Volume 29 Number 3
Feasibility and acceptability of implementing a patient education pressure injury prevention care bundle in acute care: an interview study
Sharon L Latimer, Jodie L Deakin, Wendy P Chaboyer and Brigid M Gillespie
Keywords pressure ulcer, implementation, patient perceptions, qualitative, nurse perceptions
For referencing Latimer SL et al. Feasibility and acceptability of implementing a patient education pressure injury prevention care bundle in acute care: an interview study. Wound Practice and Research 2021; 29(3):163-170
DOI
https://doi.org/10.33235/wpr.29.3.163-170
Submitted 4 June 2021
Accepted 30 June 2021
Abstract
Aim To describe and compare patients’ and nurses’ perceptions of the feasibility and acceptability of a patient education pressure injury prevention (PIP) care bundle (PPIPCB).
Methods Semi-structured patient interviews and nurse focus groups were conducted in three medical units of an Australian metropolitan hospital. Qualitative data were gathered on participants’ experiences of PIP education on hospital admission and their views of the acceptability of implementing a PPIPCB. Following inductive content analysis of the data, the categories were comparatively analysed and the themes defined.
Results Patients reported receiving limited education from nurses, while heavy workloads were a major barrier to nurses delivering patient education. Patients and nurses valued PIP education and wanted more time and resources to engage in this activity. The PPIPCB was viewed by both patients and nurses as a useful resource that could facilitate information sharing between nurses, patients and their families.
Conclusion Nurses have a key role in educating patients about PIP care, with accessible resources needed to facilitate this activity. Our PPIPCB provides patients and nurses with simple to implement strategies that could increase patients’ participation in their care.
Impact
What is already known?
- Hospital-acquired pressure injuries (HAPI) are a patient safety and quality of care issue
- Patient participation in their PIP care is a strategy that can reduce the risk of HAPI.
- In acute care hospitals, there is limited availability of patient education resources to increase patient participation in their PIP care.
What does this implementation project contribute?
- Heavy workloads reduced nurses’ ability to provide patients with PIP education on hospital admission.
- Patients and nurses valued PIP education.
- Access to PPIPCBs that outline simple prevention strategies can encourage patients to participate in their care.
Background
Hospital-acquired pressure injuries (HAPI) are preventable skin/tissue injuries resulting from unrelieved pressure, shear or friction1. For patients, HAPI result in pain, infection1,2 and an increased hospital length of stay by up to 20 days3. HAPI are a global problem, with Li et al.’s4 meta-analysis of almost two million hospital patients reporting a pooled estimate of pressure injury (PI) prevalence of 12.8% and a pooled HAPI rate of 8.4%. During 2016, treating HAPI was estimated to cost US$26.8 billion in the US3 and £5.3 billion in the United Kingdom5. In Australia during 2012–13, HAPI treatment costs were estimated at A$1.8 billion6, hence preventing HAPI is a global priority. International clinical practice guidelines recommend pressure injury prevention (PIP) strategies including repositioning, support mattresses, risk assessment, nutritional and skin care, and patient education1,7. However, inconsistencies in their implementation are reported8,9.
Care bundles are three to five evidence-based practices that, when delivered together, can prevent and manage health issues10. Centred on patient participation in their care, a PIP bundle and associated resources are freely available (http://bit.ly/PIPtoolkit) which aim to improve patients’ health literacy and educate them on preventative strategies they can implement during their hospitalisation11. This PPIPCB has been previously tested12; however, its use in routine clinical practice, including barriers and facilitators, has not been examined. The results of this study will support clinicians tasked with preventing HAPI and improving patient PIP engagement in the hospitalised setting.
Method
Aim
To describe and compare patients’ and nurses’ perceptions of the feasibility and acceptability of a PPIPCB in routine clinical practice, including barriers and enablers. The COnsolidated criteria for REporting Qualitative research (COREQ) checklist was followed13.
Design
A descriptive qualitative study.
Setting
Three, 28-bed adult acute medical units (respiratory, general medical and infectious disease) at a large metropolitan Australian hospital. Each patient’s bedside has an interactive touch screen (patient entertainment system [PES]) with 24/7 unrestricted access to entertainment and safety videos14.
