Volume 25 Number 4
Pressure cushions in a home environment: How effective are they at reducing interface pressure and does the chair surface count? A pilot study
Gavin Brealey, Erin James and Karen Hay
Abstract
Background: Pressure Injuries are a relatively common but largely avoidable result of hospitalisation and care for frail clients in their own homes. These injuries are costly, painful and debilitating. Current research and intervention guidelines have focused on clients who are either in bedded facilities or chair/wheelchair-dependent. The majority of existing pressure redistribution surfaces have been designed and tested for these populations. Method: This paper describes a small pilot study designed to explore the effectiveness of these prevention devices at reducing interface pressure when utilised on a non-standard surface (an armchair), utilising each subject as their own case control to compare against the device on a “control” surface. Results: It was found there was a statistically significant difference in cushion performance dependent upon which surface was used. It was also found that devices that are most effective at interface pressure reduction on the “control” surface were not necessarily the most effective on the non-ideal armchair. Conclusions: These findings have clinical implications for the prescription of effective pressure redistribution surfaces for use in a client’s own home.
Introduction
This article presents the results of a pilot study seeking to examine how pressure redistribution cushion effectiveness is impacted by the surface upon which it is utilised. The project sought to determine if chair surface has a significant impact on a cushion's interface pressure as measured by a pressure mapping device. Reasons for the importance of research in this area and outcomes are discussed. This pilot study was conducted in accordance with the statement on human experimentation; low-risk ethics approval was provided by the Prince Charles Hospital, Metro North Hospital and Health Service (MNHHS) ethics committee.
Background
Hospital-acquired pressure injuries (PI) cost health care systems a significant amount. Victorian and Queensland data from 2006 shows that there were 2873 hospital-acquired PI, adding $24,234,740 to the cost of care for these patients, an average of $8435.34 per case1.
These clients are often discharged to their usual place of residence, meaning many clients are living at home at high risk of a PI. A 2009 study of community-dwelling clients conducted by Asimus2 in the New South Wales Hunter region with clients of a home nursing service found a PI prevalence rate of 8.9% with 40.8% developing the PI during care by the service, the remainder having been acquired at an acute facility or prior to contact.
A systematic review conducted in 2009 by Gorecki et al.3 found that PIs are often painful and debilitating, their common locations on bony prominences leading to activity restriction and loss of occupational roles. They found these ongoing issues lead to feelings of powerlessness, anxiety, decreased appetite and mood. These issues impact fundamentally on our clients' ability to enjoy life to their fullest potential.
Clients living at home need to be provided with effective, evidence-based interventions to reduce the risk of PI occurrence and to assist in the effective healing of active wounds as per existing PI prevention guidelines4,5. One of the interventions set out in these guidelines is that clients with existing PI or at risk of PI should be managed on a pressure redistribution surface when in bed or seated. Multiple studies6-12 have focused on the use of pressure redistribution surfaces to reduce the risk of PI when lying and seated. These studies have mainly focused on PI prevention in the hospital setting or with clients who are restricted in their mobility/confined to a wheelchair, providing evidence to support the use of pressure redistribution surfaces to reduce PI incidence.
Prescription guidelines for pressure redistribution cushions have been based on this evidence and then generalised to the community setting. This may not be an effective strategy, as a study by DeFloor and Grypdonck13 found that only 13 out of 29 cushions tested on a hospital bedside armchair reduced interface pressure compared to the chair itself. A study of the Repose® 14 overlay found this to be clinically effective and cost-effective when used in the community. Provision of effective PI prevention in the community is an emerging challenge, and one that is under-represented in the current literature.
A further challenge for clinicians is the inconclusive literature regarding the clinical accuracy of pressure-mapping devices to objectively measure tissue pressure gradients. In particular, the inaccuracy of extrapolating surface pressure measurements to internal pressure levels at critical tissue bone interfaces such as the ischial tuberosity is of concern15-17.
However, it is generally accepted that pressure mapping can be accurately utilised to compare pressure redistribution surfaces for interface pressure reduction effectiveness and that these pressure measurements are useful for clinical selection of the most effective support surface for users12,18-20. The estimated capillary refill pressure of 32 mmHg has been proposed as a baseline12,21,22; however, it is not validated. It is generally agreed that PI risk rises with increasing interface pressure and sustained seating times12. In a rat study a constant pressure of 145 mmHg applied 5 times for a 6-hour period caused PI in 90% of cases21, although no research has been able to establish a safe minimum pressure due to the multitude of contributing factors12,21,22.
