Volume 29 Number 2
Reducing the incidence and severity of pressure injuries in a high level care residential aged facility: a quality improvement project
Allyson Waird, Susan Monaro
Keywords pressure injury, residential aged care, skin integrity
For referencing Waird A and Monaro S. Reducing the incidence and severity of pressure injuries in a high level care residential aged facility: a quality improvement project. Wound Practice and Research 2021; 29(2):77-85.
DOI https://doi.org/10.33235/wpr.29.2.77-85
Abstract
Aims Reduce pressure injuries (PIs) in residents of a high level care facility by increasing staff knowledge and skills through clinical support and a skin integrity education package.
Method This project was a quality improvement (QI) activity and data were de-identified and reported in aggregate. Pre- and post-implementation data included staff knowledge testing and PI prevalence and severity.
Results Pre-implementation data indicated that staff knowledge was very limited, skin inspections and PI risk assessment were not performed, and use of pressure redistribution devices was low, with point prevalence at 64% of mainly severe PIs. Despite ongoing external clinical and project support, compliance with project elements was deficient. Post-implementation knowledge change was unable to be measured, but skin inspections improved. PI point prevalence reduced to 33% and suspected deep tissue injuries (SDTI) were eliminated.
Conclusion Change in knowledge could not be measured as staff did not complete post-implementation tests. Although documentation of daily skin inspections were inconsistent, awareness of this requirement may be linked to the significant reduction in the prevalence and severity of PIs. There is an urgent need to engage residential care staff in risk assessment and the implementation of strategies to reduce skin injuries.
What is already known
- PIs are common in residential aged care facilities.
- There is a lack of skin integrity knowledge in residential aged care staff and education is often inadequate.
- Appropriate use of pressure redistribution equipment reduces the risk of PIs.
What this manuscript contributes
- Use of appropriate pressure redistribution equipment alone may not reduce the risk of PIs.
- Pressure redistribution equipment may be under-utilised in residential aged care facilities.
- Even when provided with support and education, other barriers prevent residential aged care staff from implementing PI prevention strategies.
- Regular skin inspection may have a positive impact on the incidence and severity of PIs.
Introduction
The world’s population is ageing, and there is an increasing trend in western countries for older, frail people to transition to residential aged care facilities. In Australia, almost 60,800 people entered permanent residential aged care for the first time in 2018–19, with more than half aged over 85 years. Complex needs of residents require safe nursing care to be provided by appropriately qualified and experienced nurses1. The recent Royal Commission into Aged Care has confirmed issues arising from poor skill mix need to be addressed2. The older person’s complex healthcare needs have increased steadily3 and contribute to frailty4. Geriatric syndromes and their link to frailty were first described by Tinetti et al. in 19955. Skin integrity is an element of frailty, and there is a risk of multiple types of skin injuries in the older person6.
Pressure injury (PI) is now the preferred term for skin and underlying tissue damage arising from ongoing and unrelieved pressure which may be associated with contributing factors such as moisture, shear, immobility, and/or fragile tissue7,8. Whilst PIs are found throughout healthcare facilities and the community, across ages and varied illnesses, their prevalence is highest in the aged population, especially in the very ill and frail7. Up to 70% of residents in high level care facilities (HLCFs), who are identified as high risk, develop a PI9. There is a significant cost associated with the treatment of PIs, especially when they are severe10. Appropriate knowledge and implementations can prevent PIs11. This paper will describe a quality improvement (QI) project conducted in a residential aged care setting to address gaps in PI prevention.
Background
PIs have been recognised for centuries, dating back to the time of Egyptian mummies7. They are regarded as indicators of the quality of nursing care12,13. Despite this, evidence indicates that nurses’ awareness of prevention and management may be sub-optimal14. PIs have significant adverse effects on the person, including pain, discomfort, poor sleep, and reduced quality of life15, thus increasing the complexity of care and substantially increasing costs16. With the ageing process, there are multiple declining physical functions, with the skin being one of the more observable features. Skin loses elasticity and strength, becomes fragile, and is therefore more prone to damage9. Campbell, Coyer and Osborne6 have discussed the phenomenon of ‘skin vulnerability’ and provide a conceptual model for addressing the multiple interrelated factors which contribute to skin injury. The scope of skin injury includes PIs, skin tears, moisture-associated skin damage (MASD) including incontinence-associated dermatitis (IAD), intertriginous dermatitis, periwound dermatitis, peristomal dermatitis, and medical adhesive related skin injury.
In HLCFs, residents’ skin integrity is affected by health status and care routines, and managing the breakdown of skin integrity often poses a considerable challenge to healthcare workers17. It has long been identified that wound care knowledge in HLCF staff is sub-optimal18, and ongoing education is inadequate19. HLCF residents are frequently transferred to hospital to have their PIs treated20,21. With the appropriate knowledge and support, the residents could have been safely and effectively managed in the HLCF22. Research has proven that unnecessary transfers of older persons, especially those with cognitive impairment, e.g. dementia, is a traumatic experience and frequently leads to iatrogenic complications adversely affecting this cohort’s outcomes22–24. Furthermore, many presentations to emergency departments by residents of HLCFs are often inappropriate and avoidable24,25.