Sample
Patients and nurses from the three wards were recruited once to the study. A purposive sample of nurses were recruited and a consecutive sample of patients, regardless of their PI risk, were recruited. Patient inclusion criteria were: aged ≥18 years, provided written consent, hospitalised for ≥48 hours, and could view and read the PPIPCB. Patient exclusion criteria were: receiving palliative or end-of-life care. All permanently employed nursing staff could be recruited. Purposive sampling using maximum variation (age, gender, professional role, experience)15 was used to capture a range of nurses’ perspectives16.
Implementation
PPIPCB
The PPIPCB consists of a professionally developed 6-minute video, colour poster and brochure outlining three patient PIP strategies – keep moving, eat a healthy diet, and look after your skin12. To cater to a diverse range of hospitalised patients, the PPIPCB is available in nine languages (Arabic, Chinese, Croatian, English, Greek, Italian, Somalian, Spanish, Vietnamese)12.
Data collection
Prior to data collection, the nine videos were uploaded onto the PES and colour posters and brochures were printed to retain at the bedside. The site research fellow (SL) conducted staff information sessions outlining the study purpose and collection methods. In September 2019, the researcher (SL), with doctoral expertise in PI and qualitative experience, conducted face-to-face patient interviews and nurse focus groups (one per unit) in a quiet area. The nurse in charge assisted in identifying potential patient and nurse participants. All eligible participants invited to the study were informed about the study, anonymity, withdrawal process and the research team’s goals and study site relationship. Potential participants were given time to consider their decision, with a written consent gathered from those willing to be recruited. Interviews were digitally recorded.
Patient semi-structured interviews: Using an interview guide, patient participants were asked about the PIP education they received on admission. They viewed the PPIPCB and their perceptions of the information and strategies were discussed. Finally, patients were asked how they might incorporate the information into their care, including barriers and facilitators, and how we could implement the PPIPCB in the unit. Self-reported de-identified demographic and clinical data were gathered.
Nurse focus groups: The questions, guided by the Theoretical Domains Framework17, focused on professional role, knowledge, decision making, environmental stressors, barriers and facilitators. Nurses were asked about who educated patients about PIP during their admission, including the information delivered. Next, nurses viewed the PPIPCB and were invited to comment on the information and strategies. Barriers and facilitators were explored regarding PPIPCB implementation. De-identified demographic and professional data (age, gender, years of clinical experience, highest qualification, working hours) were collected.
The interview/focus group questions were developed by the research team who have expertise in PI and qualitative research. Following pilot-testing in the first interview/focus group, minor changes to the question sequence were made, with the PPIPCB shown after the first two questions were asked18,19. Following each interview/focus group, the researcher (SL) documented detailed content summaries on key discussion points.
Ethics
Ethical approvals were granted by the relevant hospital and university Human Research Ethics Committees [HREC/2019/QGC/49756; GU/2019/375].
Data analysis
Prior to analysis, the audio data files were professionally transcribed. The researcher (SL) checked the transcripts for accuracy and deleted filler statements (e.g. “um”). Participant anonymity prevented the returning of transcripts for correcting. Demographic and professional data were entered into SPSS20, cleaned, and checked for accuracy. Depending on the data distribution, descriptive statistics were computed using absolute (n) and frequencies (%), mean [standard deviation (SD)] or median (interquartile range [IQR]).
Inductive content analysis16 then comparative analysis21 of the qualitative data was undertaken. First, the patient and nurse data were separately analysed using inductive content analysis, with an iterative and reflexive process followed to identify data patterns and meanings16. Two researchers (SL, JD) reviewed the data by re-reading the transcripts16. Next, data coding occurred, with similar codes organised into sub-categories, which were subsequently arranged into categories and defined16. The categories were comparatively analysed, with the differences and similarities compared and contrasted, and the resulting themes defined (SL, JD)21. This narrative data synthesis resulted in a deeper understanding of the similarities and differences in patients’ and nurses’ perceptions of the feasibility, acceptability, barriers and enablers to implementing the PPIPCB21. SL and JD lead the analysis, and the research team agreed on the final analysis based on consensus16.
Qualitative research rigour was established through credibility, transferability, dependability and confirmability22. Credibility was achieved by triangulation (multiple data sources), retaining participants own words throughout the analysis, and the research team discussing the preliminary findings22. Transferability or generalisability of findings was achieved through purposive sampling and context selection; hence gathering a range of participant perspectives and thick data descriptions22. Dependability was achieved by triangulation and documenting research processes and procedures to ensure consistency and reliability of data22. Confirmability, or neutrality, was established through triangulation, reflexive discussions, detailed field notes and documenting a data analysis codebook22.
