Ahead of Print
Adjustable Velcro® compression devices as compared to 4-layer compression bandages for the treatment of venous leg ulcers and optimisation of patient satisfaction
Sharon L Boxall, Keryln Carville, Joanna Smith, Shirley Jansen
Keywords venous leg ulcers, compression, compression wraps, adjustable Velcro® compression devices, 4-layer compression bandaging
For referencing Boxall SL, et al. Adjustable Velcro® compression devices as compared to 4-layer compression bandages for the treatment of venous leg ulcers and optimisation of patient satisfaction. Wound Practice and Research. 2024;32(2):To be assigned.
DOI
10.33235/wpr.32.2.To be assigned
Submitted 21 December 2023
Accepted 18 March 2024
Abstract
Aims To compare the efficacy, cost effectiveness and user satisfaction achieved when 4-layer compression bandages (4LCB) and adjustable Velcro® compression devices (AVCD) are used in the treatment of venous leg ulcers (VLU), in community dwelling adults.
Methods A prospective cross-over study was conducted. A convenience sample of 50 patients with VLUs were recruited. Patients were randomised to receive either 4LCB or AVCD for a period of 6 weeks, then crossed to the alternative treatment for an additional 6 weeks. Baseline and weekly wound assessments were recorded. Patients and nurses completed satisfaction surveys at the end of each arm. A cost analysis was completed.
Results Patients experienced a comparable reduction in ulcer size with both compression modalities.
Nurses and patients reported higher satisfaction with AVCD. The costs associated with a reusable AVCD as compared to single use 4LCB was dependent on the duration of treatment and frequency of changes. Cost benefits were associated with AVCD after 17 episodes of care where a single set of bandages was required and sooner in larger legs.
Conclusions The use of AVCD proved cost-effective and produced comparable healing rates in the community setting. Both nurses and patients expressed higher satisfaction scores when using AVCD.
Venous leg ulcers (VLU) are one of the most frequently encountered chronic wounds.1 Recent data produced by the largest community nursing service in Australia found VLUs comprise the greatest proportion of wounds and subsequently generate the highest aggregate treatment costs.2 Estimates of annual treatment costs for VLUs in Australia was estimated to be approximately A$1178 million.3
Patients with VLUs suffer pain, impaired mobility and impaired quality of life.4 Estimates of prevalence vary from 3% of people 60 years-and-over,5 to 5% among those 80 years-and-over.6 Gould, Abadir7 reported an increased incidence of three to four times in those over 80 years of age compared to those aged 65 to 70 years. These estimates may under-represent the true extent of the problem as they fail to account for those who self-manage their VLUs, a cohort which may be as high as 75% in people of working age.8
In 2020, Australians aged 65 years-and-over represented 16.3% of the population and those aged over 85 years 2.4% (n=527,400) with the number expected to double by 2042.9.10 Hence the incidence, prevalence and associated fiscal burden of managing VLUs are expected to increase in coming decades, as will the significant detrimental effects on mobility, functioning and quality of life for those afflicted.
The pathophysiological aetiology associated with the development of a VLU is valvular incompetence of the lower leg veins. This leads to chronic venous insufficiency (CVI), venous hypertension, lower leg oedema and ultimately, ulceration.11 Graduated lower leg compression therapy is the recommended treatment for VLUs.12 It works by exerting external pressure on the veins which reduces venous hypertension and oedema and improves calf muscle pump performance.13
Compression therapy can be applied using a variety of modalities including single or multi-layer bandages, hosiery, pneumatic pumps, and Velcro® adjustable compression wraps.14 However, many patients find it difficult to tolerate compression bandaging due to discomfort, and constraints in performing hygiene and wearing of preferred clothing and footwear.4 Patient tolerance is also compounded by lack of engagement, lack of empowerment, poor health literacy, financial constraints, geographical isolation or psychosocial barriers that impact wellbeing and activities of daily living.4,14-17 The proposal that compression wraps offer an efficacious alternative to compression bandaging,18,19 had, prior to this study, not been tested in a comparative study involving a cohort of patients receiving community based wound care in Australia.
Methods
A prospective crossover study was undertaken. A convenience sample of 50 patients with CVI who were receiving treatment for VLUs by a community health provider in metropolitan Perth, Western Australia, were invited to participate. Patients were eligible for recruitment if they were: over 18 years of age, without cognitive impairment, could provide informed consent and were able to launder the AVCD and liners. Significant arterial insufficiency was excluded on clinical assessment and when the ankle brachial pressure index (ABPI) was 0.8−1.2 or absolute toe pressure was >55mmHg. Prior to recruitment, potential recruits who were receiving care for a VLU underwent a comprehensive clinical lower leg assessment by a specialised wound nurse, which included documentation of clinical signs commonly associated with CVI: oedema, haemosiderosis, lipodermatosclerosis and this was used in combination with ABPI or absolute toe pressure to confirm a diagnosis of CVI and the presence of a VLU.
Computer randomisation allocated each patient to receive either 6 weeks (or less if healed prior) in four-layer graduated compression bandages (4LCB), which comprised a natural padding, crepe, light stretch and cohesive bandage which were reported to achieve 40mmHg graduated compression at the ankle. The alternative randomisation allocated participants received 6 weeks (or less if healed prior) treatment in AVCD (Jobst® AVCD BSN medical Aust Pty Ltd, an Essity company) and these were applied according to the manufacturer’s instructions. Patients received their usual wound care: washing of the leg with potable water, application of moisturiser to surrounding skin, a primary dressing based on assessment of the wound bed conditions and amount of exudate and a secondary dressing if required.
