Volume 32 Number 1
The anatomy, physiology and function of all skin layers and the impact of ageing on the skin
Zahra Lotfollahi
Keywords dermal-epidermal junction, keratinocytes, the integumentary system
For referencing Lotfollahi Z. The anatomy, physiology and function of all skin layers and the impact of ageing on the skin. Wound Practice and Research 2024;32(1):6-10.
DOI
10.33235/wpr.32.1.6-10.
Submitted 7 March 2024
Accepted 13 March 2024
Abstract
Comprehensively understanding the structure, physiology and function of the skin can help us identify skin conditions, comprehend wound healing mechanisms and explore new prevention and treatment strategies for skin disroders. This short review describes the structure, composition and different cell types that make up the skin, and discusses the functions of the skin and the impact of ageing on skin structure.
Introduction
Skin, also known as the integumetary system, is the largest organ in our body, covering the entire external surface; measuring up to 2m2 and weighing approximately 4.5−5kg in an average adult (or about 12−15% of total adult body weight).1 Skin is the first physical barrier protecting us from the external environment. Skin is made of three layers: the outermost layer the epidermis, the structure below it, the dermis and the structure below the dermis known as the subcutaneous tissue.2 The anatomy, structure, and composition of each of these layers is varied, depending on the function and role of that layer.3 The exisiting knowlegde of skin anatomy and function are well known and covered in the literature, however, in this review we also focus on the impact of ageing on skin structure, as well as revising the anatomy and structure of the skin, the cellular composition of it and skin’s main functions.
Epidermis
The epidermis has approximately 0.5−1.5mm thickness (depending on the body part: 0.5mm on the eyelids to 1.5mm on the palm of the hands and soles of the feet) and is avascular; meaning it doesn’t have any blood vessels and, as shown in Figure 1(a), is composed of keratinised, stratified squamous cells.4,5 The skin areas on the palms, soles and fingerprints are known as the ‘thick skin’ and the skin on other areas of the body is known as the ‘thin skin’.5 In thin skin, the epidermis is composed of four epithelial layers: the stratum corneum; stratum granulosum; stratum spinosum or prickle cell layer; and stratum germinativum or stratum basale as shown in Figure 1(b). In thick skin, the epidermis is composed of five epithelial layers, as shown in Figure 1(c), including the stratum corneum; stratum lucidum; stratum granulosum; stratum spinosum or prickle cell layer; and stratum germinativum or stratum basale.6 The naming of each of these layers reflects their anatomical structure which is explored in the following paragraphs. The epidermis is mainly composed of keratinocyte and melanocytes with fewer Langerhans and Merkel cells.7
