Volume 26 Number 2
Skin tear prevention in elderly patients using twice-daily moisturiser
Karen Finch, Rebecca Osseiran-Moisson, Keryln Carville, Gavin Leslie and Miriam Dwyer
Keywords skin tears, moisturiser, rehabilitation, acute/subacute.
Abstract
Skin tears increase morbidity and implicit and explicit costs for the individual and the health care system. A 580-bed private hospital in Brisbane undertook a prospective interventional study and results were compared to historical controls. A purposive sample of patients aged 65 years or older were invited to participate. The intervention was twice-daily application of pH-friendly, non-perfumed moisturiser to the extremities. The primary outcome measure was the average monthly incidence of skin tears. Monthly skin tear incidence rates were calculated as number of skin tears/patient-occupied bed days × 1000. Overall, 762 eligible patients were enrolled in the intervention group and their outcomes were compared with 415 patients in the historical control group. In total, 104 patients developed at least one skin tear (intervention group: n=60, the control group: n=44). An overall 185 skin tears were reported (mean=1.79 skin tears/patients, SD=1.55, range=19). The average monthly incidence rate in the intervention group was 4.35 per 1000 occupied bed days (96 skin tears over 12 months) which was significantly lower (p=0.006) than those found in the historical control group of 6.61 per 1000 occupied bed days (89 skin tears over 6 months). The results indicate the efficacy of twice-daily application of moisturiser when applied to the extremities of elderly patients for the prevention of skin tears.
Introduction
Greenslopes Private Hospital (GPH) is a 580-bed hospital in Brisbane, Queensland. Historically, the hospital was used for the care of repatriated returned servicemen and maintains strong links with the veteran community. As a result, the hospital has a high proportion of elderly patients and skin tears are reported to be the most common wound found amongst the elderly1. The skin is the largest body organ and morphological and physiological changes that occur with ageing impair skin function and increase its vulnerability to trauma2. In particular, the thinning of the epidermis by as much as 50%, flattening of the dermo-epidermal junction, atrophic changes to the dermis due to reduction and disintegration of collagen and elastic fibres and thinning of the adipose tissue layer lead to impaired strength and fragility3. Impaired skin barrier function and reduced production of sweat and lipids results in dryness and dry, wrinkled skin is less resilient to friction and shear3,4. In addition, elderly patients are likely to heal more slowly due to these morphological and physiological skin changes, the effects of increased co-morbidities and the use of certain medications5.
Prior to this study, the only data available on skin tear occurrence within the hospital was retrieved from the Riskman™ Incident Reporting System. An analysis of data from a three-year period (2008–2010) obtained from the Riskman System showed that an average of 384 incidents resulted in an average of 462 skin tears per year, 93% of which were in patients over the age of 65. To gain further information about the extent of the problem, a skin tear survey was conducted among all patients 65 years or older who were admitted to the hospital over the six-month period from July to December 2011. During this period, a total of 178 patients were involved in 249 incidents, resulting in 372 skin tears (GPH unpublished data). The data collected in this study demonstrated that 38% of the skin tears resulted from a fall, and 33% from friction/shear injuries; and they predominately (90%) occurred on the arms and legs.
In order to reduce the number of skin tear incidents, the hospital proposed to test the effectiveness of the twice-daily application of moisturiser to the extremities of elderly hospitalised patients in anticipation that a significant reduction in skin tears would be demonstrated. In a previous Western Australian study the application of twice-daily moisturiser to the extremities of aged care residents demonstrated almost 50% reduction in skin tear incidence6.
Methodology
Study design, setting and sample
A prospective intervention study was conducted and compared to historical controls. A purposive sample of patients aged 65 years or older and who were patients in either of two wards in this private Brisbane hospital were invited to participate in the study. Historical data concerning skin tears for patients in these two wards were available from a six-month period study conducted in 2011. These two wards contained a total of 75 beds: 45 beds in the rehabilitation ward and 30 in the acute/subacute ward, and they were selected because the proportion of skin tears for patients in these wards during the control period was high. Patients were admitted to the rehabilitation ward in order to optimise their health and functional independence. The acute/subacute ward was dedicated to the care of elderly patients who were recovering from an acute stage of illness, but were not yet ready to undertake intensive rehabilitation activities. Patients in the acute/subacute ward may have had cognitive and/or behavioural deficits.
