Volume 44 Number 1
Treatment of chronic parastomal ulceration with silver sulfadiazine and hyaluronic acid: a case series
Alison Carlin
Keywords wound, peristomal skin, hyaluronic acid, silver sulfadiazine
For referencing Carlin A. Treatment of chronic parastomal ulceration with silver sulfadiazine and hyaluronic acid: a case series. WCET® Journal 2024;44(1):36-39.
DOI
10.33235/wcet.44.1.36-39
Submitted 14 September 2023
Accepted 27 November
Abstract
Skin complications in ostomates are widely reported and can cause physical and emotional challenges in everyday life. Chronic parastomal skin complications can be difficult to heal and cause significant pain.
Two patients presented to the stomal therapy clinic for treatment and were diagnosed with chronic parastomal skin ulceration. Following standard treatment of wound management, topical corticosteroid ointment and appliance review, the ulcers were either not improving or had reoccurred. Treatment with a combination cream consisting of 0.2% Hyaluronic acid (HA) and 1% Silver sulfadiazine (SSD) was initiated and both patients demonstrated complete healing.
Treatment of parastomal skin ulceration with dual action cream 0.2% HA and 1% SSD was successful for these two patients, with a reduction in pain and purulent fluid noted throughout treatment, in addition to a reduced cost of treatment when compared with standard protocols.
Introduction
The risk of an ostomate developing a peristomal skin complication in their lifetime has been estimated as anywhere from 6–80%1. Ostomates with a skin complication report negative body image at a greater rate2. Male ostomates with a skin complication were 1.72 times more likely to report negative body image than ostomates with no skin complications, and female ostomates were even higher at 1.87 times more likely to report negative body image2. These complications account for approximately 40% of all visits to stoma care nurses3.
Peristomal and parastomal skin complication causes can be complex and include chemical injury, skin trauma, infection, contact dermatitis and disease related conditions4. Peristomal skin complications are more common in patients with an ileostomy (57%) and a urostomy (48%) than those with a colostomy (35%)5. Although peristomal skin complications, including ulcers, are quite common, chronic parastomal ulcers are unusual and can be difficult to manage6.
Ostomates who develop parastomal ulcers often have underlying conditions such as Crohn’s disease, irritable bowel disease (IBD) or Pyoderma gangrenosum (PG). Treatment and management of a parastomal ulcer consists of appliance review, wound care, systemic treatment (if patient has Crohn’s disease, IBD or PG) and local treatment, usually a corticosteroid6. If a patient does not have Crohn’s disease, IBD or PG, their parastomal ulcer is likely to respond quickly to local wound treatment6. Symptoms often include pain, appliance difficulties and leakage6. Often these ulcers may not look severe, but ostomates describe a strong burning pain, exacerbated by appliance changes6.
Stoma-associated skin complications have a wide ranging impact on an ostomate’s quality of life, and it is vital they are resolved quickly. The aim of this case study is to examine two ostomates with parastomal ulceration in which the standard treatment plan failed, with ostomates then trialling a new combination treatment of 0.2% Hyaluronic acid (HA) and 1% Silver sulfadiazine (SSD).
Product action
HA induces an accelerated tissue repair reaction, characterised by the growth of well-organised granulation tissue. HA receptor binding engages endothelial cells, macrophages, fibroblasts and keratinocytes and modifies their properties toward a more “repair oriented” condition7,8. In addition to stimulating cellular repair mechanisms, the substantial water binding capacity of HA molecules provides ideal conditions for migration and reproduction of the cells that form new tissue7,8.
SSD is a combination of two antimicrobial agents (silver and sulfadiazine) with broad spectrum antibacterial properties and is especially effective against those micro-organisms often found in infected skin lesions9. Applied on exudative wounds, SSD releases its silver ions, which increase the bacteriostatic effect of the sulfonamide radical. The sustained antimicrobial action of the sulfadiazine and silver combination is due partly to the continuous interaction with the fluids on the wound bed, which induces a slow, prolonged release of silver9.
Combination treatment of HA plus SSD (HA+SSD), as compared to SSD alone, has been proven to accelerate the repair process while also providing broad spectrum antibacterial action10. Clinical studies have demonstrated using the combination product of HA+SSD resulted in a reduction of nursing time, expenses and use of pain relief medication11,12.
Case presentations
Case 1
Patient TW is an 80-year-old female who underwent a total proctocolectomy with formation of an end ileostomy in May 2020. The patient’s ileostomy was healthy and the peristomal skin remained intact until she presented to the stomal therapy outpatient clinic in July 2021 with an ulcer of unknown aetiology. The ulcer measured 80mm x 50mm and was adjacent to her stoma at 10 o’clock. There was no pain and no odour noted, with low serous exudate and a soft base of the wound.