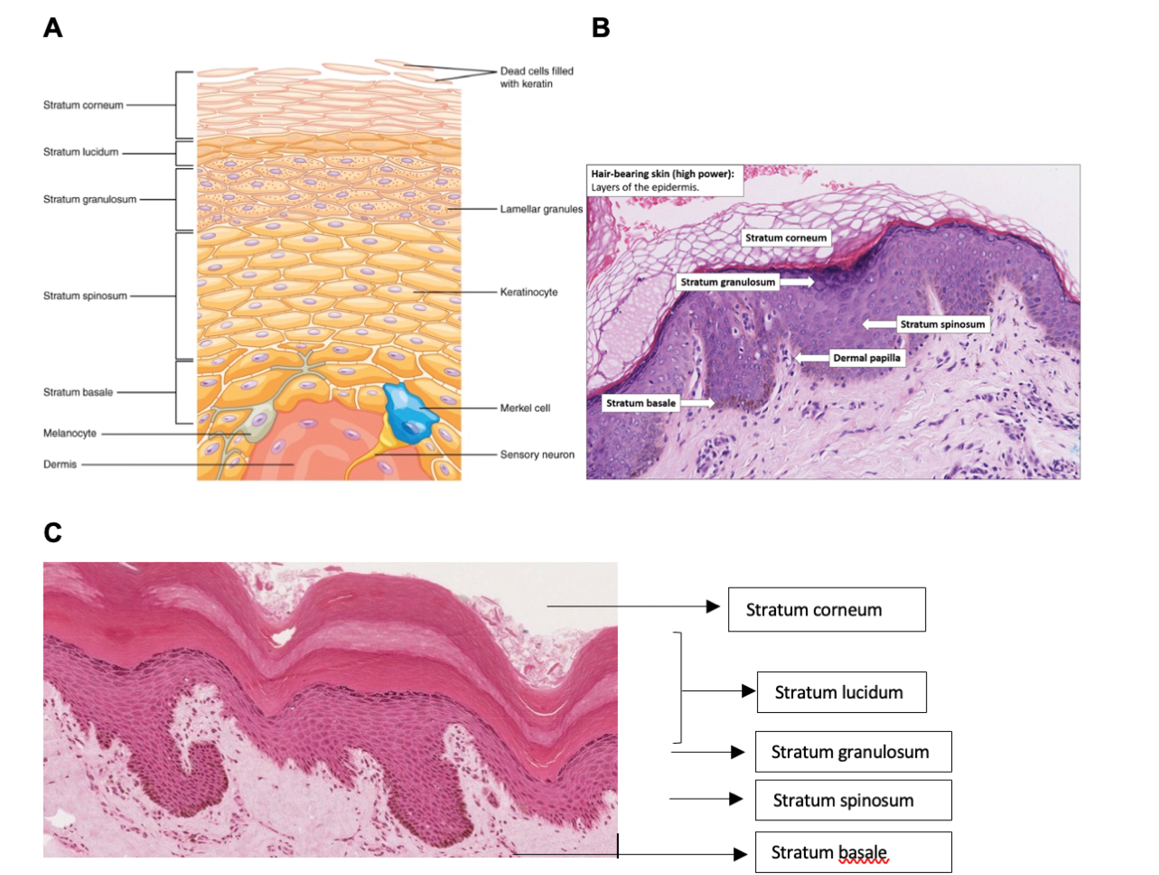
Figure 1. (a) Schematic presentation of the epidermis layer of the skin. Image courtesy of Biga et al4 (b) Histology image of skin. Image courtesy of National University of Singapore, School of Medicine8 (c) Histology of skin with stratum lucidum, image courtesy of Jamie Champan.
Stratum corneum
This is the uppermost and thickest section of the epidermis consisting of 25−30 layers. See Figure 1(b). The main cell type in this area is large and flat keratinocytes with no nucleus. The keratin and other structural proteins in these cells are tightly crossed and form rigid and impermeable layer. The pH for this area is between 4 to 6.5 and therefore anything which alters this pH can lead to skin issues, such as bacterial or fungal infections.1,9,10 This layer is continuously renewing and the entire layer is replaced by new keratinocytes during a period of four weeks.4 The turnover rate of keratinocytes is reduced in older skin, with the time taken to migrate from the basal layer to the epidermis increasing by up to 50%.11 In addition, this layer thickens with ageing, in a process believed to be related to body’s attempt to protect itself from UV radiation over time.11
Stratum lucidum
This section consists of 2−3 layers, see Figure 1(c), and is the ‘clear’ layer of the skin, only found in thick-skin areas of the body, such as palms, soles and fingerprints. The transparent nature of this layer is due to presence of transparent keratinocytes.2
Stratum granulusum (granular layer)
As the name suggests, this section (3−5 cell layers) consists of granular cells which differentiated from the spinous layer. These granular cells consist of either keratohyalin or lamellar granules: The keratohyalin granules contain keratin precursors that eventually aggregate, cross link and form bundles. The lamellar granules contain glycolipids which act as glue to keep the cells together and create hydrophobic properties.2 The flattened diamond shaped cells in this section lie parallel to the basement membrane, see Figure 1(b) B) and continue to differentiate and express molecules which help them mature to epidermal cells at the stratum corneum layer.
