Volume 43 Number 3
Contributions of irrigation for continence in permanent colostomy: a case study
Ayişe Karadağ, Havanur Kılıç
Keywords Colostomy, quality of life, irrigation, peristomal skin complications, cost analysis
For referencing Karadağ A & Kılıç H. Contribution of irrigation for continence in permanent colostomy: a case study. WCET® Journal 2023;43(3):30-35.
DOI
https://doi.org/10.33235/wcet.43.3.30-35
Submitted 8 April 2023
Accepted 6 June 2023
Abstract
Bowel management in the person with a permanent colostomy is important and the burden of continuous use of bags and adapters (base plates / skin barriers) on health care costs and the environment is known. When applied regularly, colostomy irrigation (CI) contributes to improving the quality of life (QOL) of the individual with a permanent colostomy by enabling improved faecal continence and reducing costs. The aim of this article was to examine the positive impact of CI on an individual’s QOL and health expenditures. In this case, it was found that a patient with a permanent colostomy who had performed CI for 21 years could eliminate many of the physical and psychological problems as well as peristomal skin complications (PSCs), arising from using a colostomy appliance only. It was also determined in this case scenario that bowel management using CI was three times more cost-effective than the colostomy bag system.
Introduction
The formation of a colostomy is one of the most commonly applied therapeutic interventions for pathological conditions in the large intestine, primarily for colorectal cancer. This intervention has negative effects on the patient’s QOL by altering body image, defecation habits, and lifestyles.1 A colostomy is associated with many potential or actual problems such as economic burden, psychological and sexual problems, dissatisfaction with the changes in self-image and daily routines, travel difficulties, and fatigue.2-4
Faecal evacuation via colostomies can be managed in several methods: natural spontaneous evacuation using the stoma bag, control with medication, insertion of glycerine suppository or micro-enema into the colostomy, and colostomy irrigation.5 Despite its many advantages, CI has not yet achieved the popularity it deserves among healthcare practices.6 It is the process of instilling 500-1500 ml of water into the colon through the stoma to stimulate colonic peristalsis, thus ensuring bowel evacuation.3 When applied at regular intervals, CI can result in no or minimal faecal evacuation between irrigations, thus achieving a level of continence for individuals.4 The best candidates for CI are adult patients motivated to irrigate, those who have no physical or psychological barriers, other health conditions where CI is contraindicated or issues of compliance in managing a colostomy in the descending or sigmoid colon.7 Physical barriers may include poor vision or poor manual dexterity whereas altered mental alertness or other mental health issues may pose psychologocal barriers. Irritable bowel syndromes, peristomal hernias and post radiation damage are conditions that may prevent the use
of CI8.
CI is rarely associated with complications when administered safely and correctly. It also helps to improve the QOL of individuals with a colostomy.4 CI improves one’s sense of psychological well-being (PWB) and can help overcome problems such as anxiety, depression, and uncertainty. In addition, CI has a positive effect on social challenges, such as the maintenance of intimate relationships as the colostomy appliance can be replaced with a low-profile stoma cap. In general, CI reduces odor and flatus, the most confronting social barriers for patients, and facilitates sleeping, eating, and traveling.7 Further, CI also positively affects spiritual and occupational challenges. From a spiritual perspective, CI prevents untimely noisy and porous discharge of gas and/or faeces, which invalidates ablution and may prevent participation in congregational prayers3. From an employment perspective, CI provides a greater sense of security with no pouch requiring emptying, freedom of movement and less likelihood of leakages8,9.
Furthermore, it is reported CI has a positive economic impact by reducing costs of purchasing and disposal of ostomy equipment and contributing to decrease of peri-stomal skin complications (PSCs) compared to natural evacuation using a stoma bag.8-11 As the costs of healthcare increase, medical expenses become part of the care decision-making process, since the patients may have to pay more and more out of their own pockets.9 The WCET 2020 International Ostomy Guideline12 emphasizes that the socio-economic status of the individual should be taken into account in the care planning with this statement: “It is essential that the individual/family is assessed holistically to enable them to participate in care. Planning and implementation should consider individual, social, economic and health system factors.” Healthcare costs are particularly critical for countries with middle/low socio-economic status where ostomy products are imported12.
However, the literature focusing on the cost contribution of CI is insufficient. In Türkiye, there are no studies on the cost of CI. In this paper, in addition to the positive effects of CI on the individual’s life, the effect of CI on healthcare costs was analyzed in a single case and the impact of waste management on environmental health was highlighted.
