Volume 30 Number 1
Discoloured nails
Kurt Gebauer and Keryln Carville
Keywords nail disease, melanoma, fungal infection
For referencing Gebauer K and Carville K. Discoloured nails. Wound Practice and Research 2022; 30(1):50-54.
DOI
https://doi.org/10.33235/wpr.30.1.50-54
Submitted 8 March 2022
Accepted 13 March 2022
Abstract
The nails, in combination with skin, glands and hair, comprise the integumentary system. Abnormalities in the colour, shape and clinical appearance of nails can be indicative of pathophysiological disorders, habit-tics such as bitten nails, poor grooming, nutritional deficits and cosmetic practices. Discolouration and changes in nail appearance are common reasons for referral of individuals to dermatologists. This paper presents a mélange of common nail disorders with a clinical focus on those that present with discolouration.
Introduction
The nails, in combination with skin, glands and hair, comprise the integumentary system. Nails are located on the distal dorsal phalanges of the fingers and metatarsals of the toes; their prime function is to protect the digits and, in the case of fingernails, act as useful ‘tools’ for precise picking, scratching and grasping dexterity. Fingernails begin to form at 10 weeks and toenails at 12 weeks’ gestation, and they are derived from a hardened, transparent stratum corneum of the epidermis. The anatomical nail structure is classified as the nail root, body and free edge1.
Nails are composed of hardened keratin which is generated in the germinal matrix (nail root) which lies under the proximal nail fold. At the distal edge of the matrix is the visible lunula or white ‘moon’. The matrix and lunula are responsible for growth of the nail. The lunula appears white as the epidermis below is thicker in the matrix and this inhibits the pink refection from blood vessels in the nail bed below. Furthermore, the viable cells within the lunula are still undergoing keratinisation. Nails appear pink in Caucasians and tinted bluish in dark skinned individuals. As nail cells move from the matrix over the vascular nail bed they form the nail plate or hard keratin structure which is divided into the nail body and free edge2.
The nail body (corpus unguis) is the attached, translucent portion of nail that extends from the lunula to the free edge. The free edge extends from the nail body beyond the finger tip and is attached to the nail bed by the hyponychium. The length of the free edge is related to cosmetic preference and local wear forces applied during activities of daily living. The eponychium (cuticle) covers the matrix and protects against invasion of organisms. The proximal nail fold is the thickened skin at the base of the nails and the lateral nail fold is a similar fold of skin at the lateral edges3.
Fingernails grow at approximately 1.5mm per week in children under the ages 10–144 and 1mm per week in adults1, but the growth of toenails is slower. Any abnormality in colour and appearance of nails can be indicative of pathophysiological disorders, habitual behaviours such as picking or biting nails, poor grooming, nutritional deficits or use of nail cosmetics. This paper focuses on conditions associated with discoloured nails.
Diagnostic investigations
There are many reasons for discoloured nails; those outlined in this paper will be discussed under infection, trauma, pathological conditions and atypical aetiologies. Diagnostic investigations for confirmation of nail infection involves microscopy and culture of skin swabs, sub-nail tissue scrapings and nail clippings. In addition, mycology for diagnosis of moulds and fungi may be required. Biopsy and histopathological investigations of the nail plate requires specialised skill and frequently leads to significant discomfort and potential for scarring. Therefore, a clinical diagnosis is more pragmatic and is based on the individual’s relevant clinical history and examination of the nails and the surrounding skin.
Infections
Fungal infections
Onychomycoses is a fungal infection of the nail caused by dermatophyte or non-dermatophyte organisms that can result in discolouration and separation of the nail from the nail bed5. Between 18–40% of all nail disorders that result in discolouration are due to onychomycoses of the nail6,7. Nail infections contribute to 30% of all dermatomycoses which are fungal infections of the hair, nail and skin6,7. Nail plate invasion by fungal organisms usually follows penetration of hyphae (fungal filaments) along the distal and lateral border on the under-surface of the nail plate, which is the main route of nail invasion by dermatophytes. Penetration may also originate from the proximal nail fold (Figure 1).

Figure 1. Onycholysis and destroyed distal nail plate as a result of chronic dermatomycosis. Dermatophyte identified on culture as T. rubrum
Tinea unguium is most commonly caused by Trichophyton rubrum; less frequently Trichophyton interdigitale or Epidermophyton floccosum are found to be problematic. T. rubrum is only found on humans and is particularly prevalent in damp environments and in the presence of recurrent nail trauma5.
