Volume 25 Number 2
Treatment of invasive aspergillus-associated wound infection incorporating topical amphotericin B
Leigh R Warren, Shantanu Bhattacharjya, Nitin Abrol, Christine Russell and Santosh Antony-Olakkengil
Abstract
Invasive aspergillosis is a rare complication of renal transplantation that carries a high mortality rate. We describe the case of a patient with an invasive aspergillus-associated postoperative wound infection. Successful treatment was achieved with a combination of surgical debridement and a novel approach involving the use of topical amphotericin B in addition to intravenous anti-fungal therapy.
Introduction
Aspergillus is a common fungal organism that can cause infection in an immunocompromised host. Wound infections involving aspergillus are uncommon and can be difficult to treat when they occur. This report describes the successful outcome of treatment of a postoperative wound infection associated with invasive aspergillosis using a novel approach incorporating topical anti-fungal therapy.
Clinical Presentation
A 38-year-old female was transferred from a regional centre to our transplant unit two months following renal transplantation with a persistent postoperative wound infection. The surgery and immediate postoperative care had been unremarkable. Medications included an immunosuppression regimen of tacrolimus and mycophenolate. Computerised tomography (CT) imaging demonstrated a large fluid collection deep to the wound (Figure 1). Placement of a percutaneous pigtail catheter failed to drain the collection. Wound exploration and debridement revealed a large collection of pus from which a sample was taken for culture. Growth of aspergillus sensitive to amphotericin B was observed. Repeated operative wound debridement approximately every three days, washout and intravenous liposomal amphotericin B initially failed to clear the infection and persistent growth of invasive aspergillus was seen macroscopically (Figure 2) and on histological examination. Further patient deterioration necessitated more radical debridement including transplant nephrectomy. This enabled further debulking of the affected tissues, reduced the likelihood of mycotic aneurysm development, and allowed a reduction in immunosuppressive therapy. Repeated attempts at debridement of macroscopic infection approximately every three days in association with negative pressure dressings failed to control fungal growth.

Figure 1
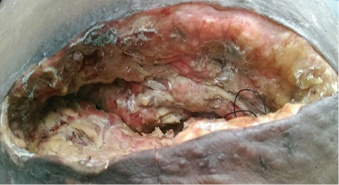
Figure 2
To achieve a higher local concentration of amphotericin B, topical antifungal therapy was commenced. Amphotericin soaked absorbable gelatin sponges (Spongostan®) were placed into the wound in addition to the intravenous liposomal amphotericin B. A total of 10 ml of sterile 0.3% amphotericin B solution was used topically on each application. This was applied following debridement approximately every three days on five separate occasions over a 16-day period. The IV dose was adjusted accordingly to account for systemic absorption. Negative pressure wound dressings were used between each debridement procedure set at a continuous negative pressure of –125 mmHg. After repeated wound debridement approximately every three days and application of this topical antifungal therapy following each debridement over a one-month period, the wound was suitable for closure (Figure 3). The patient was ultimately discharged without further wound complication.

Figure 3
Discussion
Renal transplantation is a common treatment option for patients with end-stage renal failure. Following transplantation, immunosuppressive therapy primarily targets T cell-mediated graft rejection. This immunosuppressive state leads to increased susceptibility to invasive fungal diseases including aspergillus. Incidence of invasive fungal infections in kidney transplant patients may range from 1.4% to 9.4%1-2 according to international publications. Fungal infection generally presents within the first six months following initiation of immunosuppressive therapy3. Aspergillus is a common fungal organism that can cause infection in an immunocompromised host. Infections with aspergillus may include invasive aspergillus, allergic bronchopulmonary aspergillosis (ABPA), chronic necrotising pulmonary aspergillosis (CNPA) and aspergilloma4. Diagnosis of an invasive fungal infection is made when histological analysis or culture from a specimen of tissue taken from a site of disease can reveal fungus5. Invasive aspergillosis has a high mortality rate (>70%) in solid organ transplant patients5.
Treatment options for invasive aspergillus include antifungal agents such as amphotericin B, azoles and candins5. Amphotericin B is a polyene with a broad spectrum of activity, including most filamentous fungi and yeasts. Liposomal amphotericin B is a lipid-associated formulation that has been shown to be more effective and less nephrotoxic compared with amphotericin B6.