In 2011, a dedicated outreach team was created to provide expert nursing and medical care for members of the community, including HLCF residents, with the view to reducing unnecessary emergency presentations. This type of hospital avoidance strategy improves residents’ outcomes and increases HLCF staff’s confidence and skills26,27. The team consisted of a geriatrician, a registrar, and an advanced practice nurse providing outreach aged care specialist clinical support. The advanced practice nurse, a clinical nurse consultant grade 2 (CNC2), provided clinical consultations and services including, but not limited to, urinary catheterisation, cannulation and venepuncture, comprehensive geriatric assessment, behavioural management, and advanced wound prevention and management. In addition, there was incidental and formal education provided to staff which aimed to improve care delivery on site. Indeed, ongoing education is needed to provide staff with the knowledge to facilitate recognition of deteriorating residents and avoid inappropriate hospital transfers28,29. In fact, HLCF staff would prefer to provide the necessary care for their residents, with adequate support, and not send them to hospital unless it is unavoidable28.
It soon became apparent that there was a lack of knowledge pertaining to the prevention, recognition and management of PIs, as a significant proportion of consultations were for residents with PIs. Most consultations were for severe, i.e., Stage 3 and 4, suspected deep tissue injury (SDTI) and unstageable (U/S) PIs. The outreach CNC2 recognised that there was potential to intervene earlier from a prevention perspective instead of treatment and management of an established PI.
Method
Before the commencement of the QI project, project planning was undertaken with the management and clinical staff of the HLCF. A flowchart (Figure 1) was developed to guide implementation and timeframes. Brainstorming and multi-voting on key project decisions followed, from which affinity and Pareto charts (Figure 2) were developed which identified five main concerns of the staff – lack of specialised education, lack of knowledge, poor communication/handover, lack of decision support for pressure redistribution equipment, and inadequate/absent skin inspections. Pre-implementation knowledge tests were administered to measure knowledge relating to PIs to focus the education on identified knowledge deficits (Supplementary Figure 1).
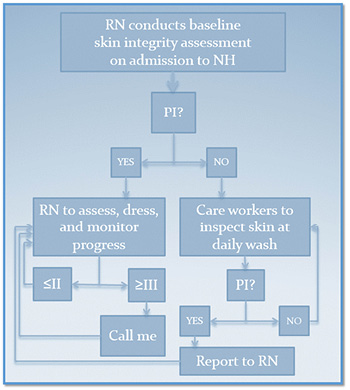
Figure 1. Flowchart of recommended PI monitoring
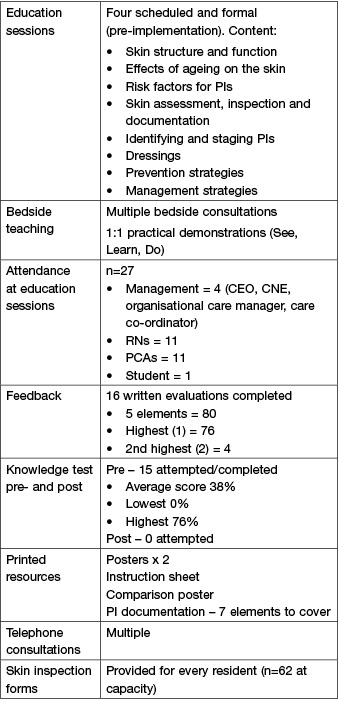
This QI project used validated pressure injury point prevalence audit (PIPPA) methodology30. A pre-implementation PIPPA was conducted to measure baseline point prevalence. Additional baseline data included an environmental survey for pressure redistribution equipment utilisation and functionality. A skin integrity-focused education implementation package (Table 1) was provided to staff, in addition to usual clinical support for residents with PIs. After 7 months, a post-implementation PIPPA was undertaken to measure the change in prevalence and severity, and compliance with a project requirement of daily skin assessments and documentation was also measured.
Table 1. Education implementation package
Ethical considerations
This project was a QI activity and supported by the Local Health District and the management team of the HLCF. Data was de-identified and reported in aggregate. Residents and their family/carers were provided with a participant information statement and consent form for participation in the project (Supplementary Figure 2). Consent from either the resident or person responsible was obtained prior to their inclusion in the PIPPAs which involved a head-to-toe skin inspection.
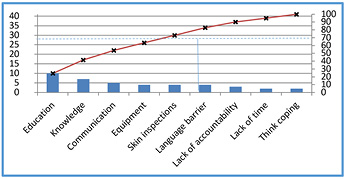
Figure 2. Pareto chart of identified barriers to PI prevention
Sample and setting
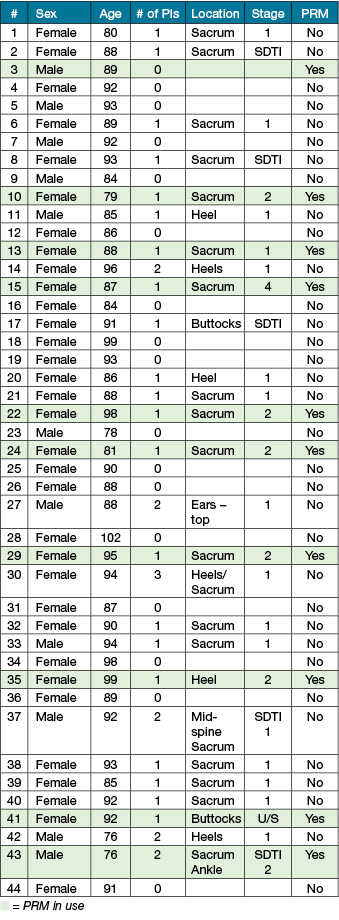
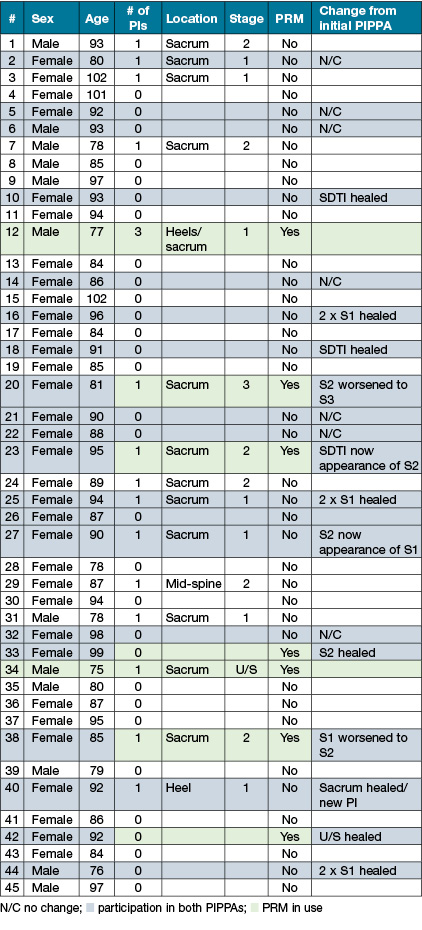
The project site was a 62 bed not-for-profit HLCF in the Sydney metropolitan area. The initial PIPPA included 44 residents over the age of 70 years. The resident, or the person responsible, consented to the skin inspection. 25% were males (11) with an average age of 86 years (range 76–94 years, median 88) and 75% were females (33) with an average age of 87.8 years (range 79–102 years, median 90) (Table 2).
