Volume 28 Number 2
Implementing the 2019 International Guideline: consultation on barriers, facilitators, challenges and resource needs
Emily Haesler and Keryln Carville
Keywords pressure injury, consultation, translation to practice
For referencing Haesler E & Carville K. Implementing the 2019 International Guideline: consultation on barriers, facilitators, challenges and resource needs. Wound Practice and Research 2020; 28(2):90-96.
DOI https://doi.org/10.33235/wpr.28.2.90-96
Abstract
In November 2019, the third edition of the International guideline was published. Dissemination of clinical guidelines and translation into practice is shown to be facilitated by resources to support the guideline and address of barriers to implementation. To identify the barriers, facilitators and challenges that influence translation of the recommendations in the International guideline into practice, and resources that might be useful to health professionals, two consultation forums were undertaken. This paper outlines the outcomes from these consultation forums and identifies resources that are considered important for translating recommendation into practice.
Background
In November 2019 the European Pressure Ulcer Advisory Panel (EPUAP), National Pressure Injury Advisory Panel (NPIAP) and Pan Pacific Pressure Injury Alliance (PPPIA) released the third edition of the Prevention and treatment of pressure ulcers/injuries: clinical practice guideline, referred to as the International guideline1. The International guideline includes 115 evidence-based recommendations and 61 best practice statements to guide clinicians, educators, researchers, policy makers, formal and informal caregivers and industry in addressing pressure injury prevention and treatment. These statements are designed to guide practice and are presented with overviews of the supporting evidence, alongside practical implementation considerations to assist clinical translation of the recommendations.
It is well recognised that regardless of the strength of the methodology, content and presentation, clinical practice guidelines are often under-utilised in the delivery of patient care2. A range of barriers to translation of guidelines into clinical practice have been highlighted previously. These barriers include – clinician-related factors such as lack of awareness or motivation; factors related to the guideline itself (for example limited evidence, availability of support resources, feasibility of recommendations or access to the guideline); and external factors (for example, lack of resources and time, or organisational constraints)2,3.
Raising awareness about guidelines is the first step in embedding the best practice outlined within into clinical practice. The EPUAP, NPIAP and PPPIA use a range of dissemination strategies to engage clinicians in the International guideline, including participation in the development and review of the guideline by a very large global team of clinicians from over 30 countries, production of a free Quick reference guideline which succinctly presents the recommendations, registration of the guideline with national guideline trusts, as well as promotion via social media alerts and conference presentations. These strategies effectively disseminated the 2014 edition of the guideline, as evidenced by over 250,000 downloads of the free Quick reference guideline and approximately 750 citations indexed in Web of Science4. The 2019 edition of the International guideline aims to present the evidence for pressure injury prevention and management in a manner that is clinically relevant and facilitates guideline implementation.
Consultation forums
Two consultation forums were hosted to explore the practical challenges experienced by health professionals when implementing the International guideline recommendations for pressure injury prevention and treatment, and to identify national and local strategies that could facilitate translation of evidence.
An open forum was conducted as a panel discussion with live audience polling at the Wounds Australia ACT Conference in Canberra in November 2019. The discussion was open to all conference delegates who attended the open panel discussion session. Following this open forum, a second consultation forum was conducted with an invited team of pressure injury experts. The expert forum was conducted as a meeting which preceded a Smith+Nephew Pressure Injury Seminar which was held in Sydney in February 2020. Participation was limited to the 19 invited experts, and participants included board representatives from Wounds Australia and the New Zealand Wound Care Society.
Both forums followed the same format. Questions were posed and responses were collected using text messages to the polling platform that had been programmed to receive one response only from each mobile phone number. All responses were anonymous, and participation was voluntary. Demographics on the participants’ practice settings and roles were collected using a multiple choice format. Next, open-ended questions were posed to which one-word responses were required. The results were presented to the participants using a dynamic live polling format which was displayed on the presentation screen. At both forums, the floor was opened to discussion after each posed question.
