Volume 6 Number 1
Tactical medicine for blast injury victims in a civilian context
John Moloney, Matthew Richardson
Keywords hot zone, tactical medicine, blast injuries
For referencing Moloney J and Richardson M. Tactical medicine for blast injury victims in a civilian context. JHTAM 2023; 6(1):to be assigned.
DOI
10.33235/JHTAM.6.1.to be assigned
Submitted 27 September 2023
Accepted 7 December 2023
Abstract
Blast injuries are not commonly seen by civilian healthcare workers. Injury patterns may be unfamiliar. In the high threat environment, which is likely to be present after an event, the types of care provided need to balance the probable clinical needs of the victim and the safety and security needs of responders.
Introduction
This paper will focus on the civilian environment where medical assets are deployed into a tactical environment to provide clinical care for those injured by an explosive event and/or subsequent events. These victims may include high value targets, e.g., politicians or other dignitaries, members of the general population, responders and perpetrators. The ethical issues associated with triaging and managing perpetrators is discussed elsewhere1,2.
The topic will also be of interest to those involved in military environments and to those specifically employed to provide security and emergency health response to potential high value targets.
Blast injury mechanisms
There are many useful sources describing the mechanisms and pathophysiology of blast injuries2. Blast injuries are categorised by the different physical ways that an explosion impacts on the body.
Primary injuries
Primary injuries are those due to the blast wave, caused exclusively by high order explosives – substances that on detonation generate a supersonic shock wave. Primary blast injuries are due to an acute increase, and subsequent decrease, of ambient pressure. These pressure changes and injuries are more significant in enclosed environments such as cafes, buses, and trains. The pressure waves are enclosed and reflect from walls. These pressure waves can reflect around a physical barrier and need to be considered in relation to both potential exposure to the primary event and safety from a potential secondary device.
Blast waves can cause dismemberment, which is generally not amenable to treatment. Other injuries included in this mechanism involve gas containing body parts – ear, lungs and the gastrointestinal tract. Ear injuries include ruptured ear drums and middle ear disruption. This can cause acute hearing loss3 and vertigo4. These can inhibit communication and movement but are not life-threatening and do not require management in the tactical environment.
Blast lung has an evolving injury pattern, with continued progression over a period of hours to days. Clinical management is generally supportive5, with an associated goal of avoiding secondary injuries, including those due to barotrauma and arterial air embolism. There is no appropriate treatment available in the direct threat care component of the event6. In the warm and subsequent zones, an awareness of the possibility of blast lung may influence further interventions, including the need for intubation and protective ventilation strategies.
Primary blast injuries to the gastrointestinal tract can cause a perforated viscus. The victim will need surgical intervention in the subsequent hours. Management in the pre-hospital environment is limited to pain management. The priority of providing this in the tactical environment will follow the provision of life-preserving care.
Secondary, tertiary, quaternary and quintenary injuries
Secondary injuries are those associated with projectiles accelerated by the explosive event2. Many terrorists pack their explosive device with various metal objects such as nuts and bolts to become projectiles to injure those in the vicinity of the explosion.
Tertiary injuries are those due to the body of the injured being thrown through the air. The patterns of injury are like those acquired from falls. Victims suffer from blunt trauma, with closed head injuries, limb fractures or internal injuries like those from other causes of blunt trauma.
Quaternary injury includes all other mechanisms of acute injury – burns, smoke inhalation, exposure to chemical, biological or radiological agents or exacerbation of pre-existing medical conditions. Quintenary injury is an inconsistently applied concept, which includes delayed issues such as chronic pain, malnutrition and infection7.
Assessing the care needed in different zones
Hot zone
DTC: the priorities of a tactical response unit have been described as “Stop the killing, Stop the dying”8. Stopping the killing is one of the tactical goals of the mission for a military or police SWAT (special weapons and training) team deployment. There are a variety of mechanisms by which “Stopping the killing” can be achieved, most of which are not within the remit of those present for their clinical skills and will not be discussed further.
In an area where there is significant and ongoing risk from firearms, explosive devices or chemical / biological / radiological (CBR) agents, no-one is safe, regardless of firepower, protection or training. Further injury or death is possible, for both the victim and caregiver. Those tasked for their tactical responsibilities accept some increased level of risk. Those primarily present to provide healthcare should be aiming to minimise this risk to an absolute minimum.
Facilitating cover from the ongoing or potential threats can prevent a victim from sustaining further injuries. Tactical teams may be able to provide some level of support to medical providers to provide immediate lifesaving care and victim extrication. Ongoing threats include the use of secondary explosive devices9, the secondary use of firearms after an explosive event10, or further injuries related to smoke or structural collapse after the explosion. There is also a potential risk of (further) exposure to chemical or radiological agents11.
