Volume 30 Number 3
An application for real-time, remote consultations for wound care at home with wound, ostomy and continence nurses: a case study
Aya Kitamura, Gojiro Nakagami, Miho Okabe, Shinsuke Muto, Tomomi Abe,
Ardith Doorenbos and Hiromi Sanada
Keywords Wound care, telemedicine, home care
For referencing Kitamura A et al. An application for real-time, remote consultations for wound care at home with wound, ostomy and continence nurses: a case study. Wound Practice and Research 2022; 30(3):158-162.
DOI
https://doi.org/10.33235/wpr.30.3.158-162
Submitted 8 November 2021
Accepted 17 January 2022
Abstract
Background Real-time remote consultations could be a way for wound, ostomy and continence nurses (WOCNs) to provide wound care alongside visiting nurses. We developed an application (app) for remote wound care consultations that facilitated high quality video calling and patient data sharing which was specifically designed for Japanese home care settings. In this report, we discuss the case of a patient who received real-time remote consultations through the app.
Case A woman aged in her 90s had a wound on the posterior aspect of her left lower leg. The wound did not show any healing progress for 3 weeks. A WOCN obtained the patient’s information through the app which was uploaded by a visiting nurse before the first consultation. Weekly real-time remote consultations were conducted through the app using video calls. The WOCN could observe the wound in detail, and communicate with both the visiting nurse and the patient. The WOCN assessed that a factor of delayed wound healing was venous insufficiency, and then gave care recommendations. The wound healed within 6 weeks.
Conclusions The WOCN could simultaneously assess the wound and provide care recommendations remotely using the app. This app could contribute to connecting WOCNs, visiting nurses and patients remotely and effectively.
Introduction
Due to the rapid rate at which Japan’s ageing population is increasing, home-based care is being promoted as a strategic medical policy1. More than 700,000 elderly people in Japan use visiting nursing services and the number has been increasing2. Consequently, the demand for wound care in home settings has increased. A pressure injury (PI) is one of the most common wounds in home care settings3. In the Japanese home healthcare system, patients can use visiting nursing services under the direction and recommendation of their doctors, and the fee for the services is covered by the national medical/long-term care insurance. Therefore, daily wound care is commonly provided by visiting nurses. Because wound healing rates can be improved by accompanying consultations from wound, ostomy and continence nurses (WOCNs)4, collaboration between WOCNs and visiting nurses is important to improve wound healing times.
However, 88.9% of WOCNs are affiliated with hospitals. Therefore, although the institutions to which WOCNs belong can obtain 1,285 insurance points (approximately US$130) when a WOCN visits one home to perform care for cases of full thickness PI, doing so is difficult, and less than 5% of patients with full thickness PIs receive WOCN services in home care settings. This can be explained by the fact that most WOCNs work at hospitals, and therefore providing external care is time consuming for them5. In addition, social distancing and isolation rules to mitigate the COVID‑19 pandemic have made it more difficult for WOCNs to perform home visits. Therefore, innovative and convenient ways for WOCNs to provide home care are required.
Remote consultation is a potential method for WOCNs to provide wound care without visiting patients’ homes6. In a previous study, weekly calls from medical professionals were provided to spinal cord injury patients with PIs which were being treated by the patients themselves or their families7. The researchers selected phones as telemedicine tools due to their ubiquity in the study regions in India and Bangladesh. Due to this intervention, experimental subjects’ scores on the Pressure Ulcer Scale for Healing (PUSH) reduced significantly compared to the control subjects, signifying improved healing due to telemedicine7. However, non‑medical personnel and non‑wound specialists were providing telemedicine support, differing from the consultation services in Japan. In another study, a cluster randomised stepped wedge trial was conducted in long‑term care facilities, where residents with PIs and facility staff received consultations with wound specialist teams8. After a control period with no consultation, an intervention period was carried out for 3 months, comprising weekly facility staff education on PI care, followed by remote consultations by phone or email. In contrast with the previous study, no significant differences in wound healing were found between the intervention and control periods. One possible reason for this result may be the means of communication used for wound assessments; since wounds could not be observed over telephones, and photographs could not have covered all sufficient information, wound assessments may not have been effective.
