Volume 30 Number 2
How generalist nurses inform their clinical decision-making in wound management: a scoping review
Adeline S Vains and Kathleen Finlayson
Keywords wound, nurse, evidence, decision-making
For referencing Vains AS and Finlayson K. How generalist nurses inform their clinical decision-making in wound management: a scoping review. Wound Practice and Research 2022; 30(2):112-118.
DOI
https://doi.org/10.33235/wpr.30.2.112-118
Submitted 22 October 2021
Accepted 8 November 2021
Abstract
Background Wound care forms a significant component of nurses’ roles across acute, long-term, community and primary healthcare settings. This scoping review aimed to examine and analyse key concepts and factors that inform nurses’ decision-making and the use of evidence-based practice (EBP) in wound management.
Methods A literature scoping review was undertaken, searching original research articles from academic databases and grey literature. Papers were screened for relevant topics and inclusion criteria included wounds, decision-making and nursing. The quality of evidence was evaluated using a validated quality assessment tool. Thematic analysis was used to analyse results through dominant and meaningful themes.
Results A total of 14 relevant peer-reviewed articles were identified. Five decision-making contributors were identified: patient factors – patient factors, education and information, expert opinion, peer guidance, and economics and logistics. These results identify evidence gaps to inform future research opportunities on nurses’ decision-making in wound management.
Conclusion The review identified factors nurses use in decision-making in wound care. Recommendations include the need for high-quality research on the area, the uptake of standardised wound assessment, improved pathways for collaboration with experts in the field, and increased training for nurses on evidence appraisal to address economic burden and optimising patient outcomes.
Introduction
Wound care is a complex, important and costly aspect of nursing that requires timely management for positive outcomes for both clinician and patient1,2. Chronic wounds in Australia affect approximately 400,000 people, are seen to cost more than A$3.5 billion or 2% of national health expenditure, and have significant impacts on health-related quality of life (HRQOL)3. Despite this, nurses spend a large portion of their day managing wounds, with an estimation of 27–50% of hospital nurses’ workload used to manage wounds4.
Nurses play a key role in wound management through their level of knowledge that informs assessment and treatment5,6. Nurses must undertake comprehensive, individualised assessment of the person and their wound to inform decisions on wound management and treatments as appropriate for each patient7. Nurses’ autonomy in practice has increased through professional accreditation and they are required to justify individualised treatment decisions that consider national and international evidence-based practice (EBP) guidelines for optimal patient outcomes8.
Sources cite a gap between implementation of research to practice, with an average of 17 years between established evidence and incorporation into practice9. Australian data suggests a lack of education in EBP wound care amongst student and registered nurses (RNs) accounting for a lack in skills, confidence, knowledge and uptake of EBP10. This scoping review aimed to examine and analyse key concepts to identify the factors that informs nurses’ decision-making and use of EBP in wound care, and identify contributing or hindering factors to EBP in wound management.
Methods
Search strategy
This descriptive scoping review is reported using the PRISMA-ScR guidelines for scoping review methodologies and scoping review checklist11; for further details see Appendix 1 (PRISMA-ScR checklist). Academic databases searched were Cochrane Library, CINAHL, MEDLINE, Joanna Briggs Institute, Scopus and PubMed. Grey literature was searched in the National Health and Medical Research Council (NHMRC), Wounds Australia, the Association for the Advancement of Wound Care (AAWC), the Tissue Viability Society, Wounds International, and the Wound, Ostomy and Continence Nurses Society sites.
Key search terms were: nurse, evidence, evidence-based practice, education, guidelines, research, knowledge, wound, ulcer, skin integrity management, care, treatment, healing, practice using the following Boolean terms (PubMed: 19 March 2020):
Search (((Nurs*[Text Word]) AND (Evidence[Title] OR “evidence-based practice”[Title] OR educat*[Title] OR guide*[Title] OR “scientific base”[Title] OR quality[Title] OR knowledge[Title] OR research[Title] OR “knowledge source”[Title])) AND (wound*[Title] OR “skin integrity”[Title])) AND (management[Title] OR care[Title] OR treatment”[Title] OR healing[Title] OR practice[Title]) Filters: Full text; English
Selection criteria
Studies were identified through a systematic database search conducted between 17–31 March 2020 to identify relevant papers based on inclusion and exclusion criteria12. Inclusion criteria were:
- Papers reporting contributing factors to nurses’ clinical decision-making in wound care.
