Volume 25 Number 1
A randomised controlled trial to evaluate the incremental effectiveness of a prophylactic dressing and fatty acids oil in the prevention of pressure injuries
Fazila Aloweni, Lim Mei Ling, Chua Tse Lert, Tan Siok Bee, Lian Siew Bee and Ang Shin Yuh
Keywords prevention, pressure injury, fatty acid oil, multi-layer dressing.
Abstract
Background: Pressure injuries lead to lower quality of life and incur substantial health care resources and costs. Pressure injury prevention is reported to be much cheaper than treatment of the condition itself.
Aim: To evaluate the incremental effectiveness of silicone foam dressing and fatty acids oil spray, in addition to standard care, in preventing sacral pressure injuries among high-risk patients.
Method: A randomised controlled trial (RCT) was conducted. Using simple random sampling, patients were allocated into one of the three groups: (1) Silicone foam dressing plus standard care; (2) fatty acids oil spray plus standard care; (3) standard care only.
Results: Four hundred and sixty-one patients were recruited. Of these, 3.9% (n=5) developed pressure injuries in the silicone foam dressing group, 5.4% (n=7) developed pressure injuries in the fatty acids oil group and 5% (n=10) developed pressure injuries in the standard care group. The difference was not statistically significant. However, significant statistical differences were found between the silicone foam dressing and standard care group (p=0.04) and between the fatty acids oil and standard care group (p=0.048) for patients with Braden score ≤12.
Conclusion: Additional preventive measures seem to be clinically beneficial in reducing sacral pressure injuries among very high-risk patients in the general ward acute care setting.
Introduction
A pressure injury is defined as a localised injury to the skin and/or underlying tissue usually over a bony prominence, as a result of pressure, or pressure in combination with shear and/or friction1. Hospital-acquired pressure injuries (HAPIs) are considered preventable2 and their occurrence is widely recognised as an indicator of sub-optimal nursing care. Pressure injuries stage III and IV that are acquired after admission to a health care facility are now classified as ‘Never Events’ or serious adverse events that are preventable3.
Pressure injuries are a significant cause of morbidity and significantly lower the quality of life for both patients and their carergivers4. Additionally, pressure injuries incur substantial health care resources and costs. In the United States healthcare system, the average cost of a pressure injury has been estimated to be between US$37,000 and US$70,000 (A$49,000 and A$93,000) per patient5. It is expected that the cost increases with injury severity, as the more extensive injury requires longer time to heal and is associated with a higher incidence of complications; therefore more health care resources are needed to care for this group of patients6.
Prevention of pressure injuries was reported to be much cheaper than treating the condition itself6. Pressure injury preventive interventions typically focus on risk assessment, reducing pressure and minimising shear and friction1. In recent years, additional prevention strategies were introduced to prevent the development of pressure injuries, such as the application of a multi-layer foam dressing and application of hyperoxygenated fatty acids oil over high-risk areas. However, most of the studies were done in temperate countries, among a largely Caucasian population and on critically ill patients. Given potential inherent differences among different ethnic skin types7, as well as the adverse impact of higher ambient temperature on skin tolerance to pressure injuries8, it is of interest to evaluate the effectiveness of these additional prevention strategies in a South East Asian country like Singapore.
Literature review
The sacrum is identified as one of the most common anatomical pressure injury sites for hospitalised patients9; with a reported prevalence rate as high as 13.6% among critically ill adults over a 35-month period10.
Effectiveness of prophylactic dressings
Recent studies have investigated the effectiveness of prophylactic multi-layer foam dressings in the prevention of pressure injuries over the sacrum. According to an in vitro study, the mechanisms of such a dressing are through moisture control (absorption of moisture caused by perspiration within the gluteal folds), reducing friction by separating skin folds, and alleviating local shear forces by creating an interface between the patient’s skin and the bed surface11,12. Most of the studies thus far were carried out among critically ill adults or adults at high risk of pressure injuries. All studies have demonstrated a positive reduction in the incidence of pressure injuries (Table 1a).