Stratum spinosum (prickle/spinous layer)
This section (8−10 cell layers) thick is immediately above the basal layer and consists of polyhedral-shaped keratinocytes with cytoplasmic processes, sometimes referred to as “spines”, which extend outwards and contact the neighbouring cells by desmosomes, see Figure 1(b).12 The keratinocytes in this section continue to differentiate and make the cells in the stratum corneum. There are also dendritic cells in this layer.2 As a person ages, the stratum spinosum becomes thinner.11
Stratum basale/stratum germinativum (basal layer)
This layer is the deepest layer of the epidermis and consists of a single layer of undifferentiated keratinocytes also known as basal cells, see Figure1(b).12 A basal cell is a cuboidal- shaped stem cell which is a precursor to a keratinocyte.4 The cells in this layer are meiotically active, meaning that they are constantly replenishing and producing new keratinocytes.1,9,13 Melanocytes are also scattered in this layer which are responsible for skin colour and provide UV protection.2,9 This layer is separated from the dermis by a structure called the basement membrane (basal lamina) and attached to the basement membrane by hemidesmosomes.2
The basement membrane
The basement membrane separates the dermis from the epidermis and is located underneath the epidermis.9 Presence of extracellular matrix molecules on both sides of the basement membrane create a ‘sticky’ environment providing a tight junction between the epidermis and dermis.14 With age, the basement membrane atrophies, flattening the dermal-epidermal junction, reducing the epidermal adhesion as the protein compostion of the dermal-epidermal layer changes resulting in less adhesiveness between the dermis and epidermis.11
Dermis
The dermis is considered the “core” of the integumentary system (dermis-= skin), as distinct from the epidermis (epi-= upon or over) and hypodermis (hypo-= below).4
The dermis is the thicker structure containing vessels and nerves, nourishing, and supporting the epidermis.10 The dermis itself is divided into two regions: the superficial papillary region and the deep reticular region (Figure 2). The superficial papillary region is the thinner upper layer, composed of loose connective tissue that contacts the epidermis connective tissue. It consists of extracellular matrix and fibroblasts. Fibroblasts also secrete fibronectin and hyaluronic acid; two major components of the extracellular matrix which plays a role in wound healing. The superficial dermis also contains blood vessels, lymphatics, epithelial cells, small muscles and neurons.10 The deep reticular dermis is the deeper layer, which is thicker, less cellular and consists of dense connective tissue.2 This area contains large network of blood vessels and collagen fibres providing tensile strength to the skin. Fibro-elastic connective tissue, mainly composed of collagen, is contained in this layer as well as fibroblasts. With ageing, the number of cells responsible for extracellular matrix deposition and tissue remodelling in the dermis decrease, as well as less organised collagen and elastin deposition, resulting in weaker and less elastic skin.15
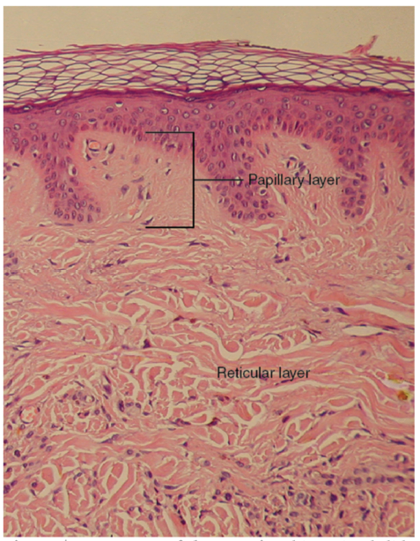
Figure 2. Histology of the skin showing the different sections
of the dermis: the papillary layer and the reticular layer.
Image courtesy of Biga et al4
.