An appreciation of these potential risks, ongoing situational awareness and assessment and continual communication from operational team members is critical. The assessment of current and projected tactical risk to current and possible victim treatment sites, and timelines for these to be secured, can be used to guide appropriate treatment priorities at any point of time.
The provision of medical care follows the MARCHH algorithm12: Massive haemorrhage control, Airway, Respiration, Circulation and then prevention and management of Hypothermia and assessment of Head injury (Figure 1).
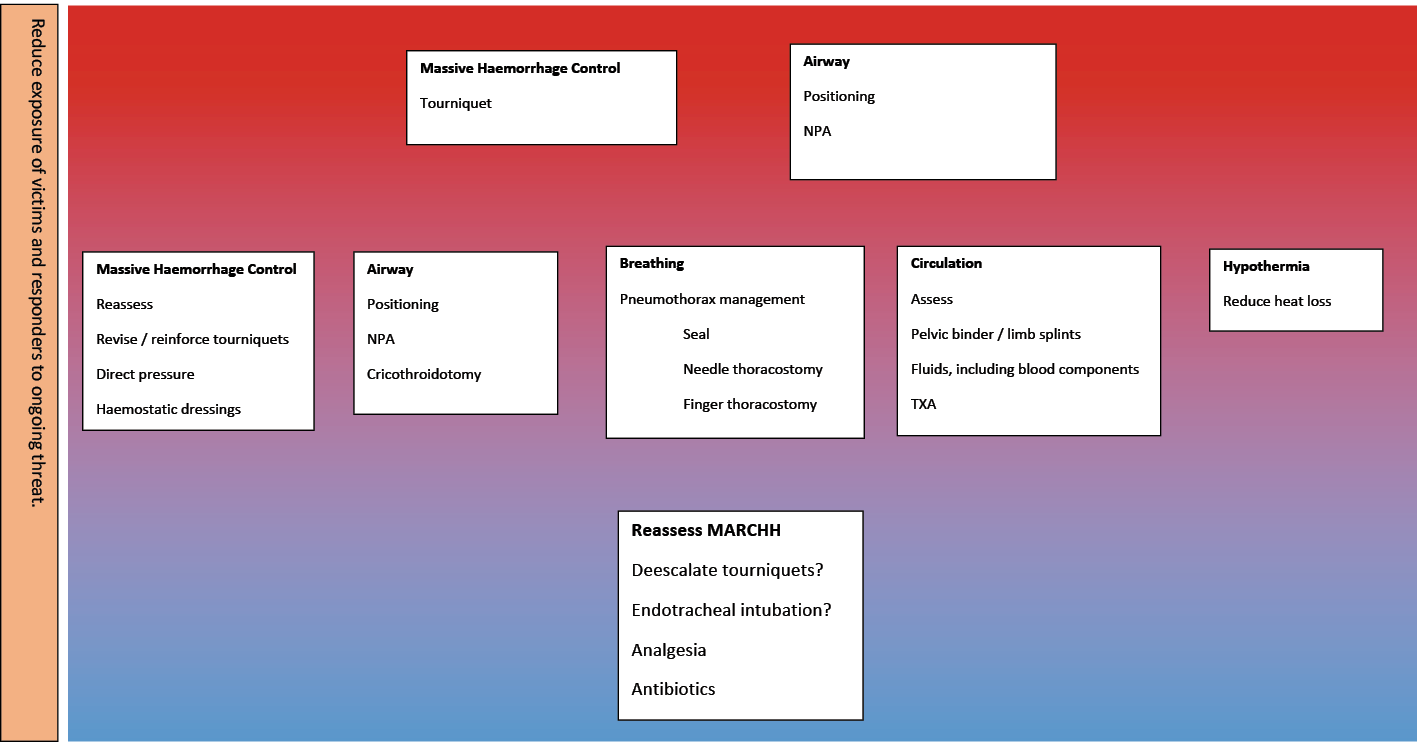
Figure 1. MARCHH treatment options during evacuation from hot and warm zones to cold
Massive haemorrhage control is time critical and should be addressed as soon as it is operationally achievable and is tactically feasible. In the very early stages this will be limited to extremity and junctional injuries. Exsanguinating torso injuries are not manageable on scene and require urgent evacuation to a surgical team. Life-threatening haemorrhage can lead to death within minutes. Self-application of arterial tourniquets can be achieved within 60 seconds and prevent life-threatening blood loss13. Medical team application of a tourniquet should occur as soon as operationally safe to do so. Tourniquets are placed about 10cm above the wound and over clothing. The time of application should be noted on the tourniquet.