- Papers reporting on all areas of nursing including but not limited to acute, medical, surgical, outpatients and community.
- Full text published in English.
- Published from January 2010 – March 2020.
- Studies were not limited by design and included qualitative and quantitative research.
Exclusion criteria were studies that did not meet inclusion criteria, studies that reported on clinical nurse specialists, and studies that did not identify contributing factors to decisions in wound management among nurses.
Data extraction
Screening was conducted within DistillerSR systematic review software which was used for removing duplicates, validation and the creation of a PRISMA flow diagram13. Literature was first screened by the first author and title, and progressed to abstract, then full text screening if inclusion criteria was met. Papers that met eligibility criteria were then comprehensively reviewed and relevant data extracted using a custom excel spreadsheet to include objectives, method, context and findings14,15. The quality appraisal checklist from Methods for the development of NICE public health guidance was used to appraise the quality of the literature16.
Data analysis
Thematic analysis was used to interpret results due to the mixture in methodologies17. The process began during the extraction phase and was reviewed and refined using an iterative approach. Overlapping themes of results and conclusions were identified in each study, looking for repeated, insightful or meaningful findings.
Results
The initial database search resulted in 701 articles relevant for screening. No relevant studies were identified in the grey literature. After excluding duplicates and irrelevant articles, 14 eligible articles remained (Figure 1)6,18–30. Following screening, secondary sources identified a relevant article which was not identified in the original search as the MESH term “ulcer” was not used in the strategy. Therefore, a decision to run a new search with the term “ulcer” through PubMed, which yielded the largest results, was conducted to check accuracy of search results. No new articles were identified; therefore, due to the low probability of identifying other relevant articles, a new search through all platforms was not conducted.
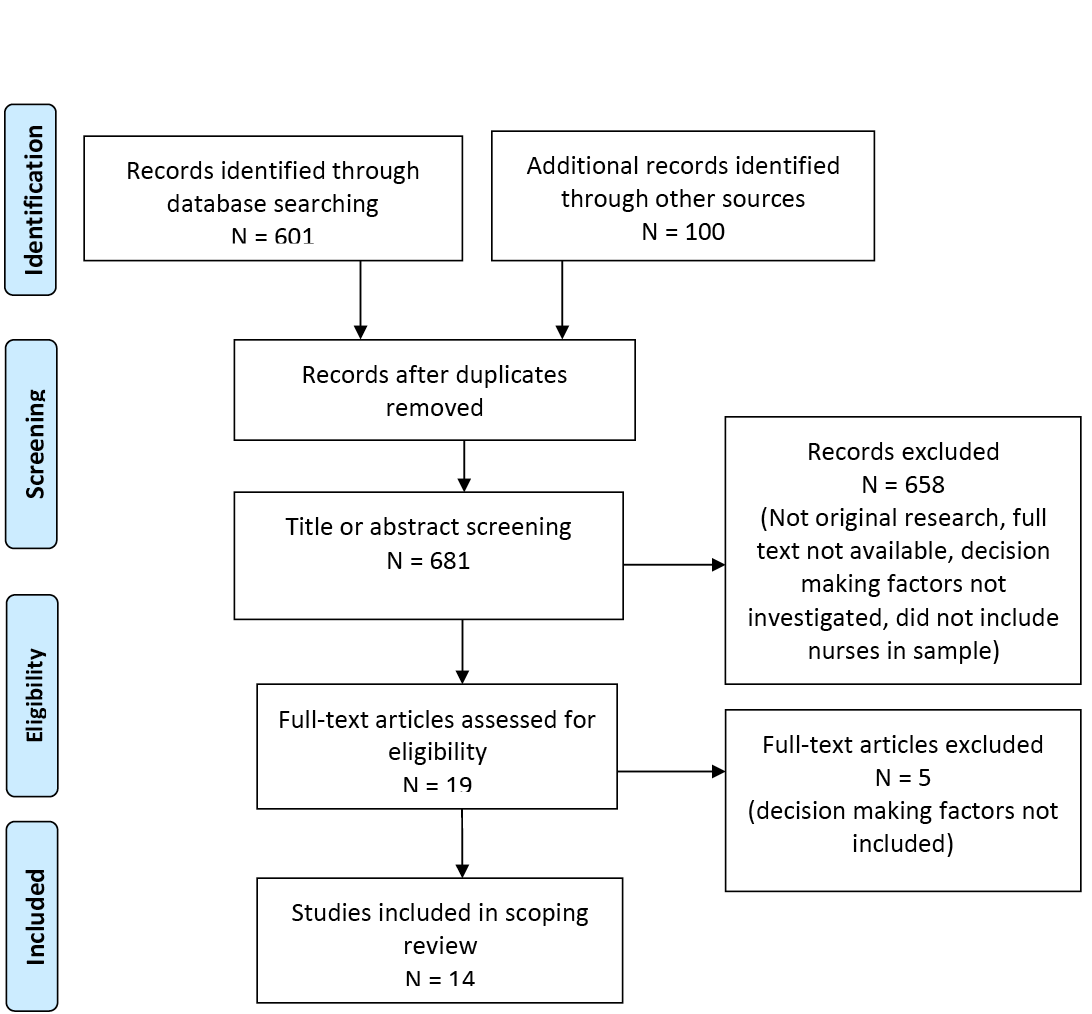
Figure 1. Flow diagram for the scoping review process
Study characteristics
