Volume 27 Number 2
Getting lower leg ulcer evidence into primary health care nursing practice: a case study
Sue Randall, Panagiota Avramidis, Naomi James, Alanda Vincent, Rebecca Armstrong and Michelle Barakat-Johnson
Keywords Audit, community nursing, evidence-based practice, nurse-led, venous leg ulcers.
For referencing Randall S et al. Getting lower leg ulcer evidence into primary health care nursing practice: a case study. WP&R Journal 2019; 27(2):78-85.
DOI https://doi.org/10.33235/wpr.27.2.78-85
Abstract
Venous leg ulcers (VLUs) are open lesions on the lower leg caused by venous disease, which are associated with high morbidity and pose a challenge to manage effectively (Scottish Intercollegiate Guidelines Network, 2010). Gold standard treatment for VLUs is graduated compression therapy to aid venous return. This paper presents an approach to the challenging management of VLUs that is based on a problem, and subsequent local audit. We use a case study that illustrates a collaborative approach to determine gaps in evidence-based practice (EBP), and a nurse-led initiative in consultation with executive managers and doctors. In our sample, 40% of patients had not consulted a vascular specialist. They did not have a formal diagnosis of leg ulcer aetiology and therefore had not received optimum treatment. Access and cost were main factors impacting on leg ulcer care. Nurses providing evidence-based management of VLUs should ensure collaboration with key stakeholders. This assists in implementing diagnosis of ulcer aetiology for best practice measures. At this local health district, a change in policy to reflect EBP for VLU management in primary health care has been achieved.
What is already known
- Evidence-based wound practice is an approach to patient care that integrates current information from research and local data, the expertise of clinicians and patient factors.
- VLUs are a common wound in primary health care that pose significant issues for the patient, caregivers, nurses and specialists.
- Graduated compression therapy is the ‘gold standard’ treatment for VLUs.
What this manuscript contributes
- Best practice VLU care in primary health care is impeded by a number of factors, including cost, access to specialist medical consultation and primary health care resources.
- A collaborative project by primary health care wound specialist nurses, an academic and a summer scholar, with time and expertise to undertake a project to investigate and address a problem, ultimately improved the quality of patient care.
- A hand-held Doppler should be available to wound specialist nurses in primary health care to aid assessment and management of venous leg ulcers.
Introduction
Venous leg ulcers (VLUs) are defined as an open lesion between the knee and ankle joint, that remains unhealed and occurs in the presence of venous disease1,p.1. VLUs are chronic and reoccurring wounds caused by venous valve incompetence2. VLUs are the most common ulcer presentation in primary health care3.
The incidence of VLUs increases with age, between 1.5 and 3/1000 people aged 65 and below and increasing to 20/1000 people over age 853. With an ageing population, the prevalence of VLUs has the potential to be greater4-6. Such an increase presents challenges to both patients and clinicians.
Chronic wounds cause considerable financial impact on health services, with costs crudely estimated as A$2 billion in Australia7 and between £168 and 600 million in the United Kingdom8. Specifically, for chronic lower leg ulcers, estimated management costs are 6.5–7 million euros/year in Ireland alone9.
Assessment of any ulcer and accurate diagnosis of aetiology is critical to developing a management plan that achieves optimum outcomes for patients. Efforts should focus on developing strategies to identify, assess and ensure nursing practice and treatment is underpinned by evidence10 in order to provide better value care.
VLUs impact considerably on patients and cause a substantial health burden. The impact on patients include symptoms for the patient, described as ‘pain-fatigue cluster’, comprising fatigue, sleep disturbance, depression and pain in the legs; and secondly, ‘inflammation cluster’, comprising fatigue, swelling, inflammation of the legs and exudate from ulcers11. Together these symptoms cause reduced quality of life (QoL)14. Individuals experience pain12 and have restricted mobility13. They may become socially isolated, with a high incidence of anxiety and depression13,14. Personal financial costs are also described15. Recurrence of VLUs presents a significant challenge. VLU recurrence in one study in Australia involving 67 participants was 44% at 12 months with median breakdown at 27 weeks14. Recurrence from 52% to as high as 70% in international studies have been reported12,16,17.