We focused on creating real‑time, remote consultations using video calls to simulate onsite consultations with WOCNs9,10. Our aim was to address some major challenges – firstly, that various tools for videophone/online meetings can pose information security risks11 which is problematic as WOCNs require comprehensive patient data to understand each case and, secondly, that online video and image qualities can often be too poor to allow careful observation. Thus, we developed an application (app) that allowed for both high quality video calling and secure data sharing. This paper outlines an effective case study using the app. The case’s full thickness wound with undermining healed within 2 months through our teleconsultation service.
Case history
System for wound teleconsultations
We developed an iPad app named CARES4WOUNDS‑JP which we developed with the Tetsuyu Healthcare Holdings company from Singapore. We interviewed a nurse with experience in both visiting and home/community‑based care to determine the app’s contents and discuss which information about patients and wounds should be shared to facilitate effective treatment; Table 1 shows items included in the app.
Table 1. Patient information shared via the app
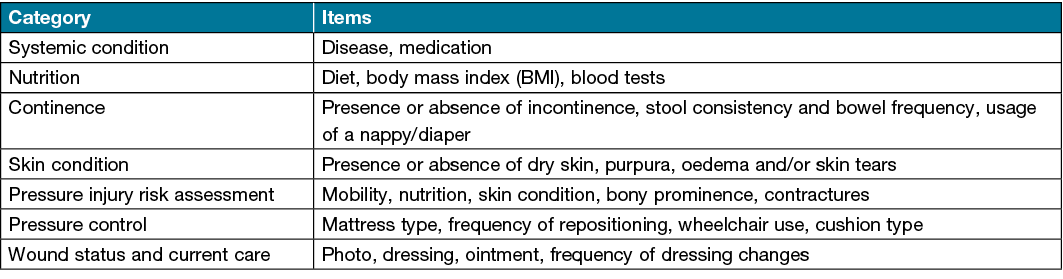
WOCNs could ask visiting nurses to input patient and wound information before the first teleconsultation and could review it through a browser system for time effectiveness. The app also has a video call system with high resolution capacities. Moreover, up to four accounts could participate in video calls simultaneously; thus, teleconsultations could be conducted between teams of medical professionals. Visiting nurses recorded patient and wound information before the first video consultation and updated the data when the patient’s condition changed. After the video consultation, WOCNs recorded a summary of assessments and care recommendations that they explained to visiting nurses during video calls. Patient data was stored in the cloud and could only be accessed by those authorised. Costs for wound treatments and visiting nursing services were borne by patients and covered by the national medical insurance/long‑term care insurance. Patents did not pay an additional fee for the teleconsultations with a WOCN in this study.
Patient information
Our case was a woman aged in her 90s who had chronic kidney failure and dementia, and resided in a group home for people with dementia. She could consume food orally and spent most of her daytime sitting in a wheelchair. The patient’s wound, on the back of her left lower leg, had occurred a few months before the consultation. The wound was treated as a PI. After several wound treatments by a physician, the patient started to receive visiting nursing services, through which it was determined that putting cushions under the leg on the bed may have exerted pressure there, hence the patient was instructed to stop using pillows. The nurses also provided daily wound care, including cleansing and dressing, for approximately 3 weeks. However, the wound did not show any healing progress. Thus, teleconsultation was initiated with a WOCN using the app.
Teleconsultation
Before the first weekly teleconsultation, the WOCN checked the patient’s information using the app. At the first teleconsultation, the wound was 5.5cm x 4.5cm in size and showed unhealthy granulation tissue with sloughing and peripheral undermining. The WOCN observed how the visiting nurse washed the wound, and advised how to improve cleaning the wound bed and surrounding skin12. The WOCN noted pigmentation and oedema on both legs, suggesting chronic venous insufficiency (Figure 1). The visiting nurse confirmed that the dorsalis pedis artery and posterior tibial artery were palpable.