Management and outcome
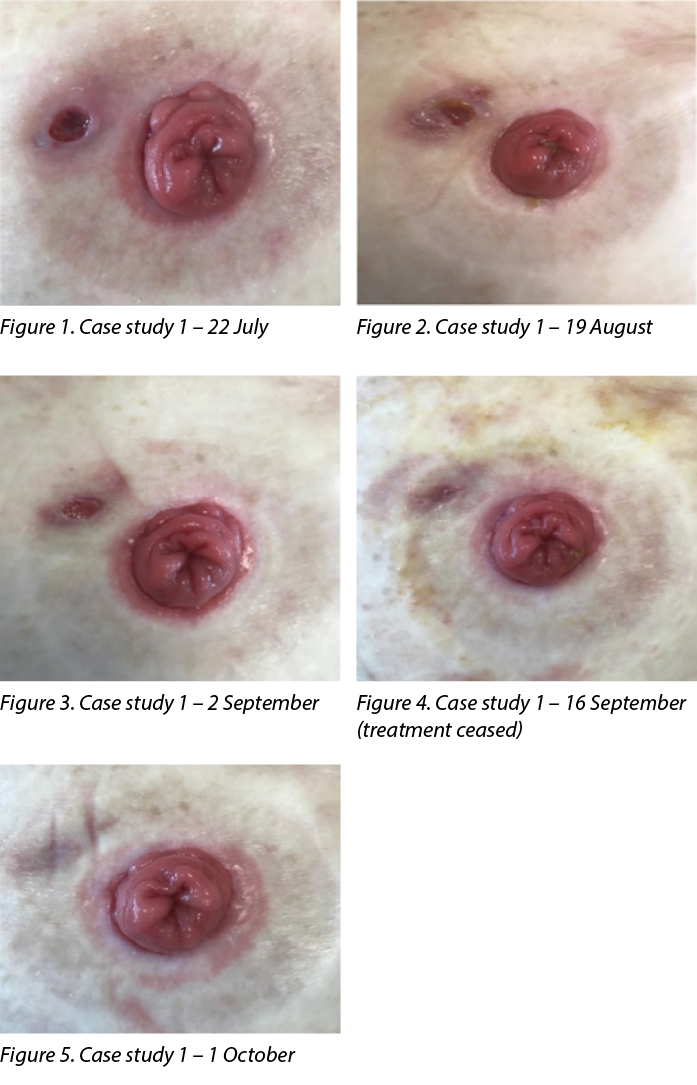
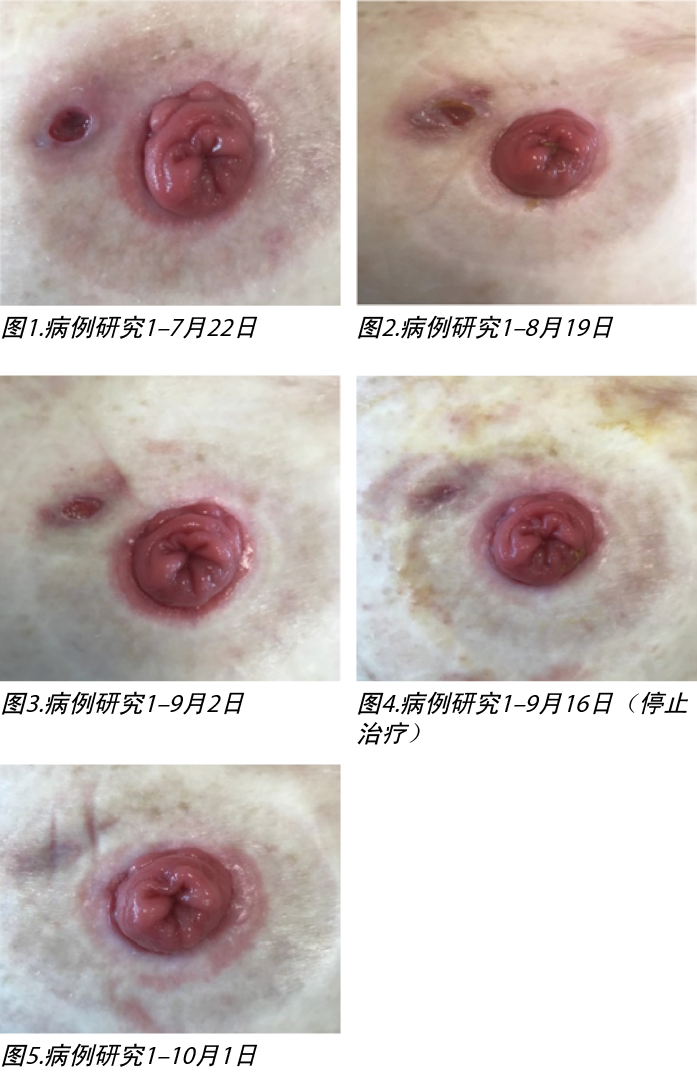
Treatment initiated on 22 July 2021 (Figure 1) was a corticosteroid ointment, a silver antibacterial barrier dressing and a hydrocolloid dressing. The dressing was changed daily in conjunction with changing their ostomy appliance. After 1 month of treatment (Figure 2) the wound was 100mm x 50mm, with a clean base and purulent fluid present. The peri-wound skin was fragile and at risk of further breakdown. The patient’s colorectal surgeon had considered a biopsy to rule out infection of the wound with PG if the wound continued to show no signs of improvement.