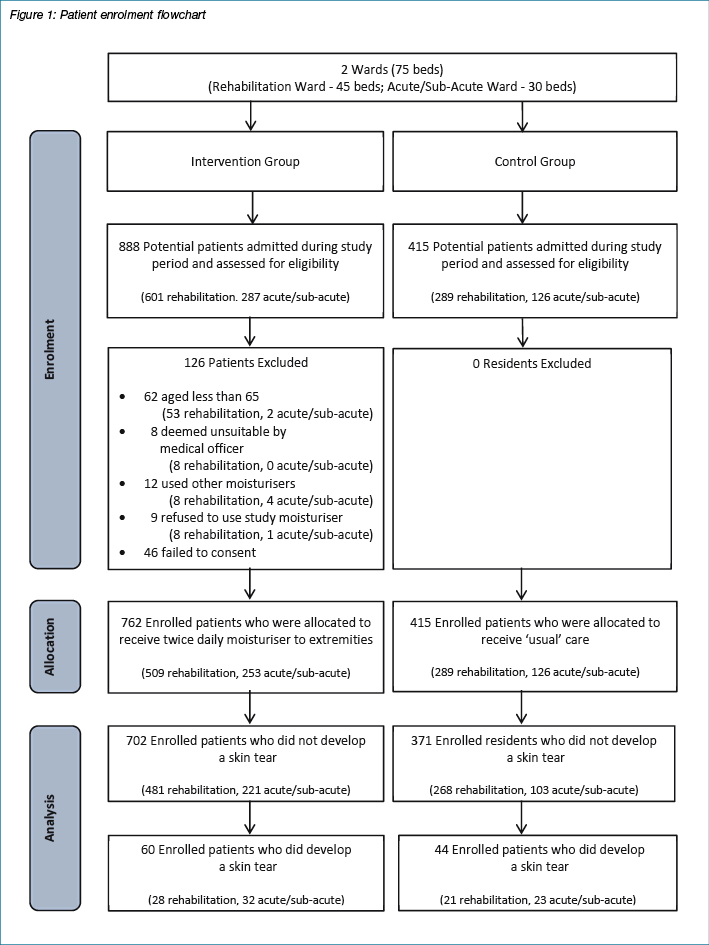
Verbal consent to participate in the study was sought from patients or their nominated representative. Patients excluded were: a) those who declined to consent; b) had a day admission to the rehabilitation ward; c) who were deemed unsuitable by medical officer for any reason; and d) who are unable to have the standardised study moisturiser applied due to conflicting medical conditions such as skin allergies or those receiving treatment for other skin conditions (see Figure 1 for enrolment flowchart). Ethics approval was granted by the Greenslopes Hospital Ethics Committee and the Wound Management Innovation Cooperative Research Centre (WMI CRC) funded the study.
Study intervention
The intervention involved a twice-daily application of non-perfumed, pH-friendly moisturiser (QV Skin Lotion from Ego™ Pharmaceuticals) to the arms and legs of participating patients (Table 1 presents the ingredients of the QV Skin Lotion®). Care staff on both wards received training regarding the study protocol and application of moisturiser. The ward staff conducted a skin integrity assessment on admission. Each patient and/or their relative received written information about the study and ongoing skin care. Care staff applied the moisturiser twice daily to the patients’ extremities in line with the study protocol. However, patients and/or their relatives were encouraged to apply the moisturiser independently if they were capable of doing so. Patients and/or relatives willing to apply the moisturiser received education on application so that application methods were standardised. The time of application of moisturiser was recorded with each application.
Table 1: Contents of the moisturiser used in the study
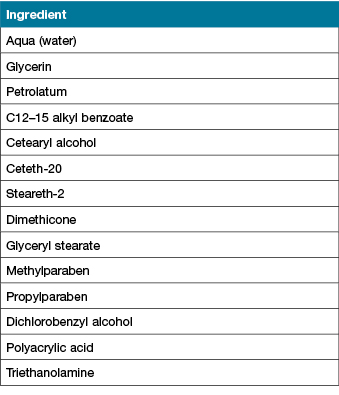
*Contents provided by Ego™ Pharmaceutics
Data collection
The intervention study took place over 12 months from January to December 2013, while the historical control study took place over six months from July to December 2011. During the control study, there was no protocol in place in either ward for routine application of a standard moisturiser.
