Volume 31 Number 2
International stakeholder survey to inform the development of a Pan-Pacific clinical guideline on venous leg ulcer prevention and management
Emily Haesler, Judith Barker, Mandy Pagan, Keryln Carville, Richard Greene, Cathy Hammond, Sivagame Maniya, Pang Yuk Kam, Pang Chak Hau, Maria Schollum, Cecilia Tin Yan Sit, Tay Hsien Ts’ung
Keywords venous leg ulcer, survey, outcomes, consumer engagement
For referencing Haesler E et al. International stakeholder survey to inform the development of a Pan-Pacific clinical guideline on venous leg ulcer prevention and management. Wound Practice and Research 2023; 31(2):59-67.
DOI
https://doi.org/10.33235/wpr.31.2.59-67
Submitted 5 May 2023
Accepted 28 June 2023
Abstract
Background Venous leg ulcers (VLUs) are chronic wounds occurring in people with venous insufficiency, causing significant burden. The last clinical guideline providing recommendations on the prevention and management of VLUs in the Pan-Pacific was published in 2011.
Method A stakeholder survey was undertaken to collect perspectives from health professionals, industry representatives, patients and caregivers. The survey was designed with consideration to guideline development methods. It was developed in consultation with a patient representative and reviewed by a Māori consultation group. The survey was based on an audit of content in the 2011 VLU guideline and collected opinions on topics of priority to include in a guideline and clinical outcomes of importance to evaluating interventions for VLUs. Recruitment was through promotion by the sponsoring wound organisations. Data were analysed using descriptive statistics.
Results A total of 271 people, including 19 patients and three caregivers, responded. Almost all the 35 topics were rated as high priority to include in a guideline. Almost all the 60 clinical outcomes were rated as critically important to evaluating VLU interventions.
Conclusion Results indicated that respondents have a high need for information about VLUs. The results will inform the development of an upcoming VLU guideline for the Pan-Pacific region.
Background
As a Pan-Pacific Alliance, the New Zealand Wound Care Society (NZWCS), the Hong Kong Enterostomal Therapists Association (HKETA), Wounds Australia and the Wound Healing Society of Singapore (WHSS) are embarking on the development of a new edition of a regional clinical guideline for the prevention and management of venous leg ulcers (VLU). A VLU is a full-thickness defect of the skin that occurs due to venous disease of the lower leg1,2. VLUs are painful3, slow to heal3,4, and frequently recur3, causing significant reduction in quality of life (QoL)3,4 and costly management4. Venous ulceration is a chronic condition that occurs due to venous occlusion, incompetent calf muscle pump function, and/or venous valvular failure, giving rise to poor venous return, venous hypertension, chronic oedema and inflammation, and venous valve damage1,2. VLUs are strongly associated with a medical history of varicose veins, chronic venous disease (CVD), phlebitis, deep vein thrombosis (DVT), congestive cardiac failure and/or previous leg injury/surgery3,5. However, further research is still required to fully understand the development of VLUs and why these wounds can be difficult to heal6.
The prevalence of symptomatic venous disease in countries of ethnic diversity similar to New Zealand and Australia is reported to range from 6.8% to 39%7. An audit conducted in a Chinese wound healing department reported prevalence of VLU as 9.4%8. In a study reporting the incidence of chronic wounds from a nationwide database in Singapore, the Indian minority had a higher incidence rate of venous wounds compared to the Chinese majority, especially among those aged 50 years and above9. Prevalence in other south-east Asian countries is unreported10,11.
Evidence-based management of VLUs
Early detection of VLU risk with consequential appropriate preventive strategies, management of underlying disease and rapid management should ulceration occur are important in reducing the burden of VLUs. Evidence-based guidelines facilitate this level of healthcare because they provide clinical recommendations based on the best available research that health professionals can translate and implement in their management of people with or at risk of VLUs. Clinical guidelines also serve as an education source for health professionals, and are an important resource for governments, health policy developers, educators, researchers, patients, informal carers and other people interested in VLUs.
Region-specific clinical guidelines provide guidance for health professionals that address the needs of the populations, with consideration to the healthcare systems in which care is delivered. The last regional clinical guideline for managing VLUs, Australian and New Zealand clinical practice guideline for prevention and management of venous leg ulcers1, was published in 2011. Since that time, a substantial body of research on the prevention and management of VLUs has been published, and wound care has advanced. Additionally, there has been a global shift, mirrored in the Pan-Pacific, from diagnosis and management primarily occurring in the tertiary healthcare sector to community-based identification and treatment12,13. Thus, it is timely to update the VLU guideline used by many Pan-Pacific wound clinicians.
Stakeholder involvement in guideline development
Engagement of stakeholders is recognised as an important component in developing clinical guidelines14–18. Patients and their caregivers can provide insight into the relevance of different interventions and clinical outcomes to their healthcare and can contribute to implementation guidance from their own health experiences. This information is important to ensure that guidelines address clinical questions of importance to patients, and that recommendations will promote outcomes that they consider significant19. Ultimately, all clinical guidelines must meet the needs of patients.
However, there are several barriers to partnering with patients and caregivers. Discrepancies between perspectives on the relevance of different information; challenges in integrating lay opinion; difficulty establishing and maintaining partnerships; recognising the level of understanding lay people have of relevant information; resource constraints; resistance to change; and cultural (e.g., language), health (e.g., sensory impairment) and physical (e.g., lack of internet) barriers, can all influence the success of partnerships14,15,20. As such, a range of recommended partnering strategies are being used throughout the VLU guideline development project. This study, which is part of that larger project, reports the results of an early consultation process collecting data on the preferences of stakeholders for guideline content and accompanying resources that was one component of engaging with patients and caregivers.
Health professionals who will use a clinical guideline are also important stakeholders. Their involvement in guideline development was recognised as a requirement for a robust clinical guideline in the earliest 2003 version of the AGREE tool for critically evaluating guidelines21. The health professionals who will use a guideline can provide input from a multidisciplinary perspective, evaluating the relevance, applicability and feasibility of recommendations to the clinical setting. As such, health professionals were involved in the development of previous editions of the VLU guideline, and this study sought to continue and improve this engagement by seeking early input from a wide health professional audience.