Case presentation
The patient and colostomy irrigation
M.A.A. is a 54-year-old male patient working as a shepherd in animal husbandry. M.A.A was admitted to a training and research hospital in a metropolitan city with a diagnosis of colon cancer in 2000. Following extensive medical reviews, M.A.A. underwent Abdominoperineal Resection surgery in February 2001, and a permanent colostomy was created. The patient applied for CI in the post-operative period at the stomatherapy unit of a university hospital in Türkiye. It was determined he met the necessary criteria for initiation of CI. After the patient was instructed about CI, CI was initiated in September 2001. The patient was initially advised to perform CI every 24 hours at the same hour each day for two months. The Stoma and Wound Care Nurse (WOC nurse) met with the patient one week later to assess whether the procedure was performed correctly and to answer the patient’s questions. Since it was determined that there was no/minimal leakage between irrigations for two months, the CI interval was increased to 48 hours.
Currently, M.A.A. has been undertaking CI every 48 hours for more than 21 years. For 13 of these years, however, he has been reusing the CI sets and stoma caps provided in exchange for his prescribed colostomy equipment which was last issued in 2008. The reason for washing and re-using the CI sets is discussed below.
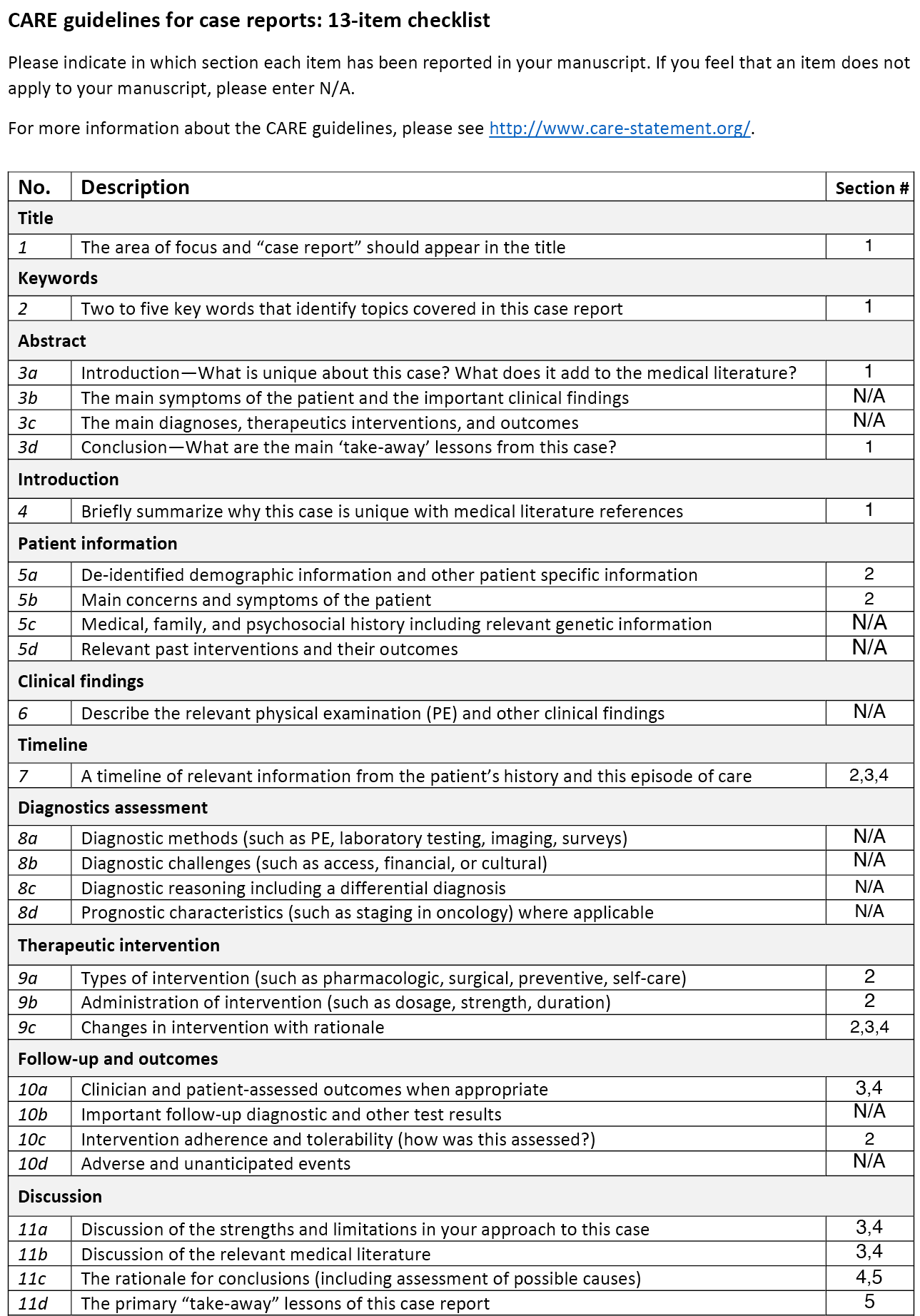
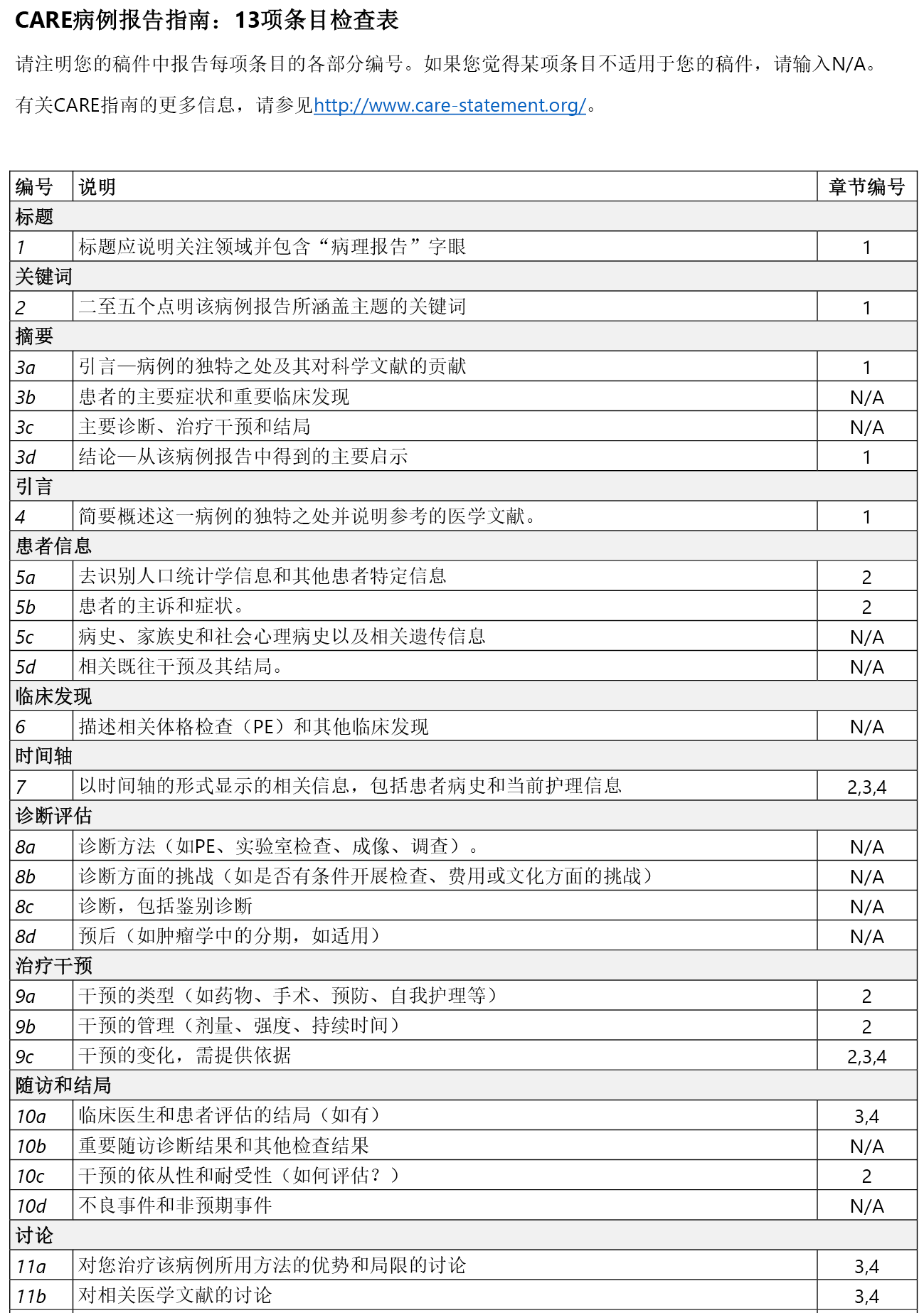
Although confronted with these challenges, M.A.A stated during an interview that since CI eliminated the problems of noise, leakage, odour and flatus his previous levels of anxiety and sleep deprivation caused by these issues were reduced. Moreover, he reported that he did not experience any skin complications in the past 21 years and did not pay for any additional medical examination or associated material costs. The photographs shared by M.A.A. showed that his peristomal skin was healthy (Figure 1-2). M.A.A. stated that he lived very happily with his sheep in the mountains and his only request from us was to seek the inclusion of the CI set and stoma cap in the scope of payment for the irrigation procedure, from which he benefited immensely as did the healthcare system.

