April 2018
Question
What is the best available evidence on collagen-based dressings for improving wound healing outcomes in adults?
Summary
Collagen-based dressings are advanced wound dressings that provide an extracellular matrix to support tissue and microcirculation growth. Collagen dressings are able to change the wound biochemistry through modulation of protease activity, creating an environment more favourable for healing1 (Level 1). Oxidised regenerated cellulose (ORC) is commonly combined with collagen to create a collagen-based composite dressing with enhanced ability to reduce protease activity (Level 4).2 Collagen dressings are designed for wounds with stalled healing2, 3 (Levels 4 and 5).
There is limited evidence on efficacy and no recent cost effectiveness studies for collagen-based dressings. Available evidence, mostly conducted on venous leg ulcers (VLUs), indicates that collagen-based dressings are at least as effective in improving healing as other contemporary wound dressings4-7 (Level 1).
Best practice recommendations
Use collagen-based dressings when a wound (particularly a venous leg ulcer) displays stalled/delayed healing (Grade B).
The following considerations are recommended for using collagen-based dressings:
- Wound dressings should be reviewed third daily (or more frequently for moderate-heavy wound exudate). If there is gel residue from the collagen dressing remaining on the wound bed/secondary dressing the collagen dressing should remain untouched until the next review.2, 10 (Level 4 and 5).
- Collagen-based dressings are recommended for four weeks’ treatment. If inadequate healing has occurred, a review of the individual’s full management plan should be conducted. If the wound is healing after four weeks, a contemporary dressing can be used2 (Level 4).
- Collagen-based dressings can be used to prepare a wound bed prior to skin grafting10 and for wounds showing clinical signs of infection10 (Level 5).
- Optimising the individual’s condition (e.g. nutrition) and the wound bed (e.g. with cleansing, debridement and/or infection management) is essential to promoting healing with any wound dressing2, 10 (Level 4 and 5).
- Collagen-based dressings are not recommended for wounds with dry eschar, or active vasculitis10 (Level 5).
Background
Collagen dressings are biological dressings developed from animal collagen. Collagen is a protein produced by fibroblasts that has a role in all stages of wound healing. Collagen is a major component of the extra-cellular matrix, providing strength. Both collagen and ORC, with which collagen is frequently combined, also reduce protease activity.2 Proteases have numerous roles in wound healing, but usually decrease as the wound heals. In chronic and/or infected wounds, inflammation can lead to continuously high protease levels. This can damage new tissues, contributing to delayed healing.1, 2 Collagen-based dressings are designed to modulate protease activity8, 9 and to balance wound moisture,10 while providing a mechanical scaffold for tissue growth and angiogenesis.8, 9 This promotes cell proliferation and stimulates microcirculation, providing a favourable healing environment.8, 9 Oxidised regenerated cellulose (ORC) is considered to have haemostatic properties, which may decrease wound bleeding.10
Evidence
Collagen dressings
There is some evidence that collagen dressings are at least equivalent to other contemporary wound dressings for treating venous leg ulcers.4-7 A systematic review4 reported from one small trial (n=22)5 that when compared to daily application of a topical antiseptic, a collagen dressing was associated with greater likelihood of reduction in VLU area after 26 days (odds ratio [OR] 26.6, 95% confidence interval [CI] 2.3 to 308)4, 5 (Level 1). A small trial (n=40) showed statistically significant greater reduction in VLU area after 12 weeks treatment with a collagen dressing 45% compared with an alginate dressing 20% (p<0.001).6 There was no difference in the per cent of VLUs fully healed at 12 weeks (approximately 25% in each group)6 (Level 1). In another small trial with non-healing VLUs (4 participants per group), the percent reduction after four weeks of treatment was similar for a collagen plus foam dressing (mean reduction 31.8%, range 28% to 34%) compared to a regular foam dressing (mean reduction 26.4%, range 17.3% to 32%)9 (Level 1). Another study that included VLUs (n=12) found a collagen dressing was associated with significantly shorter time to complete healing compared with polysaccharide beads (36 days versus 60 days, p<0.005) for VLUs7 (Level 1).