Guideline development processes: clinical questions and core outcomes
The development of a clinical guideline requires evaluation and synthesis of evidence that addresses specific clinical questions and makes recommendations based on this evidence18. In brief, clinical questions are designed around the effectiveness of an intervention for achieving a specific clinical outcome for a defined population. Because a clinical guideline and its recommendations will be based around the clinical questions that are being asked, establishing appropriate and relevant clinical questions at the outset of the development process is extremely important. To ensure the final clinical guidance is relevant to the health professionals that will implement the advice, and to the patients who will receive care, the underpinning clinical questions must address issues of relevance to end users18,22. In particular, the topic of the question should be a priority for stakeholders, and the health outcomes that particular interventions might achieve should be considered important.
Where they exist, guideline developers can use core outcome sets to identify important health outcomes. A core outcome set refers to a standardised set of outcomes that should be measured and reported in clinical trials specific to a health condition23,24. An example of a potential core outcome for VLUs is ‘complete wound healing’. Currently there is no agreed core outcome set for VLUs (or chronic wounds in general), and no published data on topics that health professionals, patients, caregivers and other stakeholders consider important to address in a VLU clinical guideline. One strategy considered appropriate to addressing the lack of information to inform guideline development decision-making includes undertaking empirical research18,25.
Purpose and aims
The purpose of this study was to collect data on the topics that stakeholders consider a priority to address, as well as clinical outcomes that they consider important to address in a VLU guideline. In the context of this project, stakeholders included patients (i.e., people currently or previously with or at risk of a VLU), informal caregivers (i.e., people who provide care in an informal capacity such as family members, friends or community) and health professionals and workers, educators and researchers, policy makers, industry representatives and special interest groups (e.g., people from Indigenous backgrounds). Collecting and analysing this data was undertaken with the aims of informing the future selection of clinical questions for address in the upcoming edition of the VLU guideline, and identifying topics for potential companion education resources.
Methods
The study was undertaken using a descriptive, cross-sectional survey design. The research received ethical approval from Curtin University Human Research Ethics Committee (HRE2022-0394) in Australia and the Māori Ngāi Tahu Research Consultation Committee and University of Otago (H22/083) in New Zealand. In consultation with the Singapore and Hong Kong wound societies, respective country-specific ethics approval was not required.
Target population and recruitment
A voluntary and anonymous survey accessible to anyone with knowledge of the survey and with internet access was used to collect data. The survey landing page included a Participant Information Sheet and consent to participate. The survey was promoted by NZWCS, HKETA, Wounds Australia and WHSS via social media, newsletters and websites, and by the research team through conference presentations and professional email lists. A recruitment poster was made available for health professionals aware of the survey to use for direct recruitment of patients and informal caregivers in their clinical practice, where this was consistent with their local policies.
Data collection survey
Data collection was undertaken using a project-specific, anonymous, online survey of stakeholders that collected primarily quantitative data on the importance of clinical topics and health outcomes related to VLU prevention and treatment. The data collection survey was developed by a research team that included wound clinicians from Australia, New Zealand, Hong Kong and Singapore, as well as a patient representative. As described below, the survey was developed with consideration to guideline development methodology19,26,27.
The survey included demographic information, level of interest in specific population groups, perspectives of how important different clinical areas are to include in a VLU guideline, and perspectives of how critical different clinical outcome measures are for evaluating interventions. Demographic information included type of stakeholder (i.e., patient, informal caregiver, health professional, educator/researcher, industry representative), country of residence, gender, age and cultural identification. Respondents identifying as patients or informal caregivers were presented with a lay version of the survey and other respondents received a professional version of the survey, the difference primarily being the terminology used.
Respondents were asked to rank their interest in different VLU at-risk populations from most to least interest. Respondents were presented with a list of specific populations, primarily developed from a review of the VLU guideline1. The specific populations addressed in previous editions of the VLU guideline were based on the National Health and Medical Research Council’s requirements for clinical guidelines28. Additional populations considered to have a higher risk of VLUs3 and clinical settings in which the clinical experts on the research team considered the guideline might be used were also included.
The next set of questions on the survey asked respondents to rank VLU-related topics according to their prority for inclusion in a guideline using a five-point categorical scale (considerable priority/must include; moderate priority/would be good to include; some priority/may include; little priority/likely not include; no priority/do not include). A total of 35 topics presented in the survey were compiled from an audit of clinical areas covered in the 2016 VLU guideline revision to determine stakeholder interest in what had previously been considered a comprehensive range of VLU-related topics. The ranking system was selected as it is recommended in methodology as the preferred system for determining the priority of different clinical questions26. Respondents were also given an opportunity to provide open-ended responses indicating any additional topics they considered to be important.
Next, respondents were asked to rank the importance they placed on different clinical outcomes using a nine-point ordinal scale. The ranking scale was one that is used in GRADE methodology for evaluating the importance of clinical outcome measures27. The clinical outcomes were developed from an audit of the 2016 VLU guideline that identified clinical outcomes reported in previous research. This audit identified 15 outcome measures reported in research on preventing VLUs, and 45 outcomes used in studies reporting management of VLUs. All these outcomes were included in the survey for professionals, and a sub-set were included in the patient/carer survey. Based on patient and caregiver consultation, some outcomes were not presented to lay stakeholders to reduce the survey’s complexity and length. For example, the lay version presented broad clinical outcomes (e.g., severity of venous disease) but not more specific options to udertake similar evaluation (e.g., score on the CEAP classification scale). Additional topics related to the Māori Te Whare Tapa Whā Health Model29 and the Fonua Pacific Model of Wellbeing30 were added based on New Zealand Māori consultation conducted in the ethics approval process.