Results
Demographic data
Ten medical patients were approached, with nine recruited and interviewed for up to 15 minutes each. The patient sample was mostly female (n=7; 78%) and their age ranged from 20–83 years, with a median of 71 years (IQR=27:80). Just over half (n=5; 55.5%) of patient participants were independently mobile. No participants had an existing PI.
Twenty nurses participated in the three focus groups, which lasted between 30–40 minutes each. The nurse sample were mainly female (n=15; 75%) and were registered nurses (n=17; 85%). Nurse participants’ age ranged between 22–68 years (Mean=40; SD=13). Most were degree level qualified (n=11; 58%) with a median 7.0 years (IQR=3:10) of clinical experience.
Patients’ perceptions
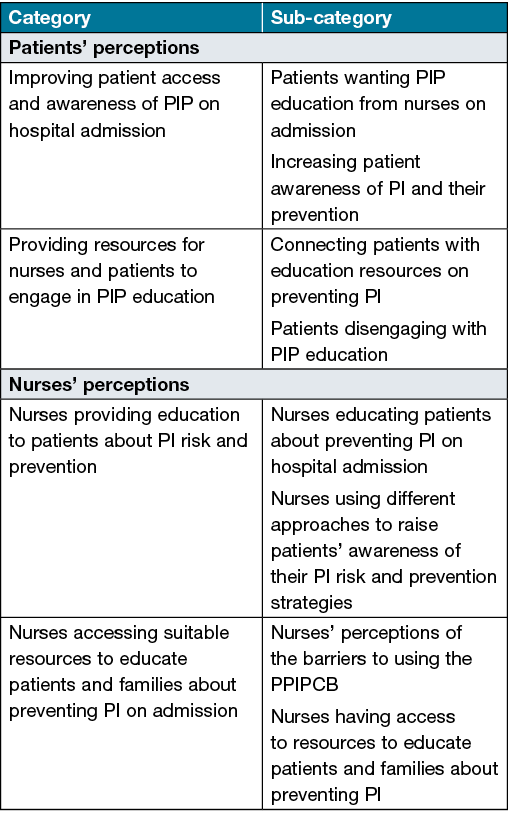
Two categories (Table 1) emerged from the patient data: improving patient access and awareness of PIP on hospital admission; and providing resources for nurses and patients to engage in PIP education.
Table 1. Inductive content analysis of patients’ and nurses’ perceptions of PPIPCB
Improving patient access and awareness of PIP on hospital admission
On hospital admission, patients had little awareness of PI, prevention and their potential negative impacts. As one patient stated, “We didn’t understand what a pressure injury was”. Furthermore, most patients reported receiving limited or no PIP education from nurses, “They briefly said, you know that there’s info if you want to look at it it’s on there [PES]. They didn’t say what was on it they just said, patient information”. All patients remarked it was important for them to know more about preventing PI, yet “it wasn’t explained to us… on admission”. Most patients also indicated they feared viewing graphic wound images during PIP education, saying “That’s to avoid… we thought it contained gruesome info”.
After viewing the PPIPCB, patients reported the information increased their awareness of PI and their prevention, claiming “Very useful, because I didn’t know any of it before”. Reflective of all patients, “The DVD [video] provides valuable and easy to use information for patients who are in hospital. It is good quality, simple messages [keep moving, eat a healthy diet and look after your skin] and easy to access on the PES”. Some patients confidently deployed the PPIPCB video on the PES platform, while others were reluctant to access the resource, saying “I would feel very confident using the DVD [video]and other resources as long and I was told where to access them”. All patients indicated they could incorporate all or some of the suggested PPIPCB strategies into their care if they received more guidance from nurses, saying “Well, it’s something that you don’t think of until you’re aware of it”.
Providing resources for nurses and patients to engage in PIP education
Patients wanted more education from nurses so they could be more involved in their PIP care. As one patient remarked, “I already had a bit of prior [PI] knowledge… [so] I was trying to move around as much as possible”. Many patients wanted nurses to facilitate their engagement with the PPIPCB on the PES by “The nurse pulling the computer over, clicking on the folder and saying, ‘look this is what it looks like, it’s here’”. Other patients suggested the healthcare organisation should develop a rolling screensaver on the PES that directed patients to the information – “If it was just on that [PES] as a screensaver and it was just continually going and… you want to click in and…. watch that video”. Patients valued individualised education sessions and reported the PPIPCB allowed them to select their preferred modality (e.g. video, poster, brochure). As one patient indicated, “I think it would just give me a little bit of information in terms of a flyer before I did gravitate towards watching the video”.