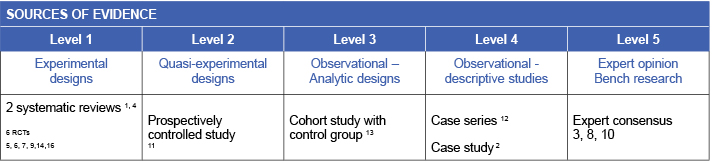
There is limited evidence that collagen dressings are at least equivalent to conventional wound dressings for treating diabetic foot ulcers (DFUs). When a collagen dressing was compared to moistened gauze, healing time was significantly faster with collagen (4.63±1.18 weeks versus 7.79±1.61 weeks, p=0.001) (Level 2).11
Limited evidence is available on efficacy for collagen for treating pressure injuries (PIs). In a small trial (n=12 PIs), a collagen dressing was associated with significantly shorter time to healing (20 days versus 47 days, p<0.001) than the comparison polysaccharide bead treatment.7 (Level 1).
Evidence on efficacy of collagen dressing for treating burns is also available. Partial thickness burns (n=42) took an average of 18.5 days to reach complete re-epithelisation (average 40.5 days for four full thickness burns in the study) when managed with a collagen dressing. The authors reported none, or only mild to moderate scarring after six months for most participants.12 (Level 4).
Another study (n=120) included wounds of various aetiology (chronic and acute) in a retrospective comparison of collagen dressing versus conventional dressings designed to manage infection (e.g. iodine, honey, topical antibiotics). There was no significant difference in the percent of wounds in each group that completely healed after six weeks (collagen 70% versus conventional 63%, p=0.22). There was also no difference in percent of wounds reaching at least 75% closure by eight weeks (p=0.21). Wounds treated with a conventional dressing were more likely to require a split skin graft (25% versus 13%, p=0.04). Swab cultures were more favourable in the wounds treated with collagen dressings; however, none of the wounds were reported to have clinical signs of infection at trial commencement or thereafter13 (Level 3).
Oxidised regenerated cellulose (ORC)/collagen dressings
There is some evidence that ORC/collagen dressings are at least equivalent to other contemporary wound dressings for treating VLUs.14-16 In the largest trial (n=73), an ORC/collagen dressing used for non-healing VLUs was associated with a non-significant 20% better improvement in wound condition (p=0.079) than a non-adherent dressing. The greater reduction in ulcer surface area that the ORC/collagen dressing group showed at 12 weeks compared to the control group was significant (average decrease 54.4%±10.9 versus 36.5%±11.4, p<0.0001) (Level 1).14 A small trial (n=27) showed that an ORC/collagen dressing was not significantly different from hydrocolloid dressing for decreasing wound size over 12 weeks. There was a favourable association between the collagen-based dressing and reductions in protease activity16 (Level 1). An ORC/collagen dressing was shown to be associated with significantly greater reduction in VLU area over 12 weeks compared with another protease modulating matrix dressing with nano-oligosaccharide factor (NOSF) as the active ingredient (mean area reduction 54.4% versus 12.9%, p=0.0029)15 (Level 1).
Methodology
The development of this evidence summary is based on the Joanna Briggs Institute methodology.17
A structured database search using variations of the search terms collagen, protease-modulating and wound dressings was employed. Searches were conducted in EMBASE, Medline, Google Scholar and the Cochrane Library for evidence from 2000 to February 2018 in English. Two systematic reviews1, 4 that conducted searches covering pre-2000 identified few additional studies to the current search – these pre-2000 studies were included in this summary. The evidence review did not include biological dressings in which collagen was combined with other active ingredient besides ORC (e.g. silver
Author(s)
Haesler E. for JBI Wound Healing and Management Node
References
- Westby MJ, Norman G, Dumville JC, Stubbs N, Cullum N. Protease-modulating matrix treatments for healing venous leg ulcers. Cochrane Database of Systematic Reviews, 2016;Issue 12:Art. No.: CD011918. (Level 1.b evidence).
