Volume 30 Number 2
Portable negative pressure wound therapy (NPWT) is an effective therapy for hard-to-heal-wounds in the community: a case series
Louise Webber, Wendy Cornish, Alison Cummins and Frances Rachel Henshaw
Keywords negative pressure wound therapy, pressure injury, venous leg ulcer, community nursing, wound management
For referencing Webber L et al. Portable negative pressure wound therapy (NPWT) is an effective therapy for hard-to-heal-wounds in the community: a case series. Wound Practice and Research 2022; 30(2):108-111.
DOI
https://doi.org/10.33235/wpr.30.2.108-111
Submitted 14 November 2021
Accepted 15 December 2021
Abstract
Aims Negative pressure wound therapy (NPWT) was introduced to assist closure in hard-to-heal wounds. The benefits of NPWT include enhanced exudate management, increased blood flow to the skin, reduced interstitial oedema, stimulation of granulation tissue formation, and reduction of pro-inflammatory cytokines. NPWT has been successfully used on wounds of various aetiologies, largely in hospital settings. The aim of this case series is to explore the use of a NPWT system with a unique Hydrofiber® wound contact layer in community settings.
Methods We present three case studies where the AvelleTM NPWT System has been used to treat hard-to-heal wounds in primary care settings.
Results Complete healing was achieved in three wounds that were complex, ‘hard-to-heal’ wounds
Conclusions This NPWT system provides a feasible, effective and well-tolerated solution for the management of complex wounds in the community Clinicians reported that the Hydrofiber® wound contact layer facilitated autolytic wound debridement, was conformable to a variety of wound locations (including wounds prone to contamination due to incontinence), and provided appropriate exudate management even in limbs subject to dependent oedema.
Introduction
In the early 1990s negative pressure wound therapy (NPWT) was introduced to assist closure in hard-to-heal wounds1. NPWT has been successfully used on wounds of various aetiologies in the hospital and outpatient care settings and has been shown to be well tolerated and able to reduce time to wound healing2. Other benefits of NPWT include enhanced exudate management, increased blood flow to the skin, reduced interstitial oedema, stimulation of granulation tissue formation, and reduction of pro-inflammatory cytokines that are known to inhibit healing3.
People with chronic wounds most commonly receive wound care in the primary healthcare setting by general practitioners (GPs), community nurses and allied health professionals, as well as in community health clinics and aged care facilities4. The AvelleTM NPWT System (ConvaTec, Deeside, UK) is a disposable, portable, canister-free NPWT system that incorporates a sterile, white, fibrous dressing derived from 100% sodium carboxymethylcellulose (Hydrofiber®). The unique dressing confers the advantage of enabling autolytic wound debridement as well as protection of the peri-wound skin in addition to the other benefits of NPWT. The system is indicated for low to moderately exuding chronic and acute wounds delivering 80mmHg vacuum via a palm-sized pump, with a 30-day therapy-life. Unlike some other NPWT systems, dressings are supplied separately to the pump which minimises waste and also enables smaller dressings to be used as the wound heals. With these features in mind we present three patient cases showing the results of the AvelleTM NPWT System in a primary care clinical practice5. The AvelleTM NPWT System was supplied by ConvaTec for the purposes of product evaluation in all three cases.
Case studies
Case 1
Introduction
Mr C, a 39-year-old male, sustained a traumatic laceration to his left lower leg in a motorcycle accident. Following washout and debridement, the wound was left wound open with a plan to heal by secondary intention using ribbon gauze and combine dressings. Second daily dressings with his GP were organised and Mr C commenced oral Cephalexin for a period of 5 days for suspected wound infection.
Mr C presented to a postoperative review clinic in regional Victoria 12 days after his initial surgery. He disclosed a history of smoking, and presented with an 11cm DVT in the left leg which had been confirmed with imaging and for which he was prescribed anti-platelet therapy (Clexane).
Methods
On presentation to the wound clinic, an open wound measuring 3.5cmx1.2cm and a depth of 1cm was documented. The wound appeared to be clean with granulation tissue present. Initially the wound was dressed with gelling Hydrofiber® dressings (AQUACEL® Ag ribbon and AQUACEL® Ag surgical dressing). These dressings were replaced with a NPWT system at day 19.
Results
Figure 1 shows the wound healing journey. Note that the figure shows healing after NPWT application; day 1 is day 19 since initial presentation. On day 1 of the NPWT application, the dressing became detached, and nursing staff identified that the seal was breached due to the presence of dense hair. The hair was clipped and the NPWT was reapplied with extra securement strips.