The initial treatment was ceased and treatment with a cream containing 0.2% HA and 1% SSD was initiated (HA+SSD). Treatment was daily in conjunction with changing their ostomy appliance, which was the patient’s preference (Figure 3).
Following treatment with HA+SSD cream the wound continually reduced in size until it was healed. There was no pain or odour noted and the serous exudate reduced. On 16 September (Figure 4) treatment was ceased and the patient was advised to restart treatment if any break down of the wound reoccurred; however, the wound continued healing (Figure 5) and has remained healed almost 12 months later.
The treatment cost of standard vs combination HA+SSD treatment showed significant differences (Figure 6). The combination SSD + HA treatment was greater than 40% less expensive per dressing change, with only 25% of the tube being used in total.
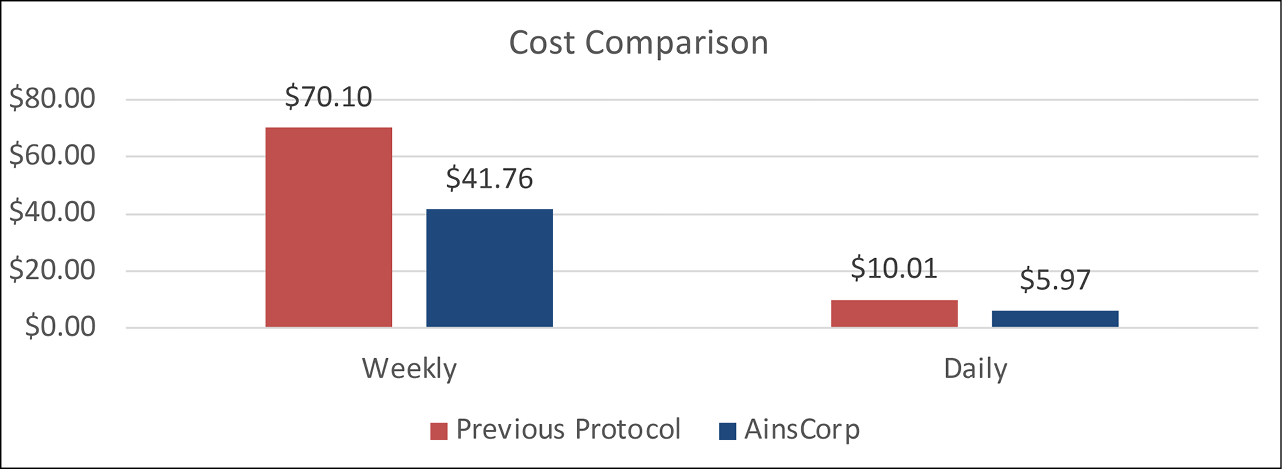
Figure 6. Case 1 – cost comparison of standard treatment vs combination HA+SSD treatment on a weekly and daily basis
Case 2
Patient ML is an 84-year-old male who had an ileal conduit formed in 2007. The patient’s ileal conduit and peristomal skin was healthy following surgery and had not been reviewed by a stomal therapist in 11 years. The patient presented to the stomal therapy outpatient clinic in June 2021 with peristomal ulceration and skin loss. The ulcer measured 20mm x 40mm and extended from the stoma edge from 12 o’clock to 7 o’clock. The ulcer was extremely painful with a sloughy base, low serous exudate and no oedema or odour.
Management and outcome
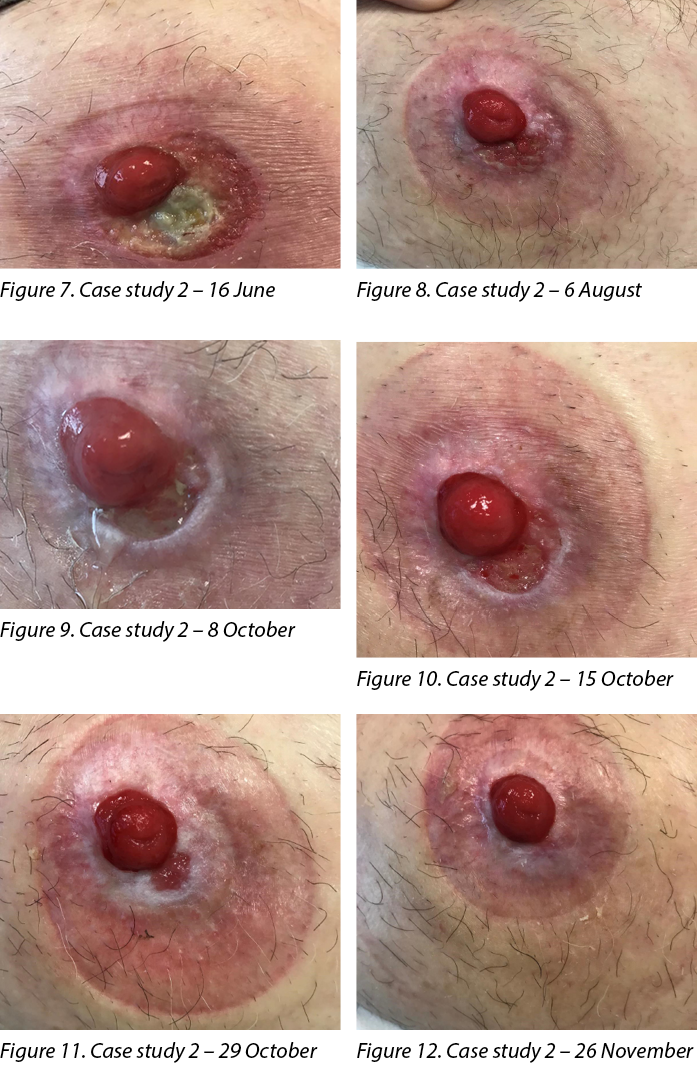
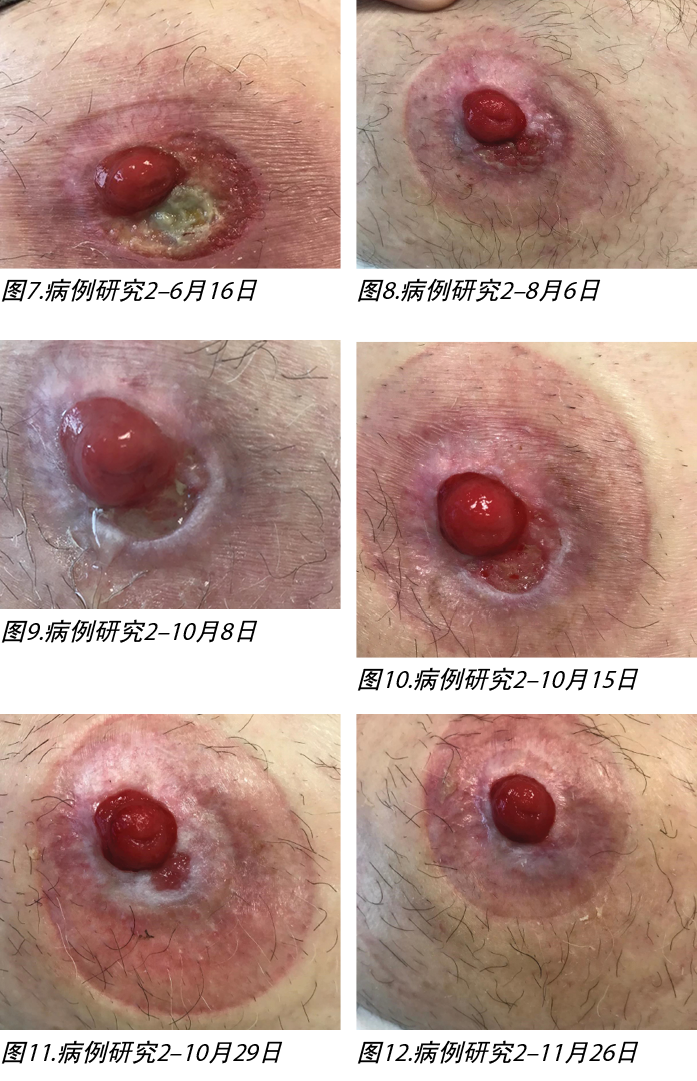
Treatment initiated on 16 June 2021 (Figure 7) was a corticosteroid ointment every second week, a silver antibacterial barrier dressing and a large and a small hydrocolloid ostomy seal. The dressing was changed according to patient preference and when the ostomy appliance leaked, which ranged from once per day to once per week.