The care of patients with VLUs presents a challenge for clinicians, creating a substantial workload for nurses that is physically demanding. For example, two nurses are often required to provide wound care: one nurse to hold the patient’s leg whilst the other nurse undertakes the dressing. Often this is because the patient’s legs are too heavy for them, or the nurses to lift, commonly due to oedema. As well as physical demands, Posnett et al.8 state that a considerable emotional burden falls on nurses, particularly when wounds such as VLUs are slow or fail to heal. Nurses who provide wound management for patients with VLUs may feel a sense of hopelessness due to slow healing, despite wound management strategies. They may also feel less optimistic and less confident in their approach to leg ulcer care18,19.
VLUs can be assessed and managed by nurses in a variety of primary health care (PHC) settings, in specialist wound, vascular or leg clinics and leg clubs (evidence-based community clinics treating patients with leg ulcers)20,21. In a recent systematic review of 17 studies, the impact of Leg Clubs on patients, despite variable study quality, noted positive outcomes on the individual’s mood, sleep and quality of life. Faster healing and less recurrence of leg ulcers were also described22.
Ankle brachial pressure index (ABPI) measurement and graduated compression therapy are two key evidence-based measures in VLU care. ABPI is a non-invasive vascular screening test that can be carried out with a hand-held Doppler to exclude peripheral arterial disease (PAD) (a vascular condition due to narrowed arteries and associated with high morbidity and mortality) by comparing systolic blood pressures in the ankle to the higher of the brachial systolic blood pressures23. The ABPI value determines the severity of PAD, which guides best assessment, and management of VLUs. For example, an ABPI of between 0.8 and 1.2 means that therapeutic graduated compression therapy of the legs is needed, whereas an ABPI of less than 0.5 indicates that graduated compression therapy should be avoided and urgent specialist review is required. For ABPI between 0.5 and 0.8 caution is required and specialist review should be recommended24. If PAD has been excluded and venous aetiology is confirmed, then graduated compression therapy is the gold standard treatment for VLUs known to improve healing rates12,25.
VLU guidelines clearly state that appropriately trained clinicians can undertake ABPI measurements and apply graduated compression therapy1,25-28. The ABPI has high sensitivity and specificity and its accuracy in establishing the diagnosis of PAD has been well supported29. However, the implementation of this as part of best practice of VLU management can be challenged by shortage of resources, both a lack of knowledge of best practice and how to identify and address a gap in practice30-32. Implementing evidence into practice has been reported to take between eight and 30 years33. This time lag can result in gaps in clinical care.
In this paper, we use a case study approach to describe a collaborative of PHC nurses specialising in wounds, an academic and a summer scholar (a pre-registration nursing student on a scholarship to gain research experience) in one Australian local health district (LHD). They combined time and expertise to undertake a project which confirmed a gap in evidence-based practice (EBP). This paper also describes the robust response to the findings by managers in the LHD.
Setting
The LHD is in a high-density, inner-city district that contains three acute public hospitals, one sub-acute public hospital, and five PHC centres, with a large, diverse population of almost 700,000 people34. The PHC nursing team, which is spread across five geographically located PHC centres, had one consultant nurse and two nurses with specific interest and expertise in wound management. In this paper, they are communally referred to as wound specialist nurses (WSNs). In February 2017, this PHC nursing team had 596 existing patients. During the study period, an additional 418 new registrations resulted in a caseload of 1014 patients. Of these, 248 existing patients had chronic leg ulceration and a further 36 new admissions with lower leg ulcers (LLU) comprising 26% of the whole PHC nursing caseload35.
Of the audited patients (n=96) seen by the LHD WSNs, 62 patients had a leg ulcer that has either been recurrent or that lasted for multiple years. Visits made to the audited cohort of patients ranged from 1 to 328 visits, with average length of visit by nurses ranging from 5 to 80 minutes. All patients in the LHD were required to have a vascular specialist doctor review to confirm diagnosis of VLU and to confirm suitability for graduated compression therapy29. The LHD policy did not include WSNs to perform an ABPI, nor initiate graduated compression therapy36. The WSNs believed this was not in line with best evidence. Before reviewing the LHD policy, the WSNs wanted evidence that included current literature and local data on management of patients with VLU.
Case study
Claudia is a 69-year-old female with bilateral chronic leg ulcers of undiagnosed aetiology (Figure 1) and unmanaged exudate. Claudia is on the pension (a regular nominal payment made by the Australian Government to people of retirement age), has no family support and had reduced mobility due to her leg ulcers, further compounded by several steps to the entrance of her house, which she was unable to navigate. She had good pedal pulses and bilateral leg oedema that was suspected to be due to venous insufficiency.