Baseline and weekly wound assessment data and wound images were collected at point of care and uploaded on the organisation’s electronic mobile wound module. Data included: wound dimensions; wound bed, edge and peri-wound characteristics; exudate type, amount and odour; and wound pain (self-reported using a numerical scale out of 10).
A patient-specific care plan was developed in accordance with the assessment outcomes and goals of care, and randomisation to the treatment group. All treatment consumables (solutions, dressings, bandages, instruments, dressing packs) used to treat each patient were recorded automatically on selection of consumables in the electronic care plan.
A seven question, five-level Likert survey in paper format was administered to nurses at the end of each treatment period. There was also room for free text nurse comments. The patients completed a 14 question, five-level Likert satisfaction survey, also in paper format, at the end of each treatment period.
Descriptive statistics were used to explore patient demographics and the percentage of wounds achieving complete healing. Chi square tests were employed to identify differences in percent healing between groups and Kruskal Wallis testing to identify differences in wound area reduction between groups. Patient and nurse satisfaction surveys were analysed using descriptive statistics.
Results
Demographic characteristics and healing information is contained in Table 1. Patients who did not complete at least one arm of the study (n=6) were excluded from this analysis. Information is based the on the client’s initial treatment arm, so healing in the first 6 weeks is based on which group they were randomised to and in the second 6 weeks based on the same treatment type. The age of patients is calculated from the date of their entrance into the study. Table 1 shows that those patients who started in 4LCB were older, on average, but this difference was not statistically significant (t(42)=-1.6772; p= 0.1009). The majority of patients in the study were male (73%) and there was no difference in gender between those who started in AVCD and those who started with 4LCB (X2(1)= 1.038; p=0.293).
Table 1. Demographics and healing
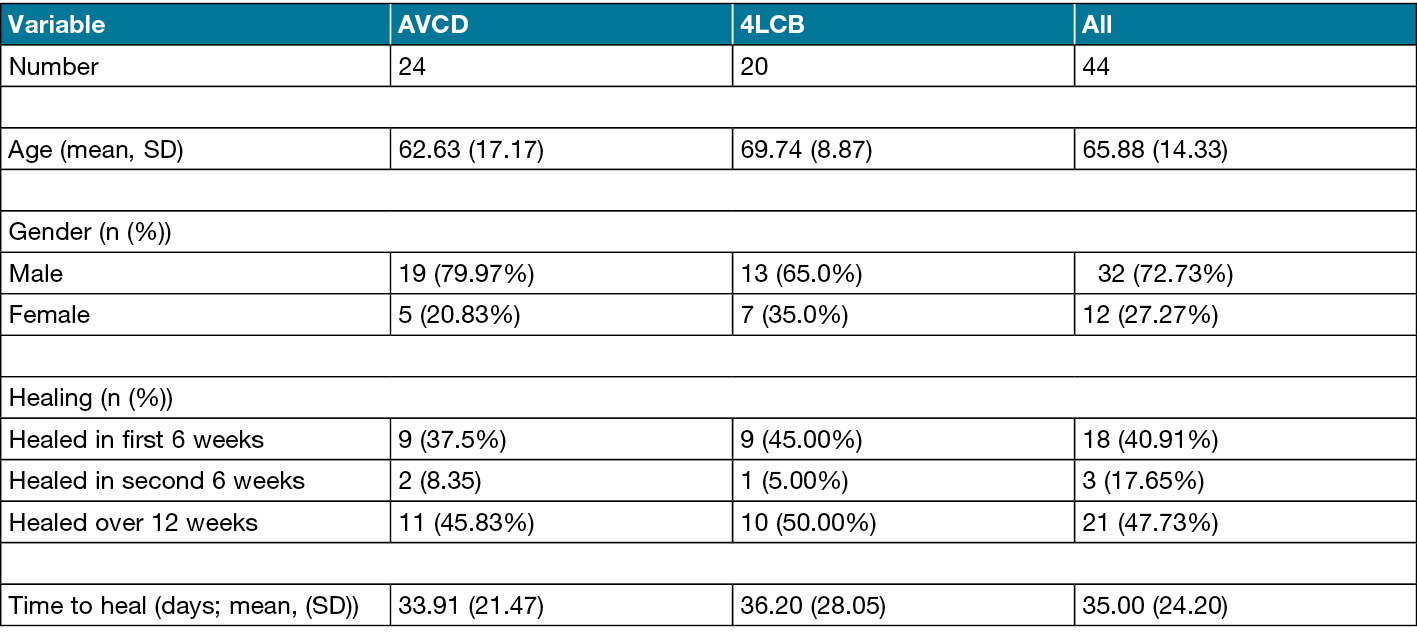
The mean ulcer size for patients starting in 4LCB was 2609mm2 (median 780; SD 5219; range 104−24,050; IQR 270−3480) and for those starting in AVCD, 7341mm2 (median 702; SD 15,100; range 12−57000; IQR 134−6194). Patients were reported as healed if they achieved complete epithelialisation of the wound during the study period.
Of all the patients in this study, 21 healed (48%), but significantly, of those who healed, 18 (86% of all healed) healed in the first 6-week period and there was no significant difference in the percentage healed (X2(1)= 0.2538; p=0.614) between treatment types. There were also no significant differences between the number of days to heal between treatment types. Both groups healed in around 35 days (t(19)=-0.2114; p=0.8348).