Onychomycosis is diagnosed with microscopy and culture of nail clippings and the crumbly material under the nail. Nail specimen collection is a skilled art and collection of appropriate specimens is dependant on the skill of pathology collection staff. Not infrequently patients report they are requested to take their own samples, which increases the risk of inaccurate diagnoses. The treatment gold standard for onychomycosis is oral antifungal therapy such as 3 months of terbinafine 250mg daily. Itraconazole 50mg or 100mg may be effective as a pulse therapy for 1 week every month8,9. This cycle is repeated three times for toenails and twice for fingernails and patients need to be advised that the antifungal agents will be imbedded in the nail. By the end of the treatment course there should be evidence of new nail regrowth, although it will take over 6–9 months to replace the damaged nails. It is always worthwhile advising patients that re-infection is likely. The cure rate falls dramatically in those over 60 years old or when associated with comorbidities such as diabetes and vascular disease5–7.
Mould infections
The most common mould is Candida. There are two main forms of nail infection; one is acute paronychia and the other is onychomycosis. Candida paronychia is found in wet, damp environments, for example those experienced by underground miners with hot, wet, sweaty feet. Fingernail involvement is most frequently found in those who have their hands occupationally wet, e.g. nurses, cooks, hairdressers, barmaids. Occasionally cultures will show both a dermatophyte and a mould infection. Itraconazole, as previously discussed, is the treatment of choice, although it is not on the PBS8. However, mould infections found in those with comorbidities, such as diabetes, or the very elderly, are far less likely to respond to oral therapy. Furthermore, both fungal and mould infections do not always respond to topical treatments or laser therapy5–8.
Bacterial infections
A characteristic green discolouration of the nails is seen with heavy colonisation of Pseudomonas aeruginosa. This follows either primary or secondary onycholysis, with the nail colour presenting as dark to light shade of green (Figure 2). Onycholysis can be superimposed with a Pseudomonas infection5,9. Again, excessive immersion of nails in water or exposure to dampness seems to be a significant inducing co-factor for infected toenails9. With regard to treatment, compounded thymol 4% in chloroform is effective. The use of supermarket vinegar may be considered and applied as a douche using a disposable syringe. This treatment option is readily available, cheap and extremely simple.
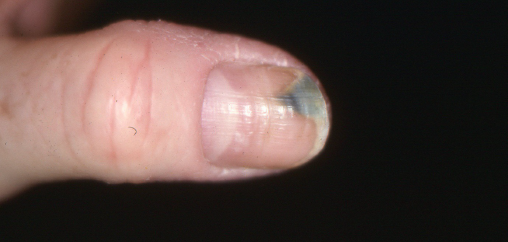
Figure 2. Onycholysis with secondary Pseudomonas infection. Dry dermatitis on the medial aspect of the thumb, ridging along the thumbnail itself, and loss of proximal nail fold
Paronychia
Paronychia is defined as infection or inflammation of the proximal or lateral nail folds, and may be classified as acute or chronic10. Acute paronychia is usually caused by invasion of pathogens such as Staphylococcus aureus11, whereas chronic paronychia is found in patients who have repeatedly traumatised their hands and nails due to frequent and extended immersion of hands in water (Figure 3)10,11. Chronic paronychia may be due to bacterial infection such S. aureus or P. aeruginosa (which may lead to a blue/green discolouration of the nail) or chronic mycotic or yeast infection11,12. If attempts to keep the skin clean and dry are not effective then topical treatment with the compounded vinegar and thymol 4% may prove effective for mycotic or yeast infection.

Figure 3. Chronic paronychia with hyperpigmentation of the lateral nail and loss of proximal nail fold due to excessive water contact
Trauma
Haematoma
Nail pigmentation due to haematoma may also be described as talon noir, a benign trauma-induced darkening or calcified haematoma or petechiae, and is the commonest injury inflicted on the nail13,14. Frequently the bleeding under the nail plate is not immediately apparent and causes the patient significant anxiety and concern when it presents at a later date. It is sometimes possible to show the patient that the blood is attached to the nail plate and not to the nail bed. This makes for a definitive diagnosis of a melanocytic lesion as compared to haematoma. Alternatively, a punch biopsy of the nail plate can differentiate these lesions. A small section of the nail plate is collected and if pigmentation caused by coagulated blood is found to be attached to the nail plate with a clear visible nail bed underlying, this is indicative of haematoma14,15.