Claudia required two registered nurses for each visit to provide treatment. She had two visits per week of approximately 30 minutes per visit. These visits were over a period of eight months, with the PHC nursing team maintaining, but not actively treating her ulcers. Although venous insufficiency was the likely cause of her ulcers, she had been unable to access the vascular specialist, and the aetiology of her ulcer had not been confirmed. Hence an inability to commence graduated compression therapy under the current LHD policy. Her leg ulcers often required expensive antimicrobial dressings due to recurrent ulcer infections. Her ulcers could have healed in a shorter period of time should she have been able to have ABPI assessment and commence graduated compression therapy. In Australia, the cost of a vascular specialist appointment is A$150–300, depending on required investigations and ongoing treatment. For Claudia, this was an impossible cost being on the pension. In this LHD, there is no cost to the patient for either nursing visits or dressings.
In addition to the cost, immobility and other factors significantly impeded Claudia’s ability to attend her other appointments, such as physiotherapy and occupational therapy. Other factors included the oedema in Claudia’s legs and the exudate from her ulcers, known as “heavy legs”. The nursing team would often arrange community transport for her to attend appointments, but without reducing the exudate, Claudia could not attend any appointments. Claudia was faced with multiple barriers to best practice: immobility, the cost of vascular specialist and social isolation. Claudia’s QoL was reduced, and her ulcers remained unhealed.
Collaboration with wound specialist nurses and academics
Concern was expressed by the WSNs about Claudia's unconfirmed diagnosis and sub-optimal treatment, so the collaborative undertook a project. The aim was to establish the evidence base and “a clear picture” of the current state of VLU practice in the LHD. The stages of the project included: 1) preparing for an audit; 2) literature review of best available evidence; 3) audit data to determine the evidence–practice gap; 4) making improvements; and 5) sustaining the change.
Stage 1: Conducting a case note audit
Stage 1 consisted of an audit. The audit had received research ethics approval (AU/6/6B6C25) and was carried out in accordance with the Declaration of Helsinki requirements37. In stage 1, it was important to identify the problem. In this example, Claudia’s current challenge included multiple barriers to best practice VLU management, such as immobility, no confirmed diagnosis, her inability to attend physiotherapy and occupational therapy, and social isolation, all leading to poor QoL.
Stage 2: Literature review of best available evidence
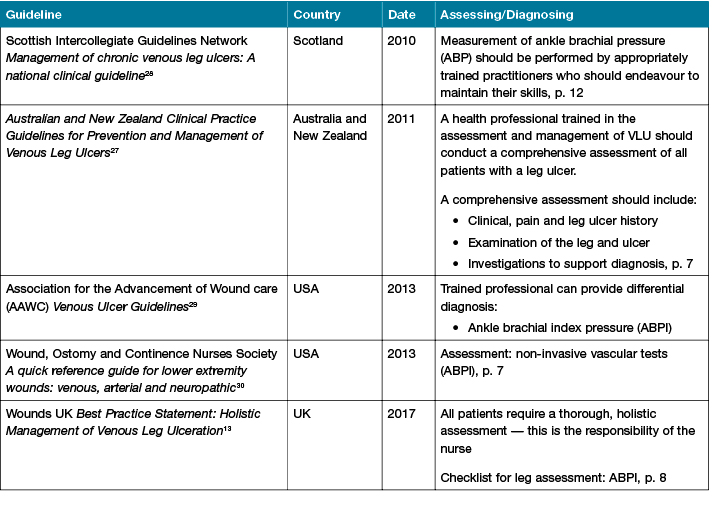
In stage 2, we determined what would be measured and what VLU “gold standards” were available to inform EBP and to add clarity and transferability. A search and review of the literature on VLU guidelines was undertaken. The databases searched were CINAHL, PubMed, Medline and Cochrane Library, and grey literature such as professional association websites. Search terms included nursing assessment, Doppler, ABPI and venous leg ulcer. This enabled the collaborative to ascertain best practice. To enable an overview of developing best practice leg ulcer care, no date limits were applied. Some VLU guidelines were found in the search; others were found through specialist nurse knowledge or through professional association websites (Table 1).
