Volume 26 Number 1
An unusual case study: Collaborative management of an atypical wound
Chloe Cara
Keywords Cancer, debridement, Skin lesion, venous leg ulcer, nurse practitioner.
Abstract
Venous leg ulcers (VLU) are a complication of chronic venous insufficiency (CVI). As well as completing a comprehensive wound assessment, practitioners strive to find a dressing that is cost-effective, increases wound healing rates and optimises a patient’s holistic care. This case study depicts a multidisciplinary team approach between a nurse practitioner wound consultant and a plastic reconstructive surgeon, to avoid surgical debridement in a patient with multiple co-morbidities: arterial fibrillation (AF), type 2 diabetes, osteoporosis, anticoagulation therapy and osteoarthritis. The case demonstrated the importance of a thorough wound assessment, as well as a collaborative approach to investigations, incorporating an innovative perspective. This, in turn, allowed the patient, Mrs B, to avoid ceasing anticoagulant therapy, have limited adverse effects in relation to opioids, and therefore remain independent throughout her atypical diagnosis to continue to healing.
Introduction
Chronic venous insufficiency (CVI) is categorised as insufficiencies within the veins, related to any one or a combination of: valvular obstruction or incompetence, trauma, renal impairment and cardiac disease4. This accumulation results in an increase in pressure in the venous system, causing venous hypertension4. This increased pressure can cause the skin to break down, causing venous leg ulcers4. Although VLUs on average account for approximately 80% of wounds in Western countries, they can be incorrectly diagnosed4. For example, in 10% of patients, skin cancers are mistakenly categorised as venous leg ulcers5.
As well as completing a comprehensive wound assessment, practitioners strive to find a dressing that is cost-effective, increases wound healing rates and optimises a patient’s holistic care. The following case study illustrates how a patient avoided repeated surgical debridement, with an atypical diagnosis, while maintaining holistic, patient-centred care.
Method
This report represents a single case study of a patient attending a wound clinic from April to September 2016. All the information presented in the case study was obtained from the patient’s medical record and does not present a deviation from usual data capture in the course of clinical care. Patient consent to publish the episode as an anonymous case study was sought and documented in writing in the patient’s record.
Results
Mrs B’s history
Mrs B is an 88-year-old female who reported an abrasion to her left lower calf, posteriorly, while donning her class 2 compression stockings. Mrs B has a history of VLU and peripheral vascular disease, in which she independently dons her compression stockings every morning. Mrs B is on anticoagulation therapy (warfarin) for her arterial fibrillation (AF). Prior to this episode, Mrs B had two episodes of VLU: one in 2013, which took just under a year to heal; and a second in 2015, which took 12 weeks to heal.
For the current episode, Mrs B self-inititated povidone iodine and first aid dressings daily, in which there was no progress. During this time, Mrs B also decided to keep her compression stockings off to avoid additional trauma. After four days, however, Mrs B was concerned the abrasion was increasing in size. Mrs B told her daughter what happened and her daughter promptly rang the clinic to request a wound review.
Wound assessment
April 2016
Upon consultation, Mrs B’s abrasion was not progressing to proliferation in the way that the nurse practitioner (NP) was familiar with from Mrs B’s past history. Mrs B was further reporting an excessive amount of haemoserous exudate and pain that was not characteristic of her past VLU episodes. The NP ordered pathology to review Mrs B’s clotting status, inflammatory markers, and overall health status. In addition to this, the NP was able to attend a Doppler ultrasound and duplex scan, with a vascular surgeon, to confirm the vascular status had in fact not changed since her previous review a year ago.
In the interim, Mrs B’s treatment approach was to protect the abrasion to assist granulation, using a foam dressing, and class 1 compression therapy, as tolerated by Mrs B, whilst awaiting for the pathology results. Mrs B’s wound management involved home visits twice-weekly by the NP. After the NP received the investigative pathology results, there was no further suggestion of abnormalities, yet the wound itself did not look like a typical VLU, similar to those the NP had treated Mrs B for in the past. The wound continued to remain stagnant in migration, from 2 cm diameter to 2 cm diameter in the space of three weeks, despite the wound looking clean, with maintenance of exudate management and a normal wound swab PCR result. Further investigations were sought to find out why Mrs B’s wound was not migrating, in the form of a punch biospy which was sent for histology.
10 May 2016
Post referral to a plastic surgeon the punch biopsy took place with no complications. For Mrs B, the recommended therapeutic guidelines were followed for the management of her anticoagulation therapy and further wound investigation6. The histology results revealed a malignant spindle cell neoplasm with features favouring atypical fibroxanthoma. By this stage the wound was presenting with slight nodules. The awareness of the difference between nodules and usual hypergranulation observed previously in Mrs B’s case could be detected because of the continuity in care Mrs B had received, documentation with patient consent to use photos to keep continuity in the wound assessment, and the advanced chronic wound assessment skills of the clinician, the NP.