In acknowledging the existing literature, the authors of this study feel that the use of pressure mapping will provide clinically useful comparative data to determine differences in pressure relief cushion effectiveness and the impact of varied chair surfaces.
Aim
This pilot study sought to compare the performance of a range of pressure redistribution cushions to reduce interface pressure on two different surfaces: an armchair compared to an ideal surface, using a small sample of health professional volunteers. We sought to identify potential trends which could be investigated in future studies to inform clinical decision making and equipment purchasing.
Research questions
- Are pressure redistribution surfaces (cushions) effective at reducing interface pressure on armchairs?
- Are the cushions that are most effective at interface pressure redistribution on an ideal surface also the most effective cushions on a non-ideal representative surface? (i.e. an Armchair)
Method
Study design: Mixed methods case series design.
Participants: Convenience sample of consenting (n=10) health professionals, 2 male and 8 female targeting a range of gender, age and body mass index (BMI). Male height range of 1.74–1.8 m, weight range of 76–78 kg and BMI range of 23.5–25.6. Female height range of 1.57–1.8 m, weight range of 51–97 kg, and BMI range of 19.36– 30.27.
Method: Two chairs were used (see Figure 1):
- A common household armchair (a used/second-hand, single timber frame, foam seat and base armchair).
- An adjustable height, firm chair was used as the control seating surface to simulate cushion testing procedures as per ISO standards testing procedures and standard practice12 (a Rehab brand bariatric compressed foam shower chair).
Both chairs were set to ideal transfer height, as estimated by measuring distance between the floor and the insertion of the participant’s biceps femoris tendon and adding 50 mm. This distinct anatomical landmark +50 mm technique was used as it provided easy access and has high repeatability23. For ease of set-up when changing cushions, the chairs were set to a fixed height for each participant and adjustable foot rests used to adjust for differences in cushion height.

Figure 1: Experimental test set-up, showing armchair and firm chair (control)
The pressure redistribution cushions used were a convenience sample of cushions currently owned and prescribed by the local service (Community Indigenous and Sub-acute Services, MNHHS). These represented a cross-section of the different types of cushions (materials, risk reduction classification) currently available in Australia.
Cushions were used by participants sitting on the two surfaces (armchair and firm chair), testing each for these seven conditions:
- Without a pressure redistribution device and on each of six cushions.
- Multi-cell air — Roho® 24. Roho makes a range of high PI risk cushions for use in pressure redistribution, utilising their patented DRY FLOTATION TECHNOLOGY®; the particular cushion used in the study was a ROHO QUADTRO high-profile cushion.
- Gel/foam — JAY® Easy25. JAY makes a range of pressure redistribution cushions and is known for gel/foam-based cushions which have contoured bases to support postural needs, The JAY Easy is one such cushion aimed at clients with low to moderate PI risk.
- Single cell air — Repose® 26. The Repose cushion used in our study is made by Frontier Medical; it has a single air chamber and comes in an easy to use pump. It is designed for people with high to very high PI risk.
- Dry gel polymer — EquaGel® 27. The EquaGel protector used in the study is made of dry-polymer gel constructed in a lattice and is designed for people at moderate to high PI risk.
- Foam — MacMed28. MacMed manufactures and supplies a range of adaptive equipment. The MacMed Deluxe Foam used in the study is designed for people at low to moderate risk of PI.
- Gel — Action® 29. Action makes a range of gel overlays and cushions. The pilot® made with Akton® polymer within the cushion is designed to allow immersion while eliminating shear and bottoming out and reducing vibration. These cushions are very low profile, meaning they have minimal impact on chair ergonomics. They are designed for people at low to moderate risk of PI.
For each condition, the participant sat on the cushion to be tested for five minutes as this was found to be the optimum time to allow for tissue deformation and cushion settling in previous studies10-12.
Outcome measures
Self-reported comfort: Self-reported perceived comfort of each cushion condition between 1 and 10, (where 1 was the least comfortable and 10 the most) was assessed at the end of each five-minute testing period.
Quantitative: Interface pressure readings were provided by the commercially available BodiTrak pressure30 mapping device to measure the reduction in interface pressure offered by a range of different cushions.
