Volume 26 Number 4
Case study: Collaboration across the care continuum to improve the patient experience
Therese Jepson, Tanya O’Hara and Susan Monaro
Keywords Venous leg ulceration, concordance, model of care, communication and collaboration.
Abstract
This case study illustrates the importance of collaboration in complex care across the hospital–community continuum to improve the patient experience The team engaged the patient by building rapport and trust, providing education, and implementing evidence-based care. These contributed to better outcomes for this patient, who had severe chronic venous leg ulceration and poor treatment concordance. Our objectives were to promote ulcer healing and increase treatment concordance by engaging the patient. Engagement was achieved by enhanced communication and the use of technology such as digital photography and advanced wound therapies. The provision of support, education and assessment of advanced skills competence of clinicians across the care continuum achieved our objectives.
What is already known:
- Venous leg ulcers are prevalent and costly.
- Evidence-based care across the care continuum is problematic.
What this manuscript contributes:
- A better understanding of the multiple factors which contribute to patient outcomes in venous leg ulcers.
- A case study to demonstrate an evolving model of care to integrate care for patients with complex wounds.
Introduction
Venous insufficiency is the most common cause of venous leg ulcers (VLUs), and it has been estimated that 1.7% of people aged over 65 years have a VLU1. The growing number of aged persons worldwide may result in increased incidence of VLU. This chronic disease may impact on an already overstretched healthcare budget2. The average cost of VLU treatment per patient in Australia was estimated in 2012–13 to be $81063. A joint position statement of the European Wound Management Association and Wounds Australia has advocated for cost-effective, evidence-based treatments to reduce VLU incidence4. This comprehensive review identified that compression therapy remained the most effective form of non-invasive therapy for VLUs. However, patient compliance with this treatment remains an issue and is often a barrier to ulcer healing5. A recent study found, through surveying stakeholders, that clinicians do not engage the patient’s trust and they are not included in the discussion of treatment options or rationale5. Moffatt6 stated that non-concordance is likely to reflect a poor relationship between the patient and practitioner. Cheng et al.3 also identified that poor communication and cooperation by health providers can reduce access to the level of care required to achieve positive outcomes and results in poor continuity of evidence-based treatment and preventative care along the health service continuum.
However, patient concordance with this therapy is often a barrier to ulcer healing7-9 with no definitive interventions that have proven successful in improving treatment concordance in VLUs8. We implemented strategies to improve patient concordance, which included the utilisation of digital photography and wound bed preparation as part of the patient’s management plan to facilitate healing of a recurrent ulcer in a patient with poor concordance. The aged care rapid response team clinical nurse consultant (ARRT CNC) and the hospital-based wound nurse ensured patient-centred care with continuity was achieved. This paper outlines specific strategies to improve patient concordance to VLU management and demonstrates the importance of collaboration across the hospital and community care continuum.
Case study
Bill (a pseudonym) was an 84-year-old male who had been living in a residential aged care facility (RACF) for the past five years. He required assistance with hygiene and transferring from bed to chair; however, while he was physically frail, his cognitive health was good and he was able to make his own decisions. He recently scored 30/30 on the mini mental examination. He was socially isolated, choosing not to mix with other residents, but enjoyed talking to staff. With the need for ongoing wound care more one-to-one time with staff was possible. His medical history included osteoarthritis, affecting mainly his hips and knees and he had developed peripheral neuropathy, secondary to type 2 diabetes which had further reduced his mobility. His type 2 diabetes was controlled with oral medications and his recent HbA1c was 8.4. Target values for HbA1c in the older residential aged care population is slightly higher than for those younger or fitter persons living with diabetes in the general community10. According to the McKellar Guidelines, an HbA1c of up to 8.5 is acceptable in the frail, older person. He was not on any medications that significantly impacted on wound healing. He also had mild congestive cardiac failure, which was well controlled, and a long history of chronic venous insufficiency and recurrent lower leg ulcerations. Previous VLUs had healed with compression but had recurred 18 months previously. He had refused compression since this recurrence, stating: "the bandages were too tight" and "too expensive". He was unaware that compression was effective in preventing ulcer recurrence.