Table 1a: Summary of literature on effectiveness of prophylactic dressing
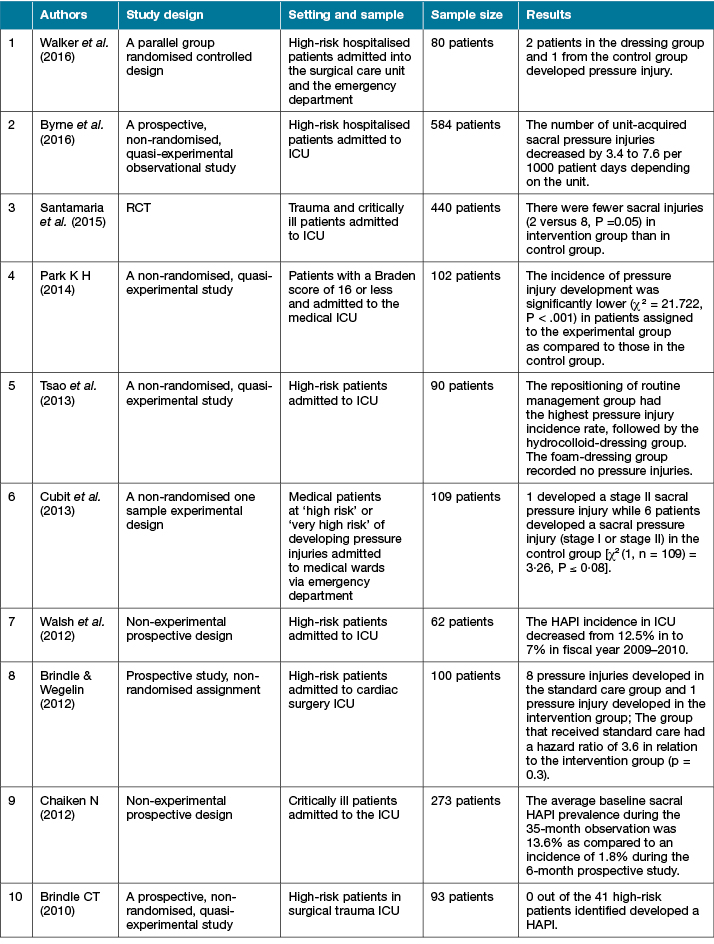
In a quality improvement study, it was concluded that the application of a silicone foam dressing over the sacrum, in addition to the adoption of prevention guidelines, reduced the incidences of HAPIs in an intensive care unit (ICU), from 12.5% to 7%13. In another similar quality improvement study, no high-risk patients developed HAPI while the sacrum dressing was in place14. Besides quality improvement studies, non-randomised, experimental studies10,15-18 were also conducted and positive effects of the prophylactic dressings were highlighted. However, these studies were limited by the lack of randomisation and had utilised a less rigorous study design. In a more recent randomised controlled trial (RCT)19 conducted on 440 ICU patients in Australia, a multilayered soft silicone foam dressing was reported to be effective in preventing pressure injuries among critically ill patients. There were significantly fewer sacral pressure injuries in the intervention group than in the control group (2 versus 8, p =0·05). However, similar to previous studies, the results were specific to critically ill patients in the ICU and little is known about the effects of prophylactic dressings on patients in the general acute ward settings. On the contrary, Brindle and Wegelin20 reported no statistically significant difference in hazard ratio between cardiac patients on a silicone border foam dressing and standard care and patients on standard care only. However, the trial was limited to patients who had undergone cardiac surgery and patients were not randomly allocated to the two groups. In addition, they only enrolled high-risk patients who had a surgical operation of more than six hours, had cardiac arrest, were on vasopressors, and there was no indication of any pressure injury risk assessment tool used.
Effectiveness of prophylactic fatty acid oil
It was suggested that fatty acid oil helps to lubricate the skin and reduce the shearing and frictional forces that contribute to pressure injury development21. Maintaining skin with adequate hydration and elasticity is vital to prevent the loss of skin integrity. Essential fatty acids (EFAs), specifically linoleic and linolenic acids, are said to play a vital role in maintaining the moisture barrier function of the skin (for example, preventing water loss and skin dehydration)22.
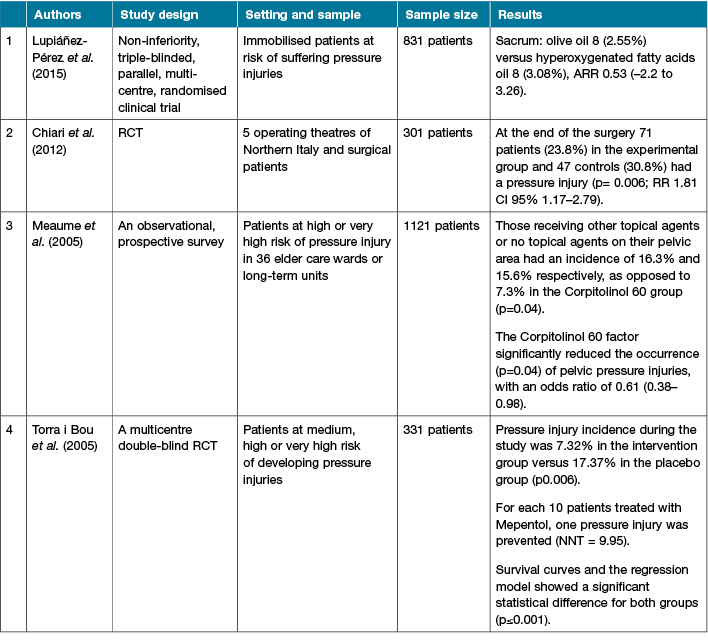
In a double-blind RCT, the authors concluded that topical application of essential fatty acids improved hydration and elasticity and helped prevent skin breakdown among patients with poor nutritional status who were fed orally with a high-protein diet and/or received parenteral nutrition23. In another RCT, researchers compared the effects of Mepentol, a hyperoxygenated fatty acid preparation, with a placebo treatment in the prevention of pressure injuries, and results showed significantly lower incidence of pressure injuries in the intervention group compared to placebo group (7.32% versus 17.37%; p = 0.006)24.