Hypodermis
This layer, also known as the subcutaneous layer or superficial fascia, lies beneath the dermis and anchors the dermis part of the skin to the underlying fascia surrounding the muscle or bone.16 The hypodermis is mainly composed of adipose tissue with the role of fat storage and provides cushioning and insulation.4 The hypodermis also contains well-vascularised, loose and areolar connective tissue.4 It is suggested that the skin flexibility and free movement over underlying structures is mainly due to the loose arrangement of collagen and elastic fibres.16 The fat storage and the cushioning function of the hypodermis decreases with the ageing process.11
Cell types in the skin
Keratinocytes
The epidermis is almost entirely made of keratinocytes (approximately 95% of epidermal cells) that originate from the deepest layer of the epidermis, the stratum basale.4 The journey of the keratinocytes begins in the stratum basale as undifferentiated keratinocytes. These cells start to differentiate to polyhedral shaped keratinocytes as they migrate up to the stratum spinosum. In the stratum granulosum, the keratinocytes contain granules with structural proteins, such as trichohyalin, as illustrated in Figure 1(b) and become flat.9 One of the main functions of the skin is to work as a barrier, to prevent the loss of water from our body and the entrance of irritants into our body. This function is heavily reliant on the water insoluble properties of keratin, the main component of keratinocytes. As the name suggests, keratinocytes produce and store keratin and are responsible for the hydrophobic property of the epidermis (epidermal water barrier) by secreting lipids.2 Keratinocytes also regulate calcium absorption via the activation of the cholesterol precursors by UVB light to form vitamin D.2
Langerhans’ cells
Langerhans cells originate from the bone marrow, migrate to and localise in the stratum basale region of the epidermis. They are also present sporadically in the stratum spinosum section of the epidermis, see Figure 1(a).5 These cells act as the first line of defence to fight invading microorganisms with their phagocytotic ability.2 With ageing, there is a decrease in Langerhans cells, which are involved in immune response, therefore reducing the skin’s immune function in the elderly.10
Melanocytes
Melanocytes are found in the deepest layer of the epidermis (stratum basale) and contain melanin, the black-brown pigment with high molecular weight which provides the pigmentation of the skin, hair and eyes.4,5 The other function of melanin is to provide protection from UV light by absorbing it and minimising the release of free radicals in the basal layer.5 There is also reduction in the number of melanocytes, which are also involved in immune function, in ageing skin 10
Merkel cells
Merkel cells are found in small numbers in the basal layer of the epidermis in both the hairless and hairy sections of the skin, see Figure 1(a).16,17 They are connected to the surrounding keratinocytes by proteins called desmosomes and play a role in sensation by being slowly adapting mechanoreceptors.17 The function of these cells is still not fully understood18 but some studies suggest that they attract nerve endings into the epidermis and stimulate keratinocyte growth.16
Function of the skin
Protection
The primary function of the skin is to act as a physical barrier against the external environment such as microoragnisms and foreign matter and protect our internal organs.4,19 As mentioned in the previous sections, specific resident cells in the skin (such as Langerhan cells), melanocytes and circulating cells (such as neutrophils and macrophages) are involved in the immunity of the skin, as part of its protective function.4 Ageing causes decreases in the number and function of all these cell types, therefore compromising the protection function of the skin.11 As mentioned previously, the uppermost layer of the epidermis is made of layers of dead keratin and glycolipids, which can withstand the wear and tear of the environment.19 Physical cushioning is provided by the hypodermis section of the skin through adipose storage and protective films secreted by the glands.19 Skin also acts as a chemical and biological barrier.4 With ageing, this physical cushioning is reduced, as the subcutanous tissue has less adispose storage and becomes thinner, and the epidermal layer also thins.11
Sensation
To protect our body from hazardous external environment, the skin has developed an effective sensory system to respond to different stimuli, such as shivering in the cold environment.7 All three layers of the skin, the epidermis, dermis, and hypodermis, contain specialised sensory nerve structures, such as Meissner corpuscles, Vater-Pacini corpuscles and unmyelinated nerve fibres.7 Meissner corpuscles are responsible for sense of light touch and are mostly concentrated on the fingertips4,7 and the Vater-Pacini corpuscles are located at a deeper level in the dermis. They are large-ended nerves responsible for detecting pressure.7