Several factors that might cause patients to disengage with the PPIPCB were highlighted. Technology accessibility and reliability reduced patients’ ability to engage with education resources, claiming “Using the touchscreen and it didn’t work [so] I was really put off by it”. Concerns were also raised about physical and cognitive impairments that would restrict patient access to the PPIPCB – “If you were too tired, deaf or had a medical problem that stops you from accessing the PES or reading/understanding the information”.
Nurses’ perceptions
Two categories (Table 1) were produced from nurse data: nurses providing education to patients about PI risk and prevention; and nurses accessing suitable resources to educate patients and families about preventing PI.
Nurses providing education to patients about PI risk and prevention
Nurses acknowledged it was their role to educate patients about preventing PI on hospital admission, saying “The primary nurse educates patients about pressure injury prevention”. Their goal was to raise patients’ awareness of their PI risk and prevention strategies, “Telling them that we’re going to get them to sit up in the chair” and “I always tell them I’ve got to move them off their bottom because it’s getting red”. Reflective of other nurse participants, one nurse described how she informs patients about “How easy it is to get them [PI] because people really have no idea how easy just a redness can actually turn into broken skin”.
Nurses conceded PIP education was often rushed and situated in a vast amount of health and safety information delivered to patients on admission – “Workload pressure, but there’s also [nurse] awareness. There’s so much pressure on bedside nurses to go through the 27 steps of a patient admission”. All nurses recognised hospital admission was a stressful and busy time for patients, resulting in some either being unwilling or too ill to fully participate in this education session, saying “[education occurs] on orientation if the patient is up to it and they’re accepting to take that”. Nurses educated patients about repositioning and moisturising their skin via face-to-face conversations, demonstrations and during care delivery – “We get them to sit up in the chair for lunches and breakfast, because they’ve got to keep moving”, and saying they “Help [patients] with the moisturising... we usually have moisturiser in each room”.
Nurses accessing suitable resources to educate patients and families about preventing PI on admission
Most nurses considered the existing hospital PI education resources were unenticing. In comparison, nurses reported the PPIPCB was a high quality and engaging production and a valuable patient education tool for them to use, especially with patients from non-English speaking backgrounds, saying “It’s an education tool for us, because sometimes those things are hard to explain without visual cues” and “The video’s good, at least it’s a different way of delivering the information than us just telling them [patients]”. All nurses agreed some patients with impairments (cognitive, hearing, visual) or those who are unwell would not be able to use the education resource, saying “Those with cognitive impairment, they wouldn’t understand it, or they’d forget it after they’ve seen it”. Others suggested families and carers could access the PPIPCB and then help patients to be involved in their PIP care – “But I think with carer support that could be good information to complement their existing knowledge or inform them of a concept which might be more [enquiring] to them”.
Comparative analysis
Three comparators were used: PIP education on admission; PPIPCB as an education resource; and implementing PPIPCB, with two themes emerging – contrasting experiences of PIP education on admission, and increasing information sharing between nurses and patients on admission through well-designed and accessible PIP education resources (Table 2).
Contrasting experiences of PIP education on admission
Patients and nurses had different experiences of PIP education on admission. Patients stated they received little or no PIP education from nurses on admission, confirming why their awareness of PI and prevention strategies was limited. Hospital patients are powerless to know how and where to access PIP education information, instead relying on nurses to guide them. Furthermore, PI awareness is often beyond the personal experience of most hospital patients and may be considered by many to be a challenging issue to discuss.
In contrast, nurses indicated hospital patients receive PIP education on admission with the aim of raising their awareness of PI risks and prevention. Workload pressures meant nurses delivered patient PIP education in a rushed manner which can result in patients experiencing surface learning of complex PI concepts. In addition, it is likely nurses lacked the time to check for patient learning and facilitate patients’ application of new PIP knowledge and strategies. Despite these differences and similarities, patients and nurses wanted more resources and time to engage in PIP education on admission because it raised their PI awareness and the importance of prevention.