The clinicians in his RACF had been attempting to manage his bilateral VLUs, but over the last three months his legs had deteriorated significantly. The right leg ulcer was much larger than the left and increasing levels of exudate made this difficult to manage due to strike-through. He had increased wound-related pain, causing him to become irritable and socially withdrawn, and this was thought to be contributing to his poor concordance.
Bill was directing his care, insisting on the use of cheap but ineffective dressings, despite the ongoing deterioration of his ulcers. The RACF clinicians had acquiesced to this because "he had the mental capacity to make decisions". In the weeks prior to his hospital admission, staff had resorted to using disposable nappies to contain the exudate at his direction. He eventually developed bilateral lower leg cellulitis and became systemically unwell and was transferred to an acute hospital for assessment and treatment.
Assessment
On admission, a full medical history, blood tests, and wound cultures were obtained. Blood profile indicated an elevation in inflammatory markers. C-reactive protein (CRP) was elevated at 44 mg/L (normal range 0–5 mg/L), his white cell count was normal (9.9 9/L) but he was mildly anaemic with an Hb of 110 g/L (normal range for males of 140–174 g/L) which may have affected wound healing11. The wound culture grew Pseudomonas aeruginosa. Bill was commenced on intravenous antibiotics to treat the systemic infection. Knowing he had previously been non-concordant with treatment, it was suggested that he would benefit from a joint review by the hospital wound nurse and community-based ARRT CNC to develop a plan that could be implemented across the continuum.
A holistic wound assessment was done in accordance with best practice12-14. Lower limb assessment revealed Bill had extensive bilateral lower leg VLUs, pitting oedema and erythema extending to above the knees. The skin showed evidence of chronic vascular disease: venous eczema and haemosiderin staining. Distal pulses were non-palpable, but popliteal pulses were present. This may have been due to significant pedal oedema. Capillary refill was slow at >2 seconds. The ulcers were painful, and he required analgesia prior to dressings and regularly throughout the day. Local wound assessment included conventional parameters and capture by digital photography. The exudate was thick and both wounds were malodorous. The wound bed was sloughy, with thick, adherent, yellow slough and the edges were rolled. The surrounding skin was warm with erythema extending 5 cm beyond the ulcer margin.
An ankle brachial pulse index (ABPI) was performed by the ARRT CNC to assess peripheral arterial perfusion14. Bill’s ABPIs were reduced with an index of 0.6 on the right leg and 0.4 on the left. However, these results were not considered reliable in the presence of medial arterial calcification, which can occur in people with diabetes15. Inaccurate measurement may also have resulted from oedema and extensive ulceration, which made it difficult to apply and inflate the blood pressure cuff, without causing pain. An additional assessment by the hospital podiatrist of toe brachial pressure index (TBPI) was done. The TBPI provides an indication of small artery function, is less painful to perform and is a more sensitive measure in the presence of medical arterial calcification in peripheral artery disease (PAD) in people with diabetes, compared to ABPI16. The right TBPI was 0.96, which confirmed adequate perfusion and indicated suitability for compression therapy, but the left TBPI of 0.38 confirmed arterial insufficiency and this leg required specialist review. Typically, TBPI thresholds used are 0.6, which indicate wound healing capacity and the safety for careful compression. In light of the abnormal pressure indexes arterial duplex ultrasonography was organised in preparation for a review by a vascular specialist. This demonstrated extensive occlusive disease in the left superficial femoral artery (SFA) and minor, diffuse disease in the right leg. Specialist consultation for opinion for both the safety and level of compression and possible need for revascularisation to the left leg followed. A plan included a recommendation for conservative (non-operative management) to the left leg and compression17 therapy to the right leg only. It was decided that it would be better and perhaps increase concordance, if compression was initially applied at a lower pressure to reduce pain and to overcome Bill’s anxiety and resistance to the reintroduction of compression therapy.
