Volume 30 Number 2
Risk factors for delayed healing or non-healing of venous leg ulcers in adults: a systematic review protocol
Christina N Parker, Sandra Johnston, Ut Bui, Erica O’Donoghue, Bec Fletcher and Kathleen Finlayson
Keywords systematic review, venous leg ulcers, risk factors, delayed healing, non-healing
For referencing Parker CN et al. Risk factors for delayed healing or non-healing of venous leg ulcers in adults: a systematic review protocol. Wound Practice and Research 2022; 30(2):119-122.
DOI
https://doi.org/10.33235/wpr.30.2.119-122
Submitted 18 November 2021
Accepted 4 February 2021
Abstract
Background Chronic leg ulcers affect 1–3% of the population and are costly to treat and health service resource intensive. Venous aetiology contributes to about 70% of all chronic leg ulcers; these ulcers are often associated with prolonged ill health, pain and decreased physical functioning, and have a substantial impact on health-related quality of life.
Aim The primary aim of this systematic review is to identify literature on the risk factors for delayed healing or non-healing of venous leg ulcers (VLUs) in adults.
Methods This systematic review will be guided by the Preferred Reporting Items for Systematic review and Meta-Analysis Protocols (PRISMA-P) 2015 statement. Studies will be identified from PubMed, ScienceDirect, Web of Science, ProQuest, CINAHL Complete, MEDLINE, APA PsychINFO, Academic Search Elite, Cochrane Library, JBI EPD (evidence-based practice database), ProQuest (Dissertations and Theses Global) and Global ETD (electronic theses and dissertations) Search Engine up to August 2021. Methodological quality will be assessed using the Mixed Methods Appraisal Tool (MMAT) 2018. A narrative synthesis of risk factors will be categorised as physiological (general/medical), clinical, demographics or psychosocial.
Introduction
Leg ulcers are known to be slow to heal and cause prolonged ill health, affecting up to 3% of adults1, increasing in prevalence with age2,3, and often lasting for many years2,4. Leg ulcers occur in the lower legs with the commonest underlying aetiologies of venous insufficiency, arterial insufficiency or a combination of both. Of all chronic leg ulcers, venous leg ulcers (VLUs) have the highest prevalence5, with venous aetiology often classified using the Clinical-Etiological-Anatomical-Pathophysicological (CEAP) international scale for classifying the clinical presentation, primary cause of venous disease, anatomical location of the affected veins and type of disease6. VLUs are classified under this system as C5 (evidence of a healed VLU) or C6 (active VLU)6.
There are more than 47,200 cases of people with active VLUs receiving care in Australian hospitals (2010–2011)7. There were 1,730 cases of people with VLUs in residential aged care facilities in 2012, and it has been noted that A$803 million is being spent to manage/treat VLUs7. A VLU is defined as an open wound between the knee and ankle joint that occurs as a result of venous disease8. Despite evidence-based care, only about 70% of VLUs will heal within a 24-week period9,10; in addition, reported costs often do not include the indirect costs to people with VLUs, with these high costs noted to be a barrier to implementation of evidence-based wound care11,12.
These ulcers can be debilitating, having a major impact on a person’s life, often with disease distress symptoms including pain, decreased physical functioning, immobility, sleep disturbance, lack of energy, limitations in leisure activities, worries and frustrations, lack of self-esteem and a substantial negative impact on health-related quality of life13.
Many published studies report risk factors for delayed/non-healing of VLUs14–19; however, to date, there have been no systematic reviews that we could find and only limited reviews of risk factors20–23, particularly those that include non-physiological factors, due to a range of definitions, methodological inconsistencies in data collection, and measurement of risk factors20. Previously reported studies have consistently concluded risk factors as being a larger ulcer area, a longer ulcer duration, a previous history of ulceration, venous abnormalities and a lack of high compression20. Other potential risk factors include decreased mobility and/or ankle range of movement, poor nutrition and increased age20.