Increasing information sharing between nurses and patients on admission through well-designed and accessible PIP education resources
Education has its greatest impact when it is individualised. Together, patients and nurses overwhelmingly valued the PPIPCB as an education tool that should be implemented into clinical practice. Most valued the resource quality, the ability to individualise education sessions, its ease of use and simple messaging. Nurses appreciated the alignment of the suggested patient strategies to the information they currently deliver. Nurses acknowledged difficulties in accessing individualised education for culturally diverse patients and families. Hence, the multi-lingual PPIPCB resources were viewed as filling this practice gap (Table 2). Nurses confirmed delays and costs associated with accessing professional interpreters. Similarly, patients and families from a non-English speaking background may be reluctant to request these services. As such, having easy access to multi-lingual PIP resources may increase culturally diverse patients and family’s willingness to engage with the PPIPCB and their care (Table 2).
Table 2. Comparative analysis of patients’ and nurses’ perceptions
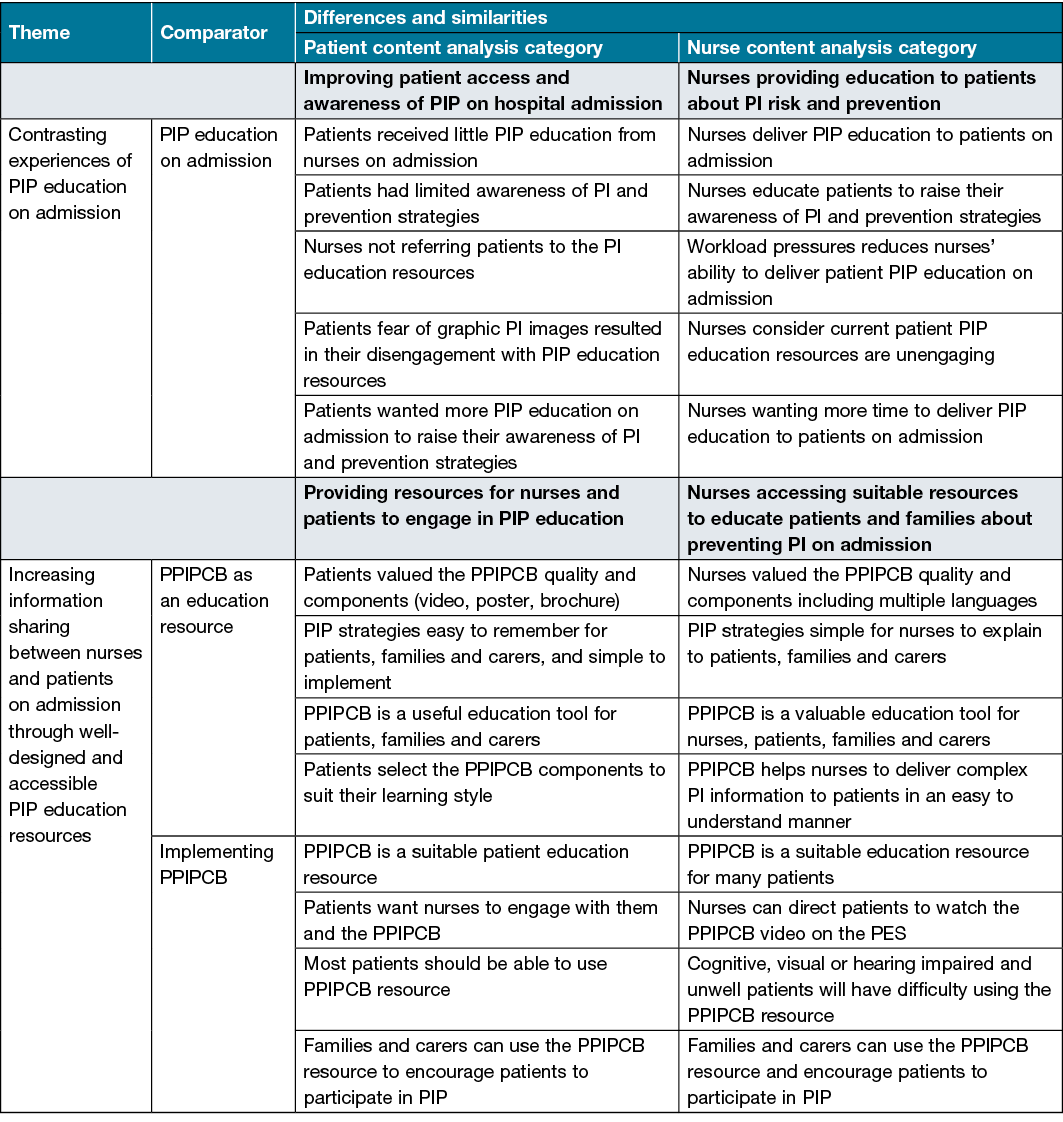
To gain the greatest benefits from patient education, active participation is needed. Patients and nurses both acknowledged some unwell or impaired patients would be unable to effectively use the PPIPCB. However, nurses suggested families and carers could watch the video and encourage unwell or impaired patients to reposition. Patients appreciated they could access the PPIPCB in a flexible and autonomous manner, yet many wanted nurses to actively engage with them in PIP education. In contrast, nurses perceived the resource could reduce their admission workload by allowing patients to view the video while they completed other admission requirements. While likely unintentional, this passive approach to patient education is probably due to the workload pressures nurses experience during the complex hospital admission process. Patients and nurses expressed similar views regarding the value of the PPIPCB as an education resource to increase information sharing on PIP.