Table 2 with green highlighting denoting use of a pressure relieving mattress
For the post-implementation PIPPA, 45 residents over the age of 70 years, or the person responsible, consented to the skin inspection. 27% were males (12) with an average age of 84 years (range 75–97 years, median 79.5 years) and 73% were females (33) with an average age of 90.6 years (range 78–102 years, median 90). Only 20 residents were included in both the pre- and post-PIPPAs (Table 3), indicating the high mortality rate in 7 months (46.4%). All residents had a high level of acuity.
Table 3 with blue highlighting denoting use of a pressure relieving mattress and green highlighting denoting participation in both PIPPAs)
The HLCF employed approximately 80 staff on a rotating roster, with the majority being part-time or casual. The skill mix was predominantly unskilled healthcare workers/personal care assistants (PCAs). Each shift had two registered nurses (RNs) rostered to oversee the care of up to 62 residents (when occupancy at 100%), although the average occupancy was 90% (approximately 56 residents). The PCAs were responsible for skincare, personal hygiene, nutrition and continence management and thus had significantly higher close interactions with the residents than the RNs. Of note, this facility employed a clinical nurse educator (CNE) from Monday to Friday (excluding public holidays) on day shift. This role is not widespread in HLCFs within the local health district.
Findings
A field observation was that PCAs and RNs did not routinely check or document the condition of residents’ skin when providing personal care, nor did they have the required knowledge and/or skills to do so. This was confirmed by the pre-test of knowledge with an average score of 38% (range 0–76%). It was difficult to establish that the educational implementation improved knowledge and skills as there were minimal pre- and no post-implementation knowledge tests completed. Barriers to their completion included high patient acuity and associated time constraints, low staff/patient ratios, lack of experience, and English language proficiency.
The educational program was well evaluated, with positive feedback such as “Great session” and “I learned so much and a lot [was] helpful to my work”. 27 staff (33%) attended the education sessions, 23 of whom were HLCF staff, including the CNE (Table 1). Sixteen (59%) completed the evaluation form, highly rating the content and that they learned a lot, which triggered requests for education on other types of wounds. Another field observation was that, although the CNE was provided with the materials to continue the remaining staff’s education sessions, these were not delivered.
The CNE was also encouraged to monitor compliance with completion of the skin inspection documentation forms by the staff. On monthly checking of the forms, which were to have been completed on a daily basis, they were mainly incomplete and none were completed in accordance with the instructions.
Over the course of the project, from February until August 2016 inclusive (a total of 212 days), approximately 82 aged persons resided in the HLCF for varying times, some arriving after the start of the project and many dying before the end of the project. All residents had skin inspection forms for staff to complete daily; however, staff only partially completed forms for 50 (61%) of those residents. No one had documentation on every day indicating that their skin had been checked. In fact, the average number of days a resident’s skin was checked over 212 days (excluding residents who did not stay for the duration, n=30), was 73 days (range 37–125, median 59), indicating a compliance rate of 34.4%. Additionally, most forms were incorrectly filled out; for example, in the column “location and stage” instead of “sacrum, Stage 1” general comments were written, such as, “feet”, “redness on bottom”, “redness on her sacrum”, “redness”, “dressing intact”, giving no indication as to the type of skin injury, or, very often, the location. Similarly, in the column “Action taken”, instead of “RN notified” or “silicone border dressing applied”, many comments read, “cream applied” or “dressing intact”. This lack of detail precluded differentiation between PI, IAD and other wound types, and the type of dressing in situ.
The HLCF did not use any risk assessment tool for identifying residents at risk of PIs, and the CNE stated, “All the residents who are admitted here are high risk for everything”. Varying levels of apathy and negativity were observed when staff were asked about PI identification and prevention strategies, such as shoulder shrugging, hands raised palms up, and statements such as “no time”, “too busy”, and “who knows”. It is possible that a lack of English language proficiency played a role in the poor uptake of the project as the majority of staff were from culturally and linguistically diverse backgrounds.