Of the 14 articles relevant for this scoping review, the majority were quantitative designs (n=11) and the remaining used qualitative designs (n=3), with studies undertaken across six different countries. Three studies were based in Australia, three in Sweden, five in the United Kingdom, and one each from Denmark, Brazil and the United States. All studies met the inclusion criteria; however, results varied in relevance depending on the aim of the study.
Of the quantitative studies, nine studies used a cross-sectional descriptive design and two used a quasi-experimental design. The smallest sample was 31 participants18 and the largest 1,717 participants19. Most of these studies had either small samples between 26–50 participants (four studies), or moderate samples between 101–150 participants (five studies). Of the qualitative studies, two used content analysis whilst one used grounded theory; the sample sizes varied between eight, 16 and 20 participants20–22.
The most common sample settings for all studies were in hospitals (n=5), followed by community/general practice/outpatient clinics (n=4), residential aged care facilities (n=2) and a mixture of hospital and community (n=2); the least common was a wound conference (n=1). An intervention was used in three out of the 14 studies, such as an educational event or champion intervention. The majority of wound types described in the studies were a mixture of acute and chronic wounds (n=10), followed by acute (n=2) and chronic wounds (n=2). Data were collected either by questionnaire or survey (n=11) or interviews (n=3).
Quality assessment
From the 14 articles in the literature search, ten articles were identified as medium-grade evidence and four were identified as low-grade evidence when using a modified mixed-method quality appraisal checklist16 (Figure 2). The external validity assessment was based on the study sample, including size, generalisability and relevance, whilst the internal validity was based on clear reporting and choice of methodology or potential bias16.
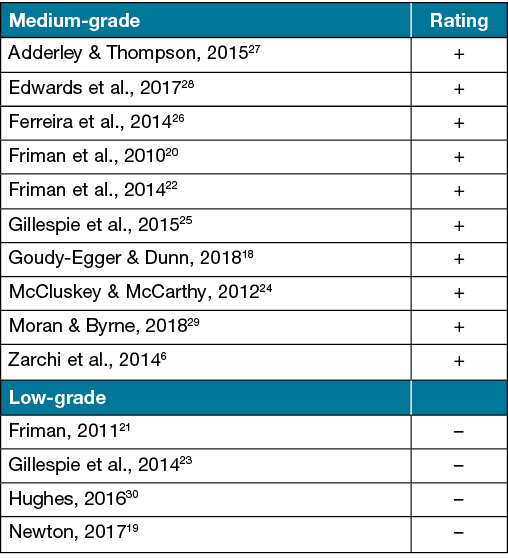
Figure 2. Quality assessment
Factors influencing nurses’ decision-making in wound management
Results from the 14 studies were read, coded and grouped based on the main decision-making influencers. Five primary themes were identified regarding the factors influencing nurses’ decision-making in wound management – patient factors, education and information, expert opinion, peer guidance, and economics and logistics.