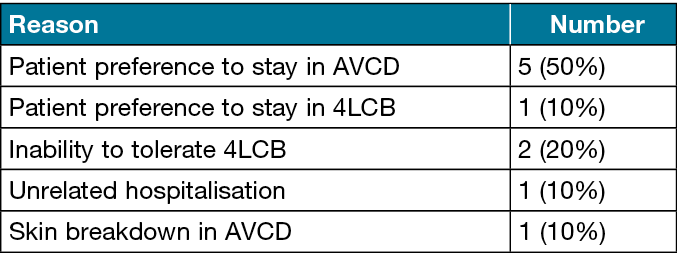
Ten patients chose to withdraw from the study. Of those who chose to withdraw, six did so because they wanted to continue using the AVCD, one left who wanted to continue using 4LCB, two withdrew as they could not tolerate 4LCB, one person had a skin reaction to the AVCD liner, one had skin breakdown due to cessation of a prior treatment of zinc paste bandaging (which was ceased prior to commencing the AVCD treatment), and another was hospitalised for an unrelated health matter (see Table 2).
Table 2. Reasons for early withdrawal from study.
A total of 34 patients spent some time in 4LCB. One patient was not able to tolerate 4LCB and removed it shortly after application. Their data was excluded. Two patients had multiple small wounds and the absolute change in wound size could not be calculated. One was swapped to AVCD too soon and their data was excluded. One was hospitalised for an unrelated matter. The remaining 28 patients were analysed for relative wound area reduction (RWAR) in 4LCB.
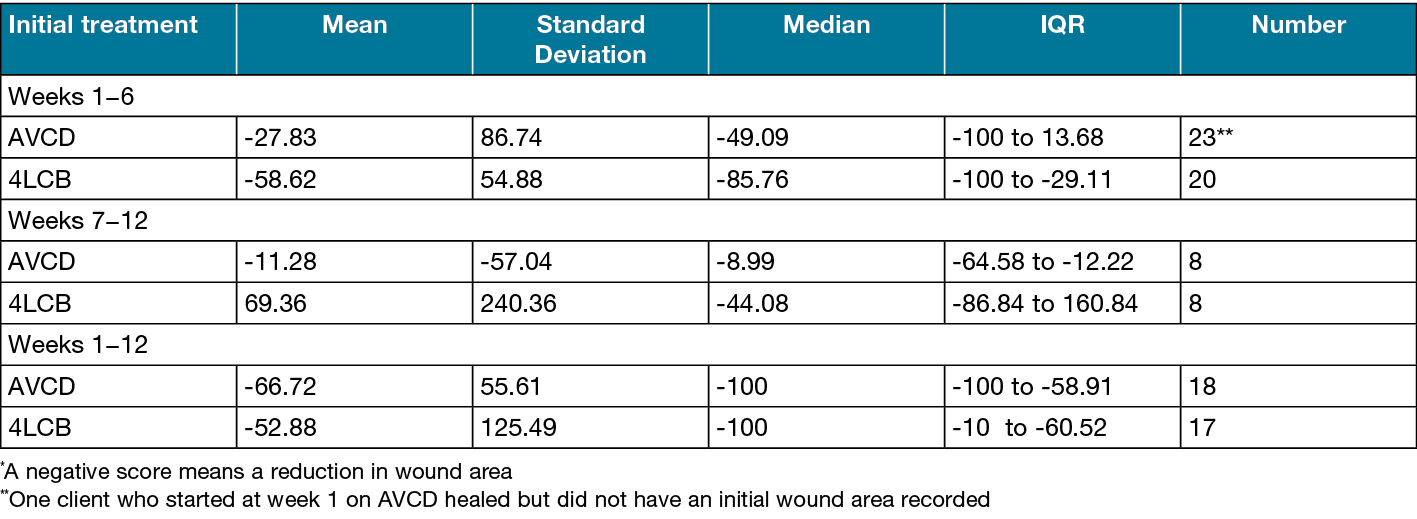
Among the 38 patients who were treated with AVCD, one patient did not tolerate the AVCD and reverted to 4LCB after two hours wear time, hence no change in wound size was identified. A second patient spent four days in AVCD and experienced a skin breakdown due to the cessation of his previous zinc paste bandaging and reverted to 4LCB. Three patients had multiple small wounds and the change in wound size could not be accurately calculated. One was swapped to AVCD too soon and their data was excluded. A single participant developed a dermatological skin disorder and wound size was not collected. The remaining 31 patients were analysed for RWAR in AVCD. RWAR is presented in Table 3.
Table 3. Relative wound area reduction*(%) by initial treatment
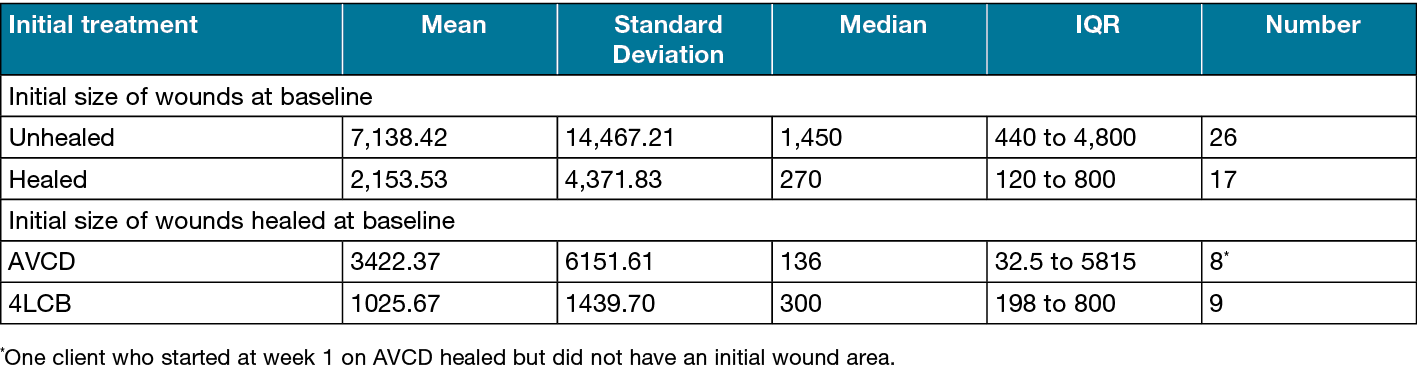
The median initial size of the clients’ wounds taken at baseline shows a significant difference between those that healed in the first 6 weeks and those that did not (H(1)=4.402; p=0.0381). The median size of those that healed was smaller than those that did not heal. There was no difference between the baseline size of the wounds that healed in the first 6 weeks and the initial treatment arm (Table 4).