The treatment plan was slowly implemented with ongoing dialogue with Bill to support his knowledge and understanding of the processes. The plan was to manage the pain with analgesia, bed rest and systemic antibiotic therapy until better control of pain was achieved and then initiate compression at reduced levels. He had a follow-up ambulatory care review planned with the vascular specialist. For the purposes of this case study, we have only focussed on the right leg.

Figure 1: Initial assessment 16 March 2017.
Wound Management Objectives
1. Reduce bacterial load
The appropriate intravenous antibiotic therapy for the systemic infection was commenced in hospital, and a topical antimicrobial cleansing agent was used to reduce the bacterial load in the wound bed13.
2. Remove non-viable tissue
Non-viable tissue delays wound healing, and debridement can be beneficial18; however, in Bill’s case even with the application of topical local anaesthetic and systemic analgesics, this was still too painful. A trial of negative pressure wound therapy with installation (NPWTi) was planned to remove non-viable tissue. A solution is instilled into the wound bed intermittently and cycled negative pressure is applied, which liberates slough. NPWTi is a new treatment option in our service and has not been available in community settings to date.
3. Contain exudate
Excessive exudate results in enzymatic degradation and maceration of the peri-ulcer skin. Containment prevents deterioration of the peri-ulcer skin19. NPWT is proven to be beneficial in exudate management as long as the surrounding skin is protected, and clinicians are educated in the application and use of the device.
Management Plan
The management plan had three elements: building rapport and trust, education, and implementing evidence-based VLU care.
1. Building rapport and trust
It was essential to build Bill’s trust in the clinicians who were providing care. The ARRT CNC and the hospital-based wound nurse worked in close collaboration with each other to engage the patient and clinicians across the care continuum. His poor eyesight meant that he could not see the ulcers, but the use of digital photography, and the zoom function allowed him to visualise the improvements week by week. Every time the dressing was done, photographs were taken of the wound and then shown to Bill. The zoom function allowed Bill to see the small islands of epithelisation and the nurses could show previous images to reinforce that healing was progressing well. The images provided clarity and were used as an educational tool for him and clinicians, to reinforce wound management and therapeutic compression therapy. Bill was included in discussions, and his opinions listened to. This strategy enabled the delivery of evidence-based care to Bill who had previously had bad experiences and was resistive to compression therapy. The RACF clinicians managed his VLUs on his return home were supported by the community-based ARRT CNC. This contact helped to promote Bill’s trust in the RACF clinicians’ ability to manage the ulcer.
2. Education
Education, didactic and printed, was provided to both Bill and the RACF clinicians about VLU pathophysiology and management by the ARRT CNC. Bill was encouraged to ask questions, so he could understand the science underpinning wound management and compression therapy. By maintaining a non-judgemental attitude and being careful not to criticise his previous decisions, we instead created learning opportunities for Bill. The RACF clinicians were given training, and this allowed consistent care and communication. Bill observed clinicians being mentored and upskilled in the technical aspects of his ulcer management
Compression therapy learning packages were given to the RACF clinicians to complete. The ARRT CNC conducted two in-house compression therapy workshops, which led to a better understanding and application of compression therapy. The RACF clinicians could practise bandage application in a workshop setting and then were assessed by the ARRT CNC in the correct application of compression bandaging on Bill’s lower leg. Bill seemed to enjoy being part of the teaching program and he became confident in the ability of the RACF nurses to safely apply compression. Achieving competence increased not only their clinical skills but also increased confidence of the clinicians in their ability to provide complex care.