Likewise, in a more recent RCT, researchers investigated the effectiveness of Corpitolinol 60 (Sanyrène®) in the prevention of pressure injuries among surgical patients and found a significant difference between the experimental and control groups (p=0.006; relative risk (RR) 1.81, 95% confidence interval (CI) 1.17–2.79) at the end of the surgery25. In another similar study on Sanyrène, the authors concluded that the use of Sanyrène in addition with standard prevention strategies significantly reduced the incidence of pelvic pressure injuries (p=0.04). However, this study was sponsored by the manufacturer of Sanyrène and there was no control group26.
To date, there are limited studies on the effectiveness of fatty acids oil in the prevention of pressure injuries and the available studies were mainly from Europe (Table 1b).
Table 1b: Summary of literature on effectiveness of fatty acids oil
Despite the availability of many prevention modalities for pressure injuries, there is limited consensus on the best interventions and a paucity of rigorous RCTs available to recommend practice guidelines. Most of the pressure injury prevention trials were done in the temperate countries and on critically ill patients in the ICU setting. There is limited evidence on the effectiveness of prophylactic dressings and/or fatty acid oil on patients in the general acute ward setting and there was no published trial on the Asian population with different skin tones.
Singapore is a tropical country which lies near to the equator and has an average daily temperature of 31º Celsius and humidity of 96% to 64%27. Some patients nursed in the general wards are not in an air-conditioned environment as opposed to the ICU setting. High humidity has been associated with increased risk of pressure injury development8,28. To the best of the authors’ knowledge, this is the first study done in an Asian context with a significantly different climate.
Aim
To determine the incremental effectiveness of a prophylactic silicone foam dressing and tropical application of fatty acids oil, in addition to standard preventive measures, in reducing the incidence of sacral pressure injury among high-risk hospitalised patients in the general ward care setting in Singapore.
Methodology
Design
An RCT was conducted.
Setting
This study was conducted at an academic acute tertiary care hospital in Singapore. Patients were recruited from eight medical-surgical wards during the period of January 2014 to February 2016.
Ethical consideration
This study was approved by SingHealth centralised institutional review board (CIRB ref no: 2013/477/A) and was exempted from full written informed consent as the intervention was considered part of daily routine nursing care.
Sample size
Sample size calculation showed that to detect a decrease in the pressure injury incidence rate of 10% (from 15% to 5%) in the intervention group with power set at 70% and alpha of 0.05, a total of 494 patients would be needed.
Participants
All adult patients who met the following inclusion criteria were recruited within 48 hours upon admission into the hospital:
- ≥21 years of age (the study venue was an adult-focused health facility).
- Without pre-existing pressure injuries.
- Assessed as being at high risk of developing pressure injuries (scoring less than or equal to 14 using the Braden Scale).
Exclusion criteria included:
- Existing sacral pressure injury.
- Allergy to fatty acids oil or silicone dressing.
- Faecal incontinence at the time of hospital admission.
All patients who were admitted to the participating wards were screened for eligibility every 48 hours by a research coordinator. Routine pressure injury risk assessment using the Braden Scale was done by the nursing staff in the ward upon admission and thereafter, as per hospital policy. All registered and enrolled nurses at the participating wards were required to undertake annual pressure injury assessment training and were competent to perform Braden Scale assessment.
The Braden Scale is a tool used to assess the pressure injury risk of patients upon admission to the hospital. It is a commonly used tool and has been validated in other studies29,30. The Braden Scale included the following variables: activity, mobility, nutritional status, sensory perception, moisture, and friction and shear. All variables were rated on a rating of 1 to 4 except for shear and friction, which was rated from 1 to 3. A higher score corresponds with a lower risk of developing pressure injuries. In this study, patients with a braden score of 14 and below were considered as “high risk” of developing pressure injury.
Using a computer-generated table of simple random sampling (ratio 1:1:2), patients were allocated into one of the three treatment arms: (1) silicone foam dressing plus standard care; (2) fatty acids oil spray plus standard care; (3) standard care only. The allocation list was performed by a research coordinator who was not involved in the study. Opaque sealed envelopes were used to maintain allocation concealment. The allocation assignment was only made known to the ward nurses after patients were successfully enrolled in the study. Patients were followed up every three days until 14 days of the hospitalisation for any presence of pressure injury. End point data collection was when a pressure injury developed or when the patient was discharged to home or another institute (if earlier than 14 days).