Day 1 Day 14 Day 26
Figure 1. Case 1 shows the left lower leg wound from commencement of NPWT (day 1), to discontinuation of NPWT (day 14), to healing (day 26)
At day 14 the wound had reduced in size to a width of 1.5cm, length of 0.5cm and a depth of 0.1cm with 20% epithelial tissue and 80% granulation tissue, whereupon NPWT system was removed. Full healing was achieved by day 26 using a standard dressing.
Discussion
The patient was very impressed with the swift healing time and found the portable NPWT easy to manage even whilst working as a chef.
Case 2
Introduction
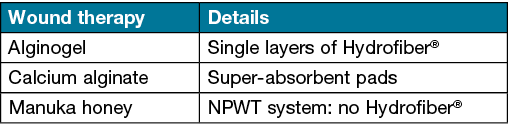
Mrs D, aged 52, presented with a venous leg ulcer measuring about 8x3cm on the right distal anterior leg which had been present for 5 years. The wound had previously been treated by wound care nurses, wound care nurse practitioners, a tertiary hospital wound clinic, community health nurses and a GP. Despite sustained efforts, the wound failed to respond to treatment regimens, including enzyme alginogels, calcium alginate with hydrocolloid particles, Manuka honey, single layers of Hydrofiber® dressing, multi-layered super-absorbent pads and a NPWT (foam interface) (Table 1).
Table 1. Wound therapies used
Several factors were identified as barriers to healing. These included type 2 diabetes, venous hypertension, recurrent infection (treated as necessary with systemic antibiotics), bilateral secondary lymphoedema related to previous excision of a malignant melanoma in 2014, as well as morbid obesity, smoking 8–10 cigarettes per day, poor nutrition and lack of motivation related to mental health issues. Mrs D also suffered from hypertension, gastro-oesophageal reflux disease (GORD), colitis, hypothyroidism, depression, chronic low back pain, neuropathic pain diffuse osteoarthritis, and had had bilateral total hip replacements in 2014.
Mrs D was frustrated at the lack of healing. She had ongoing pain issues, was unable to shower without covering the area with waterproof plastic, and was embarrassed about the wound odour. In consultation with Dr LL, a decision was taken to try the AvelleTM NPWT System with the objective of healing this stagnant wound.
Methods
In April 2020 a comprehensive management plan was instigated which included the application of topical anaesthetic (Emla cream) for pain management, sharp wound debridement using a curette, and cleansing followed by application of the AvelleTM NPWT System. Weekly dressing changes were scheduled.
The client reported that the dressing leaked three times during the trial period, for example when Mrs D fell asleep in her chair with her legs dependent, causing an unanticipated increase in wound exudate. On another occasion the system de-pressurised due to a break of the dressing seal. Increased exudate was observed on the occasions when the wound became locally or systemically infected. At these times, AQUACEL® Ag was added under the NPWT dressing.
Results
As shown in Figure 2, at 20 weeks, a wound area reduction of 40% was achieved following commencement of the new management plan which included NPWT as well as AQUACEL® Ag dressing (when clinically indicated), and AQUACEL® dressing when an anti-microbial was not indicated. NPWT was discontinued at 20 weeks and replaced with a dressing consisting of five layers of AQUACEL® Ag (cut to 1cm beyond wound margins) secured with a hydrocolloid wafer. By March 2021 the wound had reduced by 95% (Figure 2) and was completely healed by May 2021.

Week 1 Week 20 Week 48
Figure 2. Case 2 shows the wound progression of a right venous leg ulcer
In addition, improvement was observed in the peri-wound area where both erythema and dermatitis were reduced. This improvement was achieved despite the fact that, on several occasions, the client had fallen asleep with her legs dependant, increasing oedema and exudate, and had an intercurrent sub-optimal diet and blood glucose levels. The client found the system to be “comfortable, with little or no pain on removing or replacing the dressing”.
Discussion
The NPWT system, in combination with AQUACEL® Ag and ad hoc compression bandages, on the infrequent occasions when the client consented to this, provided a total wound solution to induce healing in this chronic, complex wound. The addition of NPWT conferred advantages including the capacity to increase blood supply, angiogenesis, granulation tissue formation and microbial clearance, as well as reduce oedema, all of which are known to promote wound healing.
The transition to multiple layers of AQUACEL® Ag secured with DuoDERM® was instigated after completion of the NPWT. This combination (first described in 2007 as a dressing for postoperative joint replacements and known as the Jubilee method after the hospital where it was invented6) was effective in managing exudate for prolonged periods and enabled the dressing to be left in place for up to 1 week. This Hydrofiber® and hydrocolloid combination is similar to AQUACEL® Ag surgical cover dressings (ConvaTec) which are designed to be left undisturbed over surgical sites for up to 7 days. This case study highlights the benefits of both NPWT and Hydrofiber® dressings in the management of hard-to-heal wounds and highlights the need to not give up.