Patient factors explored patient preference and the influence of individualised wound assessments. Education and information identified the sources and preferences nurses have in where to obtain information for decisions. Expert opinion highlighted the role of the multidisciplinary team and seeking advice. Peer guidance highlighted the use of input from nursing peers. Economics and logistics considered the cost of products, the frequency of dressing changes and product availability that influenced decision-making in wound management.
Patient factors
Patient factors such as the results of wound assessment or patient preference were used to inform decisions in seven of the 14 articles. This included findings from assessment of wounds, pain, aetiology, infection, exudate, general patient condition, or patient goals and preference. Two quantitative studies of low- to medium-quality found 76–90% of participants used wound assessment to guide decisions23,24, while two low- to medium-grade qualitative studies identified continuous and consistent wound assessment as important21,25. However, the accuracy or the quality of these assessments was also questioned. The literature varied in the conclusions of the quality of wound assessment from nurses but suggested there is room for improvement23,26. Although it was recognised wound management has improved since the introduction of EBP22,24, it was identified there was often a misuse of assessment, such as priority given to one aspect of wound assessment and less recognition to other important aspects such as medical history, leg ulcer pain, type or appearance27.
Assessment of pain levels was included in three studies as a decision-making factor, either to guide the aim to reduce pain during dressing changes or as an indicator of the significance of wound deterioration or infection presence. In two studies, 79–96% of participants considered pain reduction during dressing changes19,24. However, in a medium-grade cross-sectional study, only 8% of nurses thought preventing pain was an important consideration in wound management27. Only one study considered the patient’s overall condition to be an important component of assessment to support wound management decisions. This was reported by 57% of participants in a low-grade cross-sectional study23.
Wound aetiology was considered by 19–48% of nurses in decision-making in two studies19,27. The low numbers may be explained by findings from one qualitative study that highlighted nurses may lack an understanding of the importance of wound aetiology and the impact it has on wound healing, particularly when decisions are made when aetiology is unknown20.
Other less used patient considerations included presence of wound infection (14–27%)19,27 and patient gender (7%)27. Assessing exudate levels was considered by 5% and 7% of participants in two studies19,27, whilst 74% of participants in a large, low-grade cross-sectional study used the identified volume of exudate to guide decisions of ongoing management19. It was identified in the qualitative evidence that delegation of wound care to care workers in the community reduces the opportunity for accurate or timely wound assessments and appropriate escalation, and may result in poorer patient outcomes21.
Consideration of patient preference was an important factor for 48% of nurses as identified in a cross-sectional study and was also considered a challenge to EBP in wound management when patient wants or needs compete with best practice guidelines19. One qualitative study saw consideration of patient goals to be important25, whilst a medium-level quantitative study contrasted this by finding only 8% of participants considered patient goals in decisions of management27.
One study used judgement analysis of the motivators of decision-making where the competency of nurses’ decision-making in complex wounds was challenged. The study identified that “memory shortcuts” were used as a way to decipher and guide clinical pathways rather than through critical thinking or in-depth understanding27; however, these shortcuts may not be sufficient in decision-making given the complexity of skills and knowledge required in wound management. A reliance on other pieces of information or practice may occur, such as ritualistic wound practice based on familiar products, or acquiring skill through practical experience rather than EBP27. This process of decision-making was not identified in any other articles; however, this was the only study to use judgement analysis to interpret findings.
Education and information
The scoping review identified that education played an important role in guiding decisions, and the challenges in accessing ongoing professional development to support EBP in wound care practice may negatively impact decision-making. Previous wound management education was identified as a decision-making influencer by five medium-quality studies, including two qualitative studies, one quasi-experimental and two cross-sectional studies6,18,20,24,26. Three medium-quality studies identified 22%, 23% and 64% of participants made decisions based on conference or lecture information18,24,26. Analysis of data from a medium-quality cross-sectional study identified that nurse participants had “some kind” of unidentified training in wound care20 and another study found that attendance in educational wound programmes was an important predictor in the use of EBP in wound care decisions6. One study26 also identified a university extension course was utilised by 29% of participants in decision-making. Informal education such as study groups was used by 14% (n=8) and 24% (n=35) of participants24,26 and independent informal reading by 20% (n=11) of participants26.
