Volume 31 Number 4
Required wound care content for nursing curricula in Australia: a Delphi study
Holly Clegg, Catherine Fetherston, Ruth Wei
Keywords Wound care, education, nursing students, undergraduate nursing curricula
For referencing Clegg H, Fetherston C & Wei R. Required wound care content for nursing curricula in Australia: a Delphi study. Wound Practice and Research 2023; 31(4):190-196.
DOI
10.33235/wpr.31.4.190-196
Submitted 8 August 2023
Accepted 22 September 2023
Abstract
Background Insufficient wound care knowledge in nursing students affects confidence and competence. Scarce research on wound care content and delivery leads to curriculum disparities. Integrating essential content is vital for improved wound care education.
Aims This study aimed to determine Australian wound care curriculum content for a 3-year Bachelor of Nursing program and identify the optimal year for introducing each topic, as recognised by experts.
Methodology A three-round Delphi survey involved 17 wound care experts in Australia. The survey used the Standards for wound prevention and management to identify 74 wound care topics within the three categories of anatomy and physiology (A & P), assessment and treatment/therapies, requiring >70% agreement on the year of introduction for each topic.
Results The Delphi process established consensus on the initial introduction year for 65 of the 74 wound care topics. A total of 19 topics garnered consensus exceeding 70% in the first year, 19 in the second year, 15 in the third year, and 12 for postgraduate study. Expert consensus enabled a progressive development of knowledge and skills in wound theory, assessment, care planning, patient education and prevention over the 3-year program.
Conclusion The gathering of this data has allowed for conceptual scaffolding of these topics according to the stage at which wound care topics are recommended for introduction into nursing curricula.
Introduction
The integument is the largest organ in the body and is critical in maintaining physiological homeostasis and protecting against injury, infection, fluid imbalance and thermal dysregulation1. The incidence of compromise, or breakdown, of the skin’s integrity is increasing alongside the prevalence of obesity and chronic disease. This compromise presents in a range of wound presentations such as leg ulcers, pressure injuries and neuropathic ulcers (sometimes commonly referred to as a diabetic ulcer)2. Chronic wounds are a particular concern in healthcare globally, with a prevalence of approximately 2.2 per 1,000 people3. Consequently, wound care is a critical aspect of nursing practice, requiring nurses to possess knowledge and skills that will enable safe and effective care to individuals with wounds.
However, there is evidence suggesting a lack of consistency in wound care education within undergraduate nursing programs4 which can impact the confidence and competence of graduating nursing students. Potential contributing factors to this lack of preparedness have been related in the literature to the inconsistencies in the education delivered in undergraduate nursing programs5–8, the time allocated to wound care education7,9, and that wound care is often covered in the first year but not progressed throughout the course5,6. These issues have been further evidenced from the nursing students’ perspective, where it was identified that nursing students felt they received insufficient and inadequate education on some wound care topics, including anatomy and physiology (A & P), pressure injury prevention, wound assessments, dressing selection and wound infection8,10.
Upon graduation, registered nurses (RNs) are expected to possess a certain level of wound care competence. However, the specific wound care knowledge and skills that should be covered during undergraduate nursing programs remains unclear. Nursing curricula already encompass a wide range of topics and skills, posing a challenge for academics to allocate sufficient time and attention to wound care education4. Moreover, there is a dearth of literature and support to guide nursing academics in determining the essential content necessary for graduates to deliver safe and quality wound care11.
Given the challenges, it is imperative to explore and establish consensus on the necessary wound care content to be included in nursing programs. This will not only provide guidance to nursing academics but also ensure consistency across programs, enabling graduates to acquire the competence needed for proficient wound care practice. As key publications have highlighted the importance of standardised wound care education and the need to address any inconsistencies in curricula4,12–15, this study will explore expert opinion on the desired wound care content for undergraduate nursing curricula.