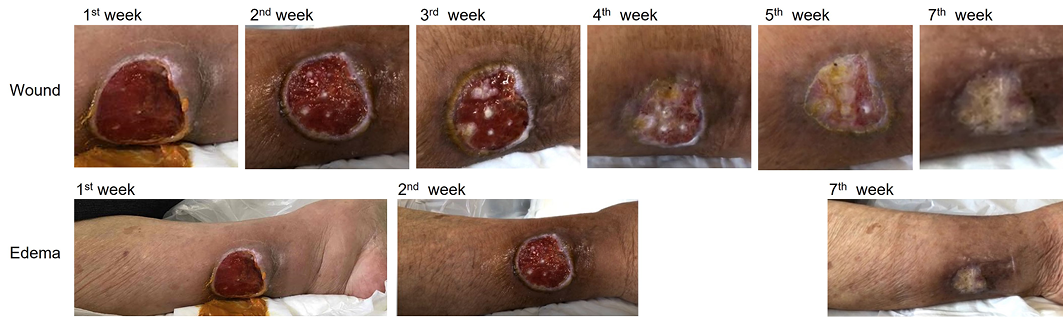
Figure 1. Wound appearance
In the first week, the wound showed undermining and unhealthy granulation tissue, and there was oedema of the lower leg. By the second week, the undermining had disappeared and the surrounding skin had wrinkled, indicating that the oedema was resolving. Epithelialisation began from around the third week. The ulcer had closed by the seventh week.
Additionally, the WOCN assessed the excessive exudate that had accumulated at the wound edge while the patient was sitting, which had resulted in sloughing and undermining. Hence, the WOCN advised that the patient begin using medical compression stockings and recommended that she elevate her leg while sitting. Visiting nurses provided the patient with the recommended care, collaborating with facility staff and the patient’s primary care physician. In concrete terms, the facility staff placed a footstool when the patient used a wheelchair from the next day of the first teleconsultation. With her physician’s agreement, the patient started wearing elastic stockings (5–10mmHg) 2 days after the teleconsultation. At each consultation, the WOCN outlined the wound status, including redness and oedema of the surrounding skin, necrotic tissue, granulation tissue, and wound edge maceration. Oedema was evaluated based on the gross appearance of the skin, such as wrinkles, and the visiting nurses’ palpation.
Additionally, at the first teleconsultation, the WOCN found redness in the wound edge; the patient complained of pain here as well. Therefore, the WOCN recommended continuing to use sucrose and povidone‑iodine ointment for infection management. The visiting nurses provided wound care of cleansing the wound and applying the ointment once a day according to the WOCN’s recommendations. As a result, the erythema and undermining had disappeared by the second teleconsultation and, by the third week, the granulation tissue had reached the same level as the surrounding skin.
In addition, the WOCN recommended vibration therapy to enhance blood flow at the third week13,14. A device for vibration therapy was placed between the mattress and a bed frame and vibration was provided for 20 minutes/day non‑invasively. Moreover, visiting nurses had increased the frequency of dressing changes from once to twice per day because the amount of exudate was too great. Although the patient complained of pain when the dressing was changed during the first week, the pain reportedly disappeared by the third week. By the fourth week, the epithelialisation had advanced remarkably and, by the seventh week, the wound had closed completely. The first three consultations took 20–25 minutes each, including wound care such as wound cleansing and ointment application (Table 2). From the fourth consultation, only wound assessments and care recommendations were conducted during the video calls, reducing the teleconsultation time to less than 15 minutes.