Discussion
This study examined medical patients’ and nurses’ perceptions of the feasibility and acceptability, including barriers and enablers, of implementing a PPIPCB in their clinical unit. This study provides insights into the differing patient and nurse experience of PIP education on hospital admission and the value of providing a well-designed PPIPCB to promote the active sharing of complex PI concepts aimed at encouraging patients to participate in their care.
Most patient participants reported their PIP awareness was limited on admission; a new study finding. In contrast, McInnes et al.23, found 86% of their acute care patient participants understood the concept of PI. Both studies were conducted in metropolitan areas and participants were a similar age, so the differences in findings could be that our patients had limited access to PIP information in the community, a factor previously reported24. Nurses also acknowledged most patients were unaware of how quickly PI develop. Recently, Durrant et al.24 found community-based patients could not adequately explain why their PI developed. Examining hospital patients’ comprehension of PI and PIP is suggested and will help to establish if this lack of knowledge is widespread.
Nurses play a key role in educating patients about PIP25. Yet, our patient participants indicated they received limited PIP education from nurses on admission, confirming previous findings23,26,27. Nurses in our study stated they delivered PIP education to patients on admission; however, they recognised workload pressures impeded their ability to consistently deliver quality education sessions, an issue reported by others28,29. Furthermore, the admission process is stressful, complex and demanding for patients and nurses28–30 which may explain our findings. For patients, in addition to being unwell, hospital admission results in separation from familial support networks, being in an unfamiliar environment30, and receiving complex health information26,27. For nurses, admitting a patient to their unit involves the hasty completion of complex administrative and clinical tasks28,29. Heavy nurse workloads impinge on patient education time and is a modifiable factor29,31 that management can address.
Our patient and nurse participants wanted more time and resources to engage in PIP education, with limited access to resources causing nurses to experience increased stress29. Hospital admission might not be the optimal time to deliver the bulk of PIP education, with consideration given to integrating education throughout their routine care, including handover throughout the course of their hospital stay32. Offering multiple opportunities to deliver the PIP education might help patients to consolidate their learning27 and confidently participate in their care2.
Some patients were reluctant to engage with the PPIPCB because they feared viewing graphic PI images, a new study finding. Graphic images on cigarette packaging are used in public health messaging as a way to change behaviour33. Patients’ prior experience with this approach in the community or just their fear of medical images might explain our findings, and is a timely reminder for clinicians using visual PIP education resources33. Deliberate, sensitive and quality patient education relies on establishing relationships based on mutual trust2,24,27 from which fear and other barriers can be identified and alleviated.
PIP education is an important component of the international PIP clinical practice guidelines1,7, yet access to quality patient PIP education resources was a limitation reported by nurses in our study. Barakat-Johnson et al.29 reported nurses who experienced limited access to PIP resources reported “a sense of powerlessness to provide quality care” (p. 98), as delivering quality PIP education relies on the availability of well-designed, quality and appropriate resources11,24. An Australian study of publicly available patient PIP education material on 212 Victorian health service (public, private and independent) websites found only 34.5% had patient information available27. It appears the scarcity of quality patient PIP information and education is widespread. Hence, increasing access to well-developed and patient-centred PIP education material is urgently needed.