Respondent demographics
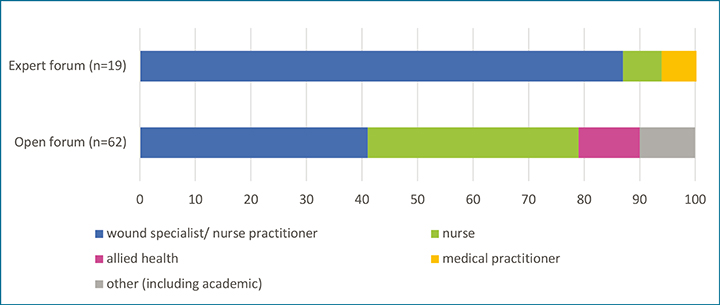
Figures 1 and 2 provide an overview of the practice settings and roles identified by respondents. Amongst the Wounds Australia ACT conference participants, 65 conference attendees who responded to the work place and role question were as follows: 40% worked in acute care, 23% in community care, 20% indicated other settings (including education and academia), 11% worked in aged care and 6% had roles in rehabilitation. Amongst participants in the expert forum, 33% had roles primarily in education and academia, 27% were from community settings and 20% each worked in aged and acute care. At the open forum, 41% of participants identified their main role to be wound specialist/clinical nurse specialist/nurse practitioner, that is, experts in wound care. There were 38% of respondents who identified themselves as other nurses, 11% as allied health professionals, 5% as non-clinical staff and 5% responded as having other roles such as industry. In contrast, 87% of respondents at the expert forum were wound specialists/clinical nurse specialist/nurse practitioners, with 7% representation from other nurses and 7% had medical practitioner backgrounds.
Figure 1. Respondents’ primary practice setting
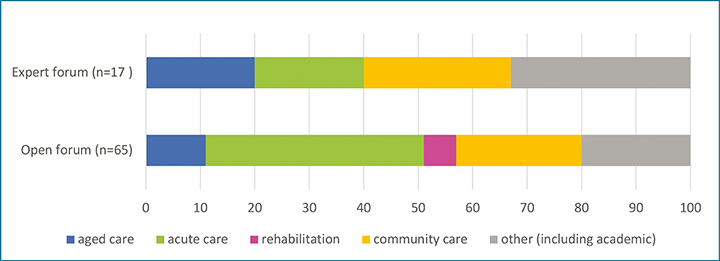
Figure 2. Respondents’ primary clinical background
Barriers and facilitators
Figure 3 shows the Wordcloud results for the single-word responses related to the biggest barriers participants experience when implementing the recommendations in the International guideline. The size of each word in the Wordcloud increases with the increased number of respondents, reflecting the popularity of the response. At both forums, ‘time’ constraint was noted to be one of the most common barriers. Culture, change, behaviours and attitudes were also common barriers identified by participants in the larger open forum. In the smaller expert forum, a lack of control, priorities, people and resources were perceived to be barriers.
Figure 3. Barriers to implementing the International guideline recommendations
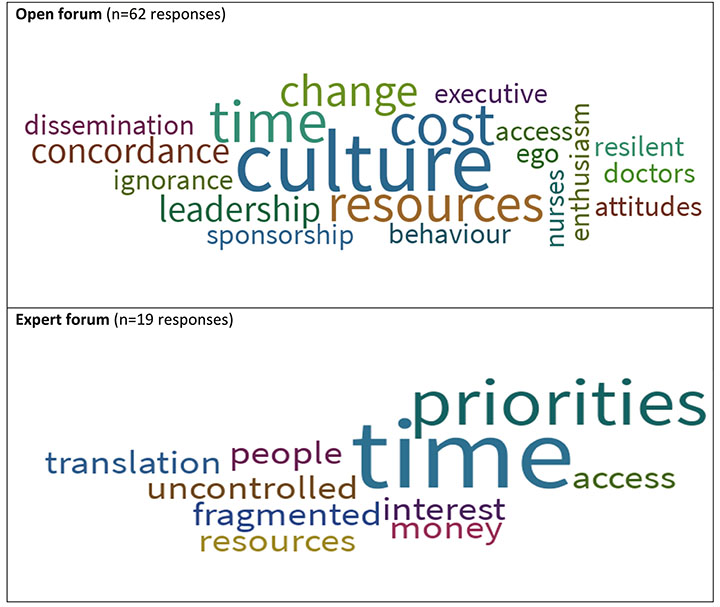
Figure 4 shows the Wordcloud for single-word responses related to identified facilitators when implementing the guideline recommendations. Both groups identified collaboration/teamwork as the biggest facilitator. Other responses included positive attitudes such as enthusiasm, passion, excitement and commitment. Themes also emerged from both forums for education, knowledge, understanding and translation, with varying degrees of popularity.
