effect of peristomal skin complications on quality of life of adults with a permanent ostomy. Ostomy Wound Manage 2017:63(5):10–23.
- Erwin-Toth P, Thompson S, Davis J. Factors impacting the quality of life of people with an ostomy in North America: results from the Dialogue Study. J Wound Ostomy Continence Nurs 2012;39(4):417–422.
- Claessens I, Probert R, Tielemans C, Steen Hansen A, Nilsson C, Andersen B, Storling Z. The Ostomy Life Study: the everyday challenges faced by people living with a stoma in a snapshot. Gastrointest Nurs 2015;13:18–25. doi:10.12968/gasn.2015.13.5.18.
- Hansen AS et al. A risk factor model for peristomal skin complications. WCET® Journal 2022;42(4):14-30.
- Nybaek H, Knudsen DB, Laursen TN, Karlsmark T, Jemec G. Skin problems in ostomy patients: a case-control study of risk factors. Adv Dermatol Venereol 2009;89:64–67.
- Herlufsen P, Olsen AG, Carlsen B, et al. Study of peristomal skin disorders in patients with permanent stomas. Br J Nurs 2006;15(16):854–862.
- Ayik C, Özden D, Cenan D. Ostomy complications, risk factors, and applied nursing care: a retrospective, descriptive study. Wound Manag Prev 2020;66(9):20–30.
- Nagano M, Ogata Y, Ikeda M, Tsukada K, Tokundaga K, Iila S. Peristomal moisture-association skin damage and independence in pouching system changes in persons with new fecal ostomies. J Wound Ostomy Continence Nurs 2019;46(2):137–142.
- Gray M, Colwell JC, Doughty D, et al. Peristomal moisture-associated skin damage in adults with fecal ostomies: a comprehensive review and consensus. J Wound Ostomy Continence Nurs 2013;40(4):389–399.
- Nybaek H, Jemec GB. Skin problems in stoma patients. J Eur Acad Dermatol Venereol 2010 Mar;24(3):249–57.
- Colwell J, Bain K, Hansen AS, Droste W, Vendelbo G, James-Reid S. International consensus results: development of practice guidelines for assessment of peristomal body and stoma profiles, patient engagement, and patient follow-up. J Wound Ostomy Continence Nurs 2019 Nov/Dec;46(6):497–504.
- Colwell J. Selection of a pouching system. In: Carmel JE, Colwell JC, Goldberg MT, eds. Wound Ostomy and Continence Nurses Society core curriculum: ostomy management. Philadelphia, PA: Wolters Kluwer; 2016. p. 120–130.
- Rolstad BS, Erwin-Toth PL. Peristomal skin complications: prevention and management. Ostomy Wound Manage 2004 Sep;50(9):68–77.
- Innes JE. Consensus building: clarifications for the critics. Planning Theory 2004;3(1):5–20.
- Bain K, Hansen AS. Strengthening implementation success using large-scale consensus decision-making-A new approach to creating medical practice guidelines. Evaluation and Program Planning. 2020 Apr 1;79:101730.
- Bain K (ed). The power of facilitation. Toronto, Canada; 2020. p. 52.
- Stone E, Jones BF. The science behind the growing importance of collaboration. Kellogg Insight; 2017. Available at: www.insight.kellogg.northwestern.edu/article/the-science-behind-the-growing-importance-of-collaboration
- Grol R, Wensing M, Eccles M, Davis, D. Improving patient care: the implementation of change in clinical practice. Edinburgh: Elsevier; 2005.
- Dalkey N, Helmer O. An experimental application of the Delphi method to the use of experts. Management Sci 1963;9:458–467.
- Martins L, Ayello EA, Claessens I, Steen Hansen A, Hentze Poulsen L, Sibbald RG, Jemec GB. The ostomy skin tool: tracking peristomal skin changes. Br J Nurs 2010 Aug 12–Sep 8;19(15):960, 932–4. doi:10.12968/bjon.2010.19.15.77691. PMID:20966862.
- Ratliff C, Goldberg M, Jaszarowski K, McNichol L, Pittman J, Gray M. Peristomal skin health. J Wound Ostomy Continence Nurs 2021;48(3):219–231.