Following 6 weeks of treatment (Figure 8), the ulcer was healed and treatment was ceased; however, the new granulation tissue in the 5 o’clock to 7 o’clock section of the ulcer appeared to be very fragile. The patient then re-presented on 8 October with the ulcer having broken down again (Figure 9). The wound measured 10mm x 5mm, with a sloughy pale base, wound edge maceration, low exudate and no pain, no oedema and no odour. At this stage the patient reverted to the initial treatment regime of a corticosteroid ointment every second week, a silver antibacterial barrier dressing and a hydrocolloid ostomy seal. The dressing was changed every 2–3 days, in conjunction with the ostomy appliance.
After 1 week (Figure 10) the wound was increasing (10mm x 20mm) and the initial treatment was ceased and treatment with a cream containing 0.2% HA and 1% SSD was initiated (HA+SSD). Treatment ocurred every two days in conjunction with changing their ostomy appliance, which was according to patient preference.
Following treatment with HA+SSD cream the wound continually reduced in size until it was healed. Two weeks following initial treatment (Figure 11) the wound had reduced from 10mm x 20mm to 5mm x 5mm. There was pink granulation tissue, low serous exudate and some maceration noted at the wound edges. No pain, oedema or odour were noted. Six weeks following treatment (Figure 12) the wound had healed and has since remained healed.
The treatment cost of standard vs combination HA+SSD treatment showed significant differences (Figure 13). The combination HA+SSD treatment was greater than 50% less per dressing change, with only 25% of the tube being used in total.