Figure 4. Facilitators to implementing the International guideline recommendations
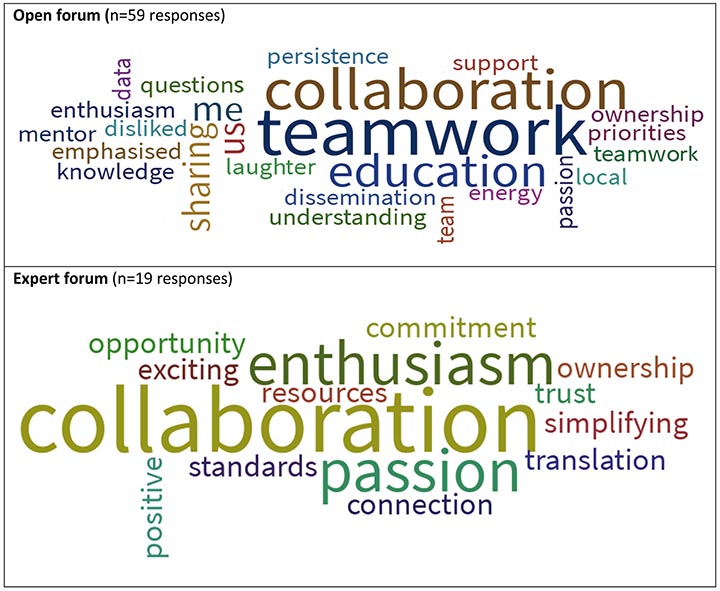
The Wordcloud results and discussion that arose from the floor at both forums highlighted a range of facilitators and barriers for guideline translation. Enthusiastic discussion amongst participants related to the care team culture and the level of engagement indicated the importance of collaboration, leadership and change planning as effective facilitators. Barriers to guideline implementation were proposed to be organisational time and budget constraints, inadequate staffing, and lack of knowledge or access to the guideline and the equipment required to provide care recommendations. Interestingly, these barriers are frequently identified in the implementation science literature as being significant to successful translation of guideline recommendations1–3,5.
Table 1. International guideline recommendations for facilitating guideline implementation1
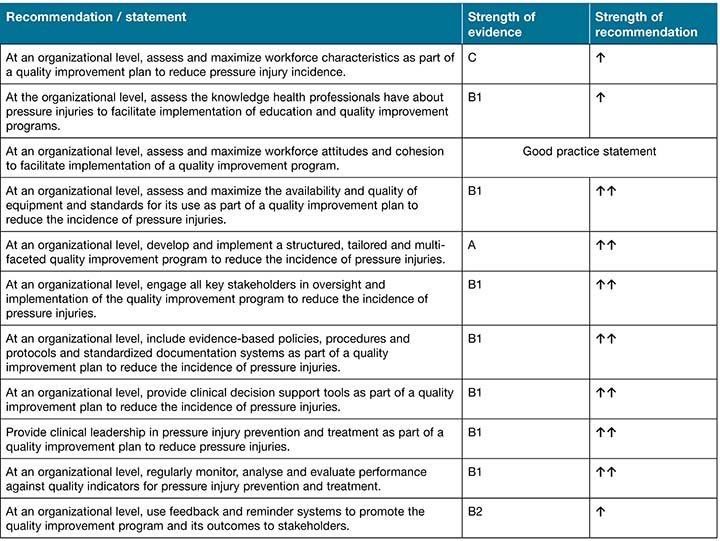
Table 2. Strength of evidence ranking1. (Reprinted with permission from EPUAP/NPIAP/PPPIA).