- Grothier L. Understanding the use of collagen/oxidised regenerated cellulose dressings Wounds Int, 2015;6(2):34-40. (Level 4.d evidence).
- Cullen B, Ivins N. Promogran™ & Promogran Prisma™ Made Easy. Wounds Int, 2010;1(3):Available from http://www.woundsinternational.com. (Level 5.c evidence).
- Bradley M, Cullum N, Nelson E, Petticrew M, Sheldon T, Torgerson D. Systematic reviews of wound care management: (2) dressings and topical agents used in the healing of chronic wounds. Health Technology Assessment, 1999;3(17 II): iii-126. (Level 1.b evidence).
- Tosti A, Veronesi S. Treatment employing collagen in ulcers. [Ruolo del collagene nel processo di riparazione delle ferite.]. G Ital Derm Venereol, 1983;118(5):289-92. (Level 1.c evidence).
- Romanelli M, Mulder G, Paggi B, Macchia M, Panduri S, Dini V. The use of a collagen matrix in hard-to-heal venous leg ulcers. Journal of Wound Care, 2015;24(11):543-7. (Level 1.c evidence)
- Palmieri B. Heterologous collagen in wound healing: a clinical study. Dextranomer vs lyophilized collagen sponge. Int J Tissue React, 1992;14(Suppl):21-5. (Level 1.c evidence).
- Fleck CA, Simman R. Modern collagen wound dressings: Function and purpose. J Am Col Certif Wound Spec, 2010 2(3):50-4. (Level 5.c evidence).
- Andriessen A, Polignano R, Abel M. Monitoring the microcirculation to evaluate dressing performance in patients with venous leg ulcers. J Wound Care, 2009 18(4):145-50. (Level 1.c evidence).
- 1Wu S, Applewhite AJ, Niezgoda J, Snyder R, Shah JP, Cullen B, Schultz G, Harrison J, Hill R, Howell M, Speyrer M, Utra H, de Leon J, Lee W, Treadwell T. Oxidized regenerated cellulose/collagen dressings: Review of evidence and recommendations. Advances in Skin & Wound Care, 2017;30:S1-S81. (Level 5.b evidence).
- Rao H, Pai A, Hussein I, Arun A, Ram HS, Pai A, Pai SR, Pain SG. A comparative study between collagen dressings and conventional dressings in wound healing. Int J Collab Res Intern Med Public Health, 2012;4(5):611-23. (Level 2.c evidence).
- Yang HT, Yim H, Cho YS, Kim D, Hur J, Chun W, Kim JH, Seo CH, Lee BC, Koh JH. Treatment of deep second degree burn wound using heterogenic type I collagen dressing. J Korean Burn Soc, 2010 13(2):136-9. (Level 4.c evidence).
- Singh O, Singh Gupta S, Soni M, Moses S, Shukla S, Kumar Mathur R. Collagen dressing versus conventional dressings in burn and chronic wounds: A retrospective study. J Cutan Aesthet Surg, 2011;4(1):12-6. (Level 3.c evidence).
- Vin F, Teot L, Meaume S. The healing properties of Promogran in venous leg ulcers. J Wound Care, 2002;11:335-41. (Level 1.c evidence).
- Schmutz J, Meaume S, Fays S, Ourabah Z, Guillot B, Thirion V, Collier M, Barrett S, Smith J, Bohbot S, Dompmartin A. Evaluation of the nano-oligosaccharide factor lipido-colloid matrix in the local management of venous leg ulcers: results of a randomised, controlled trial. International Wound Journal, 2008;5(2):172-82. (Level 1.c evidence).
- Smeets R, Ulrich D, Unglaub F, Woltje M, Pallua N. Effect of oxidised regenerated cellulose/collagen matrix on proteases in wound exudate of patients with chronic venous ulceration. Int Wound J, 2008;5(2):195-203. (Level 1.c evidence).
- The Joanna Briggs Collaboration. Handbook for Evidence Transfer Centers – Version 4. The Joanna Briggs Institute, Adelaide. 2013.