Table 1: Published guidelines for assessment and management of chronic leg ulcers (2010–2017)
Stage 3: Determining the evidence–practice gap
In order to determine the evidence–practice gap in the LHD we collected data from a simple case note audit and compared LHD performance with the VLU guidelines and best practice literature from stage 2. Data were collected from the electronic medical records (eMR). The audit tool had questions relating to demographics such as age and sex; VLU history, recurrence, and time on caseload; wound details; total nursing time in minutes; ulcer type, nicotine history, diet, history of deep vein thrombosis (as a pre-disposing factor); co-morbidities; English as first language (which has the potential to impact on understanding medical terminology); pensioner or health care card holder; whether seen by a vascular specialist; living alone or housebound; pre-disposing risk factors; and social factors. This tool was developed by the WSN and pilot-tested on the records of five patients to see if the required information could be extracted from the eMR. Information that could not be found in the eMR was removed from the tool. These variables were selected because they provided context to the clinical picture of patients with LLUs as well as direct information to help address the practice gap. The authors wanted to ensure a standardised approach to auditing to increase rigour38. Therefore, every fourth set of case notes was audited. The ‘snapshot’ audit took place in July 2017, examining patient records who were on the caseload in February 2017. Data were entered into SPSS 20 and descriptive statistical analysis was undertaken.
Findings from the audit: An audit on patients with a lower leg ulcers was undertaken. Undertaking the audit in a PHC setting offered a profile of these patients in the LHD that included prevalence. Ninety-six sets of notes were audited. This represented a quarter of eligible case notes. Of the PHC caseload in February 2017, 28% comprised patients with LLUs and in line with existing literature, the majority (86%) of those with a diagnosis had venous ulcers39.
Pre-audit, the process for diagnosis of VLU aetiology in this LHD was through a doctor, nurse practitioner (NP) or a vascular specialist. For patients living in their own homes, a vascular specialist review was conducted in private consulting rooms. The cost for this review could vary in excess of A$200 which meant that for people like Claudia, many patients were unable to pay. Like Claudia, several patients (36/96) were also housebound or had limited means of transport, making access difficult. Our LHD policy did not cover WSNs to undertake ABPI, nor initiate graduated compression therapy36.
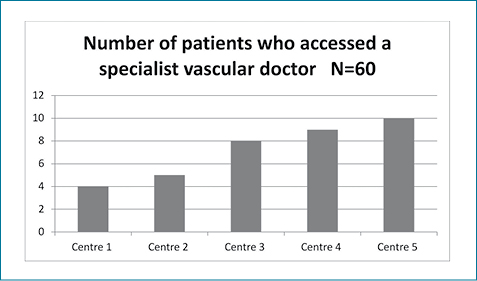
The data demonstrated a gap in evidence-based care. Of the 96 cases audited, 36 patients were new admissions so were removed from the audit, as they may not have had time to access a vascular specialist. Of the remaining, 60 patients, 40% (24/60) had not accessed a vascular specialist (Figure 2). These patients did not have a formal diagnosis of leg ulcer aetiology and hence did not receive the gold standard VLU treatment, that is, graduated compression therapy27,40. Of patients with LLUs who had not accessed a vascular specialist, 66% (40/60) were on a pension. This was statistically significant (p<0.001) and highlighted reduced equity and access. Analysing this data further, centres with patients of lower socio-economic status accessed specialist review least.
Figure 2
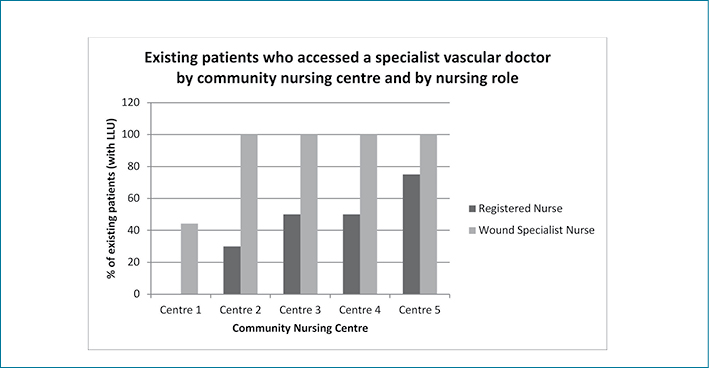
The audit highlighted further influences on care. The number of existing patients who had accessed a vascular specialist was influenced by the primary health care nurse role. Patients were more likely to have accessed a vascular specialist if they had been reviewed by a WSN rather than a registered nurse (p=0.008) (Figure 3).