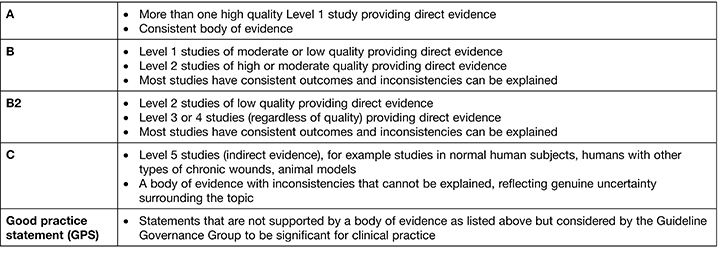
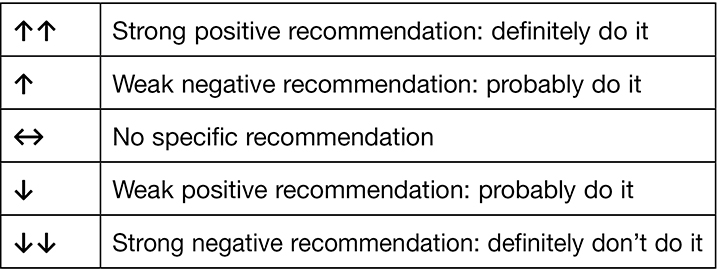
Table 3. Strength of recommendation ranking1. (Reprinted with permission from EPUAP/NPIAP/PPPIA).
Importantly, the International guideline1 outlines strategies for overcoming barriers, including 11 evidence-based recommendations and one good practice statement (Table 1, grading explanation in Tables 2 and 3). These recommendations are based on a large body of evidence (over 70 studies) that provided direct evidence for the recommended practice and were associated with a sustained (over more than 12 months) reduction in pressure injury prevalence and/or incidence. Included in the new International guideline are implementation considerations that provide additional information on how recommendations could be introduced, and outcomes evaluated. For example, the International guideline details resources that have been successfully used in the reported research to achieve this goal, including benchmarking tools5,6, electronic tracking systems7–9, computerised care planning10, and regular surveillance7,11–16.
Highlighted throughout the International guideline’s chapter on implementation is the importance of using a multi-faceted approach for introducing practice change1. Most of the studies reporting implementation of best practice in prevention of pressure injuries used bundles that incorporated a range of strategies. Establishing the best strategies to use, however, requires knowledge, leadership and a strategic approach. It is important to note that different guideline-associated resources can assist different health administrators, educators, health professionals and formal and informal caregivers in meeting best practice goals3.
Resource needs
Because the participants at the open forum identified a lack of resources as a major barrier to implementing the International guideline, one of the goals at the expert forum was to ascertain what resources/tools guideline users would consider useful – these are described in Figure 5.
Figure 5. Tools identified as facilitating International guideline implementation in the Pan Pacific region
|
In discussing tools that might be developed to facilitate implementation of best practice, the expert forum participants determined that resources were required for all health agencies and practitioners – government, academia, administration, health professionals, formal and informal caregivers and patients. Participants established that key stakeholders have different scopes of practice and levels of engagement and therefore require targeted tools that are appropriate to their knowledge level, discipline and health delivery activities. The need for tools to be locally relevant and culturally sensitive was also highlighted, with the expert forum participants in agreeance that international, national and regional tools may require adaptation across these sectors.
Moreover, participants at both the open and expert forums unanimously agreed that a national level of engagement was required to advance guideline accessibility and implementation. All participants considered that the active engagement of peak body organisations such as Wounds Australia and the New Zealand Wound Care Society was paramount for raising awareness and national dissemination and implementation of the guideline. Underpinning this strategy is the need for government-funded guideline access across all health settings. Participants also identified that national benchmarking of pressure injury prevalence, incidence and translation of evidence outcomes was key for attaining and sustaining consistent best practice.