Of the 44 residents audited in the pre-PIPPA, ten (22.7%) had pressure redistribution mattresses (PRMs). Of those ten, nine had PIs (90%) and all but one were Stage 2 or greater, two were U/S and one was a SDTI, whilst the remaining 34 residents without PRMs had a PI prevalence of 56%. In the post-PIPPA, only seven (15.6%) of the 45 residents audited had PRMs. Of those seven, five had PIs (71.4%) and three were Stage 2 or greater, whilst the remaining 38 residents not on PRMs had a PI prevalence of 26.3%. Thus, even without PRMs, it is possible that the prevalence and severity of PIs were significantly reduced due to the increased awareness resulting from skin inspections, regardless of their sporadic performance. There was a 40.3% prevalence of PIs in residents on standard support surfaces compared to a prevalence of 82.4% for residents with PRMs (Tables 2 and 3).
PRMs were not routinely used, despite the high risk of the residents for PIs. At the pre-PIPPA, ten (22.7%) of the 44 residents had alternating air mattresses (AAMs), three of which were set to ‘static’ rather than ‘dynamic’ mode, meaning all the air cells were constantly fully inflated, thus defeating the purpose of the AAM. In the post-PIPPA, only seven (15.6%) of the 45 residents had PRMs, all AAMs, but all were set on ‘dynamic’ mode, indicating an increased awareness and compliance of staff to ensuring the correct functionality of the equipment. The presence, or lack thereof, of PRMs did not appear to impact on the prevalence or severity of PIs.
The pre-PIPPA (n=44) identified 27 residents (61.4%) with a total of 34 PIs (Table 2). Six of those residents had more than one PI; five had two PIs, and one had three PIs. The most common site for a PI was the sacrum (19), followed by heels (9), buttocks (2) and others (4). The severity of PIs was 21 Stage 1 (61%), six Stage 2 (18%), no Stage 3 (0%), one Stage 4 (3%), one U/S (3%) and five SDTI (15%) (Figure 3).
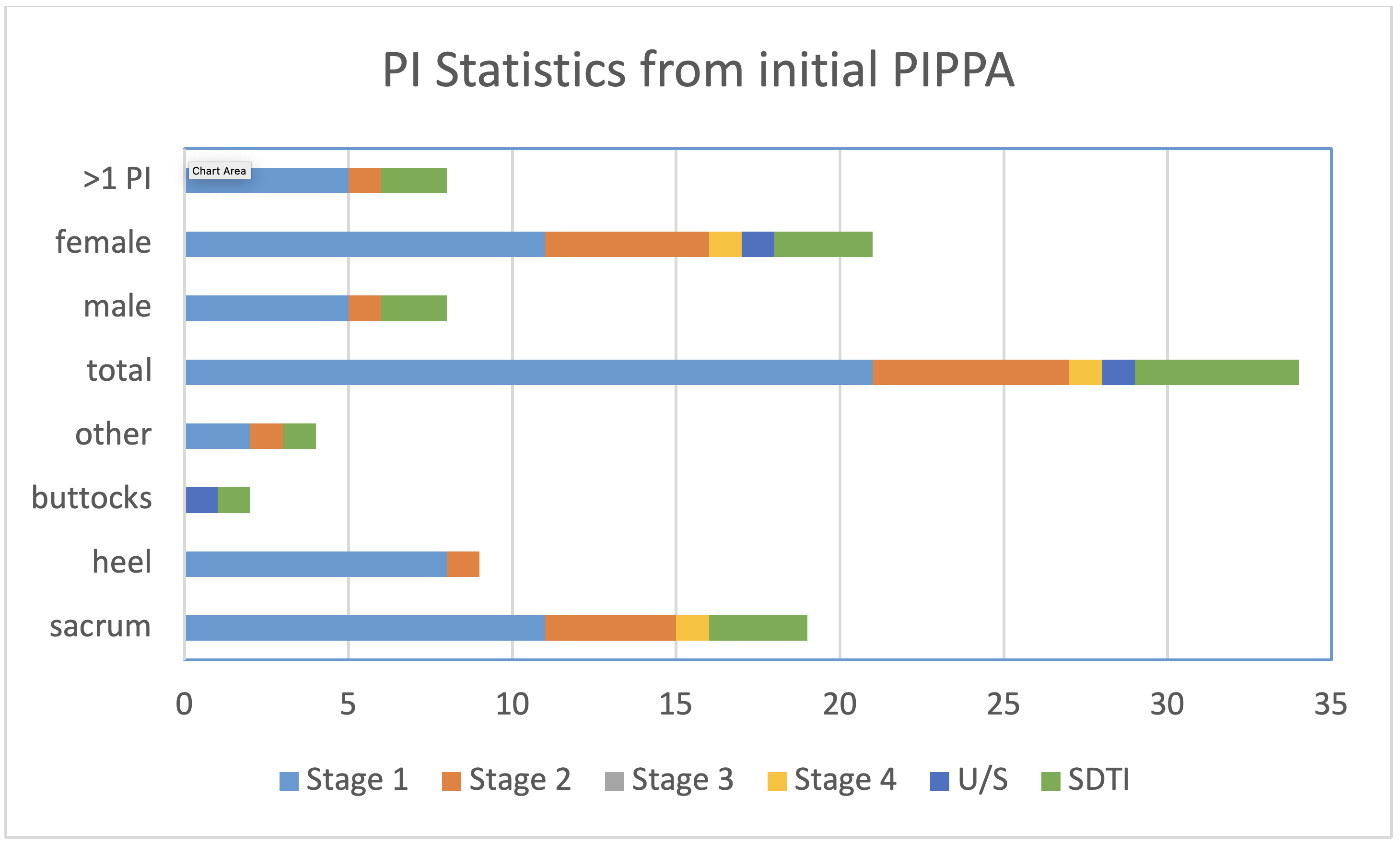
Figure 3. Number and severity of PIs found pre-PIPPA
The post-PIPPA (n=45) identified 15 residents (33.3%), a reduction of 28.1%, with a total of 17 PIs, a reduction of 50% (Table 3). Only one resident had more than one PI (3), a reduction of 83.4% in multiple PI prevalence. The most common site for a PI remained the sacrum (13), followed by heels (3), and other (1). PI severity was reduced, with nine Stage 1 (53%), six Stage 2 (35%), one Stage 3 (6%), no Stage 4 (0%), one U/S (6%) and no SDTIs (0%) (Figure 4). Most significant was a 100% reduction in SDTIs.