Table 4. Initial size (mm2) of wound and healing within the first 6 weeks
Satisfaction survey results
The responses in the seven question, five-level Likert survey administered to nurses at the end of each treatment period were clustered into three categories: disagree, neutral and agree. The responses are presented in Figure 1. The greatest satisfaction differences between modalities occurred in responses around the ease of application and removal of the compression system and perceived occupational health and safety issues. Both favoured AVCD. Nurse self-reported application times were also collected in the survey tool. The mean application time for AVCD was 12 minutes (median 8; SD 10; range 5−40; IQR 21) and for 4LCB, 21 minutes (median 18; SD 16; range 5–60; IQR 21).
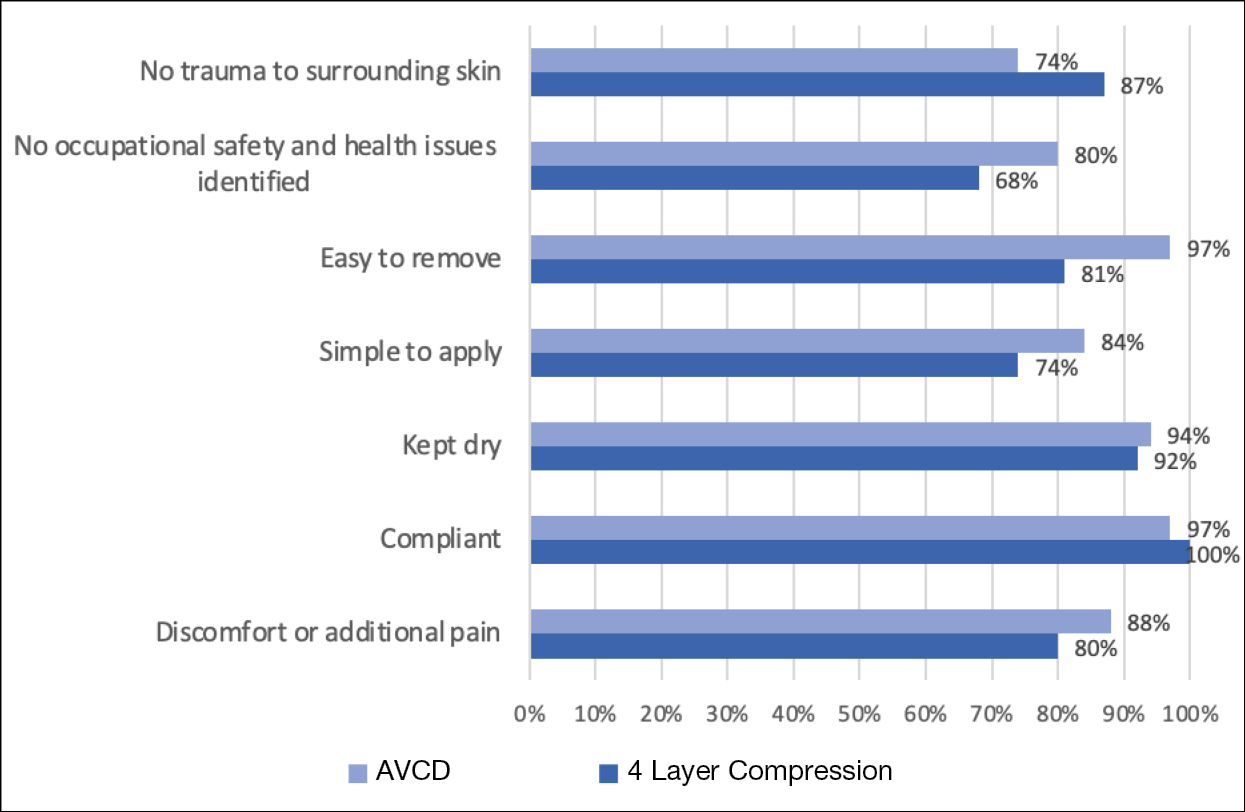
Figure 1. Nurse satisfaction: Percent of positive responses (%)
Patient satisfaction survey
The greatest differences found in patient satisfaction scores concerned the ease of attending self-hygiene and the wearing of footwear (Figure 2). Many patients found they could wear their usual shoes, which had associated benefits involving cost savings, improved cosmesis, more comfortable rest and ambulation and consequently a potential reduction in falls risk.