Patients’ demographic and health profile data were extracted from patients’ files and recorded in an electronic data management system while skin tear data were collected by trained hospital staff. Data were de-identified and checked for accuracy. Measurements included in the study were patient age; gender; current ward; pressure ulcer risk assessment (using the Waterlow Scale7); patient falls risk status; cognitive status; skin characteristics such as dry or discoloured; number of skin tears; day and time of skin tear occurrence; anatomical location of skin tears; the STAR Skin Tear Classification8; factors which may have contributed towards a skin tear (assessed by a staff member following discussion with the patient) and the ward location where the skin tear(s) occurred.
Primary outcome
The primary outcome measure was the average monthly incidence of skin tears. Monthly skin tear incidence rates were calculated as number of skin tears/resident occupied bed days × 1000.
Data analysis
Statistical analyses were performed with IBM SPSS for Windows, Version 23. Descriptive statistics (frequencies and percentages for categorical variables; means, standard deviations, and ranges for variables measured on a continuous scale) were used to analyse responses in the study. When appropriate, Chi-square, independent samples T-tests and Mann-Whitney U tests were used to compare skin tear occurrences between groups (control/intervention) and wards (rehabilitation and acute/subacute). A p-value of <0.05 was taken to indicate a statistically significant association in all tests.
Results
Overall, 762 eligible patients were enrolled in the intervention group of the study, and their outcomes were compared with 415 patients in the historical control group. In total, 104 patients developed at least one skin tear (intervention group: n=60, in the control group: n=44).
Patients profile
Recruited numbers of males and females were almost equally represented in both the intervention and control groups (p=0.891). Overall, patients were aged in their late eighties. However, patients in the intervention group were older (p=0.009) than those in the control group (Table 2). In particular, patients in the control group in the acute/subacute ward (mean age=87.9 years, SD=4.3) were older (p=0.016) than those in rehabilitation ward (mean=84.1, SD=5.7). There was no statistical difference (p=0.146) in ages in the intervention group between wards (acute/subacute ward: mean=89.94, SD=4.84; rehabilitation ward: mean=87.82, SD=6.26).
The Waterlow Score was performed for pressure injury risk and was found to be similar in both groups (p=0.249). Patients were identified as mainly at ‘high risk’ (38.8%, n=40). However, the proportion of patients at ‘risk’ and at ‘very high risk’ were alike. Additionally, almost all patients (89.83%, n=53) in the intervention group were identified to be at high risk of falls compared to 34.09% (n=15) in the control group (p <0.001). Moreover, in both groups (p >0.05), they mostly used a wheelie walker as a mobility aid (p=0.170) and one-third of them (p=0.249) used a pressure relief aid (Table 2).
Table 2: Patients' profile by group
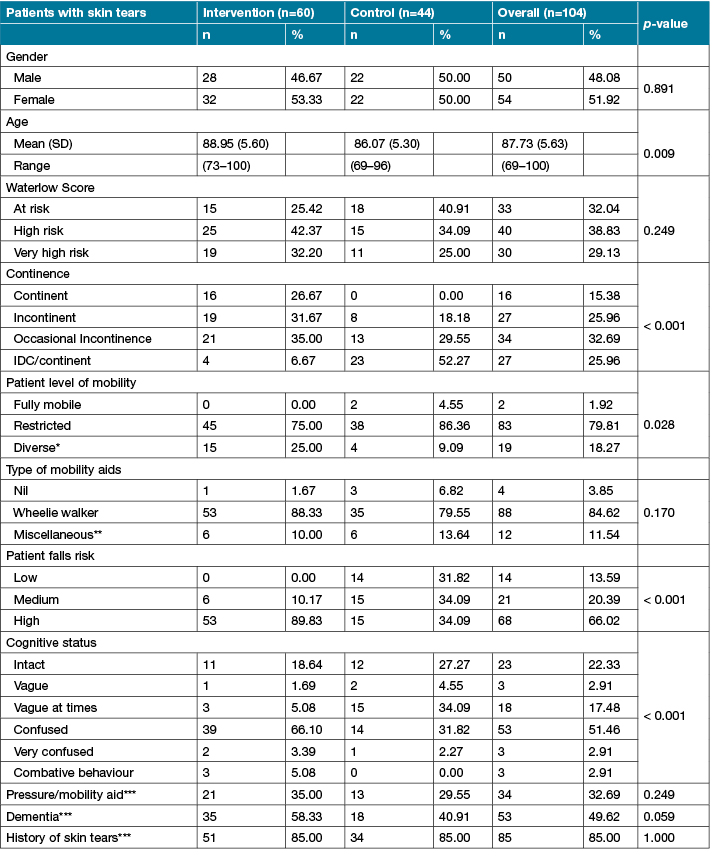
* Diverse refers to apathetic, inert/traction, unsteady gait, chairbound, bedbound, restless/fidgety
** Miscellaneous refers to crutches, hoist, walking stick, wheelchair, other
*** Yes answers
Note: 1 missing data in intervention phase for: Waterlow Score, fall risk, cognitive status — 4 missing data in control phase for history of skin tears
Patients in the intervention group were more (p <0.001) ‘occasionally’ or ‘fully incontinent’ and more confused (p <0.001) than those in the control group. Despite the statistical difference (p=0.028) in level of mobility between groups, almost all patients experienced a restricted level of mobility. Of borderline statistical significance, patients in the intervention group tended to be more likely to have dementia than those in the control group (Table 2).