Figure 1: Insertion irrigation cone into the stoma

Figure 2: Stoma cap, stoma and peri-stomal skin
Colostomy irrigation and health economics
M.A.A. has health insurance encapsulated within the general framework of health insurance, however, CI sets and stoma caps are not covered by health insurance in Türkiye. The ostomy supplies that are covered by health insurance for colostomy patients are prescribed bimonthly per the treating doctor’s prescription and include 60 bags, 20 adapters and 2 pastes. Between 2001 and 2008, M.A.A. received a prescription for colostomy bags, adapters and pastes and exchanged them for CI sets and stoma caps from the company who supplied his ostomy equipment. Between 2008 and 2021 (13 years), as the patient could not exchange his colostomy equipment, he did not have any newly prescribed colostomy equipment and continued using them by cleaning them (washing irrigation bags and sleeves).
The authors contacted the company in Türkiye M.A.A. purchased his colostomy equipment from and obtained prices for the equipment used. These prices included the two-month standard material prescription price (60 bags, 20 adapters, and 2 pastes), the price of the CI set and the stoma caps. From the prices obtained the estimated cost of the equipment was calculated to be TRY 45,288, assuming most patients with a colostomy would have a natural spontaneous evacuation with a colostomy bag and adapter on average daily between 2001 and 2022, even if no complications occurred. However, the cost of bowel management using a CI set and stoma cap in 2001-2022 was TRY 13,269. If the MAA had not re-used the available materials and had continued to receive a fresh CI set and stoma cap every six months, the cost would have been TRY 42,244.
This cost difference and the benefits that MAA has described in this singular case has demonstrated that CI is a cost-effective approach that positively impacts healthcare costs and the patient’s overall QOL. In addition, the fact MAA reportedly never developed a PSC in 21 years that required medical or nursing treatment which when compared to the known average economic burden of prevention and treatment of PSC’s and the use of healthcare resources may be a notable gain.
In this case, the above data were obtained via interviews conducted with M.A.A., review of his medical records and liaison with the company from which he obtained his supplies. Informed consent was provided by M.A.A. to publish his case details and associated images (Figures 1 and 2).
Discussion
In the literature, the CI usage rate ranges between 2 to 4%6. However, in addition to this case, the authors personal experience and literature suggest that CI has many benefits such as providing fecal continence, eliminating the need for an ostomy bag, providing a sense of security by preventing leaks, and providing comfort8,10. It also has a positive financial impact by reducing the cost of ostomy supplies, PSC interventions, and visits to healthcare facilities such as hospitals or stomal therapy clinics10. In accordance with the literature7,13, M.A.A also mentioned that he continued his usual daily activities with CI, that his anxiety and sleeping problems previously caused by noise, leakage, odour and flatus were eliminated, and that resolution these issues were positive results on the main factors affecting his peristomal skin health and QOL. The impact of CI on complications and costs was demonstrated in this case. It is certainly not possible to make generalised or assertive conclusions based on a single case. Nonetheless, a recent systematic review of stoma complications reported that long-term colostomy complications across all stoma types was 26.5% (2.0–100%). Further, across all stoma types PSCs accounted for the highest incidence of complications at 14.0% (2.4–46.2%). Those with end colostomies had the highest incidence of complications, with 62.6% (2.0–100%) of patients affected.14
It is remarkable that no complications developed in our case. Certainly, health-related social factors, such as the fact that M.A.A. is relatively young and leads a quiet, active life in the countryside, should not be overlooked. Another issue is the impact of CI on the reduction of healthcare costs. In this specific case, the cost of the materials used by M.A.A. for CI in 21 years was calculated three times lower than in the case of spontaneous evacuation with the bag system. The estimated cost projection of potential PSC complications was not included in these costs. It has been estimated however that the average cost of ostomy supplies increased sixfold over seven weeks for people with PSCs.15 Therefore, the prevention of PSCs with CI also eliminates the need for patients to pay for additional medical examinations and supplies16. Further, in agreement with the literature which suggests the main contributor to the development of PSCs is leakage16,17, no or minimal leakage between irrigations was considered as one of the factors preventing the development of PSCs in this case.