To increase cultural accessibility, the survey questions were organised to be consistent with the Māori Te Whare Tapa Whā Health Model29 and the Fonua Pacific Model of Wellbeing30. These New Zealand Indigenous peoples’ models identify dimensions that are the cornerstones for health and wellbeing. To encompass these philosophies, the questions presented to respondents were presented according to the relevant dimensions of Taha tinana (physical wellbeing), Taha wairua (spiritual wellbeing), Taha whānau (community/family wellbeing) and Taha hinengaro (mental wellbeing)29,30.
The survey was presented online and was accessible via a QR code or web address for a period of 3 months from mid-July to mid-October 2022. The survey included drop-down menus, drag-and-drop options and click-to-select options to enable a fast response with limited barriers to access. Participants were able to skip questions as preferred and were free to withdraw from the survey at any time by closing their web browser before survey submission.
Data analysis
Data was downloaded from the consumer survey platform into spreadsheets and analysed in Excel. Categorical data were summarised using frequencies and percentages and ordinal data were summarised as medians and interquartile range (IQR).
Results
There were 271 respondents, of whom 131 were from New Zealand, 103 were from Australia, 16 were from Singapore, 15 were from Hong Kong and six were from other geographic regions. Respondents included 231 health professionals/workers, 18 industry representatives, 19 patients and three informal caregivers. Respondents identifying as patients included people who currently or previously have had a VLU (n=14) and people who have been given health advice that they were at risk but had never experienced a VLU (n=5). Patient respondents primarily identified as male (n=12, 63%), as did informal caregivers (n=2, 67%). Patient respondents (n=13, 68%) and caregiver respondents (n=2, 67%) were primarily aged over 55 years. A total of 71 respondents (26%) identified as being from a cultural/linguistic background considered to be diverse in their country of residence. Five (26%) patient respondents and 16 (6.9%) health professionals/workers identified with an Indigenous background. All respondents identifying as Indigenous identified as being of Māori or Pacific Islander background, regardless of their identified country of residence.
Populations of interest
Patient and caregiver respondents were asked about their interest in receiving VLU-related information about specific risk profiles for people with or at risk of VLUs. Patient respondents had interest in information for overweight (n=8, 42%) and elderly people (n=8, 42%), and people with an Indigenous background (n=5, 26%), disability (n=3, 16%), a diverse cultural background (n=3, 16%), living alone (n=3, 16%) or living in a rural or remote region (n=2, 11%). Carer respondents had interest in VLU-related information specific for overweight people (n=2, 67%), people with disability (n=1, 33%) and people from a diverse cultural background (n=1, 33%).
Professional respondents were asked to rank specific populations at risk from most to least interest. Their interests aligned with that of patient and caregiver respondents. High interest was expressed in information specific to older and overweight people with or at risk of VLUs, there was moderate interest in information specific to Indigenous populations and people living with disability, and lowest interest in information specific to people in rural/remote areas, in isolation or from culturally/linguistically diverse backgrounds. Professional respondents also ranked the clinical settings in which they were most interested in delivery of VLU prevention and management. The highest levels of interest were in home settings, residential aged care settings and onsite wound care services. There was moderate interest in care delivery in general practice, outpatient settings and other residential care, and lower interest in care in inpatient settings.
Topics of interest
Across all respondents, ranked from most to least interest, was diagnosis of VLUs, prevention of VLUs, management of VLUs and engagement with patient/caregivers.
The median rating for whether evidence-based clinical guidance on the topic should be addressed in a VLU guideline for most interventions/issues associated with VLU prevention was ‘must include’. Both health professionals and patient/carer respondents rated compression bandaging regimens, lifestyle interventions for preventing an initial VLU, how to prevent VLU recurrence, and how to prevent an initial VLU as having higher priority to include than surgical/procedural interventions for preventing venous disease.
Across all respondents, most assessment and referral topics were rated as ‘must include’ for developing evidence-based clinical guidance. Patient/carer respondents considered assessment of nutritional status, assessment of wound infection, diagnostic criteria for a VLU and when to make referrals as ‘must include’ topics, and assessment of lifestyle and pain as ‘moderate priority to include’. Health professionals rated all assessment and referral topics as ’must include’ except assessment of nutrition, which was rated at ‘moderate priority to include’.
Median ratings from the overall respondent cohort for almost all VLU management topics were ‘must include’. Patients and caregivers rated all topics presented as ‘must include’ topics. Health professionals ranked all topics as being of highest priority to include (‘must include’) excepting negative pressure wound therapy (NPWT) (‘moderate priority to include’).
Most topics on wellbeing for people with or at risk of VLUs were rated as being a ‘moderate priority to include’ by the full cohort of respondents. Community wellbeing and spiritual wellbeing (‘some priority/may include’) were ranked as being of lower priority by patient/carer respondents than overall QoL (‘must include’), promotion of family (‘must include’) and mental wellbeing (‘moderate priority to include’). Health professionals ranked all wellbeing topics as ‘moderate priority to include’, excepting overall QoL that was ranked as ‘must include’.
Ranking of importance for clinical outcomes
Respondents used the scale of 0–9 to rate the importance of different health outcomes27 for deciding whether to use an intervention or otherwise. According to the scale, ratings of 7–9 are considered critical for decision-making27. As presented Figures 1 & 2a–c, when taking the median rating of all participants, all clinical outcomes – those related to VLU prevention and management – were rated as critical (median score of 7–9) for decision making.
With respect to evaluating the prevention of VLUs through interventions for venous disease management (Figure 1), the full cohort of respondents rated development of a new VLU with a median score of 8 (IQR=2). Using any measure of the severity of venous disease was rated as critically important (median score=8, IQR=2) to evaluating an intervention. Specific methods to evaluate venous disease severity were all rated by health professionals as critically important, including CEAP classification (median score=7, IQR=3) valid and reliable disease severity tools (median score=8, IQR=2), ultrasound (median score=8, IQR=3), and subjective opinion of both health professionals (median score=7, IQR=3) and patients (median score=7, IQR=3).