In the control group, patients in the acute/subacute ward were more (p=0.019) confused (47.83%, n=11) and had more (p=0.030) dementia (56.52%, n=13) than those in the rehabilitation ward respectively (14.29%, n=3; 23.81%, n=5).
Skin tear incidence
An overall total of 104 patients developed at least one skin tear during this study (60 patients in the intervention group and 44 in the control group). An overall of 185 skin tears were reported (mean=1.79 skin tears/patients, SD=1.55, range=19). The average monthly incidence rate (Table 3) found in the intervention group was 4.35 per 1000 occupied bed days (96 skin tears over 12 months) which was significantly lower (p=0.006) than those found in the historical control group 6.61 per 1000 occupied bed days (89 skin tears over 6 months).
Table 3: Average monthly incidence by ward across groups and overall wards
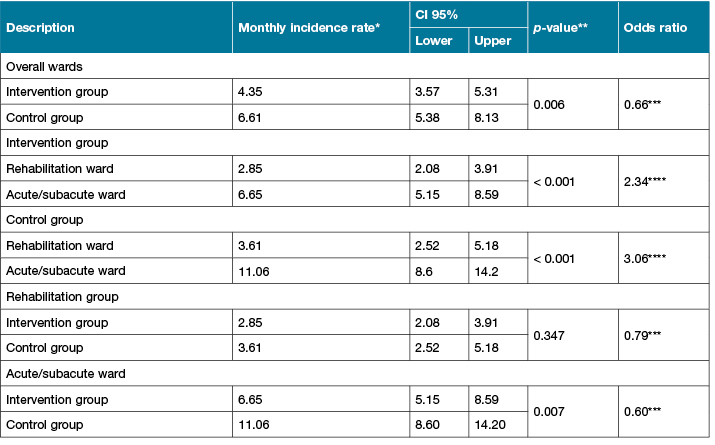
* Incidence rate per 1000 occupied bed days
** p-value significant at 0.05
*** Incidence rate of control group/Incidence rate of Intervention group
**** Incidence rate of acute/subacute ward/Incidence rate of rehabilitation ward
It is noteworthy to mention that in both groups (Table 3), the average monthly incidence rates of skin tears in the rehabilitation ward (intervention group: 2.85, control group: 3.61) were lower (p <0.001) than those in the acute/subacute ward (intervention group: 6.65, control group: 11.06). Although, the average monthly incidence rates between groups were similar (p=0.347) in the rehabilitation ward. However, in the acute/subacute ward, the average monthly incidence rate in the intervention group (6.65) was 0.6 times lower (odds ratio=0.60, p=0.007) than the control group (11.06).
Skin characteristics associated with skin tears
Only one patient in the control group was reported to have ‘healthy’ skin associated with a skin tear. All other patients in both groups (p >0.05) had morphological or physiological skin changes and almost all patients’ skin was reported to be dry (98.92% overall groups, p=0.171) (see Table 3).
Skin characteristics more commonly (p >0.05) reported in the intervention group were: discoloured (100%); ecchymosis (97.92%); tissue paper appearance (83.33%); presence of previous scarring (90.63%); and senile purpura (55.21%). As compared to those most commonly reported in the control group which were respectively: 70.79%, 30.34%, 34.83%, 5.62% and 20.22%. In both groups the proportion of skin with oedema, erythema, pruritus, clammy, haematoma and lentigines were marginal (Table 3).