Independently searching a variety of information sources to inform decisions on wound care such as libraries, guidelines or databases was also identified as a source of information to guide decisions. The use and awareness of local, national or international EBP guidelines varied greatly amongst studies. Only 5–10% of 145 participants in a medium-grade study used this; however, the study sample was narrow and only included one hospital for recruitment, indicating this may not be a generalisable result24. More consistently, 58–70% of participants in low to medium-grade studies reported using EBP guidelines to inform decisions18,23. Three studies, including one qualitative study and two cross-sectional studies, highlighted confusion regarding awareness, availability or absence of appropriate guidelines6,20,26, whilst one survey identified the potential need for deviation from clinical guidelines such as environmental, patient preference or availability of equipment/wound products as a barrier to EBP due to wound or patient complexities27.
In a cross-sectional study, 23–25% of 120 participants used information from professional wound care associations, whilst also highlighting access to this information can be challenging due to membership fees, therefore a potential barrier to its use23. In a small quasi-experimental study, textbooks were used by 42% of participants, while 52% used journals or databases. Further evidence on database use was identified in qualitative research22 and by 26–40% of participants23,26. The use of hospital libraries was used by 19% of participants (n=23)23. Through training in computer and literature searching skills, a pre/post study saw improved EBP uptake amongst nurses in residential aged care facilities28.
Two qualitative studies identified that nurses were more likely to independently seek information from sources when dealing with a slow healing or complex wound22, whilst the importance of using the best available information such as hospital policies or national guidelines were also considered important decision-making influencers25. One cross-sectional study saw a small number of general nurses (17%) had a special interest in wounds and saw themselves as experts; however, it is not identified if this opinion is supported by evidence24. The use of grey literature such as Google searches or newspapers were used by 13–28% of participants23,26. Only 11% used a local resource such as a ward folder24.
Holistic care of the whole patient rather than the wound only was identified as an important belief25. Up-to-date practice and continuity of care were important factors in wound management decision-making through a core foundational theme of “balancing evidence-based knowledge with evidence-based practice”25. Interesting findings from another study was that nurses’ wound knowledge was measured as higher when working closely with a certified wound nurse through knowledge sharing and was a significant predictor in wound management skills6. Furthermore, four studies found that wound assessment and management skills were higher in nurses that rate themselves highly in competence level, rather than years of experience, resulting in higher capabilities6,21,24,29. This highlights the value of opening up self-reflective discussions to identify those who may need increased educational opportunities.
Accessing education opportunities to support knowledge and decision-making in wound management was a repeated challenge identified by seven studies; this was compounded by a lack of support from management or the organisation8,18,19,22,28–30. Organisation culture was used to explain an unwillingness to support professional development due to the cost of attending courses, or inability to support non-clinical time for independent research due to workloads, therefore negatively impacting on the quality of decisions made in wound care6,21–23,25,28,29.
Expert opinion
The importance of a team approach in wound management, including collaboration, advice, opinion or referral to an expert in wound management, was considered an important decision-making factor, particularly in complex or non-healing wounds. Qualitative evidence identified multidisciplinary allied health involvement was sought out by nurses to support decision-making in complex wounds, such as physiotherapists to support pain management, dietitians to assess nutritional impact on wound healing, diabetic educators for diabetes control or occupational therapists to support compression application in complex chronic ulcers or pressure injury prevention20,21,25. Additionally, advice from medical practitioners was identified. Recommendations or treatment preference from the surgeon was identified in one mid-level study to guide 37% of participants’ decisions23, whilst 31% used physician recommendations26, 22% used hospital consultants, and 8% used registrars or senior house officers24. Two qualitative studies found nurses seeking advice from dermatologists, vascular surgeons and GPs when treating difficult wounds20,21; however, it was highlighted that GPs were not always considered wound experts but part of the necessary referral pathway to accessing specialist medical advice20.