Treatment groups
All groups received the standard care which consisted of the following interventions:
- Repositioning of patients every two to three hours when in bed.
- Use of positioning devices such as wedges to support patients with limited mobility.
- Use of an alternating air mattress to reduce interface pressure.
- Use of slide sheets to move patients while in bed to minimise shearing force.
- Frequent elimination rounds and diaper change to manage incontinence.
- Standard skin care such as applying barrier cream when the patients are on a diaper or applying emollient cream if patients have dry sacral skin (except for those on fatty acids oil).
Silicone foam dressing plus standard care received Mepilex Border Sacrum™, which was applied to the sacrum. The ward nurses were taught how to apply the dressing by a wound nurse specialist and the dressing was changed every seven days or when soiled.
Fatty acids oil plus standard care received Linovera oil®, which consists of hyperoxygenated essential fatty acids (sunflower seed oil), aloe vera and centella asiática extracts, that was applied to the patients’ sacrum three times daily. The ward nurses were trained to only apply a thin layer of the oil on the sacrum region.
Outcome assessment
The participants’ sacra were assessed at least once a day and the conditions were documented by the registered nurses who cared for the patient as per hospital standard practice guidelines. A study investigator also assessed patients’ sacra every three days until the patients were discharged, or for a maximum period of two weeks of their hospitalisation period. As classified by the National Pressure Ulcer Advisory Panel (NPUAP) and European Pressure Ulcer Advisory Panel (EPUAP)1, any stage I pressure injuries (skin intact, non-blanchable redness) were reported as an incident. Patients who developed diarrhoea or sensitivity reactions to the dressing material or the fatty acids oil during the study period were considered as dropped out.
Data analysis
An intention-to-treat (ITT) analysis approach was adopted to include all participants who were recruited and randomised in this study regardless of protocol violations. ITT analysis provides an unbiased estimate of the treatment effect and reflects the practical clinical scenario31. Descriptive statistics were used to describe the characteristics of the participants. Chi-square tests were used to evaluate differences in demographic variables and incidence of pressure injuries among the three treatment groups.
Participants were also categorised according to their Braden score, and Fisher’s exact test with a two-sided significance level of 0.05 was used to evaluate statistical significance of the incidence of pressure injuries within each sub-group.
Results
Demographics
A total of 461 patients were recruited. Patient enrolment, allocation, follow-up and analysis flow through the trial is presented in Figure 1 according to the CONSORT flow diagram32. The groups were comparable on all major physiological and demographic characteristics upon admission (Table 2). Out of the 461 patients recruited, a total of 64 patients did not complete the study due to various reasons (Table 3). The mean length of stay of the patients was 6.7 days (SD ±4.3 days).
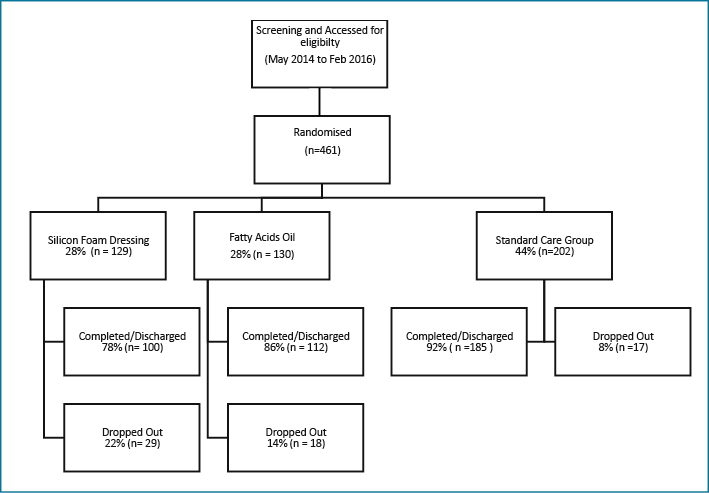
Figure 1: Consort diagram of patient flow through the study
Pressure injury incidence rate
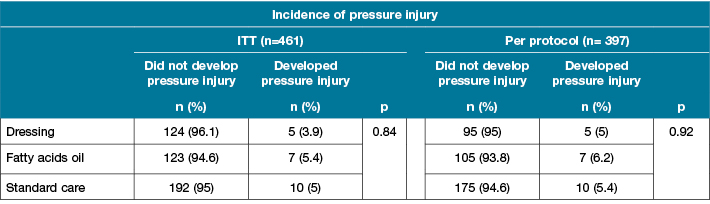
Table 4 presents the number of patients who developed a pressure injury and the incidence rate per group. Of the patients, 3.9% (n=5) in the silicone dressing group developed pressure injuries, as compared to 5.4% (n=7) of the patients in the fatty acids oil spray group and 5% (n=10) of the patients in the standard care group. The difference was not statistically significant.