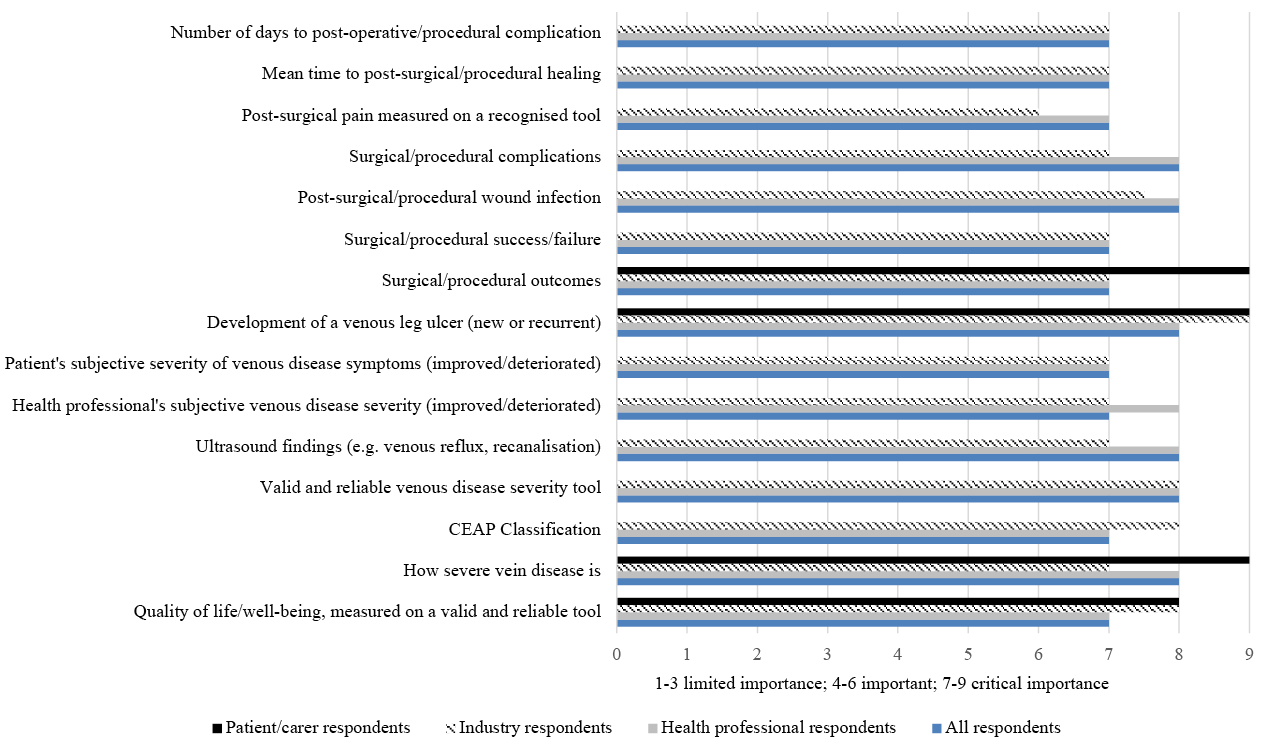
Figure 1. Median ratings of importance of clinical outcomes related to preventing VLUs.
Note: patient/carers were only asked to rate a sub-set of the outcomes
With respect to VLU healing measures to evaluate an intervention (Figures 2a–c), health professionals rated time to complete healing as a critical outcome measure (median score=8, IQR=2). This outcome was rated at median score of 9 (IQR=0.25) by industry representatives, and a median score of 9 (IQR=1) by patients and caregiver respondents. Percent decrease in wound surface area was rated as critically important by health professionals (median score=8, IQR=3), industry representatives (median score=8.5, IQR=1.25) and patients/caregivers (median score=8, IQR=2). Achieving a specific percent reduction in VLU size (e.g., 25% reduction, 50% reduction etc.) over a non-specified duration was also considered critically important by the full cohort of respondents when evaluating an intervention’s effectiveness (for all percent reduction options, median score=8, IQR=2). Across all respondents, improvements in the tissue type in a wound (median score=8, IQR=2), decrease in wound exudate (median score=8, IQR=2), decrease in wound odour (median score=8, IQR=2), wound pain (median score=8, IQR=2) and changes in signs and symptoms associated with inflammation and infection (median score=9, IQR=1) were all considered critically important to evaluate the effectiveness of an intervention. Cost of an intervention (median score=7, IQR=3) and ease of use (median score=8, IQR=3) were also rated as critically important.