One survey identified 86% (n=124) of participants believed clinical nurse specialists to be an expert source in wound management decisions24, and three cross-sectional studies identified participants would use the advice of wound nurse specialists 42%, 75% and 83% of the time18,23,29. Two qualitative studies did note difficult access to wound specialists as a potential barrier in seeking this advice21,25. One quasi-experimental study saw improved information sharing of EBP following the implementation of a skin integrity “champion” or promotor28.
Information from wound companies was also a contributing factor in decision-making. One cross-sectional study saw 19% of participants using advice from brand representatives23, whilst two qualitative studies found nurses would use familiar or well represented brands rather than objective wound assessments in decisions22,25. Nurses also recognised the potential bias from brand representatives when making clinical decisions22.
Although the significance and value of a team approach was frequently mentioned in these articles, limited access to or availability of expert advice such as wound specialist nurses due to conflicting schedules, or navigating through a complex referral process for specialist reviews such as dermatology, found use of this advice was dependent upon the service model rather than the clinical need itself20,21,23,25,26. These findings highlight the recognition that a cohesive and efficient pathway to access medical, wound nurse or allied health advice must be established to optimise patient outcomes and improve efficiency for nurses’ workloads.
Peer guidance
The studies in this review identified decisions in wound care were also guided by advice from peers such as nursing colleagues. Two surveys found 46–83% considered nursing colleagues as expert wound sources24,26. Qualitative study findings noted information and knowledge exchange amongst nursing colleagues to be important in both individual and team learning22, whilst another study found this method is commonly used due to its convenience and quick response compared to other available resources25. It was not clear if this advice from colleagues is underpinned by evidence or other factors, such as gut decision-making25 and ritualistic practice, rather than holistic assessments or evidence as drivers of decision-making30.
Economics and logistics
The final driver of decision-making in wound care was cost and logistics of available wound treatments. Two surveys saw 6% (n=7) to 67% (n=1150) of participants consider opportunities for cost reduction through dressing choice; however, one study was a narrow sample from one hospital and the other a sample of wound conference attendees with varying education levels, including students and care workers, contributing to the large variance of results19,23. Qualitative evidence supported the consideration of dressing cost; however, this was amongst a sample including multidisciplinary team participants25. Around three-quarters (78%) of participants in a large survey felt they could reduce costs to patients or organisations by reducing the frequency of dressing changes without negatively impacting on patient outcomes; however, only 6% of these participants considered the frequency of dressing changes required as a means to reduce cost19.
Only a small number of participants (7%, n=8) in a cross-sectional study considered time constraints in wound care decisions23. Despite this low number, seven of the 14 studies, including three qualitative and four quantitative studies, considered time constraints and staffing levels as a barrier to the implementation of EBP when making decisions in wound management19,21–23,25,28,29. Other identified barriers to EBP decisions saw limited product availability by 43%23 or, in contrast, the idea of an oversaturation of wound products on the market that makes decisions on appropriate EBP in dressings more difficult due to overwhelming options25.
Discussion
The results of this review identify there is insufficient quality evidence to perform a systematic review to answer the research question. However, this scoping review identified five primary factors influencing nurses’ wound care decision-making – patient factors, education and information, expert opinion, peer guidance, and economics and logistics.
The evidence identified accurate wound assessments are pivotal in the recognition of problems in the wound healing process and can lead to poor outcomes if assessments are not accurate or carried out regularly by an experienced clinician8. The results of this review identified a gap in the use of standardised assessments to guide decision-making, particularly when looking at the low numbers of articles that included wound aetiology, patient goals or patient condition, although these factors are considered part of adequate wound assessment8. Overall, there is evidence of poor standardisation of wound assessment that does not meet international and national evidence-based assessment guidelines31,32.
Another frequently found predictor of decision-making was advice or support from another health professional. There is strong evidence on the value of a team approach to wound care to improve patient outcomes, particularly in complex or non-healing wounds such as diabetic or pressure ulcers33. While the evidence suggests this is one of the more frequently used decision-making factors, it is unclear from the evidence whether seeking answers from other health professionals is over- or under-used in the studies reviewed.