Table 2: Patient demographics
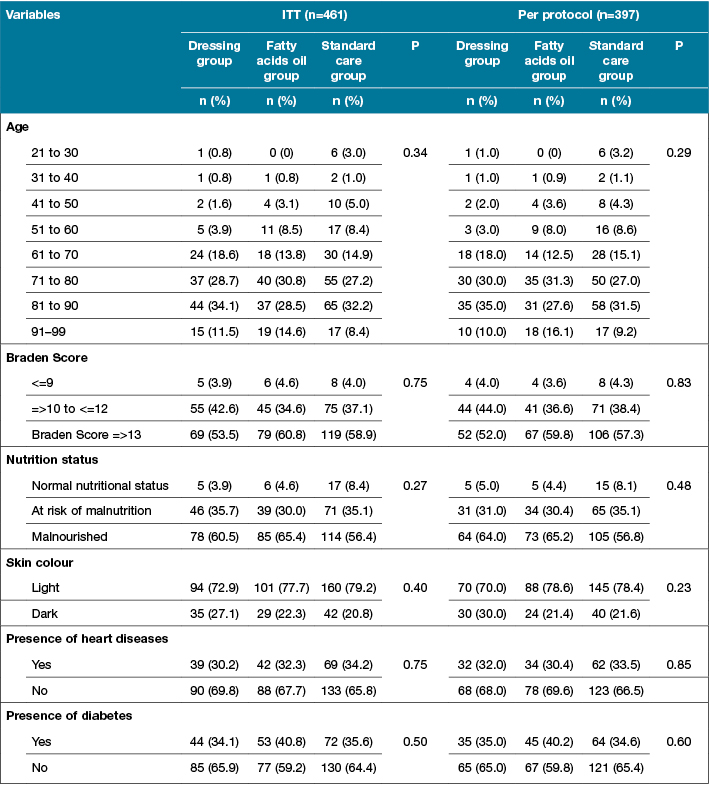
Table 3: Reasons for early termination from study
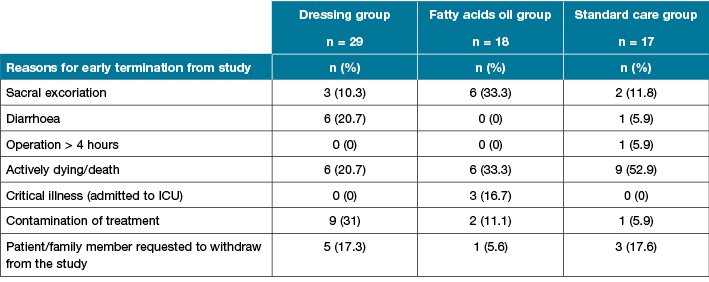
Table 4: Incidence of pressure injury
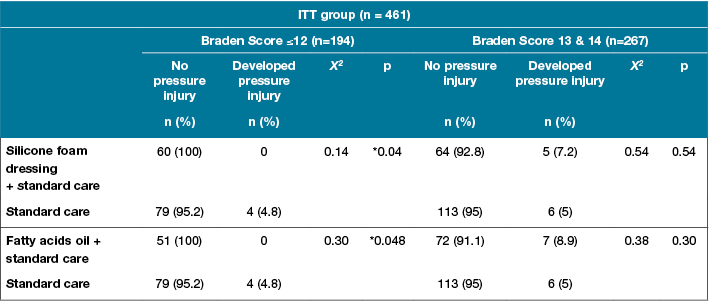
Analysis of sub-groups (based on Braden score) revealed no association between treatment groups and incidence of pressure injury among patients with a Braden score of 13 and above. However, significant association was found between the Silicone foam dressing group and the standard care group (p=0.04) and between the fatty acid group and the standard care group (p=0.048) for patients with Braden score of ≤12 (Table 5).
Table 5: Incidence rate of pressure injury by Braden Score
Discussion
Our study is the first RCT to examine the incremental effectiveness of a prophylactic silicone foam dressing and fatty acids oil among patients in the general acute care setting in Singapore. This is also the first large-scale RCT to investigate the effectiveness of a silicone foam dressing and fatty acids oil among high-risk patients in the acute general ward care setting. In our study, no significant difference was found between the treatment arms in preventing pressure injury in the ITT analysis. However, previous studies have showed positive results of fatty acids oil and silicone foam dressings in preventing pressure injury. In an RCT done by Torra i Bou et al.33, fatty acids oil was found to be effective in preventing pressure injury as compared to placebo with a lower incidence of pressure injury development (7.32% versus 17.37%, p≤0.006) among high-risk patients. However, we were unable to compare Torra i Bou et al.’s33 results with our study as their definition of “medium, high or very high risk patients” was unclear and they had included pressure injuries from multiple body sites (sacrum, heels and trochanter).