One factor that should not be disregarded is that M.A.A. used the CI set, stoma cap and irrigation elimination bags for far longer than the manufacturer’s recommended period of use. While, in this current case, M.A.A. did not experience any secondary PSCs or infections, we, the authors, as WOC nurses, advise our patients to use all ostomy equipment in accordance with the manufacturer’s instructions. However, this case has led the authors to conclude that companies should perhaps review the duration of use of these disposable materials that pose a risk to nature to see whether an extension of wear time is feasible thereby reducing tangible and environmental costs.
In addition, using CI results in less material consumption than natural spontaneous evacuation using an ostomy bag, which contributes negatively to the environment, plastic consumption, and waste management. The disposal of materials such as used adapters/bags and the impact on landfills was also a focus of comments on the environmental aspects of CI. It is a reasonable consideration to minimize plastic waste as the importance of our environment and our impact on it will be increasingly critical in the future.9
Conclusion
In this case, it was demonstrated that CI was a cost-effective approach and contributed positively to the physiological and psychosocial well-being parameters. The fact that the patient did not develop PCS contributed significantly to reducing healthcare costs. It is recommended that WOC nurses offer CI as an option to all eligible patients with a permanent colostomy irrespective of whether it is time-consuming, and that the CI set should be included in the scope of the payment system for ostomy equipment within Türkiye .
Further, it should be recognized that, despite the valuable information in this case, the management of bowel evacuation in this patient from a different culture relied entirely on his planning and feedback. It is also important to note that the frequency of use of the CI material differed from the manufacturer’s instructions.
Acknowledgements
The authors thank the company and M.A.A who took part in the study. This case report was prepared according to the CARE guidelines.18
Ethics statement
The first author of this study is Ayise Karadag, and the second author is Havanur Kilic. All authors contributed equally at all parts of the manuscript. The study was adhered to the Declaration of Helsinki. As all authors, we guarantee that we have approved this manuscript’s final version and that the study’s original version has not been previously published or evaluated in another journal. The authors declare that they have no conflict of interest and have not received any special support/funding from any financial institution.
Conflict of interest