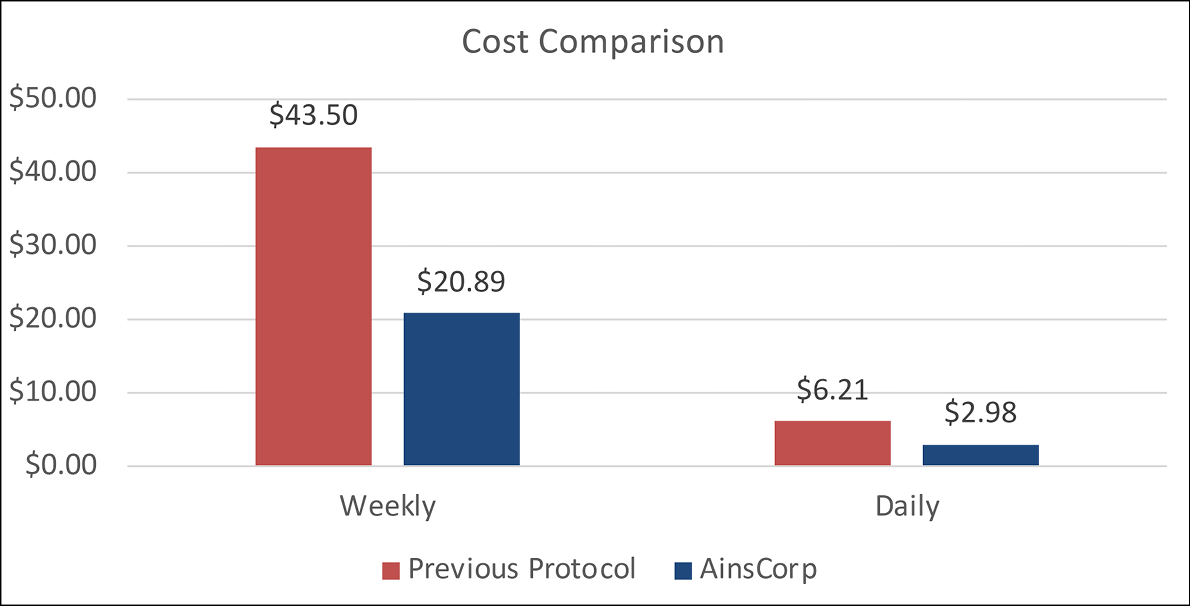
Figure 13. Case 2 – cost comparison of standard treatment vs combination HA+SSD treatment on a weekly and daily basis
Discussion
Both patients presented with parastomal ulcers of unknown aetiology which did not resolve with standard treatment. Following treatment with combination cream treatment 0.2% HA and 1% SSD (HA+SSD) the ulcers were successfully managed and healed. A small pea-sized amount of the combination cream was applied in a thin layer directly to the ulcer using a Q-tip, with no secondary dressing and the ostomy appliance applied on top. The application of cream underneath the baseplate did not affect adhesion of the hydrocolloid, and both patients reported no leakage or baseplate lifting prior to their pouch change schedule. This treatment facilitated discharge of patients from stomal therapy clinic, and both ulcers have remained healed since.
Conclusion
The cost of standard treatment compared to combination treatment of HA+SSD was significant. For Case 1 the cost of standard treatment was 1.68 times higher than the combination treatment, and for Case 2 the cost of standard treatment was 2.08 times higher than the combination treatment. In addition, the standard treatment failed for both patients and the wounds were still not healed after weeks of treatment, whereas the cost of combination treatment was calculated as time to wound healing. The significant cost difference of the HA+SSD combination cream compared to standard parastomal ulcer treatment (not taking into account additional GP reviews for scripts of Kenacomb®) indicates it could be an effective, low-cost intervention which could be applied at first presentation of a parastomal ulcer.
Acknowledgements
The patients consented to the use of their information for this case study. Photographs were taken with the patients’ verbal and written consent.
Conflict of Interest
The authors declare no conflicts of interest.
Funding
The authors received no funding for this study.