Methods
The study’s aim was to assist in improving the quality and consistency of wound care nursing education in Australia prior to graduation by using a Delphi technique to seek expert consensus on what wound care content should be delivered, and at what stage, of a 3-year entry to practice RN program. The Delphi technique involves a group facilitation technique that seeks to “obtain consensus on the opinions of ‘experts’ through a series of structured questionnaires (commonly referred to as rounds)”16,17 that enable the collection and condensing of knowledge. The benefits of the Delphi technique for this study are that it enables a combination of academic expertise and clinical practitioners’ perspectives, knowledge and experiences related to wound care education at undergraduate level18.
Delphi process
The Delphi process used in this study comprised three rounds, and the wound care topics used in the survey were constructed using the evidence-based Standards for wound prevention and management19. In round one, participants were asked to consider 73 wound care topics and identify which year they should be first introduced. Additionally, participants were encouraged to comment on why they had made this selection. In rounds two and three, participants were provided an anonymised summary of the previous round’s results and, on questions where 70% consensus had not been reached, they were asked to reconsider their selections in light of the other participants’ responses20,21.
Participants
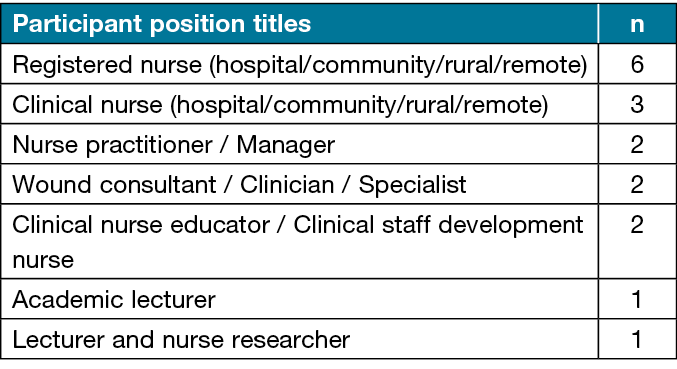
A total of 17 wound care experts, all RNs with an average of 18 years’ experience in various roles in the field of wound care, participated in all three rounds of the Delphi study (Table 1). The participants were recruited using a purposive sampling approach from diverse clinical and education settings – Western Australia (n=6), Queensland (n=2), New South Wales (n=1), South Australia (n=2), Victoria (n=5) and Australian Capital Territory (n=1) – and represented hospitals, general practice, aged care, clinics, community, rural and remote areas and the university sector. Inclusion criteria for participants required a RN qualification, a minimum of 3 years of hands-on experience in wound care, and current engagement in a clinical or educational role involving wound care. Participants were purposefully selected and approached through outreach to wound care organisations as well as connections on the professional networking platform, LinkedIn.
Table 1. Range of participants’ roles
Questionnaire development
The questionnaire was developed using the evidence-based Standards for wound prevention and management19 to identify the 73 (which then became 74 after round one) wound care topics to present to the Delphi panel (Figure 1). The questionnaire also included a section collecting demographic data about the participant’s job role, geographic area and years of experience. The topics were organised into three categories – A & P, assessment and treatment/therapies – to provide structure to the questionnaire. Each participant was provided with four options to indicate their preferred year for the delivery of each topic (first year, second year, third year and post-grad), accompanied by an additional option to express the strength of their decision. The ranking of the strength of their decision was only incorporated as a tool to assist participants to reflect on their decision if the question went back for a second round.