Formal education was also identified as a preferred decision-making contributor. Whilst supporting access to this on an organisational level is important, what may be equally important is teaching nurses how to independently search and interpret quality evidence, rather than relying upon access to formal educational seminars24.
Cost was also a key contributor to nurses’ decision-making in wound care, both of dressing products and consideration of the cost of nurses’ time. Although the evidence suggests nurses aim to reduce the burden of cost to patients and the healthcare system by selecting less expensive products, international studies have found the cost of nursing time to be the greatest cost portion in wound management34. Instead, evidence suggests there is a significant opportunity to reduce cost through improving EBP in wound care, which sees improved quality of life and outcomes through faster wound healing times, ultimately reducing the nursing time required35,36.
Limitations
Due to the nature and scope of this review there are some limitations. Firstly, a single reviewer (first author) screened all articles for inclusion. The absence of a second researcher may have resulted in transcription errors during data charting, despite all results being checked twice for errors. Reviewing and analysing both qualitative and quantitative data together may have decreased the quality of results; however, this is the nature of a scoping review. Another challenge was seen in interpreting results with mixed disciplines in the sample population, although the review was aimed at nurses. The use of thematic analysis to review both qualitative and quantitative data is also a potential limitation as this framework is more often utilised to interpret qualitative research and can be considered inconsistent or incohesive17,37.
Recommendations
The scoping review highlights there is insufficient high-quality evidence to complete a systematic review to answer the research question. It is a recommendation from this project that more studies of high-quality are required, particularly those with a large nursing population across a variety of sites who manage a larger variety of wounds. Additional qualitative research may add value in understanding the reasons decision are made without supporting evidence. Until a larger body of high-quality evidence is established and reviewed critically, it is suggested that regular updates in current wound assessment and management occur for nurses who are involved in wound care through an accredited organisation, regardless of mode (such as conference, guidelines review, webinar or online modules). It is recommended that EBP in wound management is included as a core component of undergraduate education for nurses. Registered nurses are also encouraged to seek education on how to independently source and appraise information to facilitate EBP. Additionally, there must be consideration at a national and policy level to the barriers that effect EBP teams’ approach to wound management, whether within metropolitan or rural healthcare. A focus on more streamlined access, referrals and communication from other experts in skin integrity and wounds is required for utilisation of team-based wound management.
Ethics statement
Ethics approval was not required for this study.
Conflict of interest
There were no conflicts of interest from the authors and no ethics approval required for the literature review.
Funding
There was no funding contribution to declare.
Appendix 1
Click here to download the appendix
Author(s)
Adeline S Vains1* and Kathleen Finlayson2
1Queensland University of Technology, Kelvin Grove, QLD, Australia
2Faculty of Health, Centre for Healthcare Transformation, Queensland University of Technology, Kelvin Grove, QLD, Australia
*Corresponding author Email adelinevains@hotmail.com
References
- Dowsett C. T.I.M.E. to improve patient outcomes: use of a clinical decision support tool to optimise wound care. Br J Comm Nurs 2019;24(S3):S6-S11.
- Lumbers M. Understanding and addressing dryness during wound healing. Br J Comm Nurs 2019;24(6S):11–14.
- Pacella R, et al. Solutions to the chronic wounds problem in Australia: a call to action. AusHSI; 2018. http://www.aushsi.org.au/wp-content/uploads/2018/2018-Recommendations-Paper_Chronic-Wounds-Solutions.pdf
- Posnett J, et al. The resource impact of wounds on healthcare providers in Europe. J Wound Care 2009;18(4):154.
- Annesley S. Current thinking on caring for patients with a wound: a practical approach. Br J Nurs 2019;28:290–294.
- Zarchi K, et al. Significant differences in nurses’ knowledge of basic wound management: implications for treatment. Acta Derm Venereol 2014;94:405–407.
- Brolmann F, et al. Evidence-based decisions for local and systemic wound care. Br J Surg 2012;99:1172–1183.
- Madden M, Stark J. Understanding the development of advanced wound care in the UK: interdisciplinary perspectives on care, cure and innovation. J Tissue Viability 2019;28:107–114.