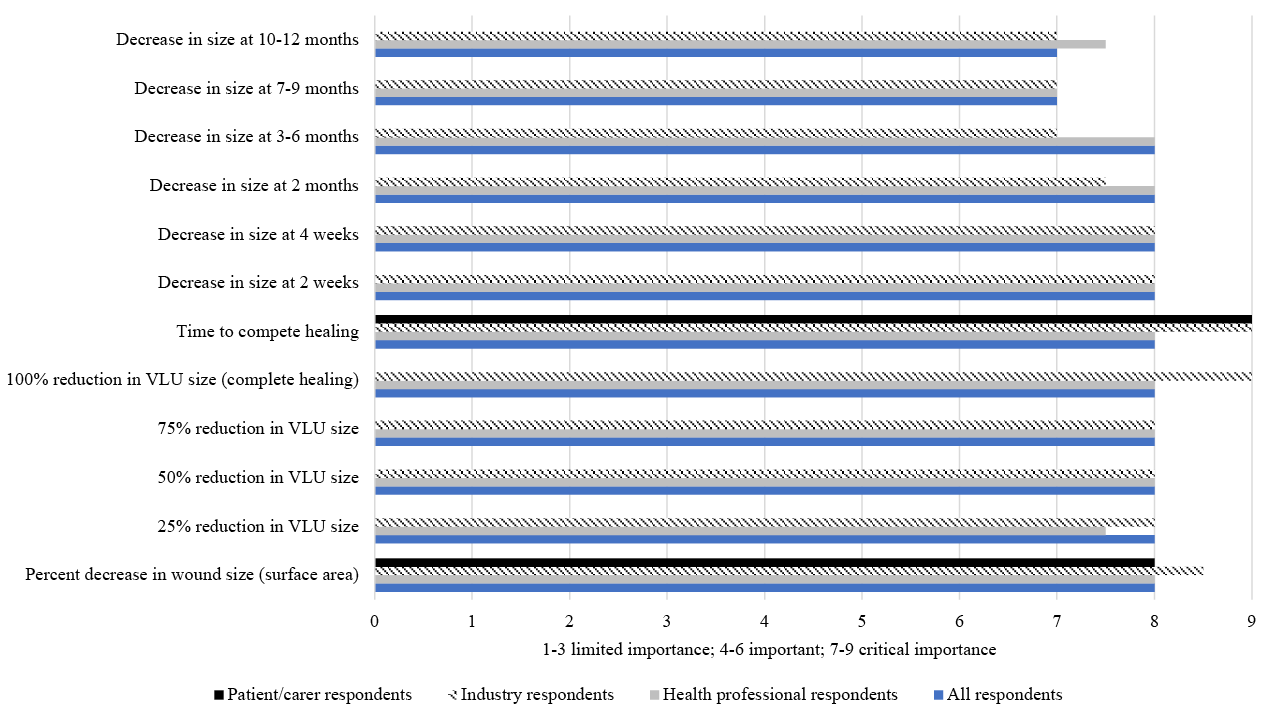
Figure 2a. Median rankings of importance of clinical outcomes for managing VLUs.
Note: patient/carers were only asked to rate a sub-set of the outcomes
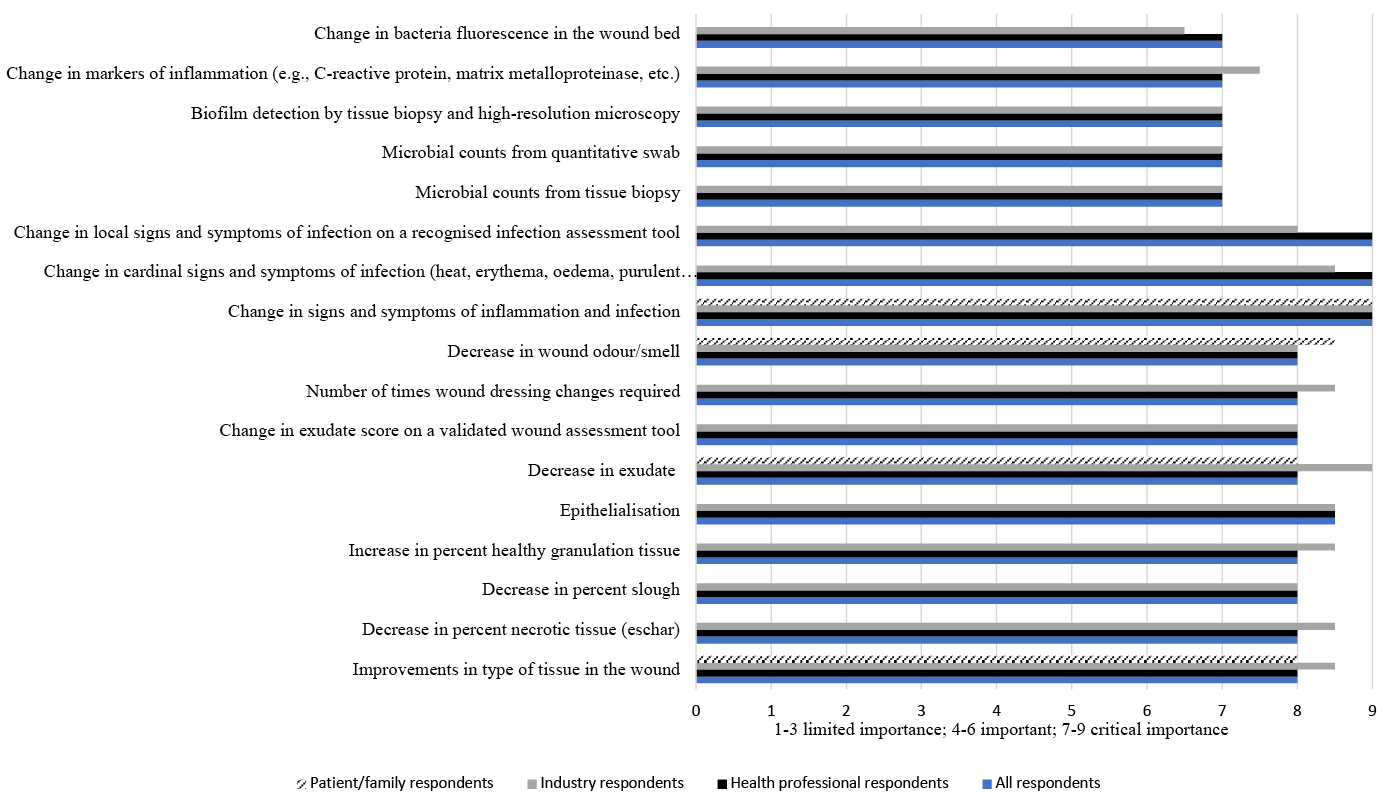
Figure 2b. Median rankings of importance of clinical outcomes for managing VLUs.