While a number of evidence-based guidelines exist for the management of VLUs24–28, with current strategies including addressing patient-related factors (pain, education, psychosocial support, elevation of lower limb, exercise, and nutrition and hydration), preparing the leg and the wound (cleansing, controlling venous eczema and maintaining skin integrity), and graduated compression therapy, evidence supporting further risk factors would be of benefit in the management of VLUs and will potentially add to existing literature in management guidelines.
Aim
This systematic review will investigate risk factors for delayed or non-healing VLUs. These factors can then be considered when caring for someone with a VLU in clinical practice and research. A preliminary search was undertaken in the PROSPERO International prospective register of systematic reviews. There were no systematic reviews found on the risk factors associated with healing of VLUs; hence the importance for this systematic review to be completed.
Methods
This review protocol is guided by the PRISMA-P (Preferred Reporting Items for Systematic review and Meta-Analysis Protocols) 2015 statement29; the completed PRISMA-P 2015 checklist is shown Supplement 1.
Protocol and registration
This systematic review has been registered with the PROSPERO International prospective register of systematic reviews (CRD42021279789).
Search strategy
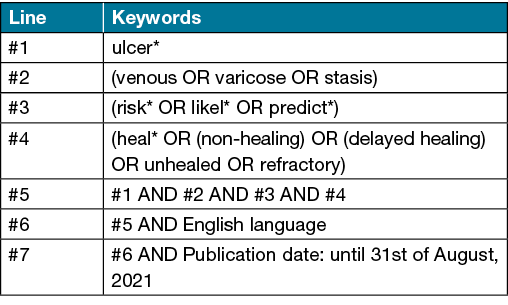
Articles will be screened to determine eligibility against the inclusion criteria. Articles that are deemed eligible for inclusion will have their reference lists searched following the same search strategy. The search strategy will be used to locate articles using the following keywords – (venous OR varicose OR stasis) AND ulcer AND (risk OR likelihood OR predict) AND (heal OR non-healing OR delayed healing OR unhealed OR refractory). The search criteria will include human studies from any country, in English language and available in full text. For example, Table 1 shows the search strategy for PubMed.
Table 1. Example search strategy from PubMed
Information sources
The search will be undertaken in the databases of PubMed, ScienceDirect, Web of Science, ProQuest, CINAHL Complete, MEDLINE, APA PsychINFO, Academic Search Elite, Cochrane Library, JBI EPD (evidence-based practice database), ProQuest (Dissertations and Theses Global) and Global ETD (electronic theses and dissertations) Search Engine. There will be no limitations on the publication starting dates; the publication dates will be limited up to 31 August 2021 with a further search run prior to finalisation of the study.
Types of studies
The type of studies will include qualitative, quantitative and mixed-methods research such as observational, longitudinal, cohort, case control, randomised controlled trials, non-randomised controlled trials, descriptive studies, systematic reviews, meta-analysis, theses or dissertations. All case studies, case reports, case series, clinical guidelines, literature reviews, general reviews, opinion papers or news items will be excluded.
Inclusion criteria
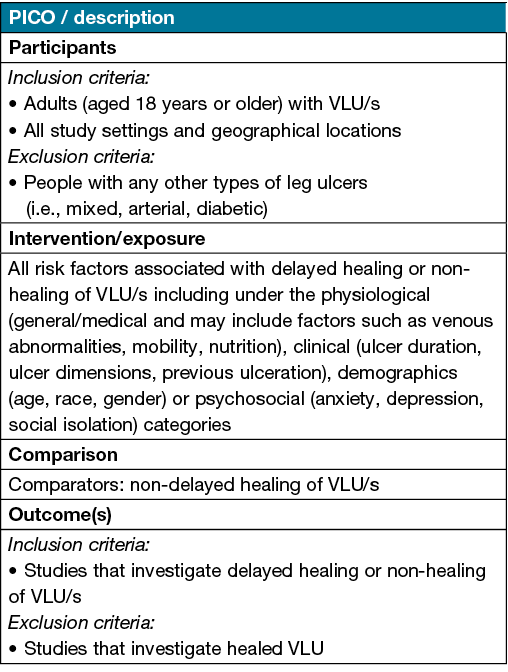
Table 2 shows the inclusion criteria which follows the aspects of the PICO mnemonic.