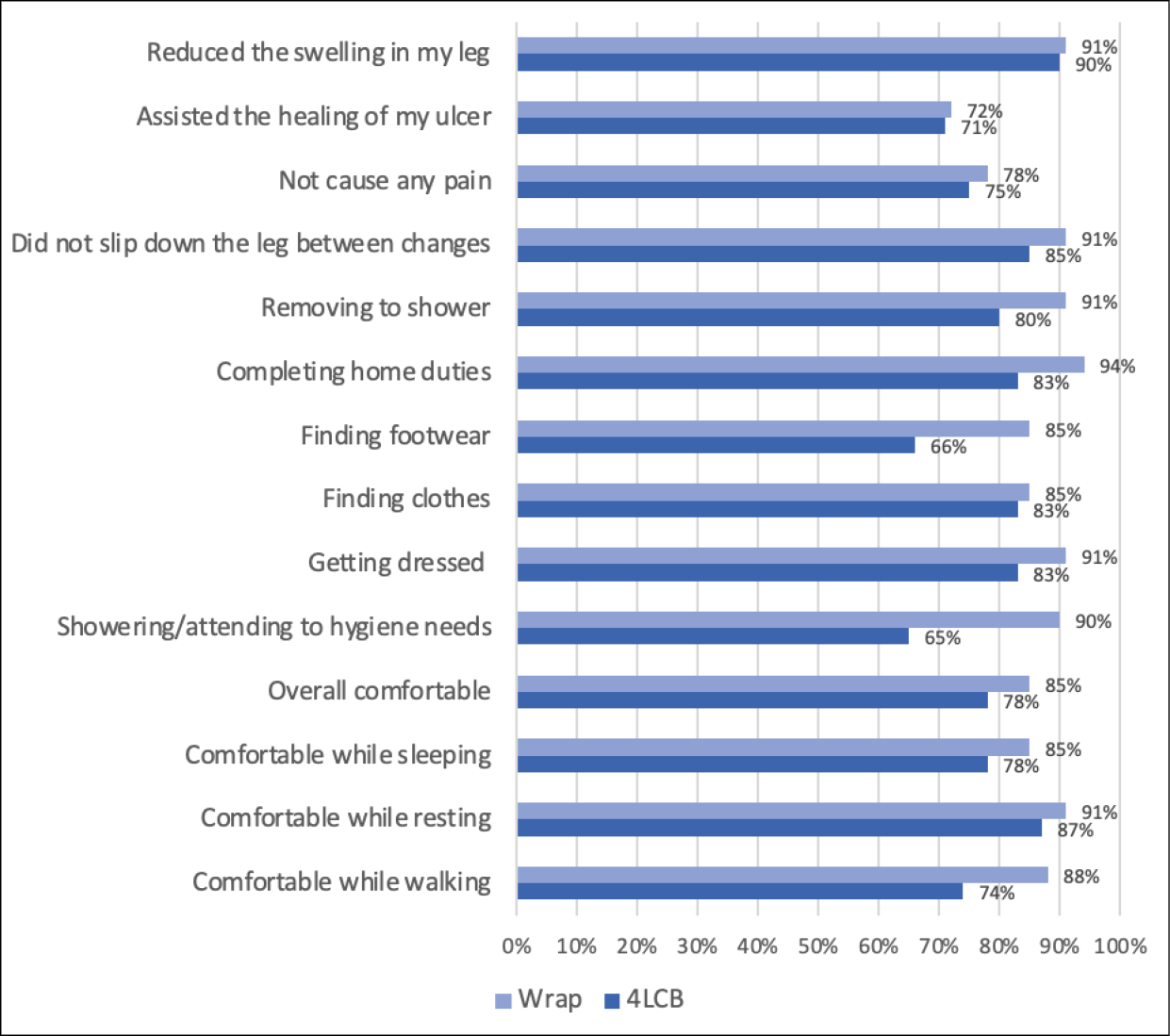
Figure 2. Client satisfaction: Percent of positive responses (%)
Costs to treat
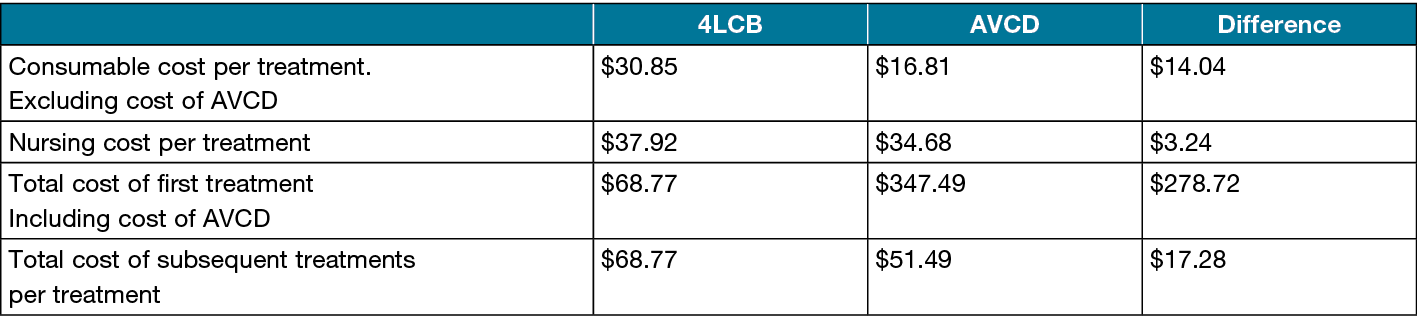
Consumable costs and nursing time were collected using the organisation’s wound module. Mean costs for each type of treatment were calculated and are presented in Table 5. The mean difference in cost to treat, after the first treatment which included the cost of the AVCDs, was A$17.28 per treatment in favour of the AVCD.
Table 5. Mean cost to treat, in Australian dollars: Consumables and nursing cost
Discussion
This study sought to compare the healing outcomes, costs and satisfaction scores associated with the use of 4LCB and AVCD in the community setting in Western Australia. A cross-over study was conducted on a convenience sample of 50 patients receiving compression therapy for the treatment of VLU. Results showed no significant differences between the two modalities with regard to wound healing, but higher satisfaction scores associated with the use of AVCD and cost savings with AVCD after 17 treatments.