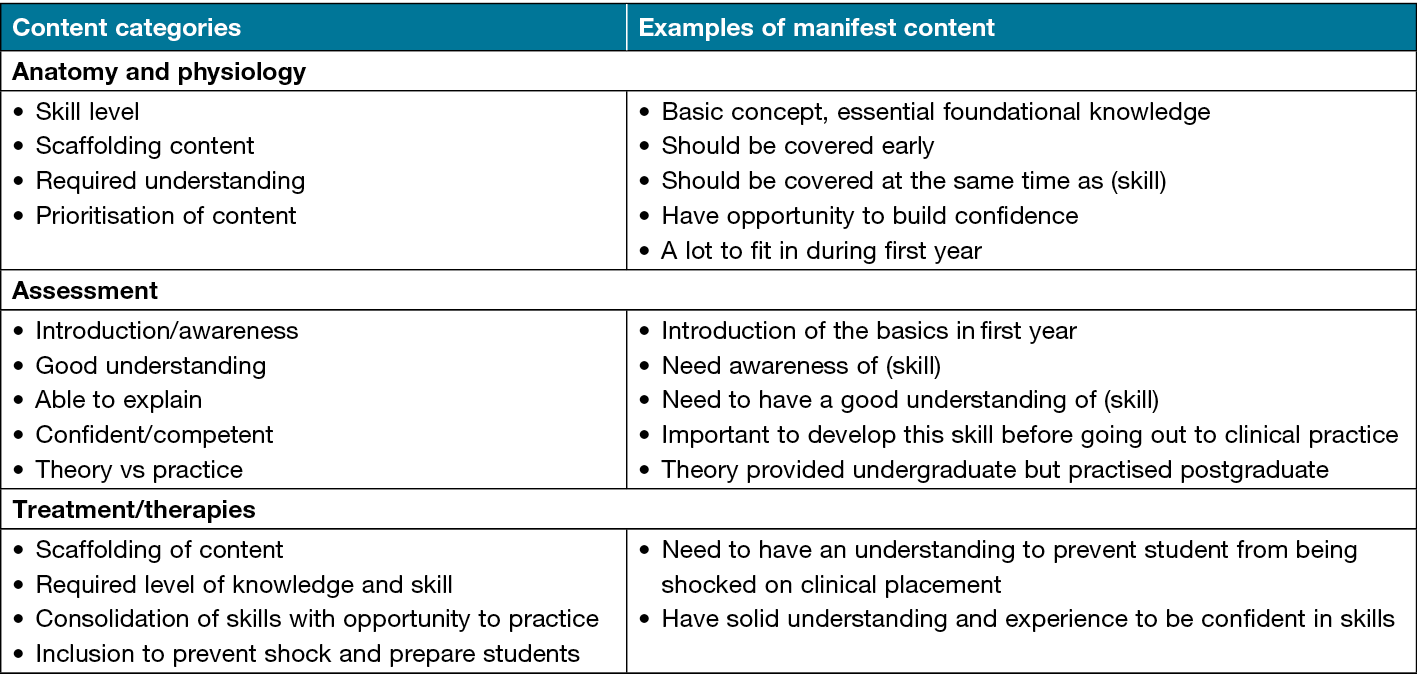
Figure 1. Content categories and variable labels with associated participants’ comments according to theme
Furthermore, participants were offered the opportunity to provide comments regarding their choices for each topic. Based on the comments and feedback received from the first round, three changes were made to the topics in the second round – stoma wound care was amended to focus on strategies to manage skin moisture and prevent skin damage in individuals requiring care of a stoma or nephrostomy; negative pressure wound therapy (NPWT) was moved from one topic to another due to its increasing prevalence in practice; and an additional topic on preventative therapies, including compression stockings for venous leg ulcers, exercise, leg elevation and skin care regimes, was added. There was no change required after the second round.
Data analysis
The quantitative data obtained from the questionnaire underwent analysis using descriptive statistics in SPPS© IBM Corp, Armonk, NY22. Results were then represented as percentages and presented in a table to provide participants with feedback on the level of consensus and how strongly participants felt about their choices. This feedback table served as a valuable resource for participants to review and consider when making subsequent selections. Moreover, to support their selections or propose additional topics, participants were invited to share their thoughts and insights on each topic, both throughout the survey and at its conclusion.