Table 4: Skin characteristics associated with skin tears (sorted by descendant overall %)
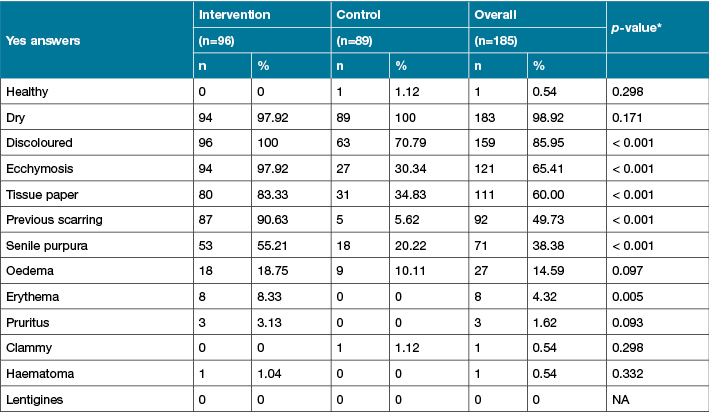
* p-value significant at 0.05
Anatomical location
Skin tears (Figure 2) were mainly located in the upper (55.14%) and lower limbs (37.84%). Skin tears occurring in other parts of the body were limited (7.03%). When anatomical skin tear locations were collapsed, more (p=0.042) skin tears occurred on locations other than limbs (11.46%) in the intervention group than in control group (2.25%). However, extremities remained the dominant location (Table 5).
Figure 2: Overall skin tears anatomical locations
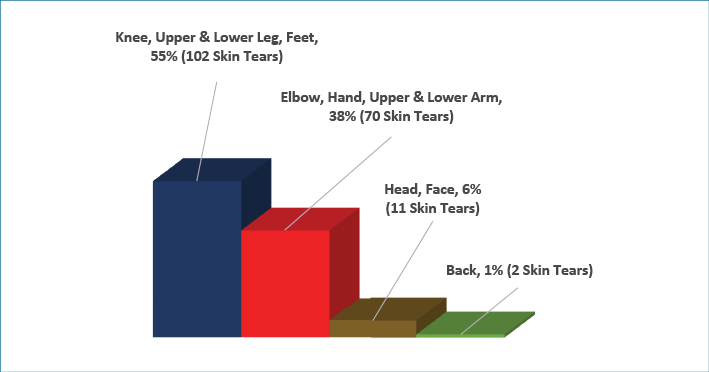
Table 5: Anatomical locations for skin tears collapsed by groups*
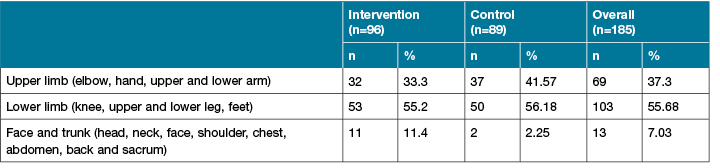
*Significant difference amongst phases (p=0.042)
STAR Skin Tear Classification
Skin tears in both groups (p=0.600) were mainly STAR Skin Tear Classification categories 1a and 1b (71.07%). The STAR 3 category represented 4.96%. It is noteworthy to mention that in both groups one-third of skin tears were not assessed (or unknown) using the STAR categorisation (Table 6).
Table 6: STAR Skin Tear Classification by group*
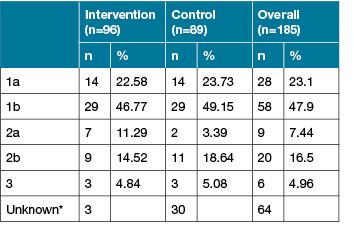
*No significant difference amongst groups (p=0.600)
** Unknown excluded from the %
The intervention group patients in the acute/subacute ward had more (p=0.007) category STAR 2 a, 2b and 3 (33.33%, n=14) than those in rehabilitation ward (25.00%, n=5).
Contributory factors
The contributory factors assessed by staff to be associated with skin tears were mainly due to ‘friction/shear’ in both groups. However, this contributory factor was more (p <0.001) common in the intervention group (77.08%) than in the control group (40.45%). The proportion of the unknown contributory factors was smaller (11.46%) in the intervention group than in the control (20.22%) group (Table 7).