Figure 3
Stage 4: Making improvements
The fourth stage of this project explored making improvements by implementing EBP. Results from the audit highlighted a gap in evidence-based care due to lack of access to vascular specialist. The findings were presented at a quality and research conference. This conference had approximately 100 nurse and executive delegates. A report of the findings35, which compared this LHD results and best practice national and international guidelines, was subsequently disseminated to the management team of PHC services. The WSNs prepared a submission to executive managers to secure funding for three Dopplers to aid assessment of housebound clients such as Claudia. For management of VLUs and improvements in service delivery, changes were made to the LHD policy on "Graduated Therapy Compression in Venous Disease", to allow WSNs to assess and authorise graduated compression therapy41.
The WSNs collaborated with the local vascular specialist doctor to discuss ways to improve the service for patients with VLUs in the community. A free LLU clinic in one PHC centre with bulk-billing services is planned. Bulk billing means that patients do not have to pay a fee for consultation as the payment is met through Medicare (publicly funded by the Australian Government).
Stage 5: Sustaining change
Stage 5 ensured the improvements we made in the LHD were going to be sustained. An annual audit will be conducted by the WSNs. A repeat audit is planned for February 2020. This audit and ongoing audits will be conducted by the collaborative to assess the impact of changes on practice and outcomes for people like Claudia who had been receiving sub-optimal treatment.
Discussion
This paper presented a staged approach to establishing best available evidence and treatment options for patients with VLUs. Findings from our approach confirm that challenges of translating best evidence into practice can be overcome by auditing, exploring current research and working in collaboration. Establishing evidence, prior to implementing strategies is key to maximising outcomes for patients. Further, our team used a collaborative approach with nurses, student nurses and academics to identify and address the evidence–practice gap.
An audit provided data, which led to greater understanding of a problem and provided opportunities to resolve a gap in practice with the potential to improve the quality of care, in part by applying the PHC principles of equity and access41-44. Results highlighted a lack of diagnosis of leg ulcer aetiology, resulting in sub-optimal treatment of patients with VLUs. Across all five centres, there was an inequity for patients who were receiving a pension, as they were less likely to have accessed a vascular specialist, due to financial constraints. This led to sub-optimal treatment when measured against national and international guidelines.
This study was presented by the WSNs to the LHD executive team, which led to discussions with management and vascular doctors about the ability of WSNs to diagnose ulcer aetiology. In line with the VLU guidelines1,25-28, WSNs have the skills and knowledge to assess and manage VLUs. This would potentially improve the standard of care for patients with VLUs in the PHC and bring the issues of both equity and access in line with the World Health Organization principles of PHC42-44.
PHC focuses on integrated care that is accessible to all patients, is socially acceptable, evidence-based, and provided by a suitably qualified workforce45. PHC promotes independence at a personal and community level, striving to address and minimise issues regarding inequality while supporting those with the greatest need. This is achieved through collaboration across health sectors45. Undertaking this study has facilitated a greater collaboration between services, underpinned by guiding principles of equity, access, empowerment, self-determinism and inter-sectoral collaboration, improving outcomes for patients with VLUs. Collaboration between hospital, PHC and the university is seen as improving both patient experience and treatment for VLUs46.
Furthermore, in this study we found that patients were much more likely to have consulted a vascular specialist if they had been seen by a WSN. In this LHD, there is currently no direct referral process for a patient in primary health care to see a vascular specialist. The positive impact on patient outcomes from the combination of expertise of a vascular specialist and advanced nurse, such as the WSN involvement is safe, acceptable, cost-neutral and contributes to improving the patient and family experience47. Tsiachristas et al.48 report that advanced NP roles such as WSNs improve access to care, provide patient information, increase satisfaction of patients and relatives, all leading to positive clinical outcomes, improved quality of care and health care utilisation. However, advanced nursing roles, such as WSNs may be impeded by a lack of clarity in boundaries and levels of practice which are, at times, individually and contextually constructed49, and as such, are an untapped health care resource50. Under-diagnosis, as noted in this audit, could be rectified by a protocol based on national and international guidelines. EBP results in both a reduction in health care costs and better patient outcomes51.
Staff engagement and organisational factors such as budget and stakeholder buy-in, could impact on implementation and should be addressed to recommend a strategy to overcome such factors. Undertaking an audit provided clear and concise local data52. Clinician-led improvement projects are associated with stronger efficacy and larger effect sizes than those that are manager-driven53. This highlights the importance of nurses and other health care professionals initiating and being involved in projects similar to this.