Habit-tic dystrophy
Habit-tic dystrophy is caused by habitual external trauma such as scratching or picking. It is frequently related to obsessive–compulsive behaviours16. The damage is usually inflicted on the thumb nail by one of the fingers of the same hand, which leads to characteristic depressions and transverse or parallel ridging across the nail (Figure 4). In severe cases, the cuticles may be eroded and the lunula can hypertrophy. Interestingly, most individuals don’t realise they are doing it and getting patients to acknowledge and overcoming their habit is challenging16.

Figure 4. Characteristic nail dystrophy caused by habitual picking and scratching along the nail
Pathophysiological conditions
Malignant melanoma
A melanoma is a malignant lesion arising from melanocytes, the cutaneous pigment producing cells17. Although extremely rare, malignant melanoma of the nail plate is a subtype of cutaneous melanoma, and originates in the nail matrix melanocytes18. It is not reported to be related to sun exposure and can present as partial to total nail pigmentation and periungual pigmentation17,18. However, 25% of melanomas in these areas are amelanotic and can present as pyogenic granuloma, granulation tissue, ingrown nail and micro-bacterial infection with nail dystrophy18. Subungual melanoma is more common in African-American, Asian and Hispanic populations, males in their 70s and females in their 60s, and is more predominate on the thumb, hallux and index finger19,20. An ABCDEF mnemonic devise by Levit et al.21 assists in diagnosing subungual melanoma and outlines:
A: Age (50–70 years old); African, Japanese, Chinese and Native American ethnicity.
B: Brown-black pigmented band ≥3mm with blurred borders.
C: Change despite treatment.
D: Digits most commonly involved are thumb, index finger or hallux.
E: Extension of pigment into the skin surrounding the nail (Hutchinson sign).
F: Family or personal history of melanoma or atypical nevus.
Unfortunately, melanoma of the nail often goes undiagnosed or is misdiagnosed; this may explain why the Jamaican reggae musician Bob Marley succumbed to a toenail plate melanoma22. However, an early diagnosis and treatment can significantly improve the prognosis20.
Psoriasis
Psoriasis is a very common cutaneous disease; it can affect the nails and may clinically indicate underlying joint inflammation, that is, psoriatic arthritis11. Few patients are asymptomatic and the range of presentations is extremely varied (Figures 6 and 7). Some individuals may have no observable psoriasis on full skin examination other than a little bit of scale and flake behind the ears or a touch of hyperkeratosis on the elbows and knees. Those with a history of skin psoriasis or examination findings of psoriasis on the skin make for easier diagnosis of nail disease, although nail clippings and histopathological examination can provide a definitive diagnosis. Psoriasis can affect nails in many different ways, predominantly with pitting, thickening, crumbling, leukonychia (white discolouration), red spots in the lunula and onycholysis11. Pitting suggests nail matrix disease. Onycholysis can occur due to nail bed disease and the use of potent topical steroid or vitamin D analogues as a fluid/gel manually rubbed into the affected area may be the treatment of choice. However, when faced with multiple affected nails or significant destruction, then systemic therapy is the treatment of choice11,13,15.

Figure 5. Pitting of the nail as found in psoriasis. The keratinocytes that are being laid down into the proximal nail plate under the nail fold do not adhere and elements of the nail fall apart; this is highly suggestive of underlying joint disease

Figure 6. Severe psoriasis; it is always worthwhile doing skin scrapings and clippings to eliminate superimposed Candida or other moulds

Figure 7. Nail dystrophy caused by chronic atopic dermatitis. There is some chronic paronychia with boggy periungual swelling on the index finger. There is pterygium formation on the second finger, namely the long ridge with a distal split; this is where there has been fracture to the nail plate. A break to the actual nail bed is usually post-trauma. Such findings can also occur in lichen planus which is characteristic of atopic dermatitis
Atopic dermatitis
Atopic dermatitis is a common skin disorder characterised by chronic inflammation, sensitive dry skin, localised or disseminated eczematous lesions, itching and epidermal-barrier dysfunction23. Chronic or acute dermatitis can affect the nails in many different ways (Figure 7). Most commonly there is destruction of the proximal nail fold. However, atopic dermatitis may cause nail pitting, trachyonychia (rough, longitudinally ridged nails), Beau’s lines (transverse grooves), onychomadesis (separation of the nail plate from the nail matrix) and onychoschizia (brittle, split, soft or thin nails)24. A definitive diagnosis is made on examination of the hands for signs of weeping, vesicular or lichenified skin and signs of scratching. Nail changes resolve once the dermatitis is controlled with perhaps the exception of nail fold covers14,15.