The authors declare no conflicts of interest.
Funding
The authors received no funding for this study.

灌洗对永久性结肠造口术患者失禁的作用:一项病例研究
Ayişe Karadağ, Havanur Kılıç
DOI: https://doi.org/10.33235/wcet.43.3.30-35
永久性结肠造口术患者的肠道管理非常重要,且众所周知,连续使用造口袋及其适用附件(底板/皮肤屏障)会对医疗费用和环境造成负担。定期进行结肠造口灌洗(CI)可改善大便失禁并减少费用,从而有助于提高永久性结肠造口术患者的生活质量(QOL)。本文旨在研究CI对个体QOL和健康支出的积极影响。在该病例中,研究者发现,一名永久性结肠造口术患者在21年内持续使用CI,可以消除仅使用结肠造口器械所导致的许多生理和心理问题以及造口周围皮肤并发症(PSC)。在该病例中,还确定了进行CI的肠道管理成本效益是结肠造口袋系统的三倍。
引言
结肠造口术是治疗大肠病理状况(主要是结直肠癌)最常用的治疗干预之一。此类干预会改变身体形象、排便习惯和生活方式,从而对患者的QOL产生负面影响。1结肠造口术会带来许多潜在或实际问题,如经济负担、心理和性问题、对自我形象和日常生活的变化感到不满、出行困难和疲劳。2-4
通过结肠造口术排泄粪便可以通过以下几种方法进行管理:使用造口袋自然自发排泄、药物控制、在结肠造口中插入甘油栓剂或微型灌肠剂以及结肠造口灌洗。5虽然CI有许多优点,但其尚未在医疗保健实践中普及。6该操作是通过造口将500 mL-1500 mL水逐渐灌入结肠,以刺激结肠蠕动,从而确保排便的过程。3定期进行CI可导致两次灌洗之间无粪便排出或只有极少量的粪便排出,从而达到一定程度的个体控便水平。4CI的最佳候选者是有灌洗动机、无生理或心理障碍、无属于CI禁忌症的其他健康状况或不存在与管理降结肠或乙状结肠造口术相关的依从性问题的成人患者。7生理障碍可能包括视觉不良或手指灵活性较差,而精神警觉性改变或其他心理健康问题可能造成心理障碍。肠易激综合征、造口周围疝气和辐射后损伤等疾病均可能会妨碍CI的使用8。
安全、正确地进行CI操作时,很少会出现并发症。它还有助于改善结肠造口术患者的QOL。4CI可提高患者的心理幸福感(PWB),有助于克服焦虑、抑郁和不确定感等问题。此外,由于可以使用低剖面造口盖替代结肠造口器械,所以CI还对维持亲密关系等社会挑战产生了积极影响。一般而言,CI可减少患者最难以克服的社交障碍Å\Å\异味和胀气,并有助于睡眠、进食和出行。7此外,CI还对精神和职业挑战产生了积极影响。从精神角度来看,CI可防止不及时的嘈杂和多孔胀气和/或粪便排放,从而使洗礼无效,并可能妨碍患者参与会众祷告3。从就业角度来看,CI提供了更强的安全感,无需排空造口袋,可自由移动,且渗漏的可能性更小8, 9。
此外,据报告,与使用造口袋自然排泄相比,CI可降低购买和处置造口设备的成本,有助于减少造口周围皮肤并发症(PSC),从而产生积极的经济影响。8-11随着医疗保健成本的増加,患者可能必须自费支付越来越多的费用,因此医疗费用将成为护理决策过程的一部分。9WCET 2020国际造口指南12强调,在制定护理计划时应考虑个人的社会经济状地位,并做出以下声明:“必须对个人/家庭进行全面评估,使他们能够参与护理工作。计划和实施应考虑个人、社会、经济和卫生系统因素。”对于需进口造口产品的社会经济地位中等/较低的国家,医疗费用至关重要12。
但重点关注CI费用分摊的文献非常少。在土耳其,尚无关于CI费用的研究。在本文中,除分析了CI对个体生活的积极影响外,还在单个病例中分析了CI对医疗费用的影响,并强调了废物管理对环境卫生的影响。
病例报告
患者和结肠造口灌洗
M.A.A.是一名54岁男性患者,他从事畜牧业,是一名牧羊人。2000年,M.A.A被诊断出患有结肠癌,因此住进了某大城市的一家培训和研究医院。经过广泛的医学审查,M.A.A.于2001年2月接受了经腹会阴直肠切除术,并建立了永久性结肠造口。术后,患者在土耳其大学医院的口腔治疗科接受CI。经确定,其符合开始进行CI的必要标准。患者接受关于CI的指导后,于2001年9月开始进行CI。最初建议患者在每天同一时间进行CI,每24小时一次,持续两个月。造口和伤口护理护士(WOC护士)在一周后与患者会面,以评估是否正确进行该操作,并回答患者的问题。由于确定两个月内进行的灌洗之间不存在/极少出现渗漏,所以将CI间隔时间延长至48小时。
目前,M.A.A.保持每48小时进行一次CI,并已持续超过21年。但是,在其中13年间,他一直重复使用提供的CI套件和造口盖,以换取于2008年最后一次向其发放的处方结肠造口术设备。清洗和重复使用CI套件的原因讨论如下。
尽管面临这些挑战,M.A.A在一次面谈中表示,由于CI消除了噪声、渗漏、异味和胀气问题,他先前由这些问题而产生的焦虑和睡眠不足程度所有减轻。此外,他还报告称,在过去21年中,他并未出现任何皮肤并发症,也未支付任何额外的医学检查或相关材料费用。M.A.A.分享的照片表明其造口周围皮肤保持健康(图1-2)。M.A.A.表示,他和他的羊群在山中生活得非常愉快,他向我们提出的唯一请求是希望将CI套件和造口盖纳入灌洗程序的支付范围,他将从中获得巨大利益,医疗保健系统亦是如此。

图1:将灌洗锥头插入造口

图2:造口盖、造口和造口周围皮肤
结肠造口灌洗和健康经济学
M.A.A.的医疗保险包含在一般医疗保险框架内,然而,CI套件和造口盖不在土耳其的医疗保险覆盖范围内。医疗保险覆盖的供结肠造口术患者使用的造口用品根据主治医生的处方每两个月开具一次,包括60个造口袋、20个适用附件和2个底板。2001年至2008年,M.A.A.收到了开具结肠造口袋、适用附件和底板的处方,并从提供造口设备的公司处换取了CI套件和造口盖。2008年至2021年(13年),由于患者无法更换结肠造口设备,他未获得任何新开具的结肠造口设备,所以通过清洁(清洗灌洗袋和套管)继续使用这些设备。
作者联系了M.A.A.在土耳其购买结肠造口设备的公司,并了解了所用设备的价格。这些价格涵盖两个月的标准材料处方价格(60个造口袋、20个适用附件和2个底板)以及CI套件和造口盖的价格。根据获得的价格,假设大多数结肠造口术患者在2001年至2022年期间,即使未出现并发症,平均每天也会使用结肠造口袋和适用附件进行自然自发排泄,由此计算的设备估计费用为45,288土耳其里拉。但是,2001-2022年使用CI套件和造口盖进行肠道管理的费用为13,269土耳其里拉。如果MAA未重复使用可用材料,并继续每六个月领取一套新CI套件和造口盖,则费用将为42,244土耳其里拉。