Table 7: Contributory factors for skin tears by group*
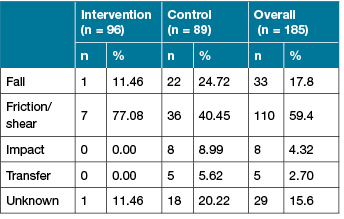
*Significant difference amongst groups (p <0.001)
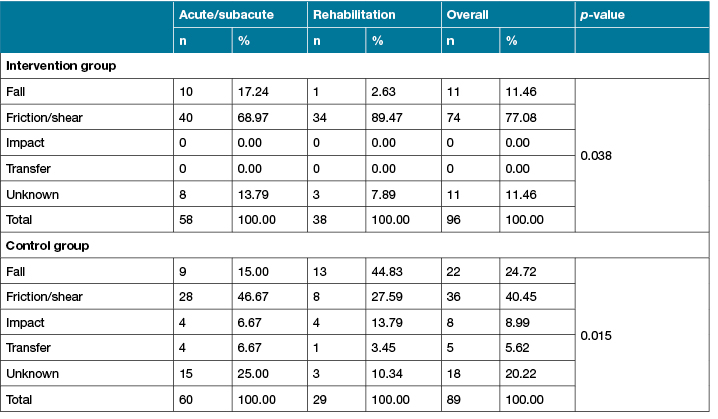
Across the two wards and groups, there were variations in the proportion of skin tears due to friction/shear or fall as a contributory factor (p<0.5). There were less unknown contributory factors in the rehabilitation ward in both the intervention and control groups as compared to those in the acute/subacute ward. In addition, no impact or transfer contributed to a skin tear in the intervention group (Table 8).
Table 8: Contributory factors for skin tears across groups and wards
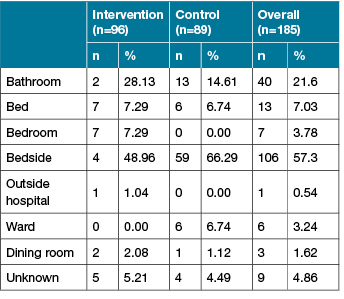
Locations where skin tears occurred
In both the intervention and the control group, skin tears occurred mainly at the bedside (57.30%) and in the bathroom (21.62%). However, the proportion between these two locations varied (p <0.001) between groups. In addition, few skin tears happened in bed (7.03%) or in the dining room (1.62%) (Table 9).
Table 9: Location where skin tears occurred by group*
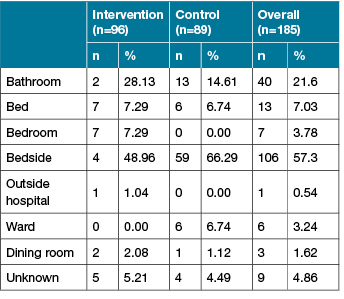
*Significant difference amongst groups (p <0.001)
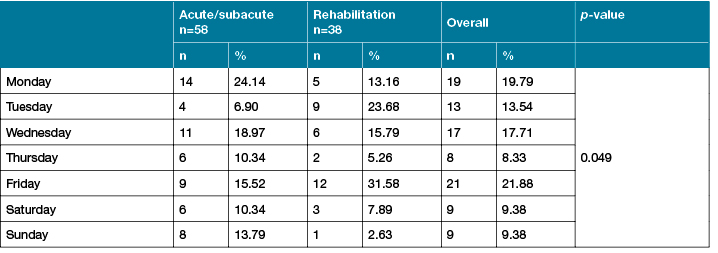
Weekday and time when skin tears occurred
Overall results of in the intervention and the control group (p=0.174), more skin tears occurred on Tuesday (19.46%, n=36), Friday (17.84%, n=33) and Monday (17.30%, n=32) than on Wednesday (14.59%, n = 27), Thursday (9.19%, n=17), Saturday (12.43%, n =23) and Sunday (9.19%, n=17). In addition, overall groups (p=0.129), skin tears occurred more commonly during the hours from 8.00 to 14.00 (Figure 3).
Figure 3: Times when skin tears occurred
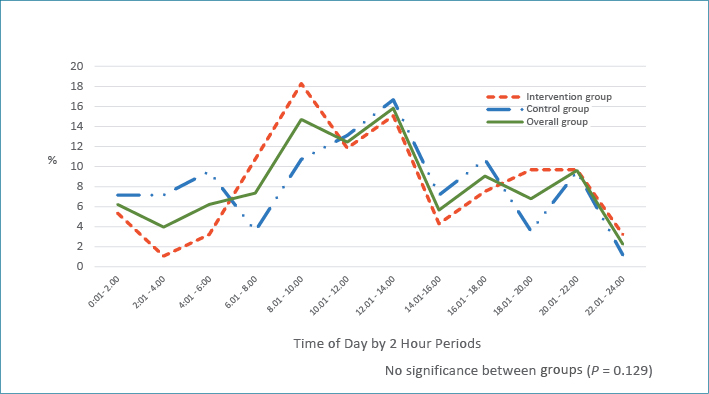
More specifically, in the intervention group, at the edge of significance (p=0.049), Monday and Wednesday were weekdays when skin tears occurred most frequently in the acute/subacute ward as compared to Tuesday and Friday in the rehabilitation ward (Table 9). Mainly skin tears occurred in the acute/subacute ward throughout the morning (6 am) until early afternoon (14.00) and during the evening (18.00) until bedtime (22.00), while in the rehabilitation ward they occurred more commonly during the morning (8.00) until early afternoon (14.00) (Figure 3).