PIP patient education resources need to be accessible, engaging, non-threatening and mutually beneficial, with patients and nurses using the resources independently and together11,26,27. Several authors have reported improvements in patient PI knowledge and care participation following engagement with an education intervention26,34. The nurses in this study overwhelmingly agreed the PPIPCB was a feasible and acceptable education resource for use in their wards because of the multiple education strategies (video, brochure, poster), which increased independent and mutual learning. The availability of multi-lingual patient PIP information is found to be lacking27, with only four education resources published on Victorian hospital websites, hence the multi-lingual availability of the PPIPCB in this study increased its accessibility. Nurse participants reported unwell, cognitively impaired and patients with reduced hearing and vision were less likely to access the PPIPCB, confirming previous research29. Using a solution-based approach, nurses indicated family members and carers could engage with the PPIPCB and encourage patients to participate in their PIP care. We know that patient PIP education facilitates patient participation2, and can contribute to reducing HAPI12, yet there are significant gaps in the availability of suitable PIP education resources for both patients and nurses, an area requiring prompt attention.
Limitations
We acknowledge the following limitations. This descriptive study was conducted on medical wards at a single study site, limiting the generalisability of the findings. Our nurse sample was mainly female, meaning the perceptions of male nurses is under-represented. Focus group participants do not have equal speaking time so, to obtain a range of views, the researcher encouraged quieter participants to contribute. To ensure participants’ own views were expressed, the researcher advised all opinions were valued.
Implications for future research
The study PPIPCB facilitates nurse and patient education. More research is needed to understand patients’ PI knowledge and awareness on admission, whilst the best time to educate patients’ needs further exploring. With greater access to mobile phones, further research is encouraged into patients’ and nurses’ acceptability and impact of technologies such as web applications (apps), in offering multiple learning opportunities to access PIP education over the course of their hospital stay.
Conclusions
Patients and nurses had different experiences of patient PIP education. Participants reported the PPIPCB was a valuable resource that simplifies complex health PI information. For patients, the PPIPCB provided flexible and individualised information. For nurses, the PPIPCB aided in their delivery of PIP patient education and outlined easy to implement strategies. Finally, it was agreed the PPIPCB could facilitate increased PI awareness and prevention for use by nurses, patients, families and carers.
Acknowledgements
We acknowledge, appreciate and thank the study participants for their valuable contribution. Study concept and design: SL, BG, WC. Data acquisition: SL. Manuscript drafting: SL, JD. Data analysis, interpretation and critical manuscript revisions: SL, JD, BG, WC.
Conflict of interest
The authors declare no conflicts of interest.
Ethics statement
Not applicable.
Funding
A 2018 Sigma Theta Tau International grant supported this study. The funders were not involved in the research.
Author(s)
Sharon L Latimer* PhD, MAP, MN,
Grad Dip L&T, BN, RN, Senior Research Fellowa,b,c
School of Nursing and Midwifery, Griffith University,
University Drive, Logan Campus, Meadowbrook, QLD, Australia
Email s.latimer@griffith.edu.au
Jodie L Deakin GCEF, BN, RN
Clinical Nurse Researchera,b
Wendy P Chaboyer PhD, ACCCN
FAAN, Director of Wiser Wounds Carea,c,d
Brigid M Gillespie PhD, RN
FACORN, Professor of Patient Safetya,b,c,d
aSchool of Nursing and Midwifery,
Griffith University, Gold Coast, Australia
bNursing Research, Clinical Governance, Education and Research, Gold Coast Hospital and Health Service, Southport, QLD, Australia
cMenzies Health Institute, QLD, Australia
dNHMRC Centre of Research Excellence in Wiser Wounds Care, Southport, QLD, Australia
* Corresponding author
References
- European Pressure Ulcer Advisory Panel (EPUAP), National Pressure Injury Advisory Panel (NPIAP), and Pan Pacific Pressure Injury Alliance (PPPIA). Prevention and treatment of pressure ulcers/injuries: clinical practice guideline. In: Hasler E, editor. The international guideline. EPUAP/NPIAP/PPPIA; 2019. p. 1–408.
- Latimer S, Chaboyer W, Gillespie BM. Patient participation in pressure injury prevention: giving patients a voice. Scand J Caring Sci 2014;28(4):648–56.
- Padula W, Delarmente B. The national cost of hospital-acquired pressure injuries in the United States. Int Wound J 2019;16(3):634–640.
- Li Z, et al. Global prevalence and incidence of pressure injuries in hospitalised adult patients: a systematic review and meta-analysis. Int J Nurs Stud 2020;105.