The BodiTrak has 256 individual sensors forming a grid of approximately 1” squares. It registers a pressure reading for each sensor in millimetres of mercury (mmHg) from 0 to 200. Sensor data is collected on the connected laptop computer. The mapping device takes a continuous recording of the interface pressure and a single representative reading (taken between 4:30 minutes and 5:00 minutes of sitting on each cushion) was selected for analysis.
Data analysis: These representative readings were exported to Microsoft® Excel as a list of individual cell numbers (such as, for example, A2, B2) with an associated pressure reading. These results were summarised for each cushion to provide an overview of the interface reduction efficacy of each cushion used in the study. The results were plotted within Excel according to numbers/percentages of sensors activated at or above certain pressure thresholds. The results represent interface pressures from 88 mmHg and above as they are well within the “at risk” range consistently postulated within the literature12,20,21.
The coefficient of variation (COV) was also chosen as a key outcome measure as it is a standard measure of variability; it is defined as the standard deviation/mean, providing a measure that takes into account mean pressure and variability. In this context a lower COV would be expected to indicate a more effective distribution of pressure as it indicates less variability over the measured cells. Associations between chair type, cushion type, subject characteristics and the COV were assessed using mixed effects linear regression modelling analyses and were performed using the Stata statistical software package (version 13).
Qualitative results were also analysed in summative form, and displayed as combined averages to enable visual comparison.
Results
Quantitative measures
Results from the mixed effects regression model for the COV are presented in Table 1. The predicted marginal means were generated and plotted as shown in Figure 2. Chair type, cushion type, the interaction term between chair and cushion and BMI were all significantly associated with the COV. The significant interaction indicates that the effect of the cushion differs depending on the type of chair. The COV was notably high for the firm chair with no cushion and the firm chair with Action Gel. With the exception of the JAY Easy and ROHO cushions, the predicted mean COV for a given cushion type was significantly lower for the armchair compared to the firm chair. Within the subjects studied, increasing BMI was significantly associated with reduced COV.
Table 1: Effect estimates for variables associated with the coefficient of variation derived from a mixed effects linear regression model
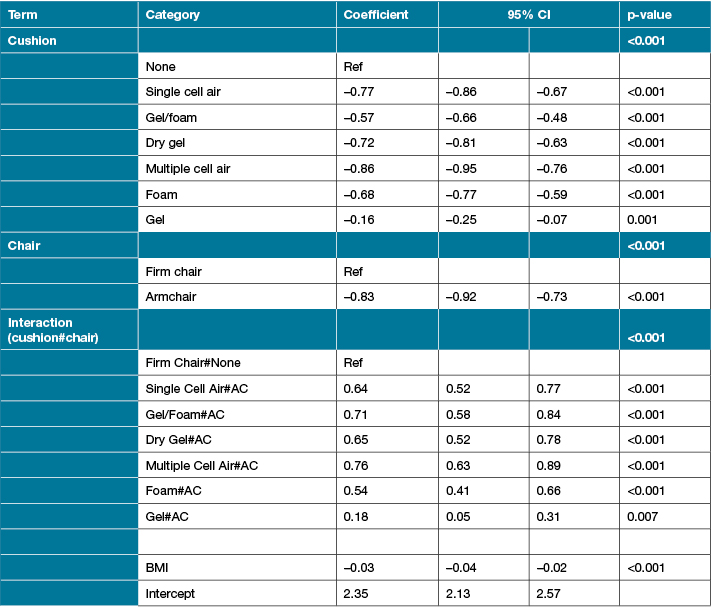

Figure 2: Margins plot of predicted COV with 95% CI by cushion and chair type
Summative results for the armchair, firm chair and comparative data are presented in Figures 3 and 4.
The summative results for the armchair shown in Figure 3 show that most of the cushions tested provided interface pressure reduction when compared to the chair alone. Though the gel/foam cushion consistently demonstrated raised interface pressure, the multi-cell air and gel cushions had quite variable results, with some people mapping a higher interface pressure on these than on the chair alone. The results are presented as a percentage of the total activated cells with a pressure reading above zero. The single cell air, dry gel and foam cushions consistently reduced interface pressure for all participants.
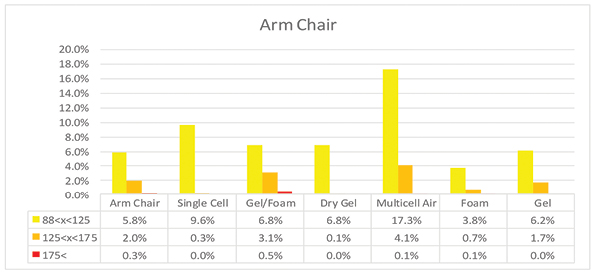
Figure 3: Demonstrates percentages of cells recording pressure measurements in the ranges indicated for cushions on the armchair.