The qualitative data obtained through their comments underwent content analysis to extract meaningful insights and perspectives. The process of content analysis used in this study considered both the participant and context whilst sorting the text into groups of related categories23. This method of content analysis is referred to as manifest content, which describes what is occurring on the surface and is concerned with data that is easily observable within the text24. During the Delphi process of this study, content analysis on participants’ comments was performed at the end of each round and then manifest content was summarised and included in a separate column in the feedback table to be sent to participants. Content categories were then developed for each of the three sections in the survey, supported by verbatim examples of the manifest content.
Results
In the initial phase, a survey comprising 73 wound care topics was administered to the Delphi panel. A consensus exceeding 70% agreement was achieved for five topics during the first round – simple wounds (88% agreement in the first year), standard aseptic technique (77% agreement in the first year), methods for cleansing simple wounds (82% agreement in the first year), methods for cleansing complex wounds (71% agreement in the second year), and hand hygiene and personal protective equipment (PPE) for wound care (94% agreement in the first year). These specific topics were excluded from subsequent rounds. The analysis of content highlighted the importance of early exposure to fundamental wound care knowledge, the value of practical experience, and the relevance of certain topics across different stages of nursing education. An additional topic concerning preventive therapies, encompassing compression stockings for venous leg ulcers, exercise, leg elevation and skin care routines, was introduced, resulting in a total of 74 wound care topics.
In the second round, consensus above 70% agreement regarding the appropriate year level for topic inclusion was reached for 21 out of 68 topics. These subjects were retained, while the remaining topics underwent further evaluation by participants to ascertain consensus levels. The content analysis during the second round emphasised the significance of early introduction, the necessity for familiarity, and the intricacies of certain topics.
During the third round, 47 topics were considered, with 38 of them obtaining consensus exceeding 70%, leaving nine topics with divergent responses. Collectively across the three rounds, a total of 64 topics achieved consensus regarding the year in which they should be introduced to nursing students. Of these, 43 topics garnered consensus exceeding 80%, with two subjects gaining unanimous agreement. Feedback from participants in the third round underscored the pertinence of specific topics to particular nursing placements, the ethical and legal considerations of wound photography, and the importance of understanding wound assessment and management to prevent complications.
All rounds achieved a 100% participation rate from the panel members. With a final tally of 74 wound care topics presented to the Delphi panel, 19 topics garnered consensus exceeding 70% in the first year, 19 in the second year, 15 in the third year, and 12 for postgraduate study. The nine topics lacking 70% consensus were allocated to the year level with the majority agreement (ranging from 53% to 65%), acknowledging the possibility that these topics could be considered outside this specific year level. Moreover, six overarching educational concepts emerged when exploring the content of wound care topics for conceptual patterns – wound theory (A & P, pathophysiology and pharmacology), physical assessment, psychosocial assessment, wound care skills, wound care planning, patient education and wound prevention.
An overview of all participant comments, categorised according to the questionnaire’s three themes (A & P, assessments and treatments/therapies), is presented in Figure 1. The wound care topics were organised based on the consensus reached by the participants, mapping out the agreed scaffolding of wound care content across different years of nursing education (Figure 2). Nine topics did not reach a 70% consensus and were placed in the year with the majority agreement, with acknowledgement that they could also be considered outside that year level. These topics are indicated in italics in Figure 2.