Table 2. PICO criteria
Outcomes
The primary outcome of the review is to identify, describe and analyse the risk factors for delayed healing or non-healing in comparison to non-delayed healing of VLUs in adults. The risk factors will be measured by key variables, the effects on healing, and level of risk as determined by significance of outcomes.
Currently there is a lack of consensus on the definitions of delayed healing and non-healing in VLUs with no agreed definition. Definitions have generally included that the wound does not proceed toward healing in a defined time period or in a timely manner30,31, hence delayed healing and non-healing in this study will be defined as a VLU that has not followed a normal healing trajectory. Non-delayed healing will be defined as a VLU/s that has healed (100% epithelialisation).
Study selection
The search results will be imported into EndNote and all studies (excluding duplicates) will be transferred to Rayyan for blinded screening. All steps involved in study selection will be presented in a PRISMA flow diagram.
Screening of titles and abstracts will be undertaken followed by screening of full text articles. Two independent reviewers will assess titles and abstracts of retrieved articles for inclusion criteria. Articles retrieved in this first step will then be assessed for full text inclusion. Two reviewers will independently assess to exclude any articles that do not meet inclusion criteria. Any disagreements in these phases will be resolved by a third independent reviewer.
Assessment of methodological quality
All eligible studies will be critically appraised by at least two reviewers using the Mixed Methods Appraisal Tool (MMAT) 201832. A third independent reviewer will resolve any disagreements in the final appraisal. All quality assessment results will be presented for each study and/or outlined in the synthesis of findings.
Data extraction
Data from included studies will be extracted into an Excel spreadsheet. One reviewer will undertake data extraction and complete the excel file, with a second reviewer checking the file. A third independent reviewer will resolve any disagreements. Any missing data will be documented, with the third reviewer to decide if any additional information should be requested to the corresponding author of the relevant study.
The study data to be extracted will include information such as authors, year, title, country, aim/objectives, study type, methodology context, setting, timeframe, sample size, demographics, ulcer characteristics, strengths and limitations. The outcomes data to be extracted will include information such as specific variables with significance of effect on healing/level of risk, variables assessed, statistical analysis and any assessment tools used or definitions.
Data synthesis
The study characteristics and descriptive findings will be presented in a tabular format. If an adequate number of similar studies/variables are found using similar methods and outcome measures of delayed healing or non-healing, a meta-analysis will be undertaken of risk factors for delayed healing and/or non-healing utilising RevMan. However, if there is heterogeneity of study methods and outcomes, results of this review will be presented as a narrative synthesis. Any qualitative studies will be reported separately. The critical appraisal categories, criteria and quality assessment result will be outlined for each study. Study data and outcomes data will be used to address the research question. Key variables, effects on healing and level of risk will be presented as the risk factors associated with delayed healing or non-healing in comparison against non-delayed healing of VLUs.
Statistical analysis of subgroups (i.e., physical and/or psychosocial) will not be undertaken. A narrative summary of any relevant subgroups may be presented such as between variables and the level of risk on delayed healing and/or non-healing.
The systematic review will be a descriptive synthesis of risk factors associated with delayed healing or non-healing of VLUs in adults.
Conclusion
Evidence supporting risk factors would be of great benefit to clinicians in the management of VLUs and could be of value in existing management guidelines.
Acknowledgements
We would like to acknowledge the support of Queensland University of Technology (QUT) as this study has been undertaken within the School of Nursing, Faculty of Health at QUT.
Author contribution
CP and KF wrote the funding grant. All authors contributed to conceptualisation and methodology. All authors will contribute to screening, critical appraisal, data extraction and data synthesis, and all authors will be responsible for manuscript preparation, including providing feedback and critical comments on the manuscript. All authors have read and approved the final protocol manuscript.