- Guest JF, et al. Health economic burden that wounds impose on the National Health Service in the UK. BMJ Open 2015;5(12):1–8.
- Nguyen K, Chaboyer W, Whitty J. Pressure injury in Australian public hospitals: a cost-of-illness study. Aust Health Rev 2015;39(3):329–336.
- Gillespie BM, et al. The quality and clinical applicability of recommendations in pressure injury guidelines: a systematic review of clinical practice guidelines. Int J Nurs Stud 2020;103857.
- Latimer S, Chaboyer W, Gillespie BM. Pressure injury prevention strategies in acute medical inpatients: an observational study. Contemp Nurse 2016;52(2–3):326–340.
- Gillespie BM, et al. Repositioning for pressure injury prevention in adults (review). Cochrane Database System Rev 2020;(6):1465–1858.
- Lavallée J, et al. The effects of care bundles on patient outcomes: a systematic review and meta-analysis. Implement Sci 2017;12(1):1–13.
- Gillespie BM, et al. Development and pilot testing of a patient-participatory pressure ulcer prevention care bundle. J Nurs Care Qual 2014;29(1):74–82.
- Chaboyer W, et al. The effect of a patient centred care bundle intervention on pressure ulcer incidence (INTACT): a cluster randomised trial. Int J Nurs Stud 2016;64:63–71.
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19(6):349–357.
- Deakin J, Gillespie BM, Chaboyer W, Nieuwenhoven P, Latimer S. An education intervention care bundle to improve hospitalised patients’ pressure injury prevention knowledge: a before and after study. Wound Pract Res 2020;28(4):154–162.
- Marshall M. Sampling for qualitative research. Family Practice 1996;13(6):522–526.
- Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today 2004;24(2):105–112.
- Cane J, O’Connor D, Michie S. Validation of the Theoretical Domains Framework for use in behaviour change and implementation research. Implement Sci 2012;7(1):37–53.
- Fusch PI, Ness LR. Are we there yet? Data saturation in qualitative research. Qualitative Rep 2015;20(9):1408–1416.
- Burmeister E, Aitken LM. Sample size: how many is enough? Aust Crit Care 2012;25(4):271–274.
- IBM Corporation. IBM SPSS Statistics for Windows 26.0. Armonk, New York; 2019.
- Gibbs G. Analysing qualitative data. London, UK: SAGE; 2007.
- Lincoln Y, Guba E. Naturalistic inquiry. California, USA: Sage Publications; 1985.
- McInnes E, et al. The role of patients in pressure injury prevention: a survey of acute care patients. BMC Nurs 2014;13(1):1–8.
- Durrant LA, et al. Health literacy in pressure injury: findings from a mixed-methods study of community-based patients and carers. Nursing & Health Sci 2019;21(1):37–43.
- Lawrence P, Fulbrook P, Miles S. A survey of Australian nurses’ knowledge of pressure injury/pressure ulcer management. J WOCN 2015;42(5):450–460.
- Schoeps LN, Tallberg AB, Gunningberg L. Patients’ knowledge of and participation in preventing pressure ulcers: an intervention study. Int Wound J 2017;14(2):344–348.
- Team V, et al. Patient education materials on pressure injury prevention in hospitals and health services in Victoria, Australia: availability and content analysis. Int Wound J 2020;17(2):370–379.
- MacPhee M, Dahinten VS, Havaei F. The impact of heavy perceived nurse workloads on patient and nurse outcomes. Administrat Sci 2017;7(1):1–17.
- Barakat-Johnson M, et al. A qualitative study of the thoughts and experiences of hospital nurses providing pressure injury prevention and management. Collegian 2019;26(1):95–102.
- Visser E, et al. Patients’ experiences and wellbeing after injury: a focus group study. PLoS One 2021;16(1):1469–1480.
- Aydin C, et al. Modeling hospital-acquired pressure ulcer prevalence on medical-surgical units: nurse workload, expertise, and clinical processes of care. Health Serv Res 2015;50(2):351–373.
- Chaboyer W, et al. Transforming care strategies and nursing-sensitive patient outcomes. J Adv Nurs 2010;66(5):1111–1119.
- Hammond D. Health warning messages on tobacco products: a review. Tobacco Control 2011;20(5):327–337.
- Deakin J, et al. An education intervention care bundle to improve hospitalised patients’ pressure injury prevention knowledge: a before and after study. Wound Practice & Res 2020;28(4):154–162.