This audit was initiated following nurses’ identification of a problem with Claudia to improve care provided to patients like Claudia. The findings from this audit provided data which confirmed evidence that there were substantial issues with equity and access for patients living in this LHD with LLUs. This impacted on VLU outcomes such as the case demonstrated by Claudia. Response from the district has been the supply of portable Doppler for WSNs to perform ABPI and to identify aetiology and commence graduated compression therapy. For Claudia this meant she was able to have a formal assessment of her legs undertaken by the WSNs. She commenced on graduated compression therapy and, as a result, her VLU healed within five months.
Limitations
The audit examined a small number of patients with an LLU. The small sample sizes meant reduced power and effectiveness of statistical tests.
Conclusion
This paper describes a case study, which led to a collaborative of WSNs, an academic and a summer scholar to undertake a study comprising five stages which addressed an identified problem with VLU care in PHC. The findings from this study highlighted gaps in EBP that affected quality care. This was addressed by implementing VLU best practice evidence into PHC in one LHD. The audit offered an opportunity to address practice gaps and allow the LHD to re-align itself with EBP. This process has changed policy to ensure patients living with VLUs have access to appropriate diagnostic services and the best available treatment.
Implications
It is a timely reminder that, despite the availability of clinical guidelines, EBP may not be followed. An audit provided evidence of which elements of care are effective and where there are gaps in practice, identifying where quality improvements can be made. Our study confirmed that an audit provided data and, combined with current EBP, literature can empower clinicians to seek and sustain change.
Acknowledgement
We wish to thank Judith Fethney, statistician at the University of Sydney Susan Wakil School of Nursing and Midwifery for her guidance in the statistical analyses.
Funding
Alanda Vincent received a stipend of A$2000 from The University of Sydney Susan Wakil School of Nursing and Midwifery as part of the Summer Scholar Program to develop research skills. No other authors received funding for this study. As a result of the project, Panagiota Avramidis, Naomi James and Rebecca Armstrong were awarded A$10,000 by Sydney Local Health District to purchase equipment. There was no involvement in project execution by either funding source.
Conflict of Interest
There are no conflicts of interest for any of the authors.
Author(s)
Sue Randall*
RGN, PhD.
Senior Lecturer in Primary Health Care Nursing University of Sydney Susan Wakil School of Nursing and Midwifery
Camperdown, NSW, Australia
Email sue.randall@sydney.edu.au
Panagiota Avramidis
RN, PGCE
Wound Clinical Nurse Specialist 2, Sydney District Nursing, Sydney Local Health District
NSW, Australia
Naomi James
RN, PGCE
Wound Clinical Nurse Specialist 2, Sydney District Nursing, Sydney Local Health District
NSW, Australia
Alanda Vincent
RN
Glebe Family Medical Practice, Glebe, NSW, Australia
Rebecca Armstrong
RN
former Wound Consultant Nurse, Sydney District Nursing, Sydney Local Health District
NSW, Australia
Michelle Barakat-Johnson
RN, PhD
District Lead Nurse Consultant, Pressure Injury Prevention and Management, Sydney Local Health District; Lecturer, Faculty of Medicine and Health University of Sydney, NSW, Australia
* Corresponding author
References
- Scottish Intercollegiate Guidelines Network (SIGN). Management of chronic venous leg ulcers: A national clinical guideline. Scotland, Edinburgh: Health Improvement; 2010. Retrieved from http://www.sign.ac.uk/assets/sign120.pdf
- Chamanga E. Community nurses’ experiences of treating patients with leg ulcers. J Community Nurs 2014;28(6):27–34.
- Nelson E, Addeley U. Venous leg ulcers. Am Fam Physician 2017;95(10):662–663.
- Yarwood-Ross L, Haigh C. Managing a venous leg ulcer in the 21st century: improving self-care. Br J Community Nurs 2015;17(10):460–465.
- Martin F, Duffy A. Assessing and managing venous leg ulcers in the community: a review. Wound Care 2011;S6–S14.
- Todd M. Venous leg ulcers and the impact of graduated compression therapy. Br J Nurs 2011;20(21):1360–1364.
- Graves N, Zheng H. Modelling the direct health care costs of chronic wounds in Australia. Wound Practice & Research 2014;22(1):20–33.
- Posnett J, Gottrup F, Lundgren, H, Saal G. The resource impact of wounds on health-care providers in Europe. J Wound Care 2009;18(4):154–161.