这一成本差异和MAA在该单个病例中描述的获益表明,CI是一种具有成本效益的方法,可对医疗费用和患者的总体QOL产生积极影响。此外,据报告,MAA在21年中从未患过需要医学治疗或护理治疗的PSC,与预防和治疗PSC的已知平均经济负担和医疗资源的使用相比,这可能是一项显著的获益。
在该病例中,上述数据均通过与M.A.A.面谈、审查其病历以及与向其提供用品的公司取得联系而获得。M.A.A.提供了知情同意书,允许发布其病例详情和相关图像(图1和图2)。
讨论
文献中的CI使用率在2%至4%范围内6。但是,除该病例外,作者的个人经验和文献资料表明,CI还具有许多益处,如有助于大便控制、无需使用造口袋、通过防止渗漏提供安全感且舒适度较高8, 10。它还可以降低造口用品、PSC干预以及前往医院或造口治疗诊所等医疗保健机构就诊的费用,从而产生积极的经济影响10。根据文献7, 13,M.A.A还提到,他在进行CI后可继续开展日常活动,先前因噪音、渗漏、异味和胀气引起的焦虑和睡眠问题均得以消除,并且这些问题的解决还对影响其造口周围皮肤健康状况和QOL的主要因素产生了积极影响。在该病例中证实了CI对并发症和成本的影响。当然,无法根据单个病例得出概括性或肯定性结论。尽管如此,最近一项关于造口并发症的系统性综述报告称,各类造口的长期结肠造口术并发症发生率为26.5%(2.0%-100%)。此外,在各类造口中,PSC的并发症发生率最高,达到14.0%(2.4%-46.2%)。末端结肠
造口术患者的并发症发生率最高,有62.6%(2.0%-100%)的患者受到影响。14
值得注意的是,在我们研究的病例中未出现并发症。当然,健康相关的社会因素也不容忽视,如M.A.A.相对较为年轻,其居住在农村,生活较为安逸且积极。另一个问题是CI对医疗费用减少的影响。在这一特定情况下,M.A.A.在21年中所用CI材料的费用比使用造口袋系统自发排泄的费用低三倍。这些费用不包括PSC潜在并发症的估计费用预测。然而,据估计,PSC患者的造口用品平均费用在七周内増加了六倍。15因此,通过CI进行PSC预防还可使患者免于支付额外的医疗检查和用品费用。16此外,与文献中指出的渗漏是导致PSC发生的主要因素的观点
一致16, 17,在该病例中,认为灌洗之间不存在或极少出现渗漏是防止PSC发生的因素之一。
一个不容忽视的因素是,M.A.A.使用CI套件、造口盖和灌洗消除袋的时间远远长于制造商建议的使用时间。虽然在本病例中,M.A.A.未发生任何继发性PSC或感染,但作者作为WOC护士,建议患者按照制造商的说明使用所有造口设备。然而,该病例使作者得出结论,公司或许应该审查这些对自然界构成风险的耗材的使用期限,以确定延长使用时间是否可行,从而降低有形成本和环境成本。
此外,与使用造口袋自然自发排泄相比,使用CI所消耗的材料更少,前者对环境、塑料消耗和废物管理均产生了负面影响。对所用适用附件/造口袋等材料的处置以及对垃圾填埋场的影响也是对CI的环境影响进行评论的重点。由于我们越来越重视环境,并且我们对环境的影响在未来将变得越来越重要,所以考虑尽量减少塑料废物十分合理。9
结论
在该病例中,已证明CI是一种具有成本效益的方法,对生理和心理社会健康参数具有积极作用。该患者未发生PCS,这在很大程度上降低了医疗费用。建议WOC护士为所有符合条件的永久性结肠造口术患者提供CI选择,无论其是否耗时,并建议将CI套件纳入土耳其造口设备支付系统的范围内。
此外,应认识到,虽然该病例提供的信息很有价值,但该例来自不同文化背景的患者的排便管理完全依赖于他的计划和反馈。还需注意的是,CI材料的使用频率与制造商的说明不同。
致谢
作者对参与研究的公司和M.A.A致以谢意。本病例报告根据CARE指南编写。18
伦理声明
本研究的第一作者是Ayise Karadag,第二作者是Havanur Kilic。所有作者对稿件各部分的贡献相同。该项研究符合《赫尔辛基宣言》。我们,即所有作者,保证我们已批准本稿件的最终版本,并且研究的原始稿件版本先前未曾在另一期刊中发表或接受评价。作者声明不存在任何利益冲突,也未获得任何金融机构提供的任何特殊支持/资助。
利益冲突声明
作者声明无利益冲突。
资助
作者未因该项研究收到任何资助。
Author(s)
Ayişe Karadağ*
PhD ET/WOC Nurse
Professor, Koç University, School of Nursing, İstanbul, Türkiye
Email akaradag@ku.edu.tr
Havanur Kılıç
RN PhD Student
Teaching Assistant, Koç University, Graduate School of Health Sciences, İstanbul, Türkiye
* Corresponding author
References
- Vonk-Klaassen SM, de Vocht HM, den Ouden ME et al. Ostomy-related problems and their impact on quality of life of colorectal cancer ostomates: a systematic review. Qual Life Res. 2016;25 (1):125-133. doi:10.1007/s11136-015-1050-3
- Stavropoulou A, Vlamakis D, Kaba E, et al. “Living with a Stoma”: Exploring the Lived Experience of Patients with Permanent Colostomy. Int J Environ Res Public Health. 2021;18 (16):8512. Published 2021 Aug 12. doi:10.3390/ijerph18168512
- Karadag A & Baykara ZG. Colostomy irrigation: an important issue for Muslim individuals. Asian Pac J Cancer Prev. 2009;10 (6):1189-1190.