Ethics and dissemination
As data will be sourced from publicly available materials, ethics will not be required. Findings will be disseminated through a peer-reviewed journal, conferences and social media.
Conflict of interest
The authors declare no conflicts of interest.
Funding
The authors received funding through a Queensland University of Technology (QUT) Centre for Healthcare Transformation (CHT) grant.
Appendix
Click here to download the appendix
Author(s)
Christina N Parker*1,2, Sandra Johnston1, Ut Bui1,2, Erica O’Donoghue1,2, Bec Fletcher3 and Kathleen Finlayson1,2
1Faculty of Health, School of Nursing, Queensland University of Technology, Victoria Park Road, Kelvin Grove,
QLD 4059, Australia
2Centre for Healthcare Transformation, Faculty of Health, Queensland University of Technology (QUT), Brisbane, QLD, Australia
3Ipswich Hospital, Ipswich, QLD 4305, Australia
*Corresponding author Email christina.parker@qut.edu.au
References
- Xie T, Ye J, Rerkasem K, Mani R. The venous ulcer continues to be a clinical challenge: an update. Burns Trauma 2018;6(1):18.
- Abbade LPF, Lastória S, Rollo HdA. Venous ulcer: clinical characteristics and risk factors. Int J Dermatol 2011;50(4):405–11.
- Berenguer Pérez M, López-Casanova P, Sarabia Lavín R, González de la Torre H, Verdú-Soriano J. Epidemiology of venous leg ulcers in primary health care: incidence and prevalence in a health centre. A time series study (2010–2014). Int Wound J 2019;16(1):256–65.
- Edwards H, Courtney M, Finlayson K, Shuter P, Lindsay E. A randomised controlled trial of a community nursing intervention: improved quality of life and healing for clients with chronic leg ulcers. J Clin Nurs 2009;18(11):1541–9.
- Norman RE, Gibb M, Dyer A, Prentice J, Yelland S, Cheng Q, et al. Improved wound management at lower cost: a sensible goal for Australia. Oxford, UK: Blackwell Publishing Ltd; 2016. p. 303–16.
- Haesler E. Evidence summary: venous leg ulcers: diagnostic tools for venous disease. Wound Pract Res 2018;26(4):212–4.
- Graves N, Zheng H. Modelling the direct health care costs of chronic wounds in Australia. Wound Pract Res 2014;22(1):20–33.
- Wounds Australia. Standards for Wound Prevention and Management. 3rd edition. Osborne Park, WA: Cambridge Media; 2016.
- Gohel MS, Taylor M, Earnshaw JJ, Heather BP, Poskitt KR, Whyman MR. Risk factors for delayed healing and recurrence of chronic venous leg ulcers: an analysis of 1324 legs. European J Vasc Endovasc Surg 2005;29(1):74–7.
- Guest M, Smith JJ, Sira MS, Madden P, Greenhalgh RM, Davies AH. Venous ulcer healing by four-layer compression bandaging is not influenced by the pattern of venous incompetence. Br J Surg 1999;86(11):1437–40.
- Pacella R, Tulleners R, Cheng Q, Burkett E, Edwards H, Yelland S, et al. Solutions to the chronic wounds problem in Australia: a call to action. Wound Pract Res 2018;26(2)84-98.
- Phillips CJ, Humphreys I, Thayer D, Elmessary M, Collins H, Roberts C, et al. Cost of managing patients with venous leg ulcers. Int Wound J 2020;17(4):1074–82.
- Hopman WM, Vandenkerkhof EG, Carley ME, Harrison MB. Health-related quality of life at healing in individuals with chronic venous or mixed-venous leg ulceration: a longitudinal assessment. J Adv Nurs 2016;72(11):2869–78.