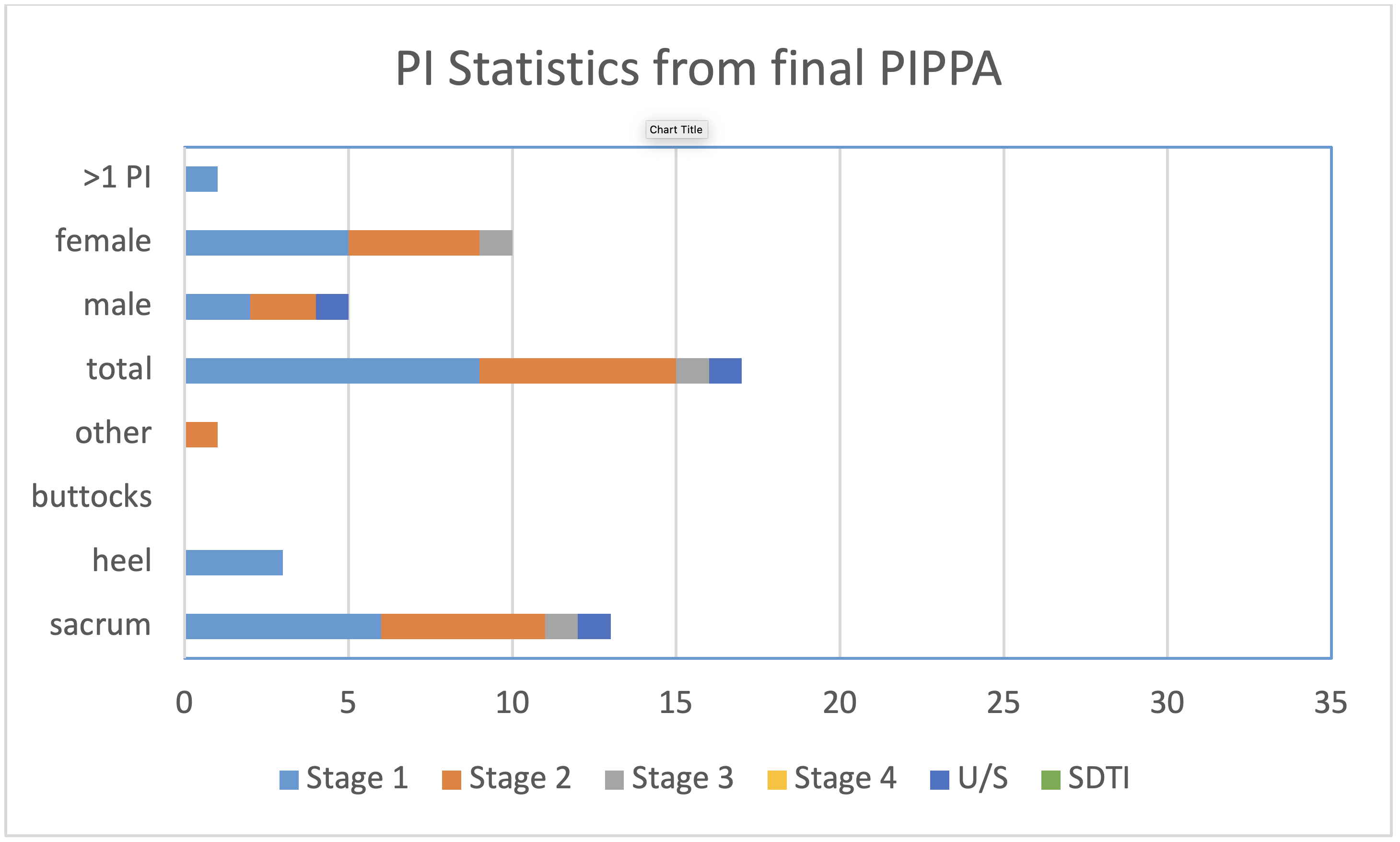
Figure 4. Number and severity of PIs found post-PIPPA
Of note, only 20 residents from the pre-PIPPA were available for and consented to the post-PIPPA. This was mainly due to the deaths of multiple residents during the project. In this group there was a reduction of 58.8% in PIs (17 down to 7) and reduced severity.
Discussion
Scoping this project through observation and project planning with the management and senior clinical teams indicated that PCAs and RNs did not routinely check the skin of residents when providing personal care, nor did they have the required knowledge and/or skills, which was confirmed by research in other aged care settings14,31,32. Limited knowledge relating to skin integrity and PI identification and prevention is common in HLCFs33, which was evident from our low pre-test results. Only 15 staff (approximately 19%) attempted the pre-test with an average score of 38%, supporting other research relating to knowledge deficits. Despite multiple requests and encouragement, no staff attempted the post-test.