Likewise, in Santamaria et al.’s19 study, statistically and clinically significant benefits of silicone foam dressings were reported in the prevention of pressure injuries. These differences in the outcomes may be due to the different types of patients’ profile and the varying risk factors involved. In Santamaria et al.’s study19, the sample population were high-risk patients in the intensive care setting, whereas our sample population were patients in the general ward setting. Patients admitted to the ICUs usually required respiratory support machines, urinary catheter, sequential compression devices, numerous intravenous catheters and infusion pumps. These devices and equipment may contribute to patients’ immobility thus increases the risk of pressure injury34. In addition, our sample population in the general ward care setting had lower risk of pressure injury as they were haemodynamically more stable and were not restricted by machines to ambulate or reposition.
Nonetheless, our finding showed that silicone foam dressing (0 versus 4, p= 0.04) and fatty acid oil (0 versus 4, p= 0.048) were more effective among patients of higher risk profile, which is congruent with the findings of previous studies on higher risk patients9,19,35.
In this study, the Braden Scale was used to assess patients’ risk of pressure injury development and patients with Braden score of ≤14 were recruited. We found no statistical significance for patients with moderate risk (score 13 or 14); however, high-risk patients with a Braden score of ≤12 benefited from the use of prophylactic silicone foam dressings or fatty acid oil for the prevention of pressure injuries. Previous studies19,20 that looked at the use of prophylactic dressings to prevent pressure injuries had also used the Braden Scale to assess their population’s risk of pressure injury development but they did not specify the cut-off scores that were used to identify and select their high-risk patients, hence we are unable to compare and generalise our findings.
The pressure injury risk assessment tool and categorisation of high-risk patients were variable in the literature. Cubit et al.18, did a similar study but had used the Waterlow Pressure Injury Risk Assessment Scale instead of the Braden Scale to identify patients who were at “high risk” of developing pressure injury. In addition, the selection criteria of categorising high-risk patients also vary between studies. In Park’s16 study, although they had used the Braden Scale to identify patients at risk of developing pressure injury, they had categorised patients with a Braden score of ≤16 to be at “high risk”, whereas in our study we categorised patients with a Braden score of ≤14 to be at “high risk”. Notably, other studies13,20 had used specific criteria such as patients who underwent surgery >6 hours, had cardiac arrest at time of admission, were on vasopressors, and suffered from shock, systemic inflammatory response syndrome or multiple organ dysfunction syndrome and did not use any pressure injury risk assessment tool or scoring to categorise their high-risk patients in their study. Hence, with varying pressure injury risk assessment tools and different categorisation cut-off scores to identify high-risk patients, it is challenging to compare results across studies.
Implications for future research
Studies28,36 have shown that microclimate (skin temperature and perspiration) is an independent risk factor for the development of pressure injuries. In our study, we did not measure the effect of microclimate in relation to pressure injury even though Singapore is a tropical country and it is likely that the patients may perspire; however, the wards in our hospital are either fully air-conditioned or installed with air coolers. Nevertheless, future studies in other tropical countries may like to study the effect of microclimate on pressure injuries among patients in a general ward care environment without being air-conditioned.
Besides microclimate, some authors37,38 had studied ethnicity as a variable in pressure injury development. However, there were not many primary studies done and the findings were inconclusive. A study by Anthony et al.38 found no evidence that members of the Pakistani ethnic minority are at higher risk than the majority white population in Burton (UK), with respect to pressure injuries. In our study, we did not include ethnicity as a risk predictor of pressure injury; however, we compared the lighter skin patients to darker skin patients and found no significant difference in the development of pressure injuries between these two groups (19 versus 3, p = 0.44).
Our study further affirms that pressure injury preventive measures should not be limited to critically ill patients in the ICUs. High-risk patients admitted to the general ward care setting can also benefit from the use of a silicone foam dressing as a preventive measure in pressure injury prevention. Future studies may look into the usefulness of silicone foam dressings in other populations, such as patients undergoing long hours of operations or patients in nursing homes. Future studies can also measure the cost-effectiveness of pressure injury preventive measures.
Limitation
Our study was conducted in a single-site acute care setting, hence the results cannot be generalised to other healthcare settings. It was also not possible to blind data collectors to the treatment interventions. Another limitation is that we only recruited patients who were identified as “high risk” upon admission and we did not consider those patients who subsequently developed a “high risk” status after 48 hours of admission.
Our study was slightly under-powered; in order to achieve 0.7 (70%) beta, we needed 494 patients but we only managed to recruit 461 eligible patients over a period of two and a half years. Due to limited resources, we had to end our trial. Our team agreed that this was one of the challenges in studying incidence of pressure injuries among high-risk patients in an acute care setting. In fact, previous RCTs19,35 on pressure injuries in the acute care setting generally had a sample size of 80 to 440 patients.