Table 2. Duration of each teleconsultation
![]()
Discussion
This case demonstrated the healing progress of an older adult patient’s wound after teleconsultation with a WOCN through the CARES4WOUNDS‑JP app. Despite the provision of general wound care by visiting nurses before the first consultation, the wound had not shown any healing progress. However, the WOCN was able to assess and identify the factors delaying wound healing, and provided accurate and effective care recommendations, promoting healing. Healing could be achieved because the app allowed the WOCN to observe the wound thoroughly and clearly through convenient video calls, including its colour and texture, the surrounding skin, and the entire leg in detail. In addition, the WOCN could observe the patient’s living environment and physical conditions, due to which the oedema was linked to posture, which was then corrected. Hence, real‑time and high quality video consultations made it possible to observe the wound and other body parts as deemed necessary by the WOCN, and to obtain relevant and detailed information from the patient and visiting nurse.
Since the management of wounds is strongly linked to daily life15, the success of this remote consultation can be attributed to the fact that the WOCN was able to simulate an onsite visit. For instance, a previous study reported that video conferencing was a key facilitator for implementing an internet clinic for the treatment of wounds16. Moreover, communication between the WOCN, visiting nurses and the patient facilitated teamwork in wound management in our intervention. While several studies have reported the use of teleconsultations through email or web systems for wound care in community settings, they did not demonstrate significant efficacy in treating wounds8,17. In contrast, our app allowed teleconsultations to reflect the convenience and accuracy of onsite consultations through high quality video calls, enabling medical professionals to conduct effective and efficient remote consultations.
The teleconsultation time for wound care was approximately 25 minutes for the first three consultations, and 10 minutes after the fourth consultation. A previous study in Japan reported that care time at nurse‑led outstation clinics for wound, ostomy and continence patients were between 30–60 minutes for 83% of patients, and less than 30 minutes for only 15% of patients18. Compared to previously reported times, our results suggest that our app cannot only eliminate WOCNs’ transportation time, but also reduce consultation times, resulting in easier scheduling and time effectiveness.
Although this study examined one case reflecting one type of wound, the WOCN also recommended care based on generalised guidelines of wound care, including exudate management and infection control19. Therefore, the app can provide support and treatment for a variety of wound types; further studies are therefore needed to examine its generalisability, significant effectiveness among a larger population, and cost effectiveness.
Conclusions
Our app, CARES4WOUNDS‑JP, could help WOCNs and visiting nurses to assess wounds together through video teleconsultations. Sharing patient data through the app before video calls supported smooth assessments. Teleconsultations using the app could further broaden WOCNs’ activities in community settings.
Ethics statement
The study procedures were reviewed and approved by the Ethics Committee of the Graduate School of Medicine, the University of Tokyo (2019157NI-(1)) and conducted after obtaining informed consent from the patient.
Conflict of interest
AK, GN, MO, TA, AD and HS declare that there is no conflict of interest. SM is a co-founder and director of Tetsuyu Healthcare Holdings.
Funding
This work was supported by a Grant-in-Aid for Scientific Research from the Japanese Society for the Promotion of Science (JSPS KAKENHI grant number JP19K19732) and a grant from the Social Insurance Union of Societies Related to Nursing.
Author(s)
Aya Kitamura1, Gojiro Nakagami1,2, Miho Okabe3, Shinsuke Muto4, Tomomi Abe4,
Ardith Doorenbos5 and Hiromi Sanada1,2*
1Department of Gerontological Nursing/Wound Care Management, Graduate School of Medicine, The University of Tokyo, Japan
2Global Nursing Research Center, Graduate School of Medicine, The University of Tokyo, Japan
3Wound and skin home care station, Gunma, Japan
4Tetsuyu Institute Medical Corporation, Tokyo, Japan
5College of Nursing, University of Illinois Chicago, Chicago, Illinois, USA
*Corresponding author email hsanada@g.ecc.u-tokyo.ac.jp
References
1. Ministry of Health Labor and Welfare Japan. Establishing ‘the Community-based Integrated Care System’; 2017. Available from: http://www.mhlw.go.jp/english/policy/care-welfare/care-welfare-elderly/dl/establish_e.pdf
2. Ministry of Health Labor and Welfare Japan. Survey of Long-term Care Benefit Expenditures 2020. Available from: https://www.mhlw.go.jp/toukei/list/45-1b.html
3. Pieper B, Templin TN, Dobal M, Jacox A. Wound prevalence, types, and treatments in home care. Adv Wound Care 1999;12(3):117–126.