Phillips et al.34 identified that new graduate RNs, especially those working in HLCFs, are apprehensive about their responsibilities and need regular education and support. There is evidence that the provision of education has a significant role in improving knowledge and skills of nursing staff and PCAs35 and reduces the incidence of PIs in HLCFs and consequent hospital transfers21,36,37. However, it was difficult for this project to establish that the reduction in prevalence and severity of PIs was a direct result of the education provided. Instead, the reduction is likely due to the introduction of skin inspections, even though they were sporadic at best. Despite the education provided and monthly follow-up visits by the project lead to check and collect the skin inspection forms, none were completed every day. Interestingly, in the education provided, the application of ‘cream’ was not recommended for PIs; rather, applying a silicone border dressing for all Stage 1 and 2 PIs was preferred, which the HLCF had readily available.
Whilst it has been demonstrated that the appropriate pressure redistribution equipment, such as AAMs, can reduce the risk of developing a PI38, this was not found in our project, with higher rates of PIs in those residents with AAMs. When asked about AAMs, most staff believed that their use was sufficient for PI prevention without additional implementations.
Further, the post-PIPPA showed a significant reduction in the number of residents with PIs, from 61.4% down to 33.3%. Most notably, there were no SDTIs, indicating a successful reduction in severe PIs. Overall, the prevalence of PIs was reduced by 50% and the prevalence of severe PIs was reduced by 71.4%.
For the residents who were audited in both PIPPAs (n=20), a decline was noted in their PI prevalence (17 down to 7) and severity. Two of the seven PIs present were significantly improved and healing well, and one Stage 1 had not worsened. One resident had complete healing of a sacral PI but then developed a Stage 1 heel PI. Two patients with three PIs between them had worsened – two Stage 1 demarcating to Stage 2, and a Stage 2 progressing to a Stage 3, all of which were on the sacrum, despite both patients being on AAMs. Our findings are similar to those reported by the AIHW12 that the majority of PIs observed in residential aged care were Stage 1 or 2 (in about equal numbers).
This project’s expected outcomes included improved knowledge and skills, increased critical thinking, and a reduction in the prevalence and severity of PIs, leading to a positive impact upon residents’ quality of life. Due to the absence of post-testing, staff knowledge levels were unable to be measured. However, the reduction in the prevalence and severity of PIs was verified and may be related to an increased awareness resulting from the skin inspections, notwithstanding their inconsistency. This may have translated into an increased implementation of risk reduction strategies.
The issues that our project highlighted need be addressed so that outcomes for residents are improved. It is likely that a whole of system approach, including funding for increased RN presence in HLCFs, is required. Specifically, RNs should be appointed as skin integrity champions and undertake training in the prevention and management of skin injuries. For PCAs, their position description should mandate daily skin inspections together with handover to the supervising RN. Ideally, ongoing education and clinical support should be provided by an advanced practice nurse on a regular basis. A major workforce issue is poor staff retention, and any initiatives developed must factor turnover into sustainability. In terms of resources, evidence-based dressings should be available for early implementation. Further studies are required to measure the prevalence and severity of PIs in HLCFs to develop targeted implementations.
Enablers and barriers to the project
The HLCF Management Team were engaged and supported the project from its inception to completion. The evidence-based silicone border multilayered foam dressings39,40 were purchased and readily available.
The HLCF had a very high ratio of PCAs to RNs; approximately 6:1 on most shifts. Because the work of PCAs has been recognised as task-oriented, arduous and stressful41, there was significant staff turnover42 during the project. Many RNs were new graduate nurses with no hospital experience or minimal/no training in aged care nursing, despite the Australian College of Nursing (ACN) Position Statement1 that, due to the complex needs of residents, safe nursing care should be provided by appropriately qualified and experienced nurses.
The staff had multiple residents under their care, and time constraints posed a significant barrier to completing the newly introduced skin inspection form. It is possible that more skin inspections were carried out than were documented. If this aspect of the project was measured at another time point when this form was more familiar to staff, there might have been an improvement in skin inspection documentation. It is likely that the introduction of a form that facilitates the capture of both PI risk assessment and skin inspections would improve not only awareness but also implementations and documentation.
Also, the time constraints likely prohibited more staff from attending the education sessions. Although the CNE was provided with additional educational materials, no further education was delivered, indicating that the staff may have had limited educational opportunities. From serial field observations, the CNE did not engage with the staff and encountered significant difficulty motivating the PCAs to document the skin inspections which was never done correctly or consistently, nor was she able to persuade them to attempt the post-test. This supports evidence that a negative attitude is not uncommon when there is a lack of knowledge and skills in an area43.
Most staff in the HLCF had a first language other than English, and their English varied from rudimentary to proficient, but mostly the former. It may be that difficulties with effective communication were a factor in the poor uptake of the project’s implementations and instruments to measure project outcomes.
This project relied on one person (CNE) in the HLCF to link the hospital-based outreach project lead (CNC2) in, and her support was variable. The CNE did not deliver the ongoing education package supplied to facilitate PI knowledge and compliance with the project. There were gaps in the project data sets due to staff failing to document skin inspections, low completion of the pre-test, and no post-testing.