Conclusion
Having additional preventive measures seems to be clinically beneficial in reducing the incidence of sacral pressure injuries among high-risk patients in the general ward acute care setting.
Acknowledgements
We would like to thank Dr Tracy Carol Ayre, all our ward collaborators and Ms Tay Ai Choo for their support during the study period. We would also like to thank SingHealth Foundation Research Grant 2012 (SHF/HSR061/2012) for funding this study.
Author(s)
Fazila Aloweni
RN, MSc
Nursing Division, Singapore General Hospital
Lim Mei Ling*
RN, BSc
Nursing Division, Singapore General Hospital
Bowyers Block B Level 2, 31 Third Hospital Avenue, Singapore 168753
Tel +65 90698107
Email lim.mei.ling@sgh.com.sg
Chua Tse Lert
RN, BSc
Nursing Division, Singapore General Hospital
Tan Siok Bee
APN, PhD
Nursing Division, Singapore General Hospital
Lian Siew Bee
APN, MN
Nursing Admin, National Cancer Centre Singapore
Ang Shin Yuh
RN, MBA
Nursing Division, Singapore General Hospital
* Corresponding author
References
- National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance. Haesler E, editor. Prevention and Treatment of Pressure Ulcers: Clinical Practice Guideline. Osborne Park, Western Australia: Cambridge Media; 2014.
- Bergquist-Beringer S, Dong L, He J, Dunton N. Pressure ulcers and prevention among acute care hospitals in the United States. Jt Comm J Qual Patient Saf 2013;39(9):404–14.
- Agency for Healthcare Research and Quality. Never Events [Internet]. 2016 [cited 29 July 2016]. Available from: https://psnet.ahrq.gov/primers/primer/3/never-events.
- Galhardo VAC, Garroni Magalhaes M, Blanes L, Juliano Y, Masako Ferreira L. Health-related quality of life and depression in older patients with pressure ulcers. Wounds 2010;22(1):20–6.
- Armstrong DG, Ayello EA, Capitulo KL, Fowler E, Krasner DL, Levine JM et al. New opportunities to improve pressure ulcer prevention and treatment: implications of the CMS inpatient hospital care Present on Admission (POA) indicators/hospital-acquired conditions (HAC) policy. A consensus paper from the International Expert Wound Care Advisory Panel. J Wound Ostomy Continence Nurs 2008;35(5):485–92.
- Demarre L, Verhaeghe S, Annemans L, Van Hecke A, Grypdonck M, Beeckman D. The cost of pressure ulcer prevention and treatment in hospitals and nursing homes in Flanders: A cost-of-illness study. Int J Nurs Stud Epub 0412. 2015;52(7):1166–79.
- Rawlings AV. Ethnic skin types: are there differences in skin structure and function? Am J Health Syst Pharm 2006;28(2):79–93.
- Gefen A. How do microclimate factors affect the risk for superficial pressure ulcers: A mathematical modeling study. J Tissue Viability 2011;20(3):81–8.
- Walker R, Aitken LM, Huxley L, Juttner M. Prophylactic dressing to minimize sacral pressure injuries in high-risk hospitalized patients: A pilot study. J Adv Nurs 2015;71(3):688–96.
- Chaiken N. Reduction of sacral pressure ulcers in the intensive care unit using a silicone border foam dressing. Wound Ostomy Continence Nurs 2012;39(2)
- Call E, Pedersen J, Bill B, Oberg C, Ferguson-Pell M. Microclimate impact of prophylactic dressings using in vitro body analog method. Wounds 2013;25(4):94–103.
- Call E, Pedersen J, Bill B, Black J, Alves P, Brindle CT et al. Enhancing pressure ulcer prevention using wound dressings: what are the modes of action? Int Wound J 2015;12(4):408–13.
- Walsh N, Blanck A, Smith L, Cross M, Andersson L, Polito C. Use of a Sacral Silicone Border Foam Dressing as One Component of a Pressure Ulcer Prevention Program in an Intensive Care Unit Setting [Internet]. 2012 [cited 29 July 2016]. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=ovftm&NEWS=N&AN=00152192-201203000-00005
- Brindle CT. Outliers to the Braden Scale: Identifying high-risk ICU patients and the results of a prophylactic dressing use. WCET J 2010;30(1).
- Byrne J. Prophylactic sacral dressing for pressure ulcer prevention in high-risk patients. Am J Crit Care 2016;25(3):228–34.
- Park KH. The effect of a silicone border foam dressing for prevention of pressure ulcers and incontinence-associated dermatitis in intensive care unit patients. J Wound Ostomy Continence Nurs 2014;41(6):580.