- Karadağ A, Menteş BB & Ayaz S. Colostomy irrigation: results of 25 cases with particular reference to quality of life. J Clin Nurs. 2005;14 (4):479-485. doi:10.1111/j.1365-2702.2004.01083.x
- Lizarondo L, Aye Gyi A, Schultz T. Fluid regimens for colostomy irrigation: a systematic review. Int J Evid Based Healthc. 2008;6 (3):303-310. doi:10.1111/j.1744-1609.2008.00103.x
- Hatton, Sue. Irrigation as an option for stoma management. Gastrointestinal Nursing 2011;9 (7) 2011: 6-7.
- Bauer C, Arnold-Long M, Kent DJ. Colostomy irrigation to maintain continence: An old method revived. Nursing. 2016;46 (8):59-62. doi:10.1097/01. NURSE.0000484963.00982.b5
- Kent DJ, Long MA, Bauer C. Does colostomy irrigation affect functional outcomes and quality of life in persons with a colostomy? J Wound Ostomy Continence Nurs. 2015;42 (2):155-161. doi:10.1097/WON.0000000000000121
- Tallman NJ, Cobb MD, Grant M, et al. Colostomy Irrigation: Issues Most Important to Wound, Ostomy and Continence Nurses. J Wound Ostomy Continence Nurs. 2015;42 (5):487-493. doi:10.1097/WON.0000000000000170
- Boutry E, Bertrand MM, Ripoche J, et al. Quality of life in colostomy patients practicing colonic irrigation: An observational study. J Visc Surg. 2021;158 (1):4-10. doi:10.1016/j.jviscsurg.2020.07.003
- Leong AF, Yunos AB. Stoma management in a tropical country: colostomy irrigation versus natural evacuation. Ostomy Wound Manage. 1999;45 (11):52-56.
- World Council of Enterostomal Therapists® International Ostomy Guideline. Chabal LO, Prentice JL, Ayello EA, eds. Perth, Western Australia: WCET®; 2020.
- Jones, H. “Colostomy irrigation (part 1): impact on quality of life.” Gastrointestinal Nursing 19. 2021: 24-29.
- Malik T, Lee MJ, Harikrishnan AB. The incidence of stoma related morbidity - a systematic review of randomised controlled trials. Ann R Coll Surg Engl. 2018;100 (7):501-508. doi:10.1308/rcsann.2018.0126
- Nichols TR, Inglese GW. The Burden of Peristomal Skin Complications on an Ostomy Population as Assessed by Health Utility and the Physical Component Summary of the SF-36v2®. Value Health. 2018;21(1):89-94. doi:10.1016/j.jval.2017.07.004
- Fellows J, Voegeli D, Håkan-Bloch J, Herschend NO, Størling Z. Multinational survey on living with an ostomy: prevalence and impact of peristomal skin complications. Br J Nurs. 2021;30(16):S22-S30. doi:10.12968/bjon.2021.30.16.S22
- Martins L, Samai O, Fernández A, Urquhart M, Hansen AS. Maintaining healthy skin around an ostomy: peristomal skin disorders and self-assessment. Gastrointestinal Nursing. 2011;9 (Suppl 2):9-13.
- Riley DS, Barber MS, Kienle GS, et al. CARE guidelines for case reports: explanation and elaboration document. J Clin Epidemiol. 2017;89:218-235. doi:10.1016/j.jclinepi.2017.04.026