4. Tochiori A, Sugama J, Okuwa M, et al. The effect of the wound ostomy and continence nurse with the participation in hospital before and after cooperation or pressure ulcer holders. Jpn J PU 2014;16(4):528–537.
5. Vaartio-rajalin H, Nasman Y, Fagerstrom L. Nurses’ activities and time management during home healthcare visits. Scand J Caring Sci 2019;34(4):1045–1053.
6. Chen L, Cheng L, Gao W, Chen D, Wang C, Ran X. Telemedicine in chronic wound management: systematic review. JMIR mHealth uHealth 2020;8(6):1–12.
7. Arora M, Harvey LA, Hayes AJ, et al. Effectiveness and cost-effectiveness of telephone-based support versus usual care for treatment of pressure ulcers in people with spinal cord injury in low-income and middle-income countries: study protocol for a 12-week randomised controlled trial. BMJ Open 2015;5(7):e008369.
8. Stern A, Mitsakakis N, Paulden M, et al. Pressure ulcer multidisciplinary teams via telemedicine: a pragmatic cluster randomized stepped wedge trial in long term care. BMC Heal Serv Res 2014;14:83.
9. Ratliff CR, Shifflett R, Howell A, Kennedy C. Telehealth for wound management during the Covid-19 pandemic case studies. J Wound Ostomy Cont Nurs 2020;47(5):445–449.
10. Wibbenmeyer L, Kluesner K, Wu H, et al. Video-enhanced telemedicine improves the care of acutely injured burn patients in a rural state. J Burn Care Res 2016;37(6):e531–e538.
11. Watzlaf VJM, Moeini S, Matusow L, Firouzan P. VOIP for telerehabilitation: a risk analysis for privacy, security and HIPAA compliance: part II. Int J Telerehabil 2011;3(1):3–10.
12. Konya C, Sanada H, Sugama J, Okuwa M, Kitagawa A. Does the use of a cleanser on skin surrounding pressure ulcers in older people promote healing? J Wound Care 2005;14(4):169–171.
13. Nakagami G, Sanada H, Matsui N, et al. Effect of vibration on skin blood flow in an in vivo microcirculatory model. BioSci Trends 2007;1(3):161–166.
14. Arashi M, Sugama J, Sanada H, et al. Vibration therapy accelerates healing of Stage I pressure ulcers in older adult patients. Adv Ski Wound Care 2010;23(7):321–327.
15. European Pressure Ulcer Advisory Panel, National Pressure Injury Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and treatment of pressure ulcers/injuries: clinical practice guideline: the international guideline. Emily Haesler (Ed.). EPUAP/NPIAP/PPPIA; 2019.
16. Walia S, Wolfe D, Keast D, et al. Facilitators and barriers for implementing and internet clinic for the treatment of pressure injuries. Telemed e-Health 2019;25(12):1237–1243.
17. Terry M, Halstead LS, O’Hare P, et al. Feasibility study of home care wound management using telemedicine. Adv Ski Wound Care 2009;22(8):358–364.
18. Management C, Tsuchida T, Iizaka S, et al. National survey report on developing a wound, ostomy and continence nurse-led outpatient care model. J Jpn WOCM 2020;24(3):338–348.
19. The Japanese Society of Pressure Ulcers Guideline Revision Committee. JSPU guidelines for the prevention and management of pressure ulcers (4th ed). Jpn J PU 2016;18(4):455–544. Available from: https://minds.jcqhc.or.jp/n/med/4/med0036/G0000956/0001