磺胺嘧啶银和透明质酸治疗慢性造口旁溃疡:病例系列
Alison Carlin
DOI: 10.33235/wcet.44.1.36-39
摘要
造口患者出现皮肤并发症的情况屡见不鲜,这可能会给患者的日常生活带来身体和精神上的挑战。慢性造口旁皮肤并发症很难治愈,并会引起明显的疼痛。
两例患者前往造口治疗诊所接受治疗,并诊断为慢性造口旁皮肤溃疡。经过伤口管理、局部外用皮质类固醇软膏和装置检查等标准治疗后,溃疡并未好转,亦或是复发。开始使用由0.2%透明质酸(HA)和1%磺胺嘧啶银(SSD)组成的复方乳霜进行治疗,两例患者的伤口均已完全愈合。
这两例患者使用0.2% HA和1% SSD双效乳霜治疗造口旁皮肤溃疡取得了成功,在整个治疗过程中疼痛和化脓性液体均有所减少,并且与标准方案相比,治疗成本也有所降低。
引言
据估计,造口患者一生中发生造口周围皮肤并发症的风险在6%-80%之间1。出现皮肤并发症的造口患者报告负面身体形象的比例更高2。出现皮肤并发症的男性造口患者报告负面身体形象的可能性是未出现皮肤并发症的造口患者的1.72倍,而女性造口患者报告负面身体形象的可能性更高,是后者的1.87倍2。这些并发症约占造口护理护士接诊总量的40%3。
导致造口周围和造口旁皮肤并发症的原因可能很复杂,包括化学损伤、皮肤外伤、感染、接触性皮炎和与疾病相关的病症4。回肠造口术(57%)和尿流改道术(48%)患者造口周围皮肤并发症的发生率高于结肠造瘘术(35%)患者5。虽然包括溃疡在内的造口周围皮肤并发症十分常见,但慢性造口旁溃疡并不常见,而且难以管理6。
出现造口旁溃疡的造口患者通常患有克罗恩病、肠易激综合症(IBD)或坏疽性脓皮病(PG)等基础疾病。造口旁溃疡的治疗和管理包括装置检查、伤口护理、全身治疗(如果患者患有克罗恩病、IBD或PG)和局部治疗,通常使用皮质类固醇6。如果患者未患克罗恩病、IBD或PG,则其造口旁溃疡可能会很快对局部伤口治疗产生反应6。症状通常包括疼痛、装置相关困难和渗漏6。通常情况下,这些溃疡看起来并不严重,但造口患者会描述有强烈的灼痛感,更换装置后疼痛加剧6。
造口相关皮肤并发症会对造口患者的生活质量产生显著影响,因此尽快解决这些并发症至关重要。本项病例研究旨在对两例患有造口旁溃疡、标准治疗方案失败的造口患者进行检查,然后让这两例造口患者试用0.2%透明质酸(HA)和1%磺胺嘧啶银(SSD)的新联合治疗。
产品作用
HA能加速组织修复反应,其特点是生长出组织有序的肉芽组织。HA受体与内皮细胞、巨噬细胞、成纤维细胞和角质细胞结合,可改变它们的特性,使其更加“以修复为导向”7,8。除了刺激细胞修复机制外,HA分子的实质性水结合能力还为形成新组织的细胞的迁移和繁殖提供了理想条件7,8。
SSD是两种抗菌剂(银和磺胺嘧啶)的复方制剂,具有广谱抗菌特性,对感染性皮肤病损中常见的微生物特别有效9。用于渗出性伤口时,SSD会释放出银离子,从而増强磺胺基团的抑菌作用。磺胺嘧啶和银复方制剂的持续抗菌作用部分归因于与伤口床上液体的持续相互作用,导致银释放速度缓慢,释放时间延长9。
研究证明,与单独使用SSD相比,HA与SSD
(HA+SSD)联合治疗可加速修复过程,同时还能发挥广谱抗菌作用10。临床研究表明,使用HA+SSD复方产品可减少护理时间、降低费用并减少止痛药物的使用11,12。
病例报告
病例1
患者TW是一例80岁女性患者,于2020年5月接受了全直肠结肠切除术,并行末端回肠造口术。该患者在2021年7月因病因不明的溃疡前往造口治疗门诊就诊,在此之前,她的回肠造口术情况良好,造口周围皮肤也保持完好。溃疡面积为80 mmÅ~50 mm,紧邻造口10点钟位置。伤口无疼痛感,也无异味,浆液性渗出液较少,基底较软。
管理和结局
2021年7月22日开始接受的治疗(图1)包括皮质类固醇软膏、含银抗菌屏障敷料和水胶体敷料。每天更换敷料并更换造口装置。治疗1个月后(图2),伤口面积为100 mmÅ~50 mm,基底清洁,有化脓性液体存在。伤口周围的皮肤较为脆弱,有进一步破溃的风险。患者的结直肠外科医生曾考虑过,如果伤口仍无好转迹象,就用PG进行活检以排除伤口感染风险。
停止初始治疗后,开始使用含0.2% HA和1% SSD的乳霜(HA+SSD)进行治疗。每天在更换造口装置时进行治疗,这符合患者的偏好(图3)。
使用HA+SSD乳霜治疗后,伤口面积不断缩小,最终愈合。为观察到疼痛或异味,浆液性渗出液也有所减少。9月16日(图4),治疗停止,建议患者在伤口再次发生破溃时重新开始治疗;然而,伤口继续愈合(图5),并在近12个月后保持愈合状态。