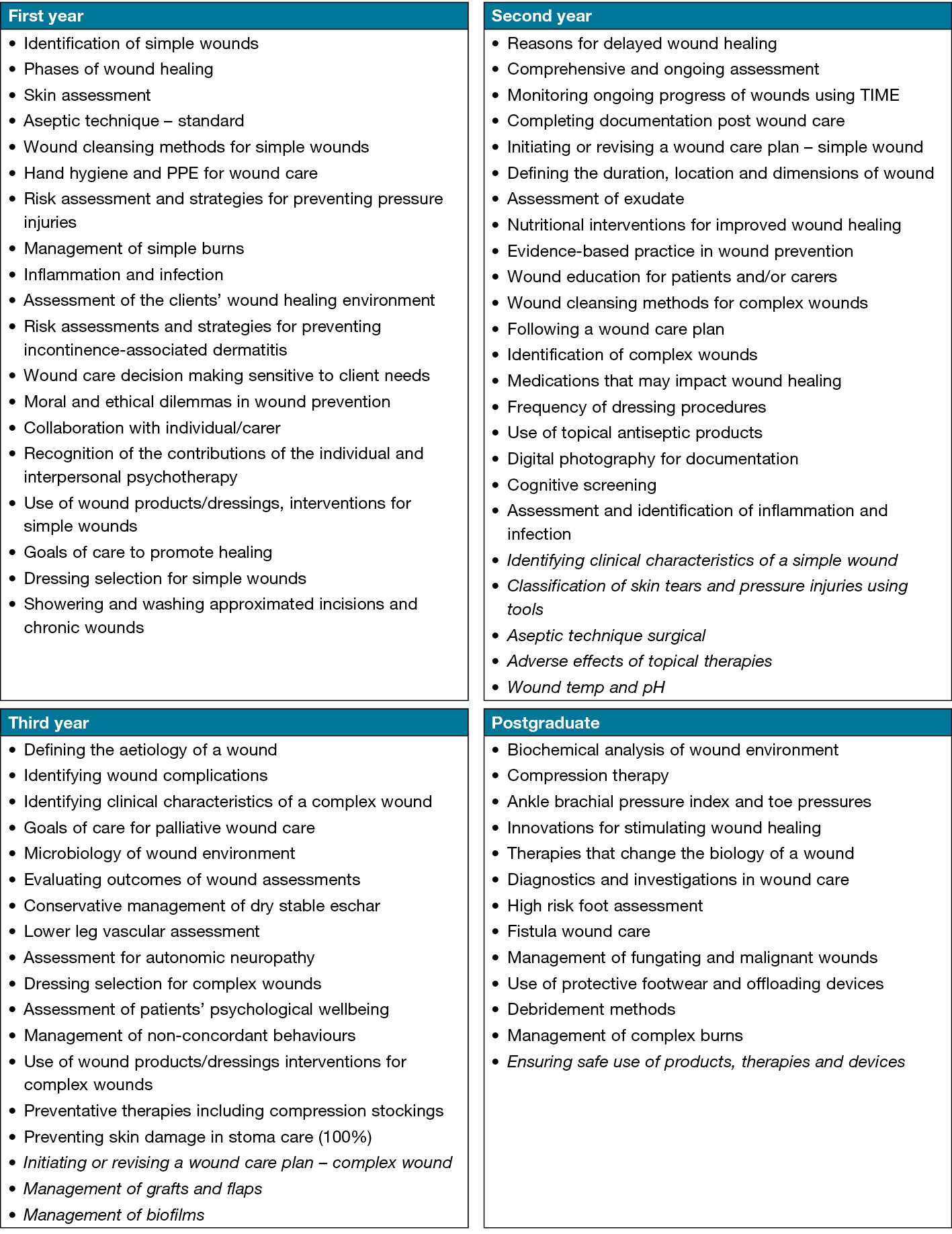
Figure 2. Stage at which wound care topics are recommended for introduction into nursing curricula.
Topics that did not meet 70% consensus are show in italics; these topics were placed in the year level with the majority consensus (59–65%)
Discussion
As this is the first robust Australian study to explore wound care content in undergraduate nursing curricula, it is not possible to make any direct comparisons of the current study’s findings. Previous studies have consistently pointed to the inadequacy of nursing education in adequately preparing students for the complexities of wound care9,25,26. They have highlighted the challenges faced by students and graduates in acquiring the necessary knowledge and skills in this critical domain. The findings of this study align with these concerns but delve deeper into identifying specific foundational skills and theoretical knowledge that are essential for nursing students.