Following the diagnosis, Mrs B had a whole body skin check. After closer inspection, another suspicious lesion on the same lower leg was found, anteriorly. This lesion was also biopsied and histology reported the same result, a malignant spindle cell neoplasm with features favouring atypical fibroxanthoma, which also required surgical excision.
20 May 2016
Mrs B was admitted for excision and skin graft. This appeared to be successful, in which Mrs B had one donor site and two graft areas, both anterior and posterior. The instruction from the surgeon and NP was to the hospital to attend the skin graft dressing daily after three days postoperatively and leave the donor site intact for seven days. The donor site went on to heal with no concern or complication.
Unfortunately, Mrs B’s dressing was left on postoperatively for 10 days, because of miscommunication in the nurses' handover as an inpatient, on both skin graft site, which resulted in 100% necrosis and failure of both skin grafts. This caused further severe pain in these areas for Mrs B. In fact, the combination of analgesia, Targin, Panadol Osteo and Endone were not relieving her pain at all, which, in turn, caused confusion and insomnia.
June 2016
For Mrs B, the option of conservatively sharp debriding by the NP, of the necrotic tissue would have caused severe, unbearable pain, even with breakthrough medication pre-dressing changes. For Mrs B to have further surgical debridement in her case related to the anaesthetic and anticoagulation regime, this was not a viable option. Therefore, an alternative approach to autolytically debride Mrs B’s wound and reduce the risk of infection was explored.
HydroClean Plus (Hartmann) was commenced. In the core of HydroClean Plus, bacteria are killed by an antiseptic polyhexanide (polyhexamethylene biguanide or PHMB) which continually deposits to autolytically debride the wound bed for up to 72 hours3. Mrs B’s dressing was changed every three days by the NP in Mrs B’s home. Mrs B was educated on the signs and symptoms of infection to report if they occurred.
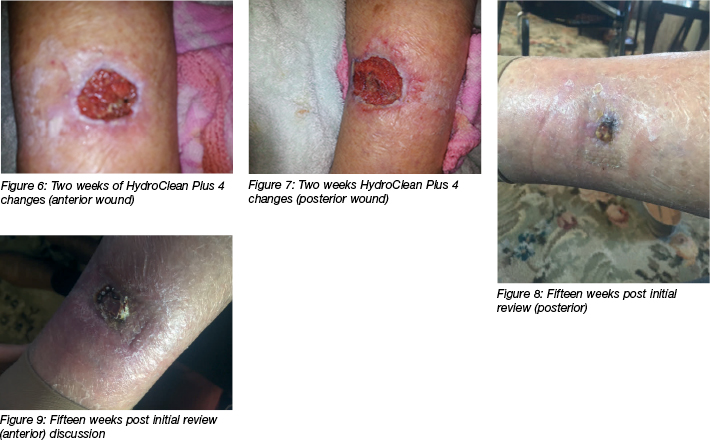
As per figures 4 and 5, the results demonstrated a significant decrease in the necrotic tissue, illustrating granulating tissue migrating through the wound bed. Even though the wound size had increased, the stimulation of proliferation and a healthy wound edge migration was evident within only three days for both wounds. Following treatment of HydroClean Plus, Mrs B decreased from Targin and Endone, as pain relief pre or post her dressing change was no longer required. This enabled Mrs B to regain her mobility and sleep, as well as not having her day revolve around her wound management regime.
Mrs B avoided another hospital admission for surgical debridement and therefore avoided the need to cease her anticoagulation therapy, which would have altered her anticoagulation profile significantly and impacted her overall cardiovascular health of AF, congestive cardiac failure and hypertension.
Mrs B went on to heal completely within 17 weeks from the initial treatment. Her progress is depicted after 15 weeks in Figures 8 and 9. Treatment with HydroClean Plus was continued until week 3, in which a hydrofibre and protective foam, changed twice weekly, were instigated as the regime. This regime included compliance with her class 1 compression stockings daily. Mrs B’s ongoing wound care has continued with a good skin care regime and compression therapy compliance. Because of the atypical carcinoma lesions, Mrs B now goes back for skin checks every 12 weeks. Since the first finding of her atypical lesion proving suspicious, the NP and plastic surgeon have prevented a further 10 suspicious carcinomas. The reason why Mrs B has a high prevalence of skin carcinomas is unclear.