标准治疗与HA+SSD联合治疗的成本存在显著差异(图6)。SSD+HA联合治疗每次更换敷料的费用降低了40%以上,总共只使用了25%的管。
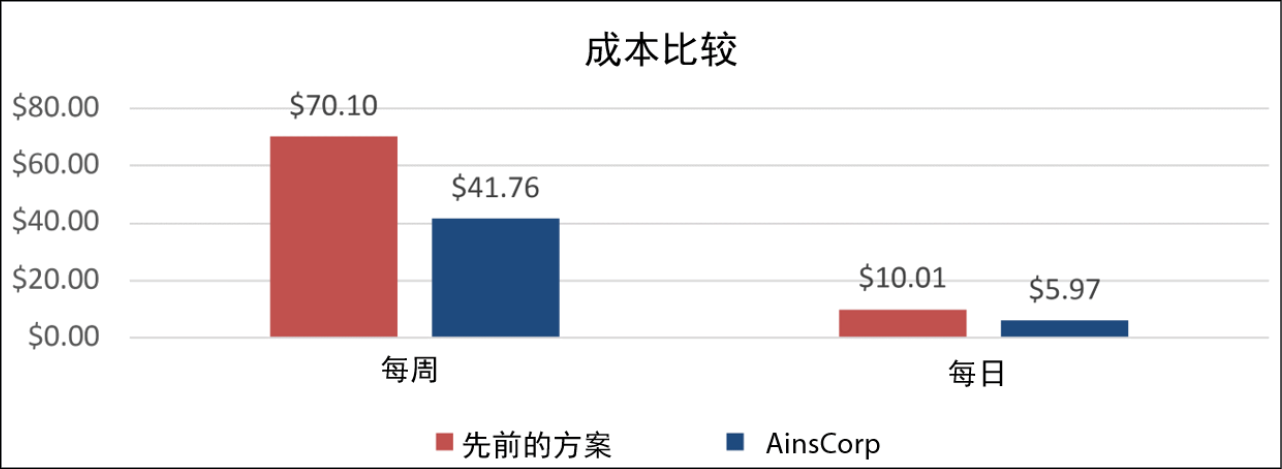
图6.病例1-标准治疗与HA+SSD联合治疗每周和每天的成本比较
病例2
患者ML是一例84岁男性患者,在2007年接受了回肠通道术。患者的回肠通道术情况良好,造口周围皮肤在手术后十分健康,并且11年来从未接受过造口治疗师的复查。2021年6月,该患者因造口周围溃疡和皮肤丢失前往造口治疗门诊就诊。溃疡面积为20 mmÅ~40 mm,从造口边缘12点钟方向延伸至7点钟方向。溃疡疼痛难忍,基底腐烂,有少量浆液性渗出液,未出现水肿或异味。
管理和结局
2021年6月16日开始接受的治疗(图7)包括每两周使用一次皮质类固醇软膏、含银抗菌屏障敷料以及一大一小两块水胶体造口密封件。根据患者的偏好以及在造口装置渗漏时更换敷料,更换频率从每日一次到每周一次不等。
治疗6周后(图8),溃疡愈合并停止治疗;然而,溃疡5点钟至7点钟方向部分的新生肉芽组织似乎非常脆弱。10月8日,患者再次就诊,溃疡再次破溃(图9)。伤口面积为10 mmÅ~5 mm,基底腐烂苍白,伤口边缘浸渍,有少量渗出液,无疼痛、无水肿、无异味。在这一阶段,患者恢复了最初的治疗方案,即每两周使用一次皮质类固醇软膏、含银抗菌屏障敷料和水胶体造口密封件。每2-3天更换一次敷料,同时更换造口装置。
1周后(图10),伤口不断増大(10 mmÅ~20 mm),于是停止了初始治疗,开始使用含0.2% HA和1% SSD的乳霜(HA+SSD)进行治疗。每两天接受一次治疗,同时根据患者的偏好更换造口装置。
使用HA+SSD乳霜治疗后,伤口面积不断缩小,最终愈合。初始治疗两周后(图11),伤口从10 mmÅ~20 mm缩小至5 mmÅ~5 mm。伤口边缘有粉色肉芽组织、少量浆液性渗出液和一些浸渍。未出现疼痛、水肿或异味。治疗六周后(图12),伤口已愈合,并持续保持愈合状态。
标准治疗与HA+SSD联合治疗的成本存在显著差异(图13)。HA+SSD联合治疗每次更换的敷料减少了50%以上,总共只使用了25%的管。
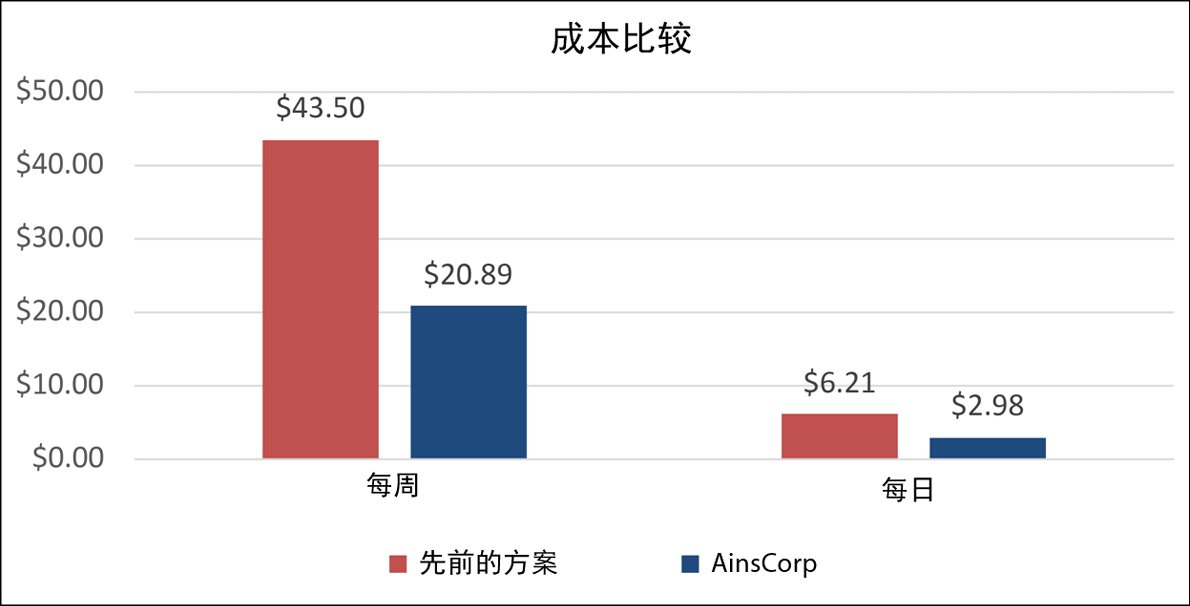
图13.病例2-标准治疗与HA+SSD联合治疗每周和每天的成本比较
讨论
这两例患者均出现了病因不明的造口旁溃疡,经标准治疗后仍不见缓解。在使用0.2% HA和1% SSD(HA+SSD)复方乳霜治疗后,溃疡成功得到管理并愈合。用Q型吸头在溃疡处直接涂上一层薄薄的豌豆大小的复方乳霜,无需辅助敷料,造口装置放置在最上方。在基底板下涂抹乳霜不会影响水胶体的粘附性,两例患者均表示在按计划更换造口袋之前未出现渗漏或基底板抬起的情况。这种治疗方法有助于患者从造口治疗诊所中出院,并且这两处溃疡此后一直保持愈合状态。
结论
与HA+SSD联合治疗相比,标准治疗的成本显著降低。病例1的标准治疗成本是联合治疗成本的1.68倍,病例2的标准治疗成本是联合治疗成本的2.08倍。此外,这两例患者的标准治疗均失败,治疗数周后伤口仍未愈合,而联合治疗的成本是按伤口愈合时间计算的。与造口旁溃疡标准治疗方法相比,HA+SSD复方乳霜的成本存在显著差异(未考虑GP对康纳乐®处方的额外审查),这表明它可能是一种成本较低的有效干预措施,可在首次出现造口旁溃疡时使用。
致谢
患者同意在本病例研究中使用他们的信息。照片均在征得患者口头和书面同意后进行拍摄。
利益冲突声明
作者声明无利益冲突。
资助
作者未因该项研究收到任何资助。
Author(s)
Alison Carlin
Grad Cert Stomal Therapy Nursing
Stomal Therapy CNC
Knox Private Hospital, VIC, Australia
Email alison.carlin@healthscope.com.au
References
- Norman T, Haesler E, Carville K, et al. Establishing a consensus on stomal, parastomal and peristomal complications. J Stomal Therapy Aust 2022;42(2):10–19.