Wound infections involving aspergillus are uncommon; however, they have been reported previously in the literature in association with pleural empyema7. Invasive fungal wound infections pose a difficult situation where intravenous antifungal treatment may be unable to penetrate adequately into the affected tissues. The use of topical antifungal therapy is common in cutaneous fungal infections and previously has been used successfully in pleural aspergillosis7-8.
Our patient had a significant wound infection with macroscopic growth of aspergillus species that did not initially respond to treatment with intravenous liposomal amphotericin B and wound debridement. The subsequent addition of topical liposomal amphotericin B complemented local control of disease and contributed to local clearance of aspergillus over a 3-4 week period. Absorbable gelatin sponges (Spongostan®) soaked in liposomal amphotericin were used as a means of releasing amphotericin into the tissues over a more prolonged period between dressing changes and avoiding rapid suction of the drug through the negative pressure system. The use of gelatin sponge material to assist with the sustained delivery of topical antifungal therapy was previously described in a case of aspergillus empyema8. Throughout management of our patient, advice was sought from the local infectious diseases unit. Expertise in the management of invasive fungal disease assisted with guiding the choice of a suitable antifungal agent, consideration of resistance patterns and antifungal therapy stewardship.
Conclusion
This case report describes the successful treatment of a significant invasive aspergillus wound infection using a combination of surgical intervention and both topical and intravenous liposomal amphotericin B. Although this disease carries a high mortality rate, aggressive treatment using surgical and non-surgical approaches may alter the course of disease.
Conflict of interest
All authors declare that they have no conflict of interest associated with the submitted material.
Author(s)
Leigh R Warren
Central Northern Adelaide Renal and Transplantation Service (CNARTS)
Royal Adelaide Hospital, SA, Australia
Shantanu Bhattacharjya
Central Northern Adelaide Renal and Transplantation Service (CNARTS)
Royal Adelaide Hospital, SA, Australia
Nitin Abrol
Central Northern Adelaide Renal and Transplantation Service (CNARTS)
Royal Adelaide Hospital, SA, Australia
Christine Russell
Central Northern Adelaide Renal and Transplantation Service (CNARTS)
Royal Adelaide Hospital, SA, Australia
Santosh Antony-Olakkengil*
Central Northern Adelaide Renal and Transplantation Service (CNARTS)
Royal Adelaide Hospital, SA, Australia
Email Santosh.Olakkengil@sa.gov.au
Tel 08 8222 4000
* Corresponding author
References
- Nampoory MR, Khan ZU, Johny KV, Constandi JN, Gupta RK, Al-Muzairi I et al. Invasive fungal infections in renal transplant recipients. J Infect 1996;33(2):95–101.
- Badiee P, Kordbacheh P, Alborzi A, Zeini F, Mirhendy H, Mahmoody M. Fungal infections in solid organ recipients. Exp Clin Transplant 2005;3(2):385–9.
- Venkataramanan R, Zang S, Gayowski T, Singh N. Voriconazole inhibition of the metabolism of tacrolimus in a liver transplant recipient and in human liver microsomes. Antimicrob Agents Chemother 2002;46(9):3091–3.
- Harman E. Aspergillosis. emedicine. 2015; Available URL: http://emedicine.medscape.com/article/296052-overview [accessed 20/11/16]
- Khan A, El-Charabaty E, El-Sayegh S. Fungal infections in renal transplant patients. J Clin Med Res 2015;7(6):371–8.
- Barrett JP, Vardulaki KA, Conlon C, Cooke J, Daza-Ramirez P, Evans EG et al. A systematic review of the antifungal effectiveness and tolerability of amphotericin B formulations. Clin Ther 2003;25(5):1295–320.
- Bonatti H, Lass-Floerl C, Angerer K, Singh N, Lechner M, Stelzmueller I et al. Successful management of postpneumonectomy Aspergillus pleural empyema by combined surgical and anti-fungal treatment with voriconazole and caspofungin. Mycoses 2010;53(5):448–54.
- Purohit M, Guleri A, Zacharias J. Salvage therapy with topical antifungal for Aspergillus fumigatus empyema complicating extrapleural pneumonectomy. Interact Cardiovasc Thorac Surg 2012;15(3):518–9.