There was a clear early consensus from the experts in the first Delphi round that focused exclusively on the first year skills required to lay the groundwork for later development. These included identification of simple wounds, standard aseptic technique, wound cleansing methods for simple wounds, hand hygiene and PPE for wound care. The experts commented on the need for students to have an early understanding of these basics and the opportunity to frequently practise these skills to build confidence. Although initially, the first round agreement for first year topics focused primarily on basic skills acquisition as identified above, in later rounds, the experts reached consensus on more theory and prevention-focused topics such as phases of wound healing, inflammation and infection, skin assessment, simple wound care products and prevention of pressure injuries. Comments were also made regarding the need for an early and concurrent introduction of wound care-related anatomy, physiology and pathophysiology with linking of the skill being learned to its theoretical underpinnings.
These findings are supported by evidence that suggests appropriate management of different wound types requires a good understanding of the A & P relating to the skin layers and wound healing4. However, there are variances in how A & P is currently delivered in nursing programs, with some courses providing stand-alone multi-disciplinary A & P units in the first year, while others offer units that integrate nursing care or ‘nursify’ basic A & P throughout the curriculum27. This raises the importance of aligning wound care education with the delivery of A & P content to ensure a comprehensive understanding of the topic.
The experts also highlighted the need for nursing students to develop critical thinking skills related to wound care. This includes the ability to assess wounds, understand wound aetiology, and make appropriate clinical judgments regarding wound management. Integration of critical thinking exercises and case studies into the curriculum was suggested to facilitate the development of these skills. Additionally, the experts recognised the importance of interdisciplinary collaboration in wound care. They suggested that nursing students should be exposed to interprofessional education opportunities to enhance their understanding of the roles and contributions of different healthcare professionals in wound management. This aligns with the growing emphasis on interprofessional education in healthcare curricula to promote effective teamwork and patient-centred care28.
A holistic approach to wound care education should also extend to the involvement of professional standards, particularly as it has been highlighted that there are inconsistencies with how and when professional nursing standards are integrated into a nursing program29. First year nursing students typically learn about professional and safety standards in a professional nursing practice unit from a theory perspective29 so, again, it is essential these standards can be linked to the wound care context in the nursing units where skills are practised, enabling the students to view a person with a wound from a holistic and professional perspective.
Overall, the findings from this study underscore the need for a comprehensive and standardised approach to wound care education in nursing curricula. It is essential to ensure early exposure to foundational wound care knowledge and skills, integrate theoretical and practical aspects of wound care, provide opportunities for repeated practice and skill development, and promote critical thinking and interdisciplinary collaboration. By addressing these factors, nursing programs can better prepare students to deliver evidence-based and quality wound care in their future practice.
Limitations
This study did not determine whether the identified wound care topics should be taught as theory or practice, nor did it specify the amount of time to allocate to each. The study had a small number of participants, but it adhered to the recommended minimum of 10 participants for a Delphi study, achieving 17 participants across all three rounds. In addition, the inclusion of academic and clinical participants provided diverse expertise and geographical representation within Australia. It is important to note that our expert panel included more clinicians than academics, which could influence the perspectives and recommendations. While the composition of the panel reflects the real-world composition of wound care professionals, with clinicians offering practical insights and academics contributing educational expertise, the potential variation in emphasis between the two groups could impact curriculum design.
The findings are specific to the Australian context and may not be generalised to other countries. However, considering the need for standardised wound care knowledge internationally, the findings may have relevance in different countries. It is worth noting that conducting a fourth round of the survey could have led to further agreement on the topics with less than 70% consensus, but this was not possible within the time constrictions of the study.
Recommendations
In terms of education recommendations, it is suggested to implement a standardised wound care curriculum for RN entry to practice programs to ensure consistent knowledge and skills amongst graduates. The curriculum should introduce basic wound care content early in the first year and progressively cover more complex topics. Emphasis should be placed on holistic care, addressing patients’ health promotion needs. Pedagogical strategies such as case-based education can be employed to scaffold content and build complexity. Additionally, educators should have the flexibility to adapt the curriculum to meet the specific needs of their programs. Ongoing wound care education for graduate RNs is also essential to develop competencies in complex areas of care.