Myxoid cysts
Myxoid cysts are benign pseudocysts and are also known as synovial cysts, periungual ganglia and joint tendon sheath cysts25. They present as soft or firm nodules on the distal intra-phalangeal joint or proximal nail fold of the fingers in middle aged or elderly individuals, particularly women. They usually measure <10mm and contain transparent or yellow coloured jelly-like fluid which is comprised of hyaluronic acid, globulin, glucosamine and albumin25,26. These cysts are considered to be due to osteoarthritis arising in the underlying joint cavity. If the cyst causes pressure on the nail bed if can affect nail growth with subsequent dystrophy26 (Figure 8). Treatments involve needling of the cyst and, although some recommend cryosurgery as a therapy, it is not particularly effective, nor are intralesional steroid injections25,26. A referral to a hand surgeon may be warranted if the patient is distressed by the cosmetic appearance.

Figure 8. Myxoid cyst denting the nail due to pressure on the proximal nail fold; visible soft tissue swelling in the tissue just proximal to the nail plate
Atypical aetiologies
Longitudinal melanonychia
These lesions are a tan, brown or black longitudinal streaks within the nail plate11. They are caused by increased melanin deposition in the nail itself which arises from either greater melanin synthesis by normally non-functional matrix melanocytes or from an increase in the total number of matrix melanocytes that synthesise melanin27. The lesions originate most often because melanocytes have become more active rather than increased density of pigment cells27,28. Individuals presenting with longitudinal melanonychia are relatively common and those from Africa, Central and East Asia by far outnumber Caucasians with this presentation. The lesions are found more commonly in dark skinned individuals; 77% of African–Americans over the age of 20 years have one finger affected and generally 100% in those over 50 years of age, and 10–20% of Japanese people are affected29.
The gold standard diagnostic investigation for longitudinal melanonychia is a nail biopsy, which can be difficult and one not without risk of morbidity. Patients are frequently left with permanent nail bed damage and persistently dystrophic nails; postoperative bacterial wound infection is not infrequent. The pathology report can be entirely normal as we are frequently looking at increased activity of melanocytes and not an increased number28. In practice, when patients present with an already established nail pigmented streak that has been present for some years and unchanged in appearance, it is likely to be benign rather than malignant. However, it is always worthwhile to emphasise that lesions can change and any substantial change in the index lesion requires review. When a lesion has been present for a few weeks or months and there is a suggestion that it is still evolving, it is advisable to photographically record the nail image and review the patient in 3 months. Surgical biopsy is offered and the ensuing discussion regarding the pros and cons of observation verses biopsy should be recorded in the patient’s records.
Conclusion
Nail abnormalities have more than cosmetic impacts. The appearance of nails can be indicative of pathophysiological disorders, habit-tics, poor grooming, nutritional deficits and cosmetic practices. Discolouration of nails in particular is frequently related to infection, trauma, pathological disorders or habit-tics. Awareness of common nail abnormalities such as discolouration and the potential aetiologies can lead to early diagnosis and targeted treatment.
Conflict of interest
The authors declare no conflicts of interest.
Ethics statement
No ethical approval was required.
Funding
The authors received no funding for this study.
Author(s)
Kurt Gebauer1* and Keryln Carville
1Clinical Assoc. Professor of Dermatology, University of Western Australia & Fremantle Dermatology, WA, Australia
2Silver Chain Group & Curtin University, WA, Australia
*Corresponding author Email kurt@fremantledermatology.com.au
References
- Van De Graaff K, Fox SI. Concepts of human anatomy and physiology. New York, NY: McGraw Hill; 1995.
- Mattson Porth C. Essentials of pathophysiology. 4th ed. Philadelphia (PA) Wolters Kluwer; 2015.
- De Berker D. Nail anatomy. Clin Derm 2013;31:509–515.