- McKinney I, Dellostritto R, Branham S. Nurses’ use of evidence-based practice at point of care: a literature review. Crit Care Nurs Q 2019;42:256–264.
- Pacella R. Issues paper: chronic wounds in Australia. 2017.
- Moher D, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015;349:1–9.
- Patino C, Ferreira J. Inclusion and exclusion criteria in research studies: definitions and why they matter. J Bras Pneumol 2018;44:84.
- Joanna Briggs Institute. The Joanna Briggs Institute reviewers’ manual 2015: methodology for JBI Scoping Reviews. Joanna Briggs Institute; 2015.
- Colquhoun HL, et al. Scoping review: time for clarity in definition, methods, and reporting. J Clin Epidemiol 2014;67:1291–1294.
- Grant M, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Hlth Info Lib J 2009;26:91–108.
- National Institute for Health and Care Excellence. Methods for the development of NICE public health guidance. National Institute for Health and Care Excellence; 2012. Available at: https://www.nice.org.uk/process/pmg4/resources/methods-for-the-development-of-nice-public-health-guidance-third-edition-pdf-2001967445701
- Clarke V, Braun V. Thematic analysis. J Posit Psycho 2017;12:297–298.
- Goudy-Egger L, Dunn K. Use of continuing education to increase nurses’ knowledge of chronic care management. J Cont Ed Nurs 2018;49:454–459.
- Newton H. Cost-effective wound management: a survey of 1717 nurses. Br J Nurs 2017;26:S44-S49.
- Friman A, Klang B, Ebbeskog B. Wound care in primary health care: district nurses’ needs for co-operation and well-functioning organization. J Interprof Care 2010;24:90–99.
- Friman A, Klang B, Ebbeskog B. Wound care by district nurses at primary healthcare centres: a challenging task without authority or resources. Scan J Caring Sci 2011;25:426–434.
- Friman A, et al. District nurses’ knowledge development in wound management: ongoing learning without organizational support. Prim Health Care Res Dev 2014;15:386–395.
- Gillespie BM, et al. Wound care practices: a survey of acute care nurses. J Clin Nurs 2014;23(17–18):2618–2626.
- McCluskey P, McCarthy G. Nurses’ knowledge and competence in wound management. Wounds UK 2012;8:37–47.
- Gillespie BM, et al. Health professionals’ decision-making in wound management: a grounded theory. J Adv Nurs 2015;71(6):1238–1248.
- Ferreira A, et al. Knowledge and practice of nurses about care for patients with wounds. J Res Fund Care 2014;6:1178–1190.
- Adderley U, Thompson C. Community nurses’ judgement for the management of venous leg ulceration: a judgement analysis. Int J Nurs Studies 2015;52:345–354.
- Edwards HE, et al. Reduced prevalence and severity of wounds following implementation of the Champions for Skin Integrity model to facilitate uptake of evidence-based practice in aged care. J Clin Nurs 2017;26(23–24):4276–4285.
- Moran N, Byrne G. Assessing knowledge of wound care among cardiothoracic nurses. Br J Nurs 2018;27:S33-S42.
- Hughes M. Wound infection: a knowledge deficit that needs addressing. Br J Nurs 2016;25:S46-S51.
- National Institute for Health and Care Excellence. Surgical site infection: prevention and treatment of surgical site infection. NICE; 2019.
- Wounds Australia. Standards for wound prevention and management. 3rd ed. Osborne Park, WA: Cambridge Media; 2016.
- Moore Z, et al. Managing wounds as a team. J Wound Care 2014;23:S1-S38.
- Whitlock E, et al. Wound care costs in general practice: a cross-sectional study. Aust Fam Physician 2014;43:143–146.
- Atkin L, Schofield A, Kilroy-Findley A. Updated leg ulcer pathway: improving healing times and reducing costs. Br J Nurs 2019;28:S21-S26.
- Gray T, et al. Opportunities for better value wound care: a multiservice, cross-sectional survey of complex wounds and their care in a UK community population. BMJ 2018;8:1–9.
- Nowell L, et al. Thematic analysis: striving to meet the trustworthiness criteria. Int J Qual Methods 2017;16:1–13.