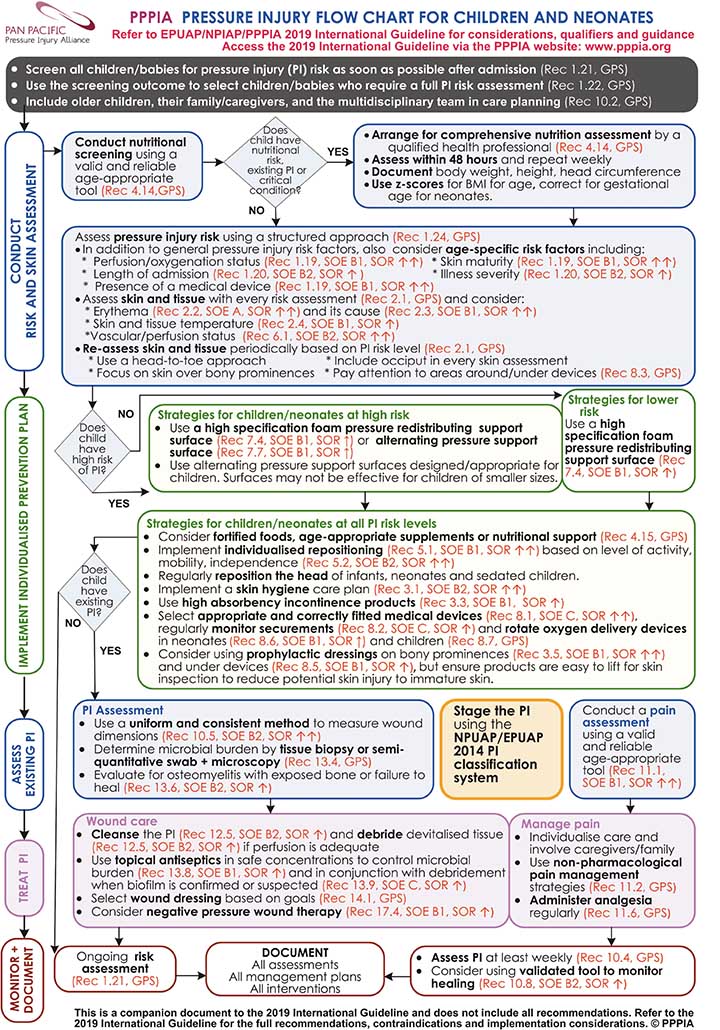
To this end, the PPPIA team have commenced development of tools to assist with the implementation of the guideline in Australia, New Zealand, Singapore and Hong Kong. The first suite of tools is care flow charts for guiding implementation of recommendations for the prevention and treatment of pressure injuries. Appendix 1 to this article shows the Pressure injury flow chart for children and neonates, which brings together recommendations for the care of this special population. Other care flow charts for adults, those in the critical care setting, and individuals with medical devices will be available from the PPPIA website (www.pppia.org) in mid to late June 2020. Additionally, the PPPIA team has developed several pressure injury classification tools for a range of different populations that are soon to be released. These resources will be available for free downloads for health professionals in the Pan Pacific region; these are intended as companion tools to the International guideline and are not intended for use in isolation.
Acknowledgements
The following people and organisations are sincerely acknowledged for their contribution to the consultation process:
- Wounds Australia ACT Committee who organised the forum at the Canberra conference.
- Nina Fan, Ruth Timmins and Cassandra Cerecedo (Smith+Nephew) for organising the expert forum held in Sydney.
- New Zealand Wound Care Society.
Forum participants in Canberra and Sydney who gave generously of their time, experience and expertise:
- Emily Haesler who prepared the live poll format for both forums.
- Keryln Carville, Emily Haesler, Pam Mitchell, Tracy Nowicki and Judith Barker who facilitated the consultation forum in Canberra.
- Keryln Carville and Emily Haesler who facilitated the expert forum in Sydney.
- Barbara Delmore and Jill Cox from NPIAP who provided the framework for this Pan Pacific region consultation process.
Conflict of interest
The authors declare no conflicts of interest.
Funding
The authors received no funding for this study.
Appendix 1. PPPIA Pressure injury flow chart for children and neonates. (Reproduced with permission from PPPIA).