3. Evidence-based care
The severity of the ulcers required consideration of advanced wound therapies such as NPWT. Although having successfully used NPWT within our facility to treat cavity wounds, we had not utilised this modality in leg ulceration. While there is some evidence to suggest that NPWT is useful for deep wounds20, there is less evidence for its use in VLUs21. Technological advancements in NPWT allows the automated and controlled delivery of wound cleansing solutions to enhance wound bed preparation. The NPWT selected uses a reticulated foam wound contact layer, which mechanically removes debris during the alternating pressure delivery cycles22. The intermittent instillation of the solution helps to cleanse and debride the wound bed, while the negative pressure is designed to remove and contain the exudate. NWPTi can be used to facilitate debridement of devitalised tissue and cleansing of infected wounds22. We chose to use polyhexanide biguanide (PHMB) antimicrobial solution for instillation, which is active against gram-negative and gram-positive bacteria, including multiresistant organisms23,24.
Once we explained the possible benefits of this therapy, Bill agreed to trial NPWTi. He was prescribed additional analgesia before dressing changes, and therapy was commenced on 16 March to the right leg. The NPWTi dressings were changed by either the ARRT CNC or the hospital wound nurse. Education was provided to the patient and the ward-based clinicians to ensure therapy was maintained. Initially, Bill complained of increased pain, so the pressure was reduced from 125 mmHg to 75 mmHg which helped to better control his pain. Dressings were changed at 48-hour intervals.
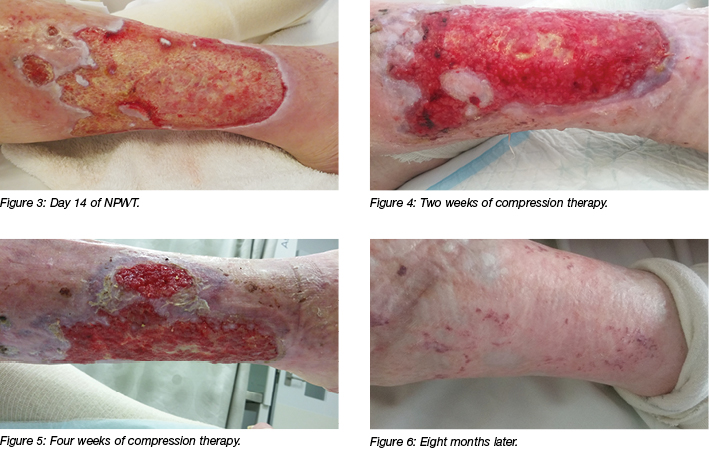
On 20 March after five days of intravenous antibiotics and four days of NPWTi, his condition improved and he was discharged home. NPWTi is not available in community settings. However, expected superior results were anticipated if NPWT could continue, so he was discharged with standard NPWT. The ARRT CNC agreed to provide education and support to the RACF clinicians. Dressings were scheduled so that either the ARRT CNC or the wound nurse would be present at the twice-weekly dressing changes to monitor the progress and support the RACF clinicians until they felt confident. NPWT was continued in the RACF for a further 25 days.

Figure 2: Day 4 of NPWTi.
The next stage in Bill’s plan of care was to initiate compression therapy. Compression bandaging was commenced on 18 April and was well tolerated. A cost-effective, washable, reusable elastic bandage with a visual application guide was selected as the preferred product. This long-stretch bandage over an underpadding layer would not only achieve the correct sub-bandage pressure, but it also gave Bill some control. If Bill found the compression too tight, the outer bandage could be removed immediately and reapplied at slightly reduced pressure. This feature made it more cost-effective than a single-use bandage system which may not have been able to be adjusted. Bill also felt more confident that clinicians would apply it correctly if they had a visual guide to follow13. Long-stretch bandages are also more effective than short-stretch bandages, particularly in patients with reduced mobility and poor calf muscle pump7. Compression therapy reduced his pain by reducing oedema. This fed into a cycle of improved satisfaction, engagement and concordance. Evidence suggests that concordance increases if people are prescribed the highest level of compression that they will tolerate9.