Note: patient/carers were only asked to rate a sub-set of the outcomes
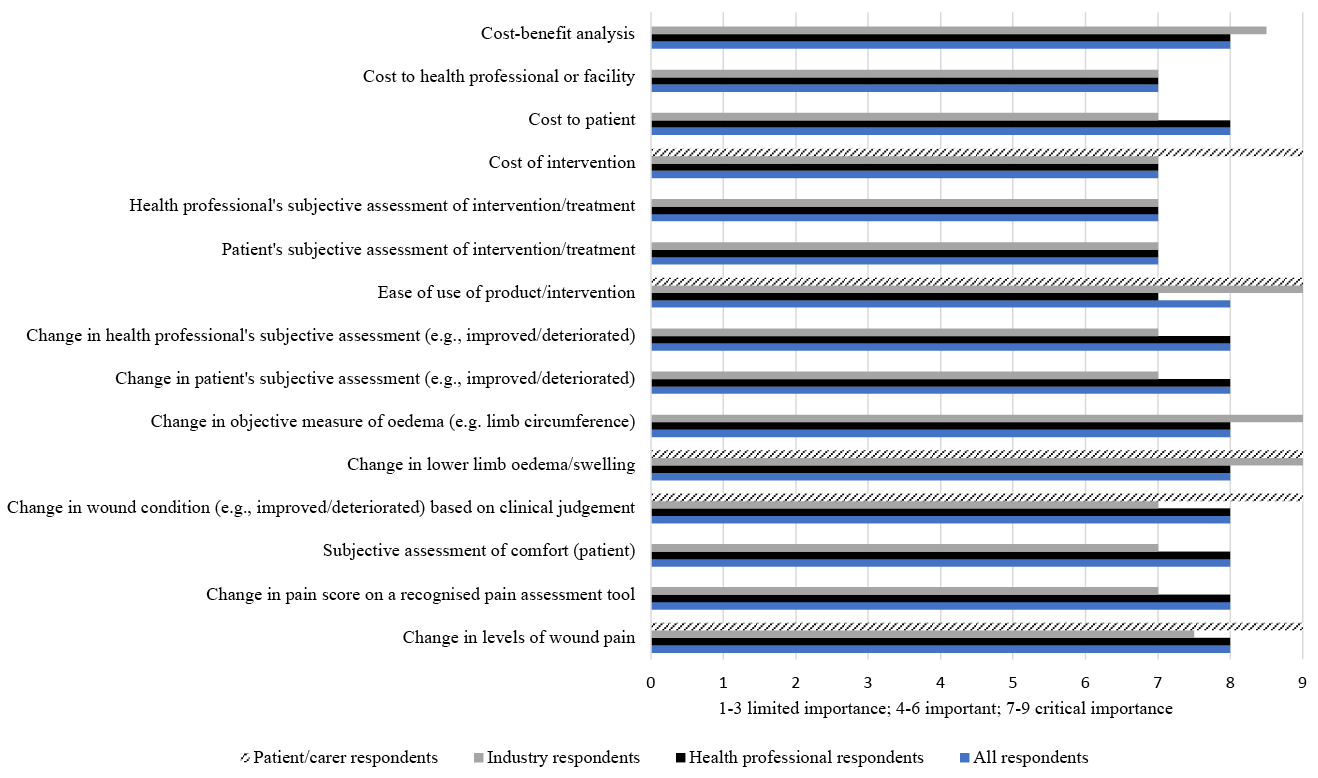
Figure 2c. Median rankings of importance of clinical outcomes for managing VLUs.
Note: patient/carers were only asked to rate a sub-set of the outcomes
Discussion
This study investigated the perspectives of health professionals, educators/researchers, industry representatives, patients with/at risk of VLUs and informal caregivers on topics of priority and clinical outcomes of importance. The data was collected to inform the development of an update of a VLU guideline for use in the Pan-Pacific region. Understanding the perspectives of stakeholders can inform the decisions that guideline development groups make regarding what clinical questions to address in an evidence-based guideline. These decisions underpin the literature search, evidence selection and ultimately the clinical guidance that a guideline will provide. The results of the survey indicated that there is broad agreement between different types of stakeholders (i.e., clinicians, educators/researchers, patients and industry representatives) on the clinical guidance that would be significant to produce. In the next stage of the larger project, the research team will use this information when developing clinical questions to address in the next VLU guideline, and to decide on information that could be developed to accompany the guideline.
In this survey, the majority of 60 clinical outcomes reported in research on VLU prevention and management were considered critically important when evaluating options for clinical care. The high number of outcome measures reported in the research reflects the lack of an existing core outcome set for VLUs (or chronic wounds), and this appears to be reflected in a lack of discrimination in clinical practice regarding utility of different VLU-related outcome measures. In particular, numerous different ways to evaluate healing of a VLU (19 outcomes, not including outcomes specific to evaluating infection) and to monitor CVD (10 outcomes) were identified in the research. Health professionals rated subjective measures as equally important as objective measures to evaluating wound healing. For example, subjective opinion of whether a wound was deteriorating or improving (median score=8, IQR=2) was rated equivalently to reduction in wound surface area (median score=8, IQR=2) and time taken to achieve healing (median score=8, IQR=2). This suggests that wound professionals rely on clinical judgement as much as objective measures in determining whether an intervention is achieving benefits. This also suggests that a clinical guideline should include information on applying clinical judgement to implementation of evidence-based recommendations.
The findings suggest that this area is ripe for future research and identification of outcome measures that truly reflect clinical significance attained from an intervention. In further work on the most critical outcomes to evaluate interventions in clinical practice (and therefore outcomes that should be included in VLU research), exploration of the correlation between wellbeing/QoL measures and different ways to evaluate wound healing and severity of venous disease would be advantageous. A core outcome set for VLUs should ultimately reflect improvements in health that are meaningful for patients.
In the next stage of this project, the results on the importance of different clinical outcomes will contribute to development of clinical questions27,31. While the survey results provide minimal guidance for refinement of specific clinical questions owing to the large number of clinical outcomes that stakeholders considered critically important, the results can also be used to inform evaluations of the evidence base that are made when developing an evidence-based guideline32.