Regulation of the body temperature
The skin has the ability to maintain it’s optimal temperature of 37°, by the process of either vasodilation or vasoconstriction.20 When the skin temperature drops below the 37°, arterioles in the dermis constrict to preserve the heat, the sweating stops and the skin hair erects to increase insulation.20 If the skin temperature increases above 37°, the sweat glands; the accessory structure of the skin, produce sweat to cool down the skin as the sweat is evaporated from the skin.4 In addition, the arterioles in the dermis vasodilate to release the extra heat carried by the blood stream and cool down the body.4
Immunological function
Human skin hosts a range of immune responses which belong to both the innate and adoptive immune systems.21 The cross talk between the cells in the skin (such as Langerhans) and the immune cells regulates local immune responses and ensures efficient host defence to prevent entry of microorganisms through the skin and possible infection.21
Endocrine function
The skin is responsible for production of various hormones, such as steroids and vitamin D.22 Vitamin D is synthesised in the epidermal layer of the skin after exposure to UV radiation.4 Vitamin D is essential for absorption of calcium and phosphorous, which are the main components of bones.4
Skin through the lifespan: The effect of ageing
The skin changes as a result of ageing can be clearly seen and are related to both intrinsic and extrinsic changes in a person’s body.23,24 Exposure to UV and pollution is generally more prolonged in older people, causing more prevalence of extrinsic changes, such as skin marks and other skin defects.23,25 While extrinsic factors could be modified, the intrinsic changes are inevitable and occur as time progresses.24
The intrinsic factors of ageing also cause structural changes to the skin of elderly people. One of the changes is that the dermal thickness decreases by approximately 20%, resulting in the appearance of paper-thin skin.14,23,26 The differentiated keratinocytes located in the stratum corneum become less adherent to each other.23 There is altered and reduced sensation, thermoregulation, rigidity, moisture retention and sagging skin, as a result of decreased dermal cells, reduction in collagen fibres, blood vessels and nerve endings.14 There is flattening of the dermal-epidermal junction, also known as the basement membrane which anchors the dermis to the epidermis.23,26 The subcutaneous fat below the dermis consists of mainly adipose tissue which provides protection, padding and insulation. The amount of this fat is reduced as a result of ageing and subsequently reduction of those protective mechanisms.27 Ageing skin is less able to synthesise vitamin D when exposed to UV rays from the sun.27
Conclusions
Skin is a vital organ; often unappreciated but complex, consisting of three multistructural layers, different cell types and additional epidermal appendages. All these layers are interconnected and establish the critical functions of protection, preventing the loss of body fluids and electrolytes, thermoregulation, vitamin D synthesis and endocrine functions. Ageing reduces the keratinocyte turn over in the epidermis, causes epidermal changes, such as the thickening of the stratum corneum and thinning of the stratum spinosum, resulting in less rigid skin and lower moisture retention in older population.11 Ageing also decreases the number of Langerhans cells, melanocytes and fibroblasts, which leads to lower immune function of the skin and less tensile strength of the skin.15
Acknowledgements
I acknowledge the support of Dr Peta Tehan, for revising this paper.
Conflict of interest
The author declares no conflicts of interest.
Ethics statement
An ethics statement is not applicable.
Funding
Monash University provided financial support for the time taken to prepare this manuscript.
Author contribution
This manuscript was prepared by one author.
Author(s)
Zahra Lotfollahi
School of Clinical Sciences, Monash University, Clayton, Australia
*Corresponding author email Zahra.Lotfollahi@monash.edu
References
- Wysocki A, Anatomy and physiology of skin and soft tissue. In: Bryant RA, Nix DP, editors. Acute & chronic wounds: Current management concepts. Mosby Elsevier; 2016. p. 40−62.
- Lopez-Ojeda W, et al. Anatomy, Skin (Integument) [Updated 2022 Oct 17]. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2024. [cited 2024 March 17].
- Yadav N, et al. Skin Anatomy and Morphology. In: Dwivedi A, et al, editors. Skin aging & cancer: Ambient UV-R Exposure.Singapore: Springer; 2019. p. 1−10.