- Weller CD, Bouguettaya A, Team V, Flegg J, Kasza J, Jayathilake C. Associations between patient, treatment, or wound-level factors and venous leg ulcer healing: wound characteristics are the key factors in determining healing outcomes. Wound Repair Regen 2020;28(2):211–8.
- Parker CN, Finlayson KJ, Edwards HE. Ulcer area reduction at 2 weeks predicts failure to heal by 24 weeks in the venous leg ulcers of patients living alone. J Wound Care 2016;25(11):626–34.
- Parker CN, Finlayson KJ, Edwards HE. Predicting the likelihood of delayed venous leg ulcer healing and recurrence: development and reliability testing of risk assessment tools. Ostomy Wound Manage 2017;63(19):16–33.
- Edwards HE, Parker CN, Miller C, Gibb M, Kapp S, Ogrin R, et al. Predicting delayed healing: the diagnostic accuracy of a venous leg ulcer risk assessment tool. Int Wound J 2018;15(2):258–65.
- Kumar N, Huda F, Mani R, Singla T, Kundal A, Sharma J, et al. Role of hospital anxiety and depression on the healing of chronic leg ulcer: a prospective study. Int Wound J 2020;17(6):1941–7.
- Senet P, Blas-Chatelain C, Levy P, Manea EM, Peschanski M, Mirault T, et al. Factors predictive of leg-ulcer healing in sickle cell disease: a multicentre, prospective cohort study. Br J Dermatol 2017;177(1):206–11.
- Parker CN, Finlayson KJ, Shuter P, Edwards HE. Risk factors for delayed healing in venous leg ulcers: a review of the literature. Int J Clin Pract 2015;69(9):967–77.
- Westby MJ, Dumville JC, Stubbs N, Norman G, Wong JK, Cullum N, et al. Protease activity as a prognostic factor for wound healing in venous leg ulcers. Cochrane Database System Rev 2018;9:CD012841.
- Smith D, Lane R, McGinnes R, O’Brien J, Johnston R, Bugeja L, et al. What is the effect of exercise on wound healing in patients with venous leg ulcers? A systematic review. Int Wound J 2018;15(3):441–53.
- Tang X-L, Chen H-L, Zhao F-F. Meta-analytic approaches to determine gender differences for delayed healing in venous leg ulcers. Phlebol 2016;31(10):744–52.
- European Wound Management Association, editor. Position document: understanding compression therapy. London: MEP Ltd; 2003.
- Scottish Intercollegiated Guidelines Network. Management of chronic venous leg ulcers – A national clinical guideline. Edinburgh; 2010.
- The Australian Wound Management Association Inc and the New Zealand Wound Care Society Inc, editor. Australian and New Zealand clinical practice guideline for prevention and management of venous leg ulcers. Perth, WA: Cambridge Publishing; 2011.
- Marston W, Tang J, Kirsner RS, Ennis W. Wound healing society 2015 update on guidelines for venous ulcers. Wound Repair Regen 2016;24(1):136–44.
- Evans R, Kuhnke JL, Burrows C, Kayssi A, Labreque C, O’Sullivan-Drombolis D, et al. Best practice recommendations for the prevention and management of venous leg ulcers. In: Foundations of best practice for skin and wound management a supplement of Wound Care Canada. Wounds Canada; 2019. p. 70. Available from: www.woundscanada.ca/docman/public/health-care-professional/bpr-workshop/1521-wc-bpr-prevention-and-management-of-venous-leg-ulcers-1874e-final/file.
- Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Rev 2015;4(1).
- Suthar M, Gupta S, Bukhari S, Ponemone V. Treatment of chronic non-healing ulcers using autologous platelet rich plasma: a case series. J Biomed Sci 2017;24(1):16.
- Frykberg RG, Banks J. Challenges in the treatment of chronic wounds. Adv Wound Care (New Rochelle, NY) 2015;4(9):56–582.
- Hong QN, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M, et al. Mixed Methods Appraisal Tool (MMAT). Registration of Copyright (#1148552). Canadian Intellectual Property Office, Industry Canada; Version 2018.