Table 9: Location where skin tears occurred by group*
*Significant difference amongst groups (p < 0.001)
Table 10: Weekday when skin tears occurred in intervention group
Discussion
The average monthly incidence rate in the intervention group was 4.35 per 1000 occupied bed days (96 skin tears over 12 months) which was significantly lower (p=0.006) than those found in the historical control group with 6.61 per 1000 occupied bed days (89 skin tears over 6 months). There were 1.5 fewer skin tears overall/1000 occupied bed days in the intervention group as compared to the control group which was significant (p=0.006). This study produced similar findings to the Western Australian study, which demonstrated the use of twice-daily moisturiser reduced skin tears by almost 50% in 14 residential aged care facilities6 and together both studies highlight the benefits associated with moisturiser use in elderly individuals, regardless of health care setting. There was, however, a difference found between the two wards. The incidence rate in the intervention group was lower in the rehabilitation ward as compared to the acute/subacute ward (OR=2.34), which equated to 2.34 fewer skin tears/1000 occupied bed days in the rehabilitation ward as compared to those in the acute/subacute ward (p<0.001). A similar finding was noted in the control group for the rehabilitation ward which had 3.06 less skin tears as compared to the acute/subacute ward (R=3.06, <0.001). However, the patients in the acute/subacute ward control group were noted to be older and they had a higher number of patients with confusion or dementia.
With the exception of the one patient in the overall control group who was reported to have “healthy” skin associated with a skin tear, all other patients were found to have had significant morphological or physiological skin changes associated with ageing and skin tears. The most commonly reported skin characteristics, many of which have also been reported by other authors to be associated with skin tears, were discoloured skin; ecchymosis9,10; fragile or tissue paper appearance6,9,10; previous scarring11,12; and senile purpura12. Overall patients in the intervention group had more of these clinical presentations than patients in the control group. In addition, almost all were reported to have dry skin (xerosis cutis) (98.92% overall groups, p=0.171), which is a common presentation amongst elderly individuals due to intrinsic and extrinsic factors such as: environmental exposure to sun and wind, alterations in the skin’s barrier function and transepidermal water loss, reduction in lipids and decreased numbers of sweat and sebaceous glands3,4,13. Dry skin is subject to injury, pruritis and infection13. The use of moisturisers, especially on dry skin, helps maintain skin hydration and sustains and repairs skin barrier function14.
Skin tears occurred primarily on the upper extremities (55.14%) followed by the lower extremities (37.84%), which is reflected in the findings of other skin tear researchers6,9,12,15. The cause of the predominance of skin tears on the upper verses lower extremities in a hospitalised patient population is open to speculation. However, as few of the injuries happened in bed and 57.30% of the skin tears occurred at the bedside and 21.62% in the bathroom, it appears that they are more likely to be associated with manual handling when patients are assisted in and out of bed or with bathing. This possible explanation is also reflected in the finding that most of the skin tears occurred during the busy patient handling times between 0800 and 1400 (p=0.129), and again between 1800 and 2200 in the acute/semi-acute ward when some patients would be assisted back to bed and settled for the night. The increase in skin tears during peak patient handling times replicates the finding of Carville et al.6 in their study.
However, other contributory factors were identified and could be an associated influence. There were found to be more patients in the overall intervention group (both wards) who were at higher risk of falls and more confused or suffering from dementia, as compared to the overall control group. Falls and impaired cognition are well-recognised factors for increased risk of skin tears11,16.
It was interesting to note that more skin tears occurred on Monday, Tuesday and Friday in both the intervention and control groups, but no insight as to why this was the case could be ascertained from the data. A limitation of this study relates to the fact that the population was recruited from two wards in one hospital. It is recommended that further studies be conducted across all wards and units and across other hospitals.