In 2016, a similar cross-over pilot study was undertaken by the same community nursing organisation, which compared the use of AVCD to 4LCB in the treatment of VLU in community dwelling, bariatric patients. That study identified several advantages associated with the use of AVCD, including: increased nurse and patient satisfaction, increased patient concordance with treatment, reduced treatment costs and reduced injuries among nurses while demonstrating that the overall treatment outcomes were comparable.20,21 There is a high degree of agreement between the findings of the two studies with regard to wound healing, costs and satisfaction, indicating benefits are maintained across a range of body morphologies. While the later study did not specifically gather concordance data it did gather patient satisfaction scores which were higher for AVCD, and patient satisfaction with treatment does contribute to concordance.4
Patient satisfaction/concordance
Concordance with compression therapy is a principal driver for achieving optimal healing of VLUs. Higher participant satisfaction correlates with higher treatment concordance, better engagement with compression and consequently, potentially faster healing4,22,23 and in this study the participants reported higher levels of satisfaction when wearing AVCD as compared to the 4LCB. The satisfaction scores were higher for AVCD for all questions posed and, in particular, the wearing of AVCD was found to be more comfortable and less of an encumbrance while performing activities of daily living and personal care.
Participants reported it was easier to wear their usual footwear which provided benefits around increased mobility and social functioning. This has implications for enhancing mobility and reducing the risk of falls and a consequent reduction in the psychological impact of VLU treatment.16,24,25 Increased mobility and the coincidental increase in calf muscle pump function is one mechanism involved in the reduction of symptoms associated with VLU and chronic venous insufficiency,13,26 as it improves venous return and reduces lower leg oedema and associated discomfort. This subsequently improves healing outcomes and quality of life.13,27
Some of the study patients complained of toe pain when using the sock-like liner. One patient cut the toes out of his stockings to increase comfort. A potential product innovation could be to develop open toe compression liners or alternatively, use a class one open toe compression stocking and a lighter AVCD thus further enhancing patient satisfaction.
Early exits from study
The methodology describes a treatment protocol whereby patients continued in the study for 12 weeks or until they achieve completed healing, whichever occuredk sooner. A total of ten patients (20%) chose to exit the study prior to completion, five (50%) of whom left the study to continue in ACVD and one (10%) who left to stay in 4LCB. It is acknowledged that higher attrition rates may introduce bias into a study, however, as the results of this study indicate a patient preference for ACVD, the reasons for withdrawal lend additional support to the findings.
Cost effectiveness
The treatment of VLUs poses a significant resource burden on individuals and health care providers.3,28 This study demonstrated AVCD required less nursing time to apply than 4LCB and reduced consumable costs. Cost savings were demonstrated where participants required more than 17 episodes of care. The AVCD are reusable, hence the total cost of the devices is amortised over the duration of treatment. However, each patient required two devices to permit laundering between uses.
To complete the analysis of the relative costs of treatment it was necessary to ascertain the duration of treatments at which cost to treat with either compression modality equalised. This was calculated by dividing the difference in total cost per treatment including the cost of the AVCD by the difference in total cost per treatment excluding the cost of the AVCD. In this investigation cost equivalence was realised at 17 treatments when patients required one set of bandages per leg per treatment. Should a patient require two sets of bandages per leg per treatment (nominal cost A$12 each), such as may be expected when treating the morbidly obese with overlarge legs, cost equivalence would be realised at ten treatments. Every treatment after this point, until replacement of the AVCD is required saved A$17.28, a saving approaching 25% of the treatment cost. Given that it is estimated the cost of treating an individual VLU in Australia is A$8106,29 a cumulative A$1178 million per annum,3 the potential savings are not insignificant.
Treatment Outcomes
This study has provided data to support the non-inferiority of AVCD in the treatment of VLU compared to the ‘gold standard’: 4LCB. There was no significant difference in the number of participants who achieved complete healing with either modality or in the time they took to do so. It was of interest that of the 21 wounds which healed during the study, 18 did so in the first 6 weeks of treatment, perhaps supporting the premise that effective compression rather than compression modality is the primary driver of VLU healing.
The wounds that did heal within the study period were in general smaller than those that did not (median 270mm2; IQR 120–800mm2 vs median 1450mm2; IQR 440−4800mm2). Larger wounds frequently take longer to heal than smaller wounds,30 so this result is unsurprising. The length of this study was determined by research suggesting 2/3 (67%) of VLU heal within 12 weeks with effective compression therapy.31,32 However, in this study the percentage healing within the 12 weeks was only 21/50 or 42%. Many of the participants were recruited from an active client list and consequently may have had already had compression, but not yet achieved healing. This may have caused bias in that the cohort may have contained a higher-than-average percentage of slow to heal wounds. Additionally, those who were first treated with AVCD and left the study to stay in AVCD were not followed for a further 6 weeks. It is unknown if these five participants healed within 12 weeks or not.
Study limitations
Some study limitations were identified. Ulcer duration was not collected; hence it was not possible to quantify how many of the patients had intractable ulceration. Likewise, history of previous compression therapy by type or duration was not collected. The high proportion of healing in the first versus second 6 weeks of the study regardless of compression modality, may actually reflect a response to effective compression in general. The literature reports great variation between target and achieved compression bandaging pressures.33 It is possible that the enrolled patients had not received an appropriate level of compression prior to commencing the study. Additionally, we did not objectively collect application time, only self-reported. This introduced a potential confounder into the cost analysis.
There was a gender imbalance in the patient cohort. Venous leg ulcers are reported to affect more females than males,32,34,35 however, in this investigation 70% of participants were male. Although the community nursing service offers both clinic and in-home wound care, the majority of participants in this study were receiving treatment in wound clinics. This was a result of using a convenience sampling method. The gender imbalance in this investigation may reflect an increased willingness among males to try new therapies or alternatively, reflect barriers to clinic attendance among females. It is not known if there is a gender imbalance in VLU healing rates generally. Further exploration of this gender imbalance may assist in identification of barriers to the use of AVCD in females and provide opportunity to enhance concordance in males.