Conclusion
The delivery of care to the frail, older person in residential aged care has increasingly fallen to unskilled workers with little to no education or support and, in many instances, of culturally and linguistically diverse backgrounds. The skin integrity issues that this project has highlighted demonstrate a need to engage these workers in risk assessment and reduction of skin problems, including PIs, skin tears and IAD, together with ongoing education and support. Regular skin inspections increase awareness and reduce the incidence and severity of injuries due to pressure and moisture. There may be an over-reliance on equipment and, in this project, PRMs had no detectable effect on the prevention of PIs. Point prevalence is not the best data to demonstrate prevention of PIs, but the difficulties of collecting robust PI incidence data has resulted in many centres resorting to point prevalence as a quality indicator. Further studies are required to measure the burden of wounds in residential aged care, including PI incidence and severity. Only from this data can specific implementations be developed and measured to ensure cost-effectiveness and improvement to both the residents’ and staff’s experience.
The Royal Commission into Aged Care2 recently highlighted issues relating to skin and wounds, and we have confirmed that this is an area for further attention, including more funding to ensure highly skilled RNs are available to care for these vulnerable people.
Acknowledgements
We acknowledge WoundsWest for the PIPPA methodology.
Conflict of interest
The authors declare no conflicts of interest.
Funding
The authors received no funding for this study.
Click here to download the supplementary tables.
Author(s)
Allyson Waird*
RN, BN, MN, JP
Aged Care, Delirium and Dementia
Clinical Nurse Consultant
North Shore & Ryde Health Service, NSW, Australia
Email Allyson.Waird@health.nsw.gov.au
Susan Monaro
RN, BAppSc (Nursing), MN and PhD
Skin Integrity Improvement Facilitator
Clinical Governance Unit
Northern Sydney Local Health District, NSW, Australia
Clinical Senior Lecturer
Susan Wakil School of Nursing and Midwifery
University of Sydney, NSW, Australia
* Corresponding author
References
- Australian College of Nursing. The role of registered nurses in residential aged care facilities: Position statement 2016. https://www.acn.edu.au/wp-content/uploads/position-statement-role-rn-residential-aged-care-facilities.pdf Accessed: 10/12/2020.
- Royal Commission into Aged Care Quality and Safety. Medium- and long-term pressures on the system: the changing demographics and dynamics of aged care: background paper 2. In: Commission Office of the Regulator, editor. Canberra: Australian Government; 2019.
- Australian Institute of Health and Welfare. Older Australia at a glance. 2018. https://www.gen-agedcaredata.gov.au/Topics/Admissions-into-aged-care/Explore-admissions-into-aged-care Accessed 12/12/2020.
- Inouye S, Studenski S, Tinetti M, Kuchel G. Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept. J Am Geriatric Soc 2007;55(5):780–91.
- Tinetti ME, Inouye SK, Gill TM, Doucette JT. Shared risk factors for falls, incontinence, and functional dependence: unifying the approach to geriatric syndromes. JAMA 1995;273(17):1348–53.
- Campbell J, Coyer F, Osborne S. The skin safety model: reconceptualizing skin vulnerability in older patients. J Nurs Scholars 2016;48(1):14–22.
- Hajhosseini B, Longaker M, Gurtner G. Pressure injury. Ann Surg 2020 271(4):671–9.
- European Pressure Ulcer Advisory Panel, National Pressure Ulcer Advisory Panel, Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers/Injuries: Clinical Practice Guideline: EPUAP/NPIAP/PPPIA; 2019.
- Payne D. Skin integrity in older adults: pressure-prone, inaccessible areas of the body. Br J Comm Nurs 2020;25(1):22–6.
- Wilson L, Kapp S, Santamaria N. The direct cost of pressure injuries in an Australian residential aged care setting Int Wound J 2019;16(1):64–70.
- Righi L, Ourahmoune A, Bene N, Rae A, Courvoisier S, Chopard P. Effects of a pressure-ulcer audit and feedback regional programme at 1 and 2 years in nursing homes: a prospective longitudinal study. PLoS ONE. 2020.
- Australian Institute of Health and Welfare (AIHW). GEN aged care data: residential aged care quality indicators. In: AIHW, editor. Canberra; 2020.
- Birkill K. Deal with heels: a pressure ulcer prevention initiative. Br J Comm Wound Care 2020;25(3):S6–S10.
- Aydin AK, Karadag A, Gül S, Avsar P, Baykara ZG. Nurses’ knowledge and practices related to pressure injury: a cross-sectional study. J Wound Ostomy Continence Nurs 2019;46(2):117–23.
- Barakat-Johnson M, Lai M, Wand T, Coyer F, White K. Systemwide practice change program to combat hospital-acquired pressure injuries: translating knowledge into practice. J Nurs Care Qual 2020;35(1):51–7.
- Campbell J, Barakat-Johnson M, Hogan M, Maddison K, McLean J, Rando T, et al. A clinical guide to pelvic skin assessment. Wounds Int 2020;11(1):30–9.
- Brimelow RE, Wollin JA. The impact of care practices and health demographics on the prevalence of skin tears and pressure injuries in aged care. J Clin Nurs 2018;27(7–8):1519–28.
- Meesterberends E, Wilborn D, Lohrmann C, Schols JM, Halfens RJ. Knowledge and use of pressure ulcer preventive measures in nursing homes: a comparison of Dutch and German nursing staff. J Clin Nurs 2014;23(13–14):1948–58.
- Teresi JA, Ramirez M, Remler D, Ellis J, Boratgis G, Silver S, et al. Comparative effectiveness of implementing evidence-based education and best practices in nursing homes: effects on falls, quality-of-life and societal costs. Int J Nurs Stud 2013;50(4):448–63.
- Mazza D, Pearce C, Joe A, Turner LR, Brijnath B, Browning C, et al. Emergency department utilisation by older people in metropolitan Melbourne, 2008–12: findings from the Reducing Older Patient’s Avoidable Presentations for Emergency Care Treatment (REDIRECT) study. Aust Hlth Rev 2018;42(2):181–8.