Twice-weekly dressings continued, using the antimicrobial PHMB solution to cleanse the ulcers before the application of an iodine-impregnated primary dressing. A highly absorbent pad was used as a secondary dressing, followed by a sub-bandage layer of padding and then the compression bandage. Improvements in ulcer characteristics and surface area were evident at each dressing change and sustained the confidence of the patient and clinicians.
After six weeks of sustained therapeutic compression and twice-weekly dressing changes, the right leg ulcer had decreased in size to 10 cm in length (from 18 cm) and 4.5 cm in width (from 12 cm). The oedema had reduced, and the limb size and shape had returned to normal. Exudate levels were minimal and he no longer required analgesia. The ulcer healed over eight months. Prophylactic compression therapy was discussed to reduce the risk of ulcer recurrence. Evidence suggests that ongoing compression therapy may reduce VLU recurrence rates, but there is insufficient evidence as to which method provides better prophylaxis9. Bill was given information on compression garments and wraps and shown samples to assist him to make a decision as to which type of compression he would use when his ulcers had healed. Evidence suggests that patient satisfaction with a garment is vital for compliance25.
Conclusion
Collaboration between hospital and community clinicians was a factor in improving the patient experience and facilitated treatment options that may otherwise have not been considered. VLU healing was sustained once Bill’s trust and confidence in clinicians was established. The initial use of NPWTi triggered healing whilst digital wound photography enabled the patient and the clinicians to visualise improvements in the ulcer. This positive reinforcement facilitated the continuation of optimal treatment and achieved VLU healing. The provision of education and competency assessment of the RACF clinicians in compression therapy increased the patient’s confidence and the RACF clinicians' knowledge and skill levels. Specific strategies to increase patient engagement and confidence in the care team were important. Bill’s new understanding of the treatment rationale subsequently increased his satisfaction and concordance. Understanding a person’s previous experiences may increase the chance of successful interventions and help to develop strategies for better concordance. Chronic VLUs require a patient-centred but evidence-based approach to care. This case study has demonstrated three elements that contributed to a better patient experience: building rapport and trust, education, and evidence-based care. Communication and collaboration between the patient and the clinicians involved in his care enabled these elements to be achieved across the care continuum. This case highlights the need for further research in this area, in particular the upskilling of RACF staff who are at the forefront of wound care in their facilities; however, they require more support to gain skills in the management of complex wounds.
Ethics
This case study was approved as part of a research project by the Ethics Committee of the Northern Sydney Local Health District. The participant’s consent was obtained for the publication of the images.
Disclosure of interests
The authors have no conflicts of interest to report.
Funding
The authors received no funding for this study.
Author(s)
Therese Jepson
RN, BN (Nursing), MN (Clinical Nursing & Teaching)
Aged Care Rapid Response Clinical Nurse Consultant
North Shore–Ryde Health Service
NSW, Australia
Tanya O’Hara
RN, BAppSc (Nursing), Acute Care Cert and Stomal Therapy Graduate Cert
Wound and Stomal Therapy Clinical Nurse Specialist 2
Ryde District Hospital
NSW, Australia
Susan Monaro*
RN, BAppSc (Nursing), MN and PhD(C)
Skin Integrity Improvement Facilitator
Northern Sydney Local Health District
Clinical Lecturer
Sydney Nursing School, University of Sydney
NSW, Australia
Email sue.monaro@health.nsw.gov.au
* Corresponding author
References
- Kelechi TJ, Johnson JJ, Yates S. Chronic venous disease and venous leg ulcers: an evidence-based update. J Vasc Nurs 2015;33(2):36–46.
- Pugliese DJ. Infection in venous leg ulcers: considerations for optimal management in the elderly. Drugs Aging 2016;33(2):87–96.
- Cheng Q, Gibb M, Graves N, Finlayson K, Pacella RE. Cost-effectiveness analysis of guideline-based optimal care for venous leg ulcers in Australia. BMC Health Serv Res 2018;18(1):421.