The summative pressure measurements for the firm chair shown in Figure 4 show that all cushions tested provided a reduction in interface pressure when compared to the firm chair alone. The single cell air and multi-cell air were most effective at interface pressure reduction, consistent with the results found by Shechtman et al.12 .This is followed by the foam cushion as evidenced by the total number of map cells activated and reduction in peak pressure. The results are presented as a percentage of the total activated cells with a pressure reading above zero.
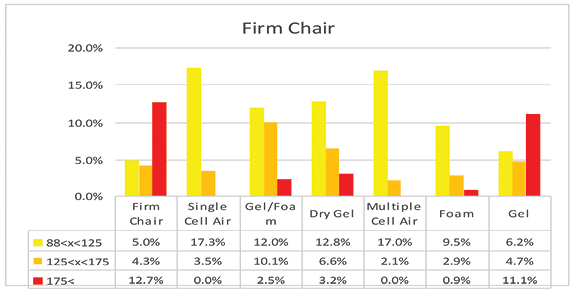
Figure 4: Demonstrates the percentages of cells recording pressure measurements in the ranges indicated for cushions on the firm chair.
The results demonstrated a higher proportion of readings in excess of 175 mmHg for the firm chair as compared to the armchair. They showed the multi-cell air cushion demonstrated a higher proportion of readings in excess of 125 mmHg when on the armchair, than when on the firm chair. In contrast, the opposite result is seen for the dry gel cushion with the proportion of cells registering above 125 mmHg higher for the firm chair than when on the armchair. It can also be seen that the single cell air and foam cushions performed consistently on both surfaces in comparison to the other cushions tested. The results are presented as a percentage of the total activated cells with a pressure reading above zero.
The summative data was used to place the cushions in order by the proportion of activated cells over 125 mmHg in Figures 3 and 4 (as a percentage of the total activated cells mmHg>0). They show a clear difference in the order of effectiveness at reducing interface pressure depending on the chair surface. As mentioned, for Figure 1 several cushions (gel, multi-cell air) had quite variable results depending on participant (Subject 1 results for the armchair were 4.2% (88<x<125), 0.8% (125<x>175) and 0% (175<x) compared to the multiple cell air 31.9%, 11.1% and 0.4% respectively; Subject 2 results for the armchair were 6.5% (88<x<125), 1.3% (125<x>175) and 0% (175<x) compared to the multiple cell air 19%, 2.3% and 0% and gel 10.9%, 4.4% and 0% respectively; Subject 3 results for the armchair were 4.6% (88<x<125), 0% (125<x>175) and 0% (175<x) compared to the multiple cell air 12.1%, 0.9% and 0% respectively; Subject 4 for results for the armchair were 4.4% (88<x<125), 0% (125<x>175) and 0% (175<x) compared to the gel 7.7%, 3.8% and 0% respectively). These cushions have been placed lower in the effectiveness rankings according to the level of inconsistency.
Self-reported comfort results
Figures 6 and 7 present the average comfort ratings for each condition. In summary, it was found that not all of the tested pressure redistribution cushions were effective at reducing interface pressure when compared to the armchair alone; some of the cushions tested actually increased measured interface pressure. Three of the cushions tested consistently reduced measured interface pressure for all participants.
It was also found that the cushions that were measured to be most effective at reducing interface pressure on the armchair were not necessarily the most effective at reducing interface pressure on the firm chair.
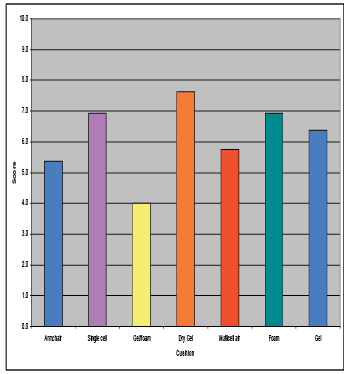
Figure 6: Armchair
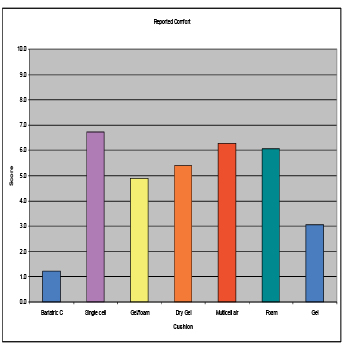
Figure 7: Firm chair
Discussion
Coefficient of variation
There were significant differences in the coefficient of variation of the cushions tested, indicating some were more effective at evenly distributing pressure across the two surfaces tested. The significant ceiling effect offered by the 200 mmHg measuring cut-off could have influenced the magnitude of these differences overall. Another statistically significant finding is that increasing BMI was significantly associated with reduced COV. This may be explained by the increased measuring device surface area covered and ceiling effect, and could warrant further study.