In this study, almost 8% of respondents were Māori and Pacific Islander people. The capture of opinions of Māori and Pacific Islander people (both health professionals and patients/caregivers) in this survey is particularly significant, as this population is under-represented in the VLU research. Consultation with Māori and Pacific Islander advisors was undertaken in the ethics approval process to facilitate development of a culturally sensitive survey, leading to adoption of the Māori Te Whare Tapa Whā Health Model and the Fonua Pacific Model of Wellbeing. Working with both patient representatives and Indigenous groups early in the design and delivery of stakeholder-based research is important to understanding expectations and promoting contribution33. Future work that will be conducted as a part of the larger project will seek consultation with Indigenous Australians and local ethnic groups in Hong Kong and Singapore.
This survey had several limitations. Respondents self-selected to participate in this survey, which may bias recruitment toward participants with a greater interest in VLUs34. This could explain the high priority ratings given to almost all VLU-related topics by the respondents. Self-selection and self-reporting have been cited as fundamental sources of bias in survey data collection.
The survey was also limited by the small number of responses received, particularly from patient/carer stakeholders (n=22), and this reduces the generalisability of the findings. The small number of patient/informal caregiver responses may reflect local restrictions health professionals experience when attempting to promote patient awareness of, and participation in, opportunities to engage in external research, including providing feedback for national guidelines. Additionally, there may have been barriers to accessing the survey. The survey took 10–15 minutes to complete, which may have reduced engagement of some respondents, and it was only available in English.
Using a descriptive cross-sectional design, this study collected perspectives from health professionals, patients, informal caregivers, industry representatives and other stakeholders without testing any a-priori hypotheses. The study was not designed to make comparisons between different types of stakeholders. The different interests and priorities between stakeholder groups could be explored in the future in comparative research studies.
Conclusion
This research sought to capture the perspectives of stakeholders, including health professionals, educators, researchers, industry representatives, patients and informal caregivers, on VLU-related topics of priority and clinical outcomes of importance. The results indicated that respondents consider most VLU-related topics and clinical outcomes to be of significance, and that different categories of stakeholders had similar perspectives. The findings will be used to inform the development of an upcoming Pan-Pacific VLU clinical guideline that will undergo further public consultation.
Conflicts of interest
The authors declare no conflicts of interest.
Ethics statement
This study was approved by Curtin University Human Research Ethics Committee (HRE2022-0394), the Māori Ngāi Tahu Research Consultation Committee and University of Otago (H22/083).
Funding
This study was funded by NZWCS, HKETA, Wounds Australia and WHSS.
Author(s)
Emily Haesler*1,2,3, Judith Barker4, Mandy Pagan5, Keryln Carville6, Richard Greene7,
Cathy Hammond, Sivagame Maniya8, Pang Yuk Kam9, Pang Chak Hau, Maria Schollum10, Cecilia Tin Yan Sit11, Tay Hsien Ts’ung12
1Curtin University, Curtin Health Innovation Research Institute (CHIRI), Wound Healing and Management Collaborative, Australia
2Adjunct Associate Professor, La Trobe University, Australian Centre for Evidence Based Aged Care, Australia
3Honorary Senior Lecturer, School of Medicine and Psychology, Australian National University, Australia
4Nurse Practitioner Wound Management, Community Care Program, Rehabilitation, Aged and Community Services, Canberra Health Services, Australia
5Wound Clinical Nurse Specialist, Te Whatu Ora Health New Zealand Southern, New Zealand
6Professor Primary Health Care and Community, Silver Chain Group and Curtin University, Australia
7Honorary Senior Lecturer, Fenner School of Environment and Society, Australian National University, Australia
8Senior Nurse Clinician, Sengkang General Hospital, Singapore
9Nurse Consultant (Stoma and Wound Care), Kowloon Central Cluster, Hospital Authority, Hong Kong
10Nurse Practitioner, Te Whatu Ora Health New Zealand Waikato, New Zealand
11Senior Lecturer, School of Nursing, The University of Hong Kong, Hong Kong
12Vascular Surgeon and Director SingHealth, Duke-NUS Vascular Centre, Singapore
*Corresponding author email emily.haesler@curtin.edu.au
References
- Australian Wound Management Association (AWMA), New Zealand Wound Care Society (NZWCS). Australia and New Zealand clinical practice guideline for prevention and management of venous leg ulcers. Osborne Park, WA: Cambridge Media; 2011.
- Nicolaides A. The most severe stage of chronic venous disease: an update on the management of patients with venous leg ulcers. Adv Ther 2020;37(Suppl 1):19–24.
- Meulendijks A, de Vries F, van Dooren A, Schuurmans M, Neumann H. A systematic review on risk factors in developing a first-time venous leg ulcer. J Eur Acad Dermatol Venereol 2019;33(7):1241–8.
- Barnsbee L, Cheng Q, Tulleners R, Lee X, Brain D, Pacella R. Measuring costs and quality of life for venous leg ulcers. Int Wound J 2019;16(1):112–21.
- de Araujo T, Valencia I, Federman D, Kirsner R. Managing the patient with venous ulcers. Ann Intern Med 2003;138(4):326–34.
- Raffetto J, Ligi D, Maniscalco R, Khalil R, Mannello F. Why venous leg ulcers have difficulty healing: overview on pathophysiology, clinical consequences, and treatment. J Clin Med 2020;10(1):29.
- Liu G, Xu X, Ziegenbein R, Clough A, Parsi Y, Oomens D, Clarke J. A critical appraisal of chronic venous insufficiency ultrasound guidelines – views of Australian sonographers. Sonography 2022;9(4):166–74.
- Sun X, Ni P, Wu M, Huang Y, Ye J, Xie T. A clinicoepidemiological profile of chronic wounds in wound healing department in Shanghai. Int J Low Extrem Wounds 2017;16(1):36–44.
- Goh O, Ganesan G, Graves N, Ng Y, Harding K, Tan K. Incidence of chronic wounds in Singapore, a multiethnic Asian country, between 2000 and 2017: a retrospective cohort study using a nationwide claims database. BMJ Open 2020;10(9):e039411.
- Taengsakul N. Risk factors for and treatment of chronic venous disease in Thai patients. Vasc Health Risk Manag 2022;18:667–76.