Author(s)
Emily Haesler*
PhD, PGradDipAdvNurs (Gerontics), BN
Adjunct Associate Professor, Western Australia Centre for Evidence Informed Healthcare Practice, Wound Healing and Management Unit, Curtin University WA
Honorary Senior Lecturer, The Australian National University, ANU Medical School, ACT
Honorary Associate, Australian Centre for Evidence Based Aged Care, School of Nursing and Midwifery La Trobe University, Bundoora, VIC
Email Emily.Haesler@anu.edu.au
Keryln Carville
RN, PhD
School of Nursing, Midwifery and Paramedicine, Curtin University, WA
Australia Silver Chain Group, WA
* Corresponding author
References
- European Pressure Ulcer Advisory Panel (EPUAP), National Pressure Injury Advisory Panel (NPIAP), Pan Pacific Pressure Injury Alliance (PPPIA). Prevention and treatment of pressure ulcers/injuries: clinical practice guidelines. The international guideline. 3rd ed. Emily Haesler, editor. EPUAP, NPIAP, PPPIA; 2019.
- Field M, Lohr K, editors. Implementing guidelines: conditions and strategies. In: Guidelines for clinical practice: from development to use. Institute of Medicine, National Academy Press: Washington, DC; 1992.
- Fischer F, Lange K, Greiner W, Kraemer A. Barriers and strategies in guideline implementation: a scoping review. Healthcare 2016;4(3):36.
- Kottner J, Haesler E. The dissemination of the Prevention and treatment of pressure ulcers clinical practice guideline 2014 in the academic literature. Wound Rep Regen 2020. doi:10.1111/wrr.12823.
- Baier R, Butterfield K, Patry G, Harris Y, Gravenstein S. Identifying star performers: the relationship between ambitious targets and nursing home quality improvement. J Am Geriatric Soc 2009;57(8):1498–1503.
- Baier RR, Butterfield K, Harris Y, Gravenstein S. Aiming for star performance: the relationship between setting targets and improved nursing home quality of care. J Am Med Director Assoc 2008;9(8):594–598.
- Beeckman D, Clays E, Van Hecke A, Vanderwee K, Schoonhoven L, Verhaeghe S. A multi-faceted tailored strategy to implement an electronic clinical decision support system for pressure ulcer prevention in nursing homes: a two-armed randomized controlled trial. Int J Nurs Stud 2013;50(4):475–486.
- Mallah Z, Nassar N, Kurdahi Badr L. The effectiveness of a pressure ulcer intervention program on the prevalence of hospital acquired pressure ulcers: controlled before and after study. Applied Nursing Research : ANR, 26 Jul 2014, 28(2):106-113.
- Sebastian-Viana T, Losa-Iglesias M, Gonzalez-Ruiz JM, Lema-Lorenzo I, Nunez-Crespo FJ, Salvadores Fuentes P, team A. Reduction in the incidence of pressure ulcers upon implementation of a reminder system for health-care providers. App Nurs Res 2016;29:107–12.
- Thomas ME. The providers’ coordination of care: a model for collaboration across the continuum of care. Prof Case Manage 2008;13(4):220–227.
- Antonio T, Conrad K. Clinical and economic improvements in pressure injury care at Ballarat Health Services. Wound Pract Res 2013;21(1):4–10.
- Baldelli P, Paciella M. Creation and implementation of a pressure ulcer prevention bundle improves patient outcomes. Am J Med Qual 2008;23(2):136–142.
- Sving E, Högman M, Mamhidir AG, Gunningberg L. Getting evidence-based pressure ulcer prevention into practice: a multi-faceted unit-tailored intervention in a hospital setting. Int Wound J 2016 Oct;13(5):645-54.
- Smith SK, Ashby SE, Thomas L, Williams F. Evaluation of a multifactorial approach to reduce the prevalence of pressure injuries in regional Australian acute inpatient care settings. Int Wound J 2017;07:07.
- Bales I, Duvendack T. Reaching for the moon: achieving zero pressure ulcer prevalence, an update. J Wound Care 2011;20(8):374–377.
- Bales I, Padwojski A. Reaching for the moon: achieving zero pressure ulcer prevalence. J Wound Care 2009;18(4):137–144.