- Barrett S, Cassidy I, Graham M. National survey of Irish community nurses’ leg ulcer management practices and knowledge. J Wound Care 2009;18(5):181–190.
- Gray T, Rhodes S, Atkinson R, Rothwell K, Wilson, Dumville J, Cullum N. Opportunities for better value wound care: a multiservice, cross-sectional survey of complex wounds and their care in a UK community population. BMJ Open 2018;8:e019440. Doi:10.1136/bmjopen-2017-019440
- Edwards H, Finlayson K, Skerman H, Alexander K, Miaskowski C, Aouizerat B et al. Identification of symptom clusters in patients with chronic venous leg ulcers. J Pain Symptom 2014;47:867–875.
- Edwards H, Courtney M, Finlayson K, Shuter P, Lindsay E. A randomised controlled trial of a community nursing intervention: improved quality of life and healing for clients with chronic leg ulcers. J Clin Nurs 2009;18:1541–1549.
- Jones J, Barr W, Robinson J, Carlisle C. Depression in patients with chronic venous ulceration. Br J Nurs 2006;15(11):S17–S23.
- Persoon A, Heinen M, van der Vleuten C. Leg ulcers: A review of their impact on daily life. J Clin Nurs 2004;13(3):341–354.
- Smith E, McGuiness W. Managing venous leg ulcers in the community: personal financial cost to sufferers. Wound Practice & Research 2010;18(3):134–139.
- Finlayson K, Wu M-L, Edwards H. Identifying risk factors and protective factors for venous leg ulcer recurrence using a theoretical approach: a longitudinal study. Int J Nurs Stud 2015; 52(6):1042–1051.
- Guest M, Smith J, Sira M, Madden P, Greenhalgh R, Davies A. Venous ulcer healing by four-layer graduated compression therapy is not influenced by the pattern of venous incompetence. Br J Surg 1999;86(11):1437–1440.
- Van Hecke A, Grypdonck M, Beele H, De Bacquer D, Defloor T. How evidence-based is venous leg ulcer care? A survey in community settings. J Adv Nurs 2008;65(2):337–347.
- Lagerin A, Hylander I, Törnkvist L. District nurses’ experiences of caring for leg ulcers in accordance with clinical guidelines: a grounded theory study. Int J Qual Stud Health Well-being. 2017;12(1):1355213. doi:10.1080/17482631.2017.1355213
- Day J. Diagnosing and managing venous leg ulcers in the community. Community Wound Care 2015;December:S22–S30.
- Weller C, Wells S. Venous leg ulcer management in general practice. Aust Fam Physician 2012;41(5):331–337.
- Ghazelah H, Arton M, Sturt J. A systematic review of community leg clubs for patients with chronic leg ulcers Prim Health Care Res Dev 2018; Doi.org/10.1017/S1463423618000610
- Rumwell, C & McPharlin, M. Vascular Technology: An Illustrated review. 4th edn. Pasadena, CA: Davies Publishing, Inc.; 2009.
- Weller D, Team V, Ivory J, Crawford K, Gethin G. ABPI reporting and compression recommendations in global clinical practice guidelines on venous leg ulcers: a scoping review. Int Wound J 2018; doi:10.1111/iwj.13048.
- Australian Wound Management Association [AWMA] & New Zealand Wound Care Society. Australian and New Zealand Clinical Practice Guidelines for Prevention and Management of Venous Leg Ulcers. Cambridge Publishing; 2011. Retrieved from http.//www.awma.com.au/publications/publications.php; 2011.
- Association for the Advancement of Wound Care [AAWC]. Venous Ulcer Guidelines. Retrieved from https://aawconline.memberclicks.net/resources; 2013
- Wound, Ostomy and Continence Nurses Society. A quick reference guide for lower extremity wounds: venous, arterial and neuropathic. Retrieved from http://c.ymcdn.com/sites/www.wocn.org/resource/resmgr/publications/Venous_Arterial__Neuropathic.pdf; 2013.
- Wounds UK. Best Practice Statement: Holistic Management of Venous Leg Ulceration. Retrieved from http://www.wounds-uk.com/pdf/content_12022.pdf; 2017.
- Haesler, E. Venous leg ulcers: Diagnostic tools for venous disease. Wound Practice & Research 2018;926(4):212–214.
- Sandstrom B, Borglin G, Nilsson R, Willman A. Promoting the implementation of evidence-based practice: A literature review focussing on the role of nurse leadership Worldviews Evid Based Nurs 2011;(8)4:212–223. doi: 10.1111/j.1741-6787.2011.00216.x.