Armchair
This pilot study found three of the cushions tested (foam, single cell air, dry gel) were effective at reducing interface pressure for all participants when compared to the armchair alone. Interestingly, these three cushions are at the lower end of the cost spectrum, are of simple design (basic cuboid shape with minimal contours) and simple to use. The fact that the foam/gel cushion demonstrated a higher proportion of readings in excess of 125 mmhg when on the armchair is of clinical concern as it indicates it is possible to increase interface pressure through the prescription of a pressure redistribution surface.
Firm chair
This pilot study found that all the cushions tested demonstrated a lower proportion of readings in excess of 125 mmHg when compared with the firm chair with no cushion. This indicates that all of the cushions performed their designed function when used within the parameters they were initially designed and created for. It was found that the two air cushions were clearly the most effective (see results, Figure 4) for this population on this surface.
Chair comparison
When the results for the two chair surfaces are compared it can be seen that the order of effectiveness ranking for the pressure redistribution surfaces is different (as measured by proportion of activated cells above 125 mmHg (Figure 5). All the cushions improved measured interface pressure in comparison to the firm chair (Figure 4); in contrast, one cushion actually increased interface (Figure 3) pressure when used on the armchair (soft surface). This could potentially place clients at increased risk of PI and has implications for prescription.
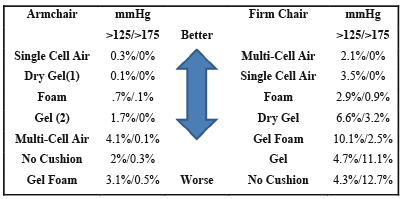
Figure 5: Shows the cushions in order by the proportion of activated cells over 125 mmHg (as a percentage of the total activated cells mmHg>0) in order to visually represent the difference in order of measured interface pressure reduction effectiveness
Note: (1) Dry gel has been placed second as its individual results were more variable than those of the single cell air cushion. (2) Gel has been placed above multi-cell air as its individual results were more variable.
Reflecting on the construction of the cushions that consistently demonstrated effective interface pressure reduction on the armchair provides possible insights. Cushions that provided the most effective and consistent interface pressure reduction on the soft and curved surface of the armchair (Figure 3) were those with relatively simple design and function, where pressure was effectively distributed, despite underlying deformation of the cushion.
Conversely, cushions that consistently demonstrated effective interface pressure reduction on the firm surface but not the armchair (Figures 3 and 4), were of more complex design and construction with multiple physical elements designed to work together to disperse pressure; they were effective at reducing interface pressure within their design parameters on the chair surface that they were designed for, but did not perform as well or not at all when used on non-standard surfaces.
The gel foam cushion’s measured increase in interface pressure in comparison to the armchair alone (Figure 3) may have been due to its contoured, firm foam base designed to provide postural support when used on an ideal surface, as on the curved sling base it was observed to bend and deform. This may have resulted in the gel and contours no longer being able to conform to the subject.
A possible reason for differences seen between the multi-cell air cushion on the armchair versus the firm chair may be that it is not able to effectively distribute pressure due to ‘crowding’ of the cells, with each cell sticking to the cells surrounding it, or the air channels connecting them collapsing due to the curved/soft sling base, thus not allowing them to equalise air pressure amongst the cells.
Self-reported comfort results
From the graphs it can be seen that increasing comfort was generally associated with improving interface pressure reduction effectiveness. The match is not exactly the same as the order of interface pressure reduction effectiveness but it is closely indicative of which cushions were clinically effective. The key indication from the self-reported comfort results was that comfort and effectiveness at pressure reduction were closely related for all participants. Though not identical, participant perceived comfort reflected cushion effectiveness; all cushions perceived as more comfortable than the chair surface alone effectively reduced interface pressure. This result has clinical prescription implications that are worthy of future research.