Case 3
Introduction
Mr B, a 76-year-old resident in an aged care facility, had a complex medical history which included T4/5 paraplegia, an ileal conduit, chronic stage III pressure injuries on the left and right hips, Fournier’s gangrene on the right thigh with a failed skin graft followed by skin flap, psoriasis and Guillian-Barre syndrome.
He was referred to a nurse practitioner for review of the pressure injuries to both hips which had been present for approximately 12 months. Wound healing had been impeded by poor health, immobility, faecal incontinence and as well as hospital stays for infection and bowel obstruction. He required full care with ADLs, including a hoist transfer from bed to wheelchair, and enjoyed sitting outside and going out with his family on a regular basis.
Prior to the nurse practitioner review, both pressure injuries were managed with povidone iodine paste and a hydrocolloid dressing. Dressing contamination due to faecal incontinence and skin sensitivity to dressing adhesives were identified as chief barriers to wound healing.
Methods
The recommendation was for the AvelleTM NPWT System to be used on the bilateral hip wounds. However, there were challenges in retaining the dressing to the right side. This was in a location that was compromised by incontinence-associated moisture and this, in tandem with the bony architecture of the location, meant it was difficult to maintain a seal bilaterally whilst frequently repositioning the patient to prevent further pressure injures. Therefore the AvelleTM NPWT System was discontinued and, to date, this wound has remained unhealed.
Upon commencement of the AvelleTM NPWT System to the left hip pressure injury, the wound was ~0.8cms in diameter with tracking ~1.7cms (between 3–4 o’clock) and nil to low serous exudate. The wound bed had dusky granulation tissue. Wound management included gelling Hydrofiber® ribbon, loosely packed into the sinus, and the AvelleTM NPWT System. Given the history of psoriasis and sensitivity to several dressings, DuoDERM® Thin was applied to frame the wound in order to protect the skin. Initially the dressing was changed twice weekly; this was subsequently reduced to weekly.
Results
The wound healing trajectory is shown in Figure 3. Mr B was admitted to hospital for a few days with a bowel obstruction 5 weeks after commencement of the AvelleTM NPWT System therapy where the NPWT remained in situ. At day 60 post-application, the NPWT was removed – the wound sinus had healed, and the wound bed was almost at skin level. In contrast to previous dressings, no skin sensitivity was observed. The dressing was changed to an antimicrobial gel and film dressing.
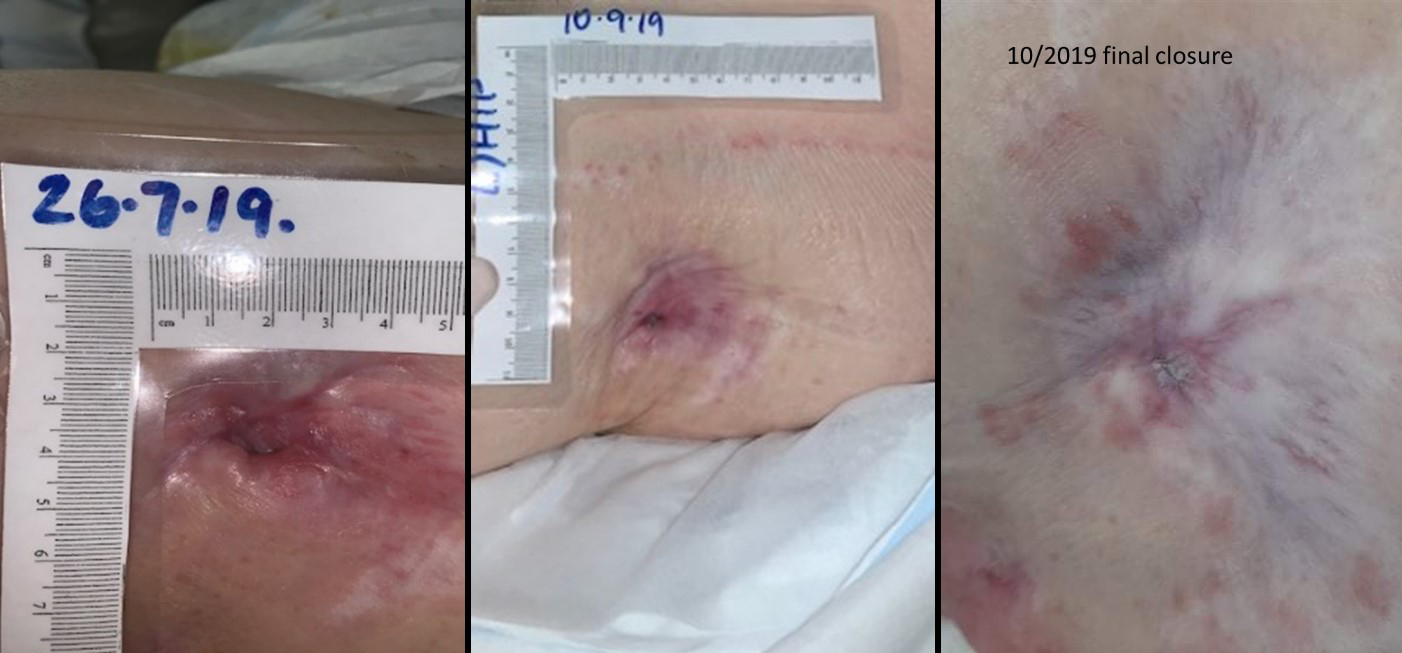
Day 1 Day 60 Day 90
Figure 3. Case 3 shows the wound progression from initiation of the NPWT, to discontinuation at day 60, to complete healing at day 90
Discussion
Introducing the AvelleTM NPWT System to the aged care facility was challenging. It required education for carers and staff about the system, with detailed instruction on application, trouble shooting and monitoring. Success was attributed to one clinician leading the wound care combined with cooperation from Mr B. Both Mr B and his clinicians found that the decreased frequency of dressing changes and the reduced time taken to change the NPWT compared to the previous dressings was noted as an advantage. In addition, the system was cost-effective in comparison to over 12 months of standard wound care dressings and the frequent dressing changes that were necessary in this previously stagnant wound.