- Starace M, Alessandrini A, Piraccini BM. Nail disorders in children. Skin Appendage Disord 2018;4:217–229.
- Elewski B. Onychomycosis: pathogenesis, diagnosis, and management. Clin Microb Rev 1998;11(3):415–429.
- Achten G, Wanet-Rouard J. Onychomycoses in the laboratory. Mykosen Suppl 1978;1:125–7. PMID: 162561.
- Baran R, Hay R, Haneke E, Tosti A. Onychomycosis – the current approach to diagnosis and therapy . London: Martin Dunitz; 1999.
- Australian Medicines Handbook. Australian Medicines Handbook 2022. Adelaide: Australian Medicine Handbook Pty Ltd; 2022. Available from: https://amhonline.amh.net.au/auth
- Kreijkamp-Kaspers S, Hawke K, Guo L, Kerin G, Bell-Syer SE, Magin P et al. Oral antifungal medication for toenail onychomycosis. Cochrane Database Syst Rev 2017;(7): CD010031.
- Reineck J, Hinshaw M. Nail health in women. Intern J Women’s Derm 2020;6:73–79.
- Lee D, Lipner S. Optimal diagnosis and management of common nail disorders. Annals of Med 2022;54(1):694–712.
- Bauer MF, Cohen BA. The role of Pseudomonas aeruginosa in infection about the nails. Arch Derm 1957;75(3):394–396.
- Baron R, de Berker D, Holzberg M, Piraccine BM, Richert B, Thomas L. (Eds.). Baran and Dawber’s diseases of the nails and their management (5th ed.). Hoboken, NJ: Wiley-Blackwell; 2019.
- Baran R, Barth J, Dawber R. Nail disorders: common presenting signs, differential diagnosis and treatment. London: Churchill Livingstone; 1991.
- Zaias N. The nail in health and disease. 2nd ed. Norwalk, CT: Appleton and Lange; 1990.
- Perrin A, Lam J. Habit-tic deformity. Canadian Med Assoc J 2014;186(5):371.
- Davisa L, Shalinb S, Tacketta A. Current state of melanoma diagnosis and treatment. Cancer Bio Ther 2019;20(11):1366–1376.
- Banfield CC, Dawber RP. Nail melanoma: a review of the literature with recommendations to improve patient management. British J Derm 1999;141:628–632.
- Boespflug A, Debarbieux S, Depaepe L, et al. Association of subungual melanoma and subungual squamous cell carcinoma: a case series. J Am Acad Dermatol 2018;78(4):760–768.
- Bristow I, de Berker D, Acland K, et al. Clinical guidelines for the recognition of melanoma of the foot and nail unit. J Foot Ankle Res 2010;3(25). doi:10.1186/1757-1146-3-25.
- Levit E, Kagen M, Scher R, Grossman M, Altman E. The ABC rule for clinical detection of subungual melanoma. J Am Acad Dermatol 2000;42(2 Pt.1):269–74.
- Kyriakou G, Kyriakou A, Papanikolaou S, Glentis A. Don’t worry about a thing… every little thing gonna be all right (except for acral lentiginous melanoma). Clin Derm 2020;5(19). doi:10.1016/j.clindermatol.2020.11.011
- Bieber T. Atopic dermatitis: an expanding therapeutic pipeline for a complex disease. Nat Rev Drug Discov 2022;21:21–40.
- Chung BW, Choi YW, Park CW. Nail dystrophy in patients with atopic dermatitis and its association with disease severity. Ann Derm 2019;31(2):121–126.
- Jabbour S, Kechichian E, Haber R, Tomb R, Nasr M. Management of digital mucous cysts: a systematic review and treatment algorithm. Int J Dermatol 2017;56(7):701–708.
- Fan Z, Chang L, Su X, Yang B, Zhu Z. Treatment of mucous cyst of the distal interphalangeal joint with osteophyte excision and joint debridement. Frontier Surg 2022;8: doi:10.3389/fsurg.2021.767098
- Jefferson J, Rich P. Melanonychia. Dermatol Res Pract 2012;952186. doi:10.1155/2012/952186
- Haneke E, Baran R. Longitudinal melanonychia. Derma Surg 2001;27:580–584.
- Cao Y, Han D. Longitudinal melanonychia: how to distinguish a malignant condition from a benign one. Clin J Plastic Recon Surg 2021;3(1):56–62.