- Biga LM, et al, Anatomy & Physiology. 1st ed. OpenStax; 2019.
- Narasimha Murthy S, Shivakumar HN. Chapter 1: Topical and transdermal drug delivery. In: Kulkarni VS, editor. Handbook of non-invasive drug delivery systems. Boston: William Andrew Publishing; 2010. p. 1−36.
- Honari G. Skin structure and function. In Honari G, Andersen R, Maibach HL, editors. Sensitive skin syndrome. CRC Press; 2017. p. 16−22.
- Gilaberte Y. et al. Chapter 1: Anatomy and function of the skin. In: Hamblin MR, Avci P, Prow TW, editors. Nanoscience in dermatology. Boston: Academic Press; 2016. p. 1−14.
- National University of Singapore School of Medicine. Skin: Normal Histology. [Internet] c2024 [cited 2024, March 17]Available from: https://medicine.nus.edu.sg/pathweb/normal-histology/skin/.
- Cowin A, Waters J. The science of wound healing. In: Swanson T, Asimus, M McGuinesss B, editors. Wound management for the advanced practitioner. IP Communications; 2014. Chapter 1.
- Sussman C, Bates-Jensen B. Skin and soft tissue anatomy and wound healing physiology. In: Sussman C, Barbara M, Bates-Jensen B, editors. Wound care: A collaborative practice manual for physical therapists and nurses. Philadelphia, PA: Lippincott Williams & Wilkins; 2012. p. 17−52.
- Bonham CA, Kuehlmann B, Gurtner GC. Impaired neovascularization in aging. Adv Wound Care (New Rochelle). 2020;9(3):111−126.
- Menon GK. New insights into skin structure: scratching the surface. Advanced Drug Delivery Reviews. 2002;54:S3−S17.
- Tortora GJ, Derrickson B. Principles of anatomy and physiology. John Wiley and Sons; 2017.
- Baranoski S, Ayello EA. Wound Care Essentials: Practice Principles. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2012.
- Sgonc R, Gruber J. Age-related aspects of cutaneous wound healing: a mini-review. Gerontology. 2013;59(2):159−64.
- Monteiro-Riviere NA. Toxicology of the skin. Boca Raton: Informa Healthcare; 2010.
- Fenner J, Clark RAF. Anatomy, physiology, histology, and immunohistochemistry of human skin. In: Albanna M, Holmes JH IV, editors. Skin tissue engineering and regenerative Medicine. Boston: Academic Press; 2016. p. 1-17.
- Barbieri JS, Wanat K, Seykora J. Skin: Basic structure and function. In McManus LM, Mitchell RN, editors. Pathobiology of human disease. San Diego: Academic Press; 2014. p. 1134−1144.
- Kim JY, Dao H. Physiology, (Integument) [Updated 2023 May 1]. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2024. [cited 2024 March 17].
- Guyton AC, Hall JE. Text book of medical physiology. 2006: China: Elsevier; 2006.
- Pasparakis M, Haase I, Nestle FO. Mechanisms regulating skin immunity and inflammation. Nat Rev Immunol, 2014;14(5):289−301.
- Nejati R, Kovacic D, Slominski A. Neuro-immune-endocrine functions of the skin: an overview. Expert Rev Dermatol. 2013; 8(6):581−583.
- Fenske NA, Lober CW. Structural and functional changes of normal aging skin. J Am Acad Dermatol. 1986;15(4/1):571−585.
- Baumann L. Skin ageing and its treatment. The Journal of Pathology. 2007;211(2):241-251.
- Uitto J. Understanding premature skin aging. NEJM. 1997;337(20):1463-1465.
- Gilhar A, et al. Ageing of human epidermis: the role of apoptosis, fas and telomerase. Br J Dermatol. 2004;150(1):56−63.
- Waller JM, Maibach HI. Age and skin structure and function, a quantitative approach (II): protein, glycosaminoglycan, water, and lipid content and structure. Skin Res Technol. 2006;12(3):145−154.