For further scholarship and research, it is recommended to develop wound care skill competencies for entry to practice RNs. Exploring innovative pedagogical tools like virtual reality can enhance wound care education and address resource limitations. Further research is needed to determine the delivery mode (theory or practice) and assessment methods for wound care topics. It would also be beneficial to prioritise wound care topics based on factors such as patient impact, prevalence and economic burden.
To bring about widespread transformation, we might explore the idea of advocating for updated accreditation standards related to graduate competencies. This could compel Bachelor of Nursing programs to align with these standards.
Conclusions
A total of 65 wound care topics were identified for inclusion in the undergraduate nursing curricula, with consensus achieved by a panel of wound care experts on which year these topics should be first introduced. These wound care topics include content that has been recommended as best practice in the Standards for wound prevention and management document19. The gathering of this data has allowed for conceptual scaffolding of these topics according to the educational stage at which wound care topics are recommended for introduction into nursing curricula. Reducing the inconsistencies in wound care education and improving the standards of knowledge and skills in graduate nurses is essential for the safe, effective and evidence-based care of individuals with wounds and ultimately improving wound healing outcomes.
Acknowledgements
We would like to acknowledge the participants that took part in this study and thank them for their time and invaluable contributions which were essential in making this research possible.
Conflict of interest
The authors have no conflict of interest to declare.
Ethics statement
Ethical approval was obtained from Murdoch University Human Research Ethics Committee (approval code: 2020/007) and informed consent was obtained from all participants prior to their participation in the Delphi survey.
Funding
The principal author received funding from the Wounds Australia Research Grant Scheme.
Authors contribution statement
The authors confirm contribution to the paper as follows: HC & CF completed study conception and design; HC, CF & RW developed the questionnaire; HC completed data collection; HC, CF & RW completed analysis and interpretation; HC completed the draft manuscript preparation; and CF & RW critical reviewed for revision of all aspects of the study and draft manuscript. All authors reviewed the results and approved the final version of the manuscript.
Author(s)
Holly Clegg*, Catherine Fetherston, Ruth Wei
Murdoch University, WA, Australia
*Corresponding author email h.clegg@murdoch.edu.au
References
- Mohamed SA, Hargest R. Surgical anatomy of the skin. Surgery 2022;40(1):1–7. doi:10.1016/j.mpsur.2021.11.021
- Jaul E, Barron J, Rosenzweig JP, Menczel J. An overview of co-morbidities and the development of pressure ulcers among older adults. BMC Geriatr 2018;18(1):305–305. doi:10.1186/s12877-018-0997-7
- Martinengo L, Olsson M, Bajpai R, Soljak M, Upton Z, Schmidtchen A, et al. Prevalence of chronic wounds in the general population: systematic review and meta-analysis of observational studies. Annals Epidemiol 2019;29:8–15. doi:10.1016/j.annepidem.2018.10.005
- Kielo E, Suhonen R, Salminen L, Stolt M. Competence areas for registered nurses and podiatrists in chronic wound care, and their role in wound care practice. J Clin Nurs 2019;28(21–22):4021–34. doi:10.1111/jocn.14991
- Abuleal SV. Wound care education for undergraduate nursing students. J Health Commun 2018;3(2:28):1–5. doi:10.4172/2472-1654.100138
- Holloway S, Probst S, Murphy S. Determining the current level of wound management education in the pre-registration nursing curricula. EWMA J 2018;9(2):83–87.
- Moore Z, Clarke E. A survey of the provision of education in wound management to undergraduate nursing students. EWMA J 2011;11(1).
- Zulkowski K, Capezuti E, Ayello EA, Sibbald G. Wound care content in undergraduate programs: we can do better. WCET J 2015;35(1):10–13.
- Ousey K, Stephenson J, Cook L, Kinsey L, Batt S. Final year student nurses’ experiences of wound care: an evaluation. Br J Community Nurs 2013;18(Sup3):S7–S16.