- Franks PJ, Barker J, Collier M, Gethin G, Haesler E, Jawien A, et al. Management of Patients With Venous Leg Ulcers: Challenges and Current Best Practice. Journal of Wound Care. 2016;25(Sup6):S1-S67.
- Pacella R, Tulleners R, Cheng Q, Burkett E, Edwards H, Yelland S et al. Solutions to the chronic wounds problem in Australia: A call To action; 2018.
- Moffatt CJ, Franks PJ, Doherty DC, Martin R, Blewett R, Ross F. Prevalence of leg ulceration in a London population. QJM 2004;97(7):431–7.
- O’Meara S, Cullum N, Nelson EA, Dumville JC. Compression for venous leg ulcers. Cochrane Database Syst Rev 2012;11.
- The Wound Healing and Management Node Group, Li Y. Venous Leg Ulcers (Compression Therapy): Patient Adherence. Joanna Briggs Institute; 2017.
- Nelson EA, Bell‐Syer SE. Compression for preventing recurrence of venous ulcers. The Cochrane Library; 2014.
- Dunning T. The McKellar guidelines for managing older people with diabetes in residential and other care settings. 2014.
- Wright JA, Richards T, Srai SK. The role of iron in the skin and cutaneous wound healing. Front Pharmacol 2014;5:156.
- Harding K, Gray D, Timmons J, Hurd T. Evolution or revolution? Adapting to complexity in wound management. Int Wound J 2007;4(s2):1–12.
- Franks PJ, Barker J, Collier M, Gethin G, Haesler E, Jawien A et al. Management of patients with venous leg ulcers: challenges and current best practice. J Wound Care 2016;25(Supp 6):S1–S67.
- Australian Wound Management Association Inc. and the New Zealand Wound Care Society Inc. Australian and New Zealand Clinical Practice Guideline for Prevention and Management of Venous Leg Ulcers. Osborne Park: Cambridge Publishing; 2011.
- Fahey V. Vascular Nursing. 4th edn. Fahey VA, editor. St Louis Missouri: Sanders; 2004.
- Hoyer C, Sandermann J, Petersen LJ. The toe-brachial index in the diagnosis of peripheral arterial disease. J Vasc Surg 2013;58(1):231–8.
- Dougherty D. Arterial Ulcers. In: Bryant RA, Nix DP, editors. Acute & Chronic Wounds: Current Management Concepts. 5th edn. New York: Elsevier Health Science; 2015.
- International Wound Infection Institute. Wound infection in clinical practice. Wounds International. 2016.
- Vowden P, Bond E, Meuleneire F. Managing high viscosity exudate. Wounds UK 2015;11(1):56–60.
- Apelqvist J, Willy C, Fagerdahl A-M, Fraccalvieri M, Malmsjö M, Piaggesi A et al. EWMA Document: Negative Pressure Wound Therapy. J Wound Care 2017;26(Supp 3):S1–S154.
- Dumville JC, Land L, Evans D, Peinemann F. Negative pressure wound therapy for treating leg ulcers. The Cochrane Library. 2015.
- Back DA, Scheuermann-Poley C, Willy C. Recommendations on negative pressure wound therapy with instillation and antimicrobial solutions — when, where and how to use: what does the evidence show? Int Wound J 2013;10(s1):32–42.
- Cutting K, Hermans M, Kwonlee S, Wolcott R, Treadwell T. Key considerations in choice of wound management therapeutics — a USA perspective. 2013.
- Kim PJ, Attinger CE, Oliver N, Garwood C, Evans KK, Steinberg JS et al. Comparison of outcomes for normal saline and an antiseptic solution for negative-pressure wound therapy with instillation. Plast Reconstr Surg 2015;136(5):657e–64e.
- Powell G, Wicks G, Will K. Managing venous leg ulcers using compression therapy and dressings. Br J Nurs 2015;24:S42.