- Unroe KT, Carnahan JL, Hickman SE, Sachs GA, Hass Z, Arling G. The complexity of determining whether a nursing home transfer is avoidable at time of transfer. J Am Geriatric Soc 2018;66(5):895–901.
- Dwyer R, Gabbe B, Stoelwinder JU, Lowthian J. A systematic review of outcomes following emergency transfer to hospital for residents of aged care facilities. Age Ageing 2014;43(6):759–66.
- Hullick C, Conway J, Higgins I, Hewitt J, Dilworth S, Holliday E, et al. Emergency department transfers and hospital admissions from residential aged care facilities: a controlled pre-post design study. BMC Geriatric 2016;16(1):1–10.
- Dwyer RA, Gabbe BJ, Tran T, Smith K, Lowthian JA. Predictors of transport to hospital after emergency ambulance call-out for older people living in residential aged care. Australas J Ageing 2020.
- Lukin B, Fan L-j, Zhao J-z, Sun J-d, Dingle K, Purtill R, et al. Emergency department use among patients from residential aged care facilities under a hospital in the nursing home scheme in public hospitals in Queensland Australia. World J Emerg Med 2016;7(3):183.
- Santosaputri E, Laver K, To T. Efficacy of interventions led by staff with geriatrics expertise in reducing hospitalisation in nursing home residents: a systematic review. Australas J Ageing 2019;38(1):5–14.
- O’Neill BJ, Dwyer T, Reid-Searl K, Parkinson L. Managing the deteriorating nursing home resident after the introduction of a hospital avoidance programme: a nursing perspective. Scand J Caring Sci 2017;31(2):312–22.
- Stokoe A, Hullick C, Higgins I, Hewitt J, Armitage D, O’Dea I. Caring for acutely unwell older residents in residential aged-care facilities: perspectives of staff and general practitioners. Australas J Ageing 2016;35(2):127–32.
- Lemoyne SE, Herbots HH, De Blick D, Remmen R, Monsieurs KG, Van Bogaert P. Appropriateness of transferring nursing home residents to emergency departments: a systematic review. BMC Geriatric 2019;19(1):1–9.
- Prentice J, Stacey M, Lewin G. An Australian model for conducting pressure ulcer prevalence surveys. Primary Intent 2003;11(2):87–8,90–1,3–6,8–100,2–9.
- Courvoisier DS, Righi L, Béné N, Rae A-C, Chopard P. Variation in pressure ulcer prevalence and prevention in nursing homes: a multicenter study. Applied Nurs Res 2018;42:45–50.
- Fulbrook P, Lawrence P, Miles S. Australian nurses’ knowledge of pressure injury prevention and management: a cross-sectional survey. J Wound Ostomy Continence Nurs 2019;46(2):106.
- Seo Y, Roh YS. Effects of pressure ulcer prevention training among nurses in long-term care hospitals. Nurse Educ Today 2020;84:104225.
- Phillips C, Kenny A, Esterman A, Smith C. A secondary data analysis examining the needs of graduate nurses in their transition to a new role. Nurse Educ Pract 2014;14(2):106–11.
- Berlowitz D, Berman RS, Cochran A. Epidemiology, pathogenesis, and risk assessment of pressure-induced skin and soft tissue injury. UpToDate; 2020. Available from: https://www-uptodatecom.proxy2.biblio.supsi. ch/contents https://www.uptodate.com.acs.hcn.com.au/contents/epidemiology-pathogenesis-and-risk-assessment-of-pressure-induced-skin-and-soft-tissue-injury Accessed: 21/09/2020.
- Olsho LE, Spector WD, Williams CS, Rhodes W, Fink RV, Limcangco R, et al. Evaluation of AHRQ’s on-time pressure ulcer prevention program: a facilitator-assisted clinical decision support intervention for nursing homes. Med Care 2014:258–66.
- Yilmazer T, Tuzer H, Erciyas A. Knowledge and attitudes towards prevention of pressure ulcers: intensive care units sample in Turkey. Turkiye Klinikleri Hemsirelik Bilimleri 2019;11(2).
- Ahtiala M, Kivimäki R, Laitio R, Soppi E. Effect of mattress deployment on pressure ulcer development: a real-world observational cohort experience. Wounds Int 2020;11(1):10–7.
- Serrano J, Paiva CF, Dong F, Wong D, Neeki M. Sacral pressure injury prevention in trauma patients: silicone-bordered multilayered foam dressing. J Trauma Nurs 2020;27(4):246–9.
- Santamaria N, Gerdtz M, Sage S, McCann J, Freeman A, Vassiliou T, et al. A randomised controlled trial of the effectiveness of soft silicone multi-layered foam dressings in the prevention of sacral and heel pressure ulcers in trauma and critically ill patients: the border trial. Int Wound J 2015;12(3):302–8.
- Brodaty H, Draper B, Low LF. Nursing home staff attitudes towards residents with dementia: strain and satisfaction with work. J Adv Nurs 2003;44(6):583–90.
- Roe J, Coulson S, Ockerby C, Hutchinson AM. Staff perceptions of caring for people exhibiting behavioural and psychological symptoms of dementia in residential aged care: a cross-sectional survey. Australas J Ageing 2020;39(3):237–43.
- Lotfi M, Aghazadeh AM, Asgarpour H, Nobakht A. Iranian nurses’ knowledge, attitude and behaviour on skin care, prevention and management of pressure injury: a descriptive cross-sectional study. Nursing Open 2019;6(4):1600–5.