- Aloweni F, Uthaman T, Agus N, Xian T, Maniya, Yuh A, Tec C. The cost of venous leg ulcers in a Singapore tertiary hospital: an explorative study. Wound Prac Res 2022;30(2):75–81.
- Smith E, McGuiness W. Managing venous leg ulcers in the community: personal financial cost to sufferers. Wound Prac Res 2010;18(3):134–9.
- Bui U, Tehan P, Barakat-Johnson M, Carville C, Haelser E, Lazzarini P, Twigg S, Weller C, Finlayson K. A scoping review of research in chronic wounds: protocol. Wound Prac Res 2021;29(4):234–7.
- Armstrong M, Mullins C, Gronseth G, Gagliardi A. Recommendations for patient engagement in guideline development panels: a qualitative focus group study of guideline-naïve patients. PLoS One 2017;12(3):e0174329.
- National Health and Medical Research Council (NHMRC). Statement on consumer and community involvement in health and medical research; 2016 [cited 2023 Jun]. Available from: https://www.nhmrc.gov.au/_files_nhmrc/file/publications/16298_nhmrc_-_statement_on_consumer_and_community_involvement_in_health_and_medical_research-accessible.pdf.
- Patient-Centered Outcomes Research Institute (PCORI). PCORI methodology standards; 2015 [cited 2023 Jun]. Available from: https://www.pcori.org/research-results/about-our-research/research-methodology/pcori-methodology-standards
- Qaseem A, Forland F, Macbeth F, Ollenschlager G, Phillips SM, van der Wees P, et al. Guidelines International Network: toward international standards for clinical practice guidelines. Ann Intern Med 2012;156(7):525–31.
- National Health and Medical Research Council (NHMRC). Guidelines for guidelines: forming the questions; 2019 [cited 2023 Jun]. Available from: https://www.nhmrc.gov.au/guidelinesforguidelines/develop/forming-questions
- Schünemann H, Brozek J, Guyatt G, Oxman A, editors. Overview of the GRADE approach; 2013 [cited 2023 Jun]. In: Handbook for grading the quality of evidence and the strength of recommendations using the GRADE approach. Available from: https://gdt.gradepro.org/app/handbook/handbook.html
- Légaré F, Boivin A, van der Weijden T, Pakenham C, Burgers J, Légaré J, Sylvie St-Jacques S, Gagnon S. Patient and public involvement in clinical practice guidelines: a knowledge synthesis of existing programs. Med Decis Mak 2011;31(6):E45–74.
- The AGREE Collaboration Writing Group, Cluzeau F, Burgers J, Brouwers M, Grol R, Mäkelä M, Littlejohns P, Grimshaw J, Hunt C. Development and validation of an international appraisal instrument for assessing the quality of clinical practice guidelines: the AGREE project. Qual Saf Health Care 2003;12(1):18–23.
- Eccles M, Grimshaw J, Shekelle P, Schünemann H, Woolf S. Developing clinical practice guidelines: target audiences, identifying topics for guidelines, guideline group composition and functioning and conflicts of interest. Implement Sci 2012;7:60.
- Prinsen C, Vohra S, Rose M, King-Jones S, Ishaque S, Bhaloo Z, Adams D, Terwee C. Core Outcome Measures in Effectiveness Trials (COMET) initiative: protocol for an international Delphi study to achieve consensus on how to select outcome measurement instruments for outcomes included in a ‘core outcome set’. Trials 2014;15(1):247.
- Webbe J, Sinha I, Gale C. Core outcome sets. Arch Dis Child Educ Pract Ed 2018;103(3):163–6.
- Schünemann HJ, Brozek J, Guyatt GH, Oxman AD, editors. Handbook for grading the quality of evidence and the strength of recommendations using the GRADE approach. Available from: https://gdt.gradepro.org/app/handbook/handbook.html; 2013 [cited 2023 Jun].
- McMaster University, Evidence Prime Inc. GRADEPro GDT. https://www.gradepro.org/: GRADEPro GDT; 2021 [Accessed June 2023].
- Schünemann HJ, Brozek J, Guyatt GH, Oxman AD, editors. Selecting and rating the importance of outcomes; 2013 [cited 2023 Jun]. In: Handbook for grading the quality of evidence and the strength of recommendations using the GRADE approach. Available from: https://gdt.gradepro.org/app/handbook/handbook.html
- National Health and Medical Research Council (NHMRC). Procedures and requirements for meeting the 2011 NHMRC standard for clinical practice guidelines. Canberra: NHMRC; 2011.
- Manatu Hauora Ministry of Health. Te Whare Tapa Whā Māori health model; 2021 [cited 2023 Jun]. Available from: https://www.health.govt.nz/system/files/documents/pages/maori_health_model_tewhare.pdf.
- Health Promotion Forum of New Zealand. Pacific health models; 2022 [cited 2023 Jun]. Available from: https://hpfnz.org.nz/pacific-health-promotion/pacific-health-models
- Alonso-Coello P, Schünemann H, Moberg J, Brignardello-Petersen R, Akl E, Davoli M, Treweek S, Mustafa R, Rada G, Rosenbaum S, Morelli A, Guyatt G, Oxman A, GRADE Working Group. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 1: Introduction. BMJ 2016;353:i2016.
- Alonso-Coello P, Oxman A, Moberg J, Brignardello-Petersen R, Akl E, Davoli M, Treweek S, Mustafa R, Vandvik P, Meerpohl J, Guyatt G, Schünemann H, GRADE Working Group. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 2: Clinical practice guidelines. BMJ 2016;353:i2089.
- Māori Policy Unit. Engaging with Māori: a guide for staff of the Bay of Plenty Regional Council; 2011 [cited 2023 Jun]. Available from: https://www.boprc.govt.nz/media/717746/engagement-toolkit.pdf.
- Althubaiti A. Information bias in health research: definition, pitfalls, and adjustment methods. J Multidiscip Health 2016;9(1):211–17.