Conclusion
Skin tears are traumatic wounds found commonly amongst elderly individuals, regardless of health care setting. They constitute considerable pain and loss of quality of life for the individual and implicit and explicit costs to the individual and the health care system. Moreover, they have the potential to become significant chronic wounds in a vulnerable population. This study has produced evidence to support the benefits of twice-daily application of moisturiser to the extremities of elderly hospitalised patients when the aim is to reduce skin tear incidence. This relatively low-cost intervention has the potential to reduce health care costs and improve care outcomes.
Acknowledgements
The authors would like to acknowledge the support of the Wound Management Innovation Cooperative Research Centre, the Australian Government’s Cooperative Research Centres Program and to Ego™ Pharmaceuticals who generously provided moisturiser for the project. The authors are indebted to Bronwyn Casey who assisted with data collection, Carolyn Wilson and team from the rehabilitation ward and Tina Coetzee and the team from the subacute ward, without whom this project would not have been possible.
Author(s)
Karen Finch
RN
Greenslopes Private Hospital, QLD, Australia
Rebecca Osseiran-Moisson
MPhil
Curtin University, WA, Australia
Keryln Carville
RN, PHD
Curtin University, WA, Australia
Silver Chain Group, WA, Australia
Gavin Leslie
RN, PhD
Curtin University, WA, Australia
Miriam Dwyer*
Greenslopes Private Hospital
Newdegate Street
Greenslopes, QLD 4120, Australia
Email DwyerMiriam@ramsayhealth.com.au
* Corresponding author
References
1. Rayner R, Carville K, Leslie G, Roberts P. A review of patient and skin characteristics associated with skin tears. J Wound Care 2015;24(9):406–414.
2. Ratcliff CR, Fletcher KR. Skin tears: a review of the evidence to support prevention and treatment. Ostomy Wound Manage 2007;53(3):32–4
3. Zouboulis C, Makrantonaki E. Clinical aspects and molecular diagnostics of skin aging. Clin Dermatol 2011;29:3–11.
4. Seyfarth F, Schliemann S, Antonov D, Elsner P. Dry skin, barrier function, and irritant contact dermatitis in the elderly. Clin Dermatol 2011;29:31–36.
5. Carville K. Wound Care Manual, 7th edn. Osborne Park WA: Silver Chain Foundation, 2017.
6. Carville K, Leslie G, Osseiran-Moisson R, Newall N, Lewin G. The effectiveness of a twice-daily skin moisturising regimen for reducing the incidence of skin tears. Int Wound J 2014;11:446–453.
7. Waterlow J. A risk assessment card. Nurs Times 1985;81(48):49–55.
8. Carville K, Lewin G, Newall N, Haslehurst P, Michael R, Santamaria N, Roberts P. STAR: a consensus for skin tear classification. Primary Intention 2007;15(1):18–28.
9. Lopez V, Dunk AM, Parke J, Larkin D, Trudinger M, Stuart M. Skin tear prevention and management among patients in the acute aged care and rehabilitation units in the Australian Capital Territory: a best practice implementation project. Int J Evid Based Healthc 2011;9:429–434.
10. Everett S, Powell T. Skin tears: the underestimated wound. Primary Intention 1994;2:8–30.
11. LeBlanc K, Christensen D, Cook J et al. Prevalence of skin tears in a long-term care facility. J Wound Ostomy Continence Nurs 2013;40(6):580–584.
12. Lewin GF, Newall N, Alan JJ, Carville KJ, Santamaria NM, Roberts PA. Identification of risk factors associated with the development of skin tears in hospitalised older persons: a case–control study. Int Wound J 2016;13(6):1246–1251.
13. Blume-Peytavi U, Kottner J, Sterry W et al. Age associated skin conditions and diseases: current perspectives and future options. Gerontology 2016;56(S2):S230–S242.
14. Barr JE. Skin matters: impaired skin integrity in the elderly. Ostomy Wound Manage 2007;52(5). Retrieved 2 March 2018 from: http://www.o-wm.com/content/impaired-skin-integrity-elderly
15. Malone M, Rozario N, Gavinski M, Goodwin J. The epidemiology of skin tears in the institutionalised elderly. J Am Geriatr Soc 1991; 39 (6):591-595.
16. Koyano Y, Nakagami G, Iizaka S et al. Exploring the prevalence of skin tears and skin properties related to skin tears in elderly patients at a long-term medical facility in Japan. Int Wound J 2016;13(2):189–97.