- Leach M, Tucker B. Current understandings of the research-practice gap in nursing: a mixed methods study. Collegian 2018; 25(2):171–179.
- Edwards H, Finlayson K, Courtney M, Graves N, Gibb M, Parker C. Health service pathways for patients with chronic leg ulcers: identifying effective pathways for facilitation of evidence based wound care. BMC Health Serv Res 2013;13:86. https://doi.org/10.1186/1472-6963-13-86
- Hutchinson A, Johnston L. Beyond the BARRIERS scale: Commonly reported barriers to research use. JONA 2006;(36)4:189–199.
- Public Health Observatory. A demographic and social profile of Local Health District https://www.slhd.nsw.gov.au/PopulationHealth/pdf/slhd_demography_2016.pdf
- Randall S, Vincent A, Avramidis P, James N Executive summary and report on the profile of lower leg ulcers in Sydney Local Health District. 2018. (Available from corresponding author)
- Sydney Local Health District (SLHD). Graduated Compression Nursing Procedural Guideline. SLHD; 2015.
- World Medical Association (WMA). WMA declaration of Helsinki: Ethical principles for medical research involving human subjects. WMA; 2013 Available at: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/ Accessed 28 September 2018.
- Stephenson M, McArthur A, Giles K, Lockwood K, Aromataris E, Pearson A. Prevention of falls in acute hospital settings: A multi-site audit and best practice implementation project. Int J Qual Health Care 2016;28(1):92–98. doi:10.1093/intqhc/mzv113
- Kelechi T, Johnson J, Yates J. Chronic venous disease and venous leg ulcers: an evidence-based update. J Vasc Nurs 2015;33(2):36–46.
- Franks P, Barker J, Collier M et al. Management of patients with venous leg ulcers: challenges and current best practice. J Wound Care 2016;25(Supp6):S1–S67. doi: 10.12968/jowc.2016.25.Supp6.S1.
- Sydney Local Health District (SLHD). Graduated Therapy Compression in Venous Disease. Policy. SLHD; 2018.
- World Health Organization (WHO). Declaration of International Conference on Primary Health Care, Alma-Ata, USSR, 6–12 September 1978. Geneva. Retrieved from http://www.who.int/publications/almaata_declaration_en.pdf; 1978.
- World Health Organization. The World Health Report: The core principles of primary health care. Retrieved from http://www.who.int/whr/2003/chapter7/en/index1.html; 2003.
- World Health Organization. The world health report. Retrieved from: http://www.who.int/whr/2008/overview/en/;2008.
- Oliver-Baxter J, Lunnay B, MacIntyre E. Primary health care matters: Fact sheet; 2014. Available at: http://www.phcris.org.au/phplib/filedownload.php?file=/elib/lib/downloaded_files/publications/pdfs/phcris_pub_8371.pdf
- Jepson T, O’Hara T, Monaro S. Case study: collaboration across the care continuum to improve the patient experience. Wound Practice & Research 2018;26(4)Dec.
- Moore J, McQuestion M. The clinical nurse specialist in chronic diseases. J Adv Nurs Prac 2012;26(3):149–163.
- Tsiachristas A, Wallenburg I, Bond C. Costs and effects of new professional roles: Evidence from a literature review. Health Policy 2015;119(9):1176–87.
- Wilkes L, Luck L, O’Baugh J. The role of a clinical nurse consultant in an Australian Health District: a quantitative survey. BMC Nurs 2015;(1):25.
- Gosby H & Australian College of Nurse Practitioners (ACNP). Transforming Health Care [Press release]. Retrieved from Proceedings of the ACNP National Conference, Hobart, Australia; 2013.
- Melnyk B, Gallagher-Ford L, Long L, Fineout-Overholt E. The establishment of evidence-based practice competencies for practicing registered nurses and advanced practice nurse in real world clinical settings: Proficiencies to improve healthcare quality, reliability, patient’s outcomes and cost. Worldviews Evid Based Nurs 2014;11(1):5–15.
- Bradshaw W. Importance of nursing leadership in advancing evidence-based nursing practice. Neonatal Network 2010; (29)2:doi:10.1891/0730-0832.29.2.117.
- Scott I. What are the most effective strategies for improving quality and safety of healthcare? Intern Med J 2009;39:389–400.