- Tsao WY, Lo SF, Harmod T, Lee RP. A comparison of the efficacy of different wound dressing management techniques in preventing pressure ulcers. Hu Li Za Zhi 2013;60(4):65–75.
- Cubit K, McNally B, Lopez V. Taking the pressure off in the Emergency Department: evaluation of the prophylactic application of a low shear, soft silicon sacral dressing on high risk medical patients. Int Wound J 2013;10(5):579–84.
- Santamaria N, Gerdtz M, Sage S, McCann J, Freeman A, Vassiliou T et al. A randomised controlled trial of the effectiveness of soft silicone multi-layered foam dressings in the prevention of sacral and heel pressure ulcers in trauma and critically ill patients: the border trial. Int Wound J 2015;12(3):302–8.
- Brindle CT, Wegelin JA. Prophylactic dressing application to reduce pressure ulcer formation in cardiac surgery patients. J Wound Ostomy Continence Nurs 2012;39(2):133–42.
- Lyder CH, Ayello EA. Pressure Ulcers: Safety Issue [Internet]. 2008 [cited 29 July 2016]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK2650/
- Ovington LG. Essential fatty acids lubricate skin, prevent pressure sores [Internet]. 1998 [cited 29 July 2016]. Available from: http://www.ahcmedia.com/articles/38778-essential-fatty-acids-lubricate-skin-prevent-pressure-sores
- Declair V. The usefulness of topical application of essential fatty acids (EFA) to prevent pressure ulcers. Ostomy Wound Manage 1997;43(5):48–52, 54.
- Torra i Bou JE, Segovia Gómez T, Verdú Soriano J, Nolasco Bonmatí A, Rueda López J, Arboix i Perejamo M. The effectiveness of a hyper-oxygenated fatty acid compound in preventing pressure ulcers. J Wound Care 2005;14(3):117–21.
- Chiari P, Giorgi S, Ugolini D, Rado E, Montanari M, Giudanella P et al. Randomized controlled trial on the effectiveness of Corpitolinol 60 in the prevention of pressure sores in patients undergoing surgery. Assist Inferm Ric 2012;31(3):131–7.
- Meaume S, Colin D, Barrois B, Bohbot S, Allaert FA. Preventing the occurrence of pressure ulceration in hospitalised elderly patients. J Wound Care 2005;14(2):78–82.
- Meteorological Service Singapore. Climate of Singapore [Internet]. 2016 [cited 27 July 2016]. Available from: http://www.weather.gov.sg/climate-climate-of-singapore/
- Yusuf S, Okuwa M, Shigeta Y, Dai M, Luchi T, Rahman S et al. Microclimate and development of pressure ulcers and superficial skin changes. Int Wound J 2015;12(1):40–6.
- Braden BJ, Maklebust J, Maklebust J. Preventing pressure ulcers with the Braden scale: an update on this easy-to-use tool that assesses a patient’s risk. Am J Nurs 2005;105(6):70–2.
- Stausberg J. The Braden scale and care dependency scale each demonstrate at least 70% sensitivity and specificity for identifying inpatients at risk of pressure ulcer. Evidence Based Nursing Dec 15 2010;14(1):20–1.
- Gupta SK. Intention-to-treat concept: A review. Perspect Clin Res 2011;2(3):109–12.
- Moher D, Hopewell S, Schulz KF, Montori V, Gøtzsche PC, Devereaux PJ et al. CONSORT 2010 Explanation and Elaboration: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340
- Torra i Bou JE, Segovia Gómez T, Verdú Soriano J, Nolasco Bonmatí A, Rueda López J, Arboix i Perejamo M. The effectiveness of a hyper-oxygenated fatty acid compound in preventing pressure ulcers. J Wound Care 2005;14(3):117–21.
- Cooper KL. Evidence-based prevention of pressure ulcers in the intensive care unit. Crit Care Nurse 2013;33(6):57–66.
- Walker R, Huxley L, Juttner M, Burmeister E, Scott J, Aitken LM. A pilot randomized controlled trial using prophylactic dressings to minimize sacral pressure injuries in high-risk hospitalized patients. Clin Nurs Res 2016; 1–20.
- Yoshimura M, Nakagami G, Iizaka S, Yoshida M, Uehata Y, Kohno M et al. Microclimate is an independent risk factor for the development of intraoperatively acquired pressure ulcers in the park-bench position: A prospective observational study. Wound Repair Regen 2015;23(6):939–47.
- Harms S, Bliss D, Garrard J, Cunanan K, Savik K, Gurvich O et al. Prevalence of pressure ulcers by race and ethnicity for older adults admitted to nursing homes. J Gerontol Nurs 2014;40(3):20–6.
- Anthony D, Johnson M, Reynolds T, Russell L. Ethnicity in pressure ulcer risk assessment, with specific relation to the Pakistani ethnic minority in Burton, England. J Adv Nurs 2002;38(6):592–7.