- Nichols TR, Riemer M. Body image perception, the stoma peristomal skin condition. Gastrointest Nurs 2011;9(1):22–26.
- Antonini M, Arena R, Mancini S, et al. Peristomal skin changes: what treatment should be adopted? Results of an observational multi-centre study. WCET J 2018;38(1):30–34.
- Taneja C, Netsch D, Rolstad BS, et al. Clinical and economic burden of peristomal skin complications in patients with recent ostomies. J Wound Ostomy Cont Nurs 2017;44(4):350–357.
- Herlufsen P, Olsen AG, Carlsen B et al. Study of peristomal skin disorders in patients with permanent stomas. J Wound Ostomy Cont Nurs 2013;40(4):400–6.
- Yeo H, Abir F, Longo WE. Management of parastomal ulcers. World J Gastroenterol 2006;12(20):3133–7.
- Chen CP, Hung W, Lin SH. Effectiveness of hyaluronic acid for treating diabetic foot: a systematic review and meta-analysis. Dermatol Ther 2014;27(6):331–6.
- Voigt J, Driver VR. Hyaluronic acid derivatives and their healing effect on burns, epithelial surgical wounds, and chronic wounds: a systematic review and meta-analysis of randomized controlled trials. Wound Repair Regen 2012;20(3):317–31.
- Farris A, Prosdocimi M, Bevilacqua C. Association of hyaluronic acid and silver sulphurdiazine for topical use: rational basis and recent clinical evidence in wound healing. Farmaci 2010;9(6):1–7.
- Costagliola M, Agrosi M. Second degree burns: a comparative, multicentre, randomized trial of hyaluronic acid plus silver sulfadiazine alone. Curr Med Res Opin 2005;21(8):1235–40.
- Soma PF, Stella M, Comitini S. Role of a HA based hyaluronic acid in re-epithelisation: a clinical model. 37th National Meeting of the Italian Society of Plastic, Reconstructive, and Aesthetic Surgery, 1988.
- Torregrossa F, Caroti A. Clinical trial of the topical use of hyaluronic acid-soaked gauzes in the treatment of sluggish ulcers. Giorn It Derm Vener 1983;118.