Discussion
The NP endorsement allows one to work autonomously and provide advanced continuity in patient care. In wound management, in particular, one main part of the wound assessment, that being the wound bed preparation itself, still remains subjective. The wound bed preparation is often a description based on the tissue viability the NP sees during their visit, to then dictate the goals of care and treatment. In Mrs B’s case, because the NP had advanced knowledge of her past history, the normal appearance and her healing pattern, along with the combinations of medication management she was on, the NP knew the presenting wound was atypical.
In Mrs B’s case, the small size, yet appearance of exudating haemoserous with little to no trauma, along with the raised appearance, did not appear to be the usual presentation in which Mrs B reacted to skin trauma, nor was it the normal way Mrs B would bleed, despite being on anticoagulation therapy. This was further questioned in the NP’s mind, when the wound did not respond to the wound dressing regime, as it usually would.
Usually in the community, patients can wait anywhere from four to eight weeks for further investigations when a wound is not progressing6. The Australian and New Zealand Society for Vascular Society5 suggests that 10% of wounds with suspected VLU origin upon investigation have carcinoma aetiology. For Mrs B, having an NP with a collaborative care model with a plastic surgeon meant that Mrs B was able to recieve the correct investigations in a timely manner. For Mrs B, in this instance, it meant prompt care was important to avoid the risk of further morbidity or mortality.
For Mrs B postoperatively, it was imperative to manage her pain, her polypharmacy from multiple co-morbidities, and new increased pain, along with avoiding further surgery. Mrs B had known mild kidney impairment, along with diabetes, and warfarin therapy, so any further operations meant at least a two-week preparation time, and a four- to six-week stabilisation time of her coagulation profile post operation. Therefore, Mrs B needed all treating practitioners to work cohesively together, combined with a dressing that did not create additional bleeding to interrupt her coagulation profile, yet would debride, relieve pain and assist to reduce her risk of infection, due to her surgery and history of type 2 diabetes. HydroClean Plus was an added success in reducing the affects of polypharmacy, such as constipation, and falls risk being on opioids.
In this case study, the wound healed successfully. HydroClean Plus was used with good effect to progress the wound to heal, and was a pain management solution for Mrs B.
Mrs B went on to heal completely, with minimal indention in her lower leg after 16 weeks. Mrs B has stepped up to comply with her class 2 compression therapy, independently, with no wound recurrences.
Conclusion
Often practitioners gather past history of a patient and automatically start treatment based on past wound management. This case study demonstrated the importance of a comprehensive history, examination and cohesive, investigative, where sharps debridement requiring anaesthetic, due to Mrs B’s multiple comorbidities was not a viable option, to provide an alternate holistic approach.
Acknowledgements
The authors would like to acknowledge Paul Hartmann for their alternative approach that encompassed the patient’s needs. A special thank you to Mrs B for consenting to her case and photos being part of the case study and overall wound management education in the community.
Conflicts of Interest
There is no conflict of interest that needs to be noted. Treatment was commenced from the best clinical judgement of the nurse practitioner, not from any endorsements or recommendations, nor was funding support received from a for-profit enterprise.
Author(s)
Chloe Cara
MNursing/Nurse Practitioner; PhD (C), La Trobe University; Grad Cert Diabetes Education; CDE: ADEA Member and Mentor; Grad Cert Women’s Health; Healthcare United Owner;
Swinburne University Lecturer
Email healthcareunited1@gmail.com
References
- MacGregor L. Principles of compression in venous disease: A practitioner’s guides to treatment and prevention of venous leg ulcers. Wounds Int 2013.
- Al Shammeri O, Al Hamdan N, Al-hothaly B, Midhet F, Hussain M, Al-Mohaimeed A. Chronic venous insufficiency: prevalence and effect of compression stockings. Int J Health Science 2014;8:3: 231–6.
- Hartmann. Management of chronic wounds. Retrieved from: https://www.hartmann.info/en-AU/medical-knowledge/wound-management/Management-of-chronic-wounds. 2017
- Velnar T, Bailey T, Smrkolj V. The wound healing process: An overview of the cellular and molecular mechanisms. J Int Med Res 2009;37:1528–40.
- The Australian and New Zealand Society for Vascular Surgery. Chronic venous insufficiency and leg ulcer. Retrieved, URL: http://www.anzsvs.org.au/patient-information/chronic-venous-insufficiency-and-leg-ulcers. 2018
- Australian Family Physician. Patients and technology. 2014; Retrieved, URL: https://www.racgp.org.au/afp/2014/december/new-oral-anticoagulants-and-perioperative-management-of-anticoagulantantiplatelet-agents/