Conclusions
Each of these case studies demonstrate the benefits and versatility of a portable NPWT system in community settings. In particular, the series shows that the AvelleTM NPWT System is able to manage exudate, promote healing and decrease frequency of dressing changes, therefore reducing nursing time and costs associated with wound management. Clinicians reported that the system facilitated autolytic debridement, was conformable to a variety of wound locations (including wounds prone to contamination due to incontinence), and provided appropriate exudate management, even in limbs subject to dependent oedema, and that this was attributable to the Hydrofiber® wound interface layer. The system was also reported to be effective in protecting wound periskin from moisture-associated skin damage and in minimising local skin sensitivity which had previously been an issue in two of the cases. This NPWT system is well tolerated by patients and provides a comprehensive solution for hard-to-heal wounds in community settings.
Acknowledgement
We would like to thank the nurses and participants for sharing their stories.
Ethics statement
Written consent was obtained from all participants in this case series.
Conflict of interest
This manuscript was co-authored by an employee of ConvaTec (FH). However, this person had no direct or indirect involvement in patient care.
Funding
The authors received no funding for this study.
Author(s)
Louise Webber1, Wendy Cornish2, Alison Cummins3 and Frances Rachel Henshaw*4
1MNursing Sc (NP), BA (Hons), Grad Cert (Wound Management), Grad Cert. (Orthopaedics), RN
Director, Wound Therapies, QLD, Australia
2Wound Resource Nurse, Hobart Community Health Nursing, Hobart, TAS, Australia
3Nurse Manager, Albury Community, Albury, VIC, Australia
4Professional and Clinical Development Manager, ConvaTec Australia and New Zealand
Conjoint Lecturer, School of Medicine, Western Sydney University, Locked Bag 1797 Penrith, NSW, Australia
*Corresponding author Email Frances.Henshaw@convatec.com
References
- Argenta LC, Morykwas MJ. Vacuum-assisted closure: a new method for wound control and treatment: clinical experience. Ann Plast Surg 1997;38:563–77.
- Apelqvist J, Willy C, Fagerdahl A-M, Fraccalvieri M, Malmsjö M, Piaggesi A, et al. EWMA document: negative pressure wound therapy: overview, challenges and perspectives. J Wound Care 2017;26(Sup3):S1-S154.
- Thompson G. An overview of negative pressure wound therapy (NPWT). Br J Community Nurs 2008;13(Sup3):S23-S30.
- Dhar A, Needham J, Gibb M, Coyne E. The outcomes and experience of people receiving community-based nurse-led wound care: a systematic review. J Clin Nurs 2020;29(15–16):2820–33.
- Duteille F, Sharp E, Traynor C. The AvelleTM NPWT System: clinical experiences. J Wound Care 2018;27(Sup3):S14-S6.
- Dillon J, Clarke J, Kinninmonth A. The Jubilee method: a modern dressing design which reduces complications and improves cost-effectiveness following total hip and knee arthroplasty. Paper presented at: 8th European Federation of National Associations of Orthopaedics and Traumatology Congress; 2007 May 11–15; Florence (Italy).