Additional observations
When observing participants it was noted that:
- No cushion reduced interface pressure to below 32 mmHg.
- Placing arms on arm rests provided high levels of interface pressure reduction.
- Off-loading postures were effective at significantly decreasing interface pressure in high-risk areas (sacrum, ischial tuberosity).
Study Limitations
This study has several limitations:
- The study was conducted with a small number of staff volunteers who may not accurately reflect the target population of older, community-based clients.
- The study was conducted comparing only two chair surfaces, and repeating this study using a wider range of surfaces (as exist in our client’s homes) is recommended for future research.
- The study used a convenience sample of six readily available pressure redistribution cushions currently in use with MNHHS CISS.
- Due to the limitations of the cushions, test rig and measuring device it was not possible to map bariatric participants.
- A significant ceiling effect was found from the 200 mmHg upper pressure reading limit that impacted results for the control surface.
Conclusion
This study confirms that the chair surface influences the performance of pressure redistribution cushions. This small pilot study indicated that pressure redistribution cushions do behave differently on an armchair compared to a firm chair. Therefore, cushions considered “gold standard” on an ideal surface may not perform consistently on non-ideal surfaces. This has significant importance for future research directions and clinical practice in pressure redistribution equipment prescription. Further research is required to:
- Explore the impact of chair materials, structures and ergonomics in measured interface pressure to determine if there are consistent trends that can be easily identified to support effective cushion prescription.
- Validate these initial results with the target population utilising a larger sample size.
- Further explore the relationship between self-perceived comfort and interface pressure reduction effectiveness in the target population.
- Replicate this study with bariatric clients.
Acknowledgements
The authors would like to acknowledge contributions made by Ms Jo Walters (as the project’s Executive Sponsor), Community, Indigenous and Sub-acute Services (CISS) Occupational Therapists (as the research participants), Dr Sally Eames (for research design and manuscript preparation advice) and Dr Vanessa Constable (for support with ethics and governance application/s).
Author(s)
Gavin Brealey*
BHSc OT, GCert Health Service Management
Director, Occupational Therapy
Community, Indigenous and Sub-acute Services Metro North Hospital and Health Service
Brisbane, QLD, Australia
Email gavin.brealey@helath.qld.gov.au
Erin James
MSc OT, B Human Movement Science (Education) Senior Occupational Therapist, Interim Care Service, Community, Indigenous and Sub-acute Services, Metro North Hospital and Health Service Brisbane, QLD, Australia
Email erin.james@health.qld.gov.au
Karen Hay
BVSc, MEpi, PhD
Biostatistician, QIMR Berghoffer Medical Research Institute
Email Karen.Hay@qimrberghofer.edu.au
* Corresponding author
References
- Jackson T, Nghiem HS, Rowell D, Jorm C, Wakefield J. Marginal costs of hospital acquired diagnoses: Information for priority setting for patient safety programs and research. J Health Serv Res Policy 2011;16(3):141–146.
- Asimus M, Li P. Pressure ulcers in home care settings: Is it overlooked? Wound Practice & Research [serial on the Internet]. 2011 [cited April 11, 2017];19(2):88. Available from: Informit Health Collection.
- Gorecki C, Brown JM, Nelson EA, Briggs M, Schoonhoven L, Dealey C, Defloor T, Nixon J and on behalf of the European Quality of Life Pressure Ulcer Project group. Impact of pressure ulcers on quality of life in older patients: A systematic review. J Am Geriatr Soc 2009;57:1175–1183. DOI:10.1111/j.1532-5415.2009.02307.x
- Australian Wound Management Association. Pan Pacific Clinical Practice Guideline for the Prevention and Management of Pressure Injury. Osborne Park, WA: Cambridge Media, 2012. ISBN Print: 978-0-9807842-5-1 ISBN Online: 978-0-9807842-3-7.
- National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure injury Alliance. Prevention and Treatment of Pressure Ulcers: Quick Reference Guide. Emily Haesler (Ed.). Osborne Park, WA: Cambridge Media, 2014.
- Cullum NA, McInnes E, Bell-Syer SEM, Legood R. Support surfaces for pressure ulcer prevention. Cochrane Database of Syst Rev 2004, Issue 3. Art. No.: CD001735. DOI: 10.1002/14651858.CD001735.pub2.