Opportunities for future research
This study generated several opportunities for further research. These include accurate data collection of application times for each compression modality by a range of clinicians. It is known that compression bandage pressures reduce over time36 but to the best of our knowledge no longitudinal study exists which examines the change over time of compression pressures beneath AVCD, particularly those subjected to home laundering. The development of a decision-making framework around compression modality rather than just compression pressure may facilitate the prescription of a compression modality best matched to the patients’ individual preferences and circumstances.
The patients in this study describe being able to find suitable footwear more easily when using AVCD compared to 4LCB. Choice of footwear can influence gait, bandaging can limit range of movement, and both can affect the function of the calf pump,37 which consequently drives venous return, reduces oedema and facilitates the healing of VLU. Examining the effect of compression modality on gait and ROM on specific patients could further inform the choice of the most appropriate and effective type of compression for each individual.
Conclusions
The AVCD has a role to play in the armamentarium of compression therapy and has cost, and acceptability advantages in the community setting. The application of 4LCB requires a trained clinician, however AVCD can be applied by carers and in many cases by patients themselves. 38,39 This improves access to compression therapy in rural and remote locations where access to health providers may be limited. Feelings of self-efficacy and empowerment are gained when patients can contribute to their own care16,40 and enhanced self-efficacy encourages concordance with treatment.14,41
Additionally, based on the research of Petrovska,20 the use of AVCD may reduce the occupational injury risk to those applying compression therapy in a non-clinical setting, such as the home care environment. The costs associated with worker injury have not been factored into the cost analysis performed for this study but cannot be ignored when examining the total cost burden associated with VLU treatment.
Further research to develop a decision-making framework around choice of compression therapy modality would maximise the opportunity to target compression type to an individual’s clinical and socio-economic situation, potentially enhancing patient concordance and optimising treatment outcomes.
Acknowledgements
The authors wish to acknowledge and thank BSN medical Aust Pty Ltd, an Essity company, for their unconditional research grant and in-kind donations of AVCD and liners that enabled the study to be conducted.
Conflict of interest
The authors declare no conflicts of interest.
Ethics statement
Ethics approval for this study was obtained from the Silver Chain Group Human The Silver Chain Group HREC (Ethics Application 130. Date: 1 April 2019).
Funding
An unconditional research grant and in-kind donation of AVCD and liners was received from BSN Medical Aust Pty Ltd, an Essity company.
Author contribution
Sharon Boxall was involved in the study design, collection, analysis and interpretation of data and drafting and revision of the paper. Keryln Carville was involved in the conception, design, analysis and interpretation of data and critical revision of the paper as well as the final approval of the version of the paper to be published. Joanna Smith was involved in the analysis and interpretation of the data and drafting of the paper. Shirley Jansen was involved in the conception, design, analysis and interpretation of data and critical revision of the paper as well as the final approval of the version of the paper to be published.
Author(s)
Sharon L Boxall*1,2,3 Keryln Carville1,2 Joanna Smith2 Shirley Jansen3,4,5
1Curtin University School of Nursing, Perth, Australia
2Silver Chain Group Limited (Silverchain), Perth, Australia
3Heart and Vascular Research Institute, Harry Perkins Institute of Medical Research, Perth, Australia
4Curtin Medical School, Curtin University, Perth, Australia
5Dept Vascular and Endovascular Surgery, Sir Charles Gairdner Hospital, Perth, Australia
*Corresponding author email Sharon.Boxall@curtin.edu.au
References
- Simon D, Dix F, McCollum C. Management of venous leg ulcers. BMJ. 2004; 328: 1358−1362.
- Silverchain Group. Comcare wound module data 2020−2021. Silverchain Group, 2021.
- Graves N, Zheng H. Modelling the direct health care costs of chronic wounds in Australia. Wound Pract Res. 2014; 22: 20−33.
- Boxall S, Carville K, Leslie G, Jansen S. Compression bandaging: Identification of factors contributing to non-concordance. Wound Pract Res. 2019; 27: 6-20. DOI: 10.33235/wpr.27.1.6-20
- Rayner R, Carville K, Keaton J, et al. Leg ulcers: Atypical presentations and associated comorbidities. Wound Pract Res. 2009; 17: 168−172, 174,176−178, 180−185.
- Brajesh K. Venous ulcers of the lower extremity: Definition, epidemiology, and economic and social burdens. Semin Vasc Surg. 2015; 28(1): 3−5.
- Gould L, Abadir P, Brem H, et al. Chronic wound repair and healing in older adults: Current status and future research. J American Geriatr Soc. 2015; 63:427−438.
- Firth E, Nelson E, Hale C, et al. A review of design and reporting issues in self-reported prevalence studies of leg ulceration. J Clin Epidemiol. 2010; 63: 907−913.
- Australian Bureau of Statistics. Population aged over 85 to double in the next 25 years [Internet]. Canberra: ABS; 2018 November 22 [cited 2024 May 8]. Available from: https://www.abs.gov.au/articles/population-aged-over-85-double-next-25-years.
- Australian Bureau of Statistics. Twenty years of population change [Internet]. Canberra: ABS; 2020 December 17 [cited 2024 May 8]. Available from: https://www.abs.gov.au/articles/twenty-years-population-change.
- Anderson I. Understanding chronic venous hypertension. Wound Essentials. 2008; 3.
- Australian Wound Management Association Inc & New Zealand Wound Care Society. Australian and New Zealand clinical practice guideline for prevention and management of venous leg ulcers. Osborne Park, W. Australia: Cambridge Publishing, 2011, p.132.
- Sarin S, Scurr JH, Smith PDC. Mechanism of action of external compression on venous function. Br J Surg. 1992; 79: 499−502. DOI: 10.1002/bjs.1800790608.