- Stephen-Haynes, J. Preregistration nurses’ views on the delivery of tissue viability. Br J Nurs 2013;22(Sup20), S18-S23. doi:10.12968/bjon.2013.22.Sup20.S18
- Clegg H. Required wound care content for nursing curricula in Australia: A Delphi study [Masters by research]. Perth (Australia): Murdoch University; 2022.
- Ferreira A, Rigotti M, Barcelos L, Simão C, Ferreira D, Gonçalves R. Knowledge and practice of nurses about care for patients with wounds. Rev Pesquisa, Cuidado Fundament 2014;6(3):1178–90.
- Kielo-Viljamaa E, Suhonen R, Ahtiala M, Kolari T, Katajisto J, Salminen L, et al. The development and testing of the C/WoundComp instrument for assessing chronic wound-care competence in student nurses and podiatrists. Int Wound J 2021;18(1):62–78. doi:10.1111/iwj.13495
- Norman RE, Gibb M, Dyer A, Prentice J, Yelland S, Cheng Q, et al. Improved wound management at lower cost: a sensible goal for Australia: Int Wound J 2016;13(3):303–16. doi:10.1111/iwj.12538
- Welsh L. Wound care evidence, knowledge and education amongst nurses: a semi-systematic literature review. Int Wound J 2018;15(1):53–61. doi:10.1111/iwj.12822
- Hasson F, Keeney S, McKenna H. Research guidelines for the Delphi survey technique. J Adv Nurs 2000;32(4):1008–1015.
- Linstone HA, Turoff M. The Delphi method: techniques and applications. Addison-Wesley Publishing Company; 1976.
- Trevelyan EG, Robinson PN. Delphi methodology in health research: how to do it? Eur J Integr Med 2015;7(4):423–428.
- Wounds Australia. Standards for wound prevention and management. Wounds Australia; 2016.
- Chang AM, Gardner GE, Duffield C, Ramis MA. A Delphi study to validate an advanced practice nursing tool. J Adv Nurs 2010;66(10):2320–30. doi:10.1111/j.1365-2648.2010.05367.x
- McIlrath C, Keeney S, McKenna H, McLaughlin D. Benchmarks for effective primary care-based nursing services for adults with depression: a Delphi study. J Adv Nurs 2010;66(2):269–81. doi:10.1111/j.1365-2648.2009.05140.x
- IBM Corp. IBM SPSS Statistics for Windows [Internet]. Armonk, NY: IBM Corp; 2020
- Graneheim UH, Lindgren B-M, Lundman B. Methodological challenges in qualitative content analysis: a discussion paper. Nurse Ed Today 2017; 56, 29–34. doi:10.1016/j.nedt.2017.06.002
- Kleinheksel AJ, Rockich-Winston N, Tawfik H, Wyatt TR. Demystifying content analysis. Am J Pharmaceut Ed 2020; 84(1), 127–137. doi:10.5688/ajpe7113
- Guerra DS. Undergraduate nursing students’ experiences with learning about wound care. ProQuest Dissertations Publishing; 2016.
- Redmond C, Davies C, Cornally D, Adam E, Daly O, Fegan M, et al. Using reusable learning objects (RLOs) in wound care education: undergraduate student nurse’s evaluation of their learning gain. Nurse Ed Today 2018;60:3–10. doi:10.1016/j.nedt.2017.09.014
- Mortimer-Jones S, Fetherston C. The nursification of a bioscience unit and its impact on student satisfaction and learning in an undergraduate nursing degree. Nurse Ed Today 2018;64:1–4. doi:10.1016/j.nedt.2018.02.006
- Pardue KT. A framework for the design, implementation, and evaluation of interprofessional education. Nurse Ed 2015;40(1):10–5.
- Krautscheid LC. Teaching professional nursing accountability: a phenomenological investigation of faculty experiences. ProQuest Dissertations Publishing; 2012. https://go.exlibris.link/cVbv8XYt