- Brienza DM, Karg PE, Geyer MJ, Kelsey S, Trefler E. The relationship between pressure ulcer incidence and buttock–seat cushion interface pressure in at-risk elderly wheelchair users. Arch Phys Med Rehabil 2001;82:529–33
- Brienza D, Kelsey S, Karg P et al. A randomised clinical trial on preventing pressure ulcers with wheelchair seat cushions. J Am Geriatr Soc 2010;58:2308–14.
- Maen Aljezawi. Exploring Preventive Interventions and Risk Factors of Hospital-Acquired Pressure Ulcers: A Retrospective Matched Case-Control Design Doctoral thesis 2011.
- Crawford SA, Stinson MD, Walsh DM, Porter-Armstrong AP. Impact of sitting time on seat-interface pressure and on pressure mapping with multiple sclerosis patients. Arch Phys Med Rehabil 2005;86:1221–5
- Yuen HK, Garrett D. Case report — Comparison of three wheelchair cushions for effectiveness of pressure relief. Am J Occup Ther 2001;55:470–75.
- Shechtman O, Hanson C, Garrett D, Dunn P. Comparing wheelchair cushions for effectiveness of pressure relief: A pilot study. Occupational Therapy Journal of Research 2001;21(1): 29–48 DOI: 10.1177/153944920102100103
- DeFloor T, Grypdonck F. Do pressure relief cushions really relieve pressure? Western J Nurs Res 2000;22(3):335–350.
- Hampton S. Repose: The cost-effective solution for prompt discharge of patients. Br J Nurs 2000;2249–50
- Gefen A & Levine J. The false premise in measuring body-support interface pressures for preventing serious pressure ulcers, J Med Eng Technol 2007;31:5:375–380, DOI: 10.1080/03091900601165256
- Reenalda J, Jannink M, Nederhand M & IJzerman M. Clinical use of interface pressure to predict pressure ulcer development: A systematic review. Assist Technol 2009;21(2):76–85. DOI:10.1080/10400430903050437
- Swain I, Bader D. The measurement of interface pressure and its role in soft tissue breakdown. J Tissue Viability [serial on the Internet]. (2002, Oct 1), [cited April 12, 2017];12132–146. Available from: ScienceDirect.
- Hollington J, Hillman S. Can static interface pressure mapping be used to rank pressure distributing cushions for active wheelchair users?. J Rehabil R D [serial on the Internet]. (2013, Jan), [cited April 12, 2017];50(1):53–60. Available from: CINAHL Complete.
- Shelton F, Lott J. Conducting and interpreting interface pressure evaluations of clinical support surfaces. Geriatr Nurs [serial on the Internet]. (2003, Jan 1), [cited April 12, 2017];24222–227. Available from: ScienceDirect.
- Russell L. Overview of research to investigate pressure-relieving surfaces. Br J Nurs 2001;10(21):1421–1426. DOI:10.12968/bjon.2001.10.21.9343
- Salcido R, Fisher S, Donofrio J, Bieschke M, Knapp C, Carney J et al. An animal model and computer-controlled surface pressure delivery system for the production of pressure ulcers. J Rehabil R D [serial on the Internet]. (1995, May), [cited April 18, 2017];32(2):149–161.
- Lyder C. Pressure ulcer prevention and management. JAMA [serial on the Internet]. (2003, Jan 8), [cited April 20, 2017];289(2):223–226. Available from: MEDLINE Complete.
- Tuttle N. A comparison of methods used for measuring popliteal height. Ergonomics Australia 2004;18:14–18.
- ROHO. 2016. Product information retrieved from: https://roho.com/product/products/cushions/adjustable-skin-protection/high-profile-single-compartment-cushion/
- JAY Easy Fluid. 2016. Product information retrieved from: http://www.sunrisemedical.com.au/seating/jay/wheelchair-cushions/jay-easy-fluid
- REPOSE. 2016. Product Information retrieved from Frontier Medical Group: http://www.reposedirect.com/product/cushion/
- Think Mobility. 2016. Product Information retrieved from: http://www.thinkmobility.com.au/dva-range/cushions-pillows/cushion-equagel-protector-20-x-18
- MacMed. 2016. Product Information retrieved from MacMed: https://macmedhealthcare.com/shop/macmed-premium-cushion/
- Action Gel. 2016. Product Information retrieved from Active Medical Supplies: http://www.activemedicalsupplies.com.au/site/DefaultSite/filesystem/Documents/3542-d1.pdf
- Boditrak (2016). Product Information retrieved from: http://www.boditrak.com/products/bt1510.php