- Ritchie G, Freeman N. Understanding compression: Part 3 - compression hosiery stockings and adjustable compression wraps. Journal of Community Nursing. 2018; 32: 20−28.
- Van Hecke A, Grypdonck M, Defloor T. A review of why patients with leg ulcers do not adhere to treatment. Journal of Clinical Nursing 2009; 18: 337−349.
- Upton D, Upton P. Psychology of Wounds and Wound Care. Springer International Publishing, 2015.
- Todd M. Venous leg ulcers and the impact of compression bandaging. Br J Nurs. 2011; 20: 1360−1364.
- Damstra RJ, Partsch H. Prospective, randomized, controlled trial comparing the effectiveness of adjustable compression Velcro wraps versus inelastic multicomponent compression bandages in the initial treatment of leg lymphedema. J Vasc Surg Venous Lymphat Disord. 2013;1:13−19. DOI:10.1016/j.jvsv.2012.05.001.
- Mosti G, Cavezzi A, Partsch H, et al. Adjustable Velcro® compression devices are more effective than inelastic bandages in reducing venous edema in the initial treatment phase: a randomized controlled trial. Eur J Vasc Endovasc Surg. 2015; 50: 368−374. DOI: https://doi.org/10.1016/j.ejvs.2015.05.014.
- Petkovska G. Comparing the effectiveness of compression wraps against compression bandages in obese clients with venous leg ulcers. Report, Silver Chain Group, Perth, Australia, 2016.
- Petkovska G. Protocol development: Comparing compression wraps against compression bandages for management of bariatric clients with venous leg ulcers. J Nurse Pract. 2017; 13: e336-e336. DOI:10.1016/j.nurpra.2017.05.046.
- Anderson I. Encouraging compliance and concordance in leg ulcer patients. Wounds UK. 2012; 8: S6-S8.
- Greaves T, Ivins N, Stephens C. A compression bandage system that helps to promote patient wellbeing. Journal of Community Nursing. 2014; 28: 25−26,28−30.
- Vishwanath V. Quality of life: Venous leg ulcers. Indian Dermatol Online J. 2014;5(3):397−399.
- Green J, Jester R, McKinley R, Pooler A. The impact of chronic venous leg ulcers: a systematic review. J Wound Care. 2014; 23: 601−612. DOI: 10.12968/jowc.2014.23.12.601
- Caggiati A, de Maeseneer M, Cavezzi A, et al. Rehabilitation of patients with venous diseases of the lower limbs: State of the art. Phlebology. 2018;33(10):663-671. DOI:10.1177/0268355518754463.
- Recek C. Calf pump activity influencing venous hemodynamics in the lower extremity. Int J Angiol. 2013;22:23-30. DOI:10.1055/s-0033-1334092.
- Ma H, O’Donnell T, Rosen N, Iafrati M. The real cost of treating venous ulcers in a contemporary vascular practice. J Vasc Surg Venous Lymphat Disord. 2014;2:355−361. DOI:10.1016/j.jvsv.2014.04.006.
- Jepson T, O’Hara T, Monaro S. Case study: Collaboration across the care continuum to improve the patient experience. Wound Pract Res. 2018;26:182−187.
- Margolis DJ, Berlin JA and Strom BL. Which venous leg ulcers will heal with limb compression bandages? Am J Med 2000;109:15−19. DOI:10.1016/S0002-9343(00)00379-X.
- Kieser D, Roake J, Hammond C and Lewis D. Negative pressure wound therapy as an adjunct to compression for healing chronic venous ulcers. J Wound Care. 2011; 20: 35-37.
- Raffetto JD, Ligi D, Maniscalco R, et al. Why venous leg ulcers have difficulty healing: Overview on pathophysiology, clinical consequences, and treatment. J Clin Med. 2021;10:1−33. DOI:10.3390/jcm10010029.
- Boxall S, Carville K, Leslie G, Jansen S. Controlling compression bandaging pressure in leg ulcer research trials: A summary of the literature. Phlebology. 2019;34:501−514. DOI:10.1177/0268355519825590.
- Agale SV. Chronic leg ulcers: Epidemiology, aetiopathogenesis, and management. Ulcers 2013; 2013.
- Atkin L. Venous leg ulcer prevention 1: Identifying patients who are at risk. Nursing Times. 2019; 115: 24−28.
- Howse E. Determining the effectiveness of inelastic short stretch bandages in sustaining sub-bandage graduated compression. Thesis (M.Phil.). Curtin University, 2011.
- Shiman MI, Pieper B, Templin TN, et al. Venous ulcers: A reappraisal analyzing the effects of neuropathy, muscle involvement, and range of motion upon gait and calf muscle function. Wound Repair Regen. 2009;17:147−152. DOI:10.1111/j.1524-475X.2009.00468.x.
- Partsch H. Reliable self-application of short stretch leg compression: Pressure measurements under self-applied, adjustable compression wraps. Phlebology. 2018;34(3):208-213. DOI: 10.1177/0268355518793467.
- Cox A, Bousfield C. Velcro compression wraps as an alternative form of compression therapy for venous leg ulcers: a review. Br J Community Nurs. 2021;26:S10-S20. DOI:10.12968/bjcn.2021.26.Sup6.S10.
- Bainbridge P. Why don’t patients adhere to compression therapy? Br J Community Nurs. 2013;18:S35-S40. DOI:10.12968/bjcn.2013.18.Sup12.S35.
- Barnes H. To explore the factors that impact on patient concordance with venous leg ulcer management using compression therapy. Br J Community Nurs. 2023;28:S8-S18. DOI:10.12968/bjcn.2023.28.Sup3.S8.