Even victims who have lost consciousness, particularly in the absence of significant head injury, should have a tourniquet applied to exsanguinating injuries. Blood loss and resultant hypotension causes decreased oxygen delivery to the brain and loss of consciousness. Impaired mentation can begin with the loss of 30% of the blood volume14, approximately 1500ml in a 70–80kg adult. Larger blood loss is obviously life-threatening but is not without the possibility of a good outcome if the victim can survive long enough to receive higher levels of care. If the victim is making respiratory effort, attempts at haemorrhage control remains indicated.
If tactically feasible, basic airway management can also be undertaken in a hot zone. There are multiple mechanisms which can contribute to airway obstruction in a blast injury victim. A decreased conscious state is associated with loss of tone of muscles in the upper airway. The tongue will fall towards the posterior wall of the oropharynx, obstructing airflow15. Positioning an unconscious victim on their side or in the recovery position may be sufficient to provide a patent airway. There is a theoretic advantage to placing the victim left side down16 to reduce some consequences of arterial air embolism. In the hot zone, this positioning may not be the most urgent priority.
The insertion of a nasopharyngeal airway (NPA) can also provide a passage for air movement. Positioning and NPA insertion can be quickly and safely performed by providers with only basic training. They do not require a light source, the use of which may alert protagonists to the presence and location of responders. The cervical spine is more likely to be injured in a blast event compared to ballistic events. This is due to the possibility of multiple projectiles or significant blunt trauma from bodily displacement or structural collapse. However, in the hot zone, with a patient with an acute upper airway obstruction, proper positioning, with or without a NPA, is appropriate.
Blast injuries can cause airway obstruction by multiple methods. Secondary (projectiles), tertiary (physical displacement) and quaternary (crush) blast injuries can cause bleeding and/or tissue swelling. Burns, either thermal or chemical, can also cause swelling of the face and upper airway and cause airway obstruction, particularly if the victim has been trapped within a burning structure. These injury patterns are less responsive to patient positioning and NPA management, so are less able to be managed when under fire. Other clinical interventions are generally not suitable to be performed in the hot zone.
Warm zone
In the warm zone the risk of further injury is significantly less but remains above baseline (Figure 1). This elevated risk suggests that this area could potentially and quickly deteriorate into a hot zone. Therefore, all interventions need to be performed expediently as the victims and carers may need to evacuate the area with minimal notice. There are also constraints on resources and personnel.
On arrival in the warm zone, the patient should be reassessed. Movement may dislodge previously implemented treatments. Attention should be again focused on the control of massive haemorrhage. The effectiveness of tourniquets is reassessed, confirming the absence of peripheral pulses. An additional tourniquet can be applied to any limb with ongoing bleeding. Bleeding that is not amenable to management by limb or junctional tourniquets might be able to be controlled by direct pressure and/or the use of haemostatic gauze.
The use of Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA) in a combat casualty care setting has been described17. By occluding the descending aorta, arterial bleeding below the diaphragm can be controlled. Ideally, REBOA patients require access to definitive surgery within approximately 60 minutes. In a multi-victim incident, even if it were available, REBOA would rarely be appropriate in the warm or cold zones.
Airway management can be escalated. Upper airway obstruction due to loss of consciousness can continue to be managed as in the hot zone – positioning and NPA. Soft tissue swelling due to ballistic, blunt or thermal injury mechanisms can have more intensive management. The use of cricothyroidotomy can provide a definitive airway as well as the ability to prevent further aspiration and enable positive pressure ventilation, should this be necessary18. A cricothyroidotomy is an easier skill to develop than endotracheal intubation and can be more reliably be performed in the presence of soft tissue injuries around the upper airway. A cricothyroidotomy can be performed through burns tissue on the front of the neck if necessary.
Some victims of a blast event will have facial fractures. These victims, if capable, are likely to position themselves in such a manner as to maintain a patent airway. As much as possible, this should be facilitated.
Respiration can be adversely affected by multiple mechanisms in the victims of a blast event. Ballistic or blunt trauma can disrupt nerve supplies to the respiratory muscles – the intercostals and the diaphragm. The ability of the muscles to generate sufficient negative pressure to adequately inhale is impacted. The provision of positive pressure ventilation, such as through using a bag/valve assembly attached to a cricothyroidotomy tube or through a mask tightly applied to the face, can address hypoxia and hypercarbia. A small amount of PEEP can be used but is not critical. Mouth to mouth should not be used in cases involving potential chemical exposure.
Ballistic injury can produce an open pneumothorax. In this injury, the negative pressure generated to inhale instead sucks air through a hole in the chest wall directly into the pleural space. With exhalation, this gas leaves19. This reduces the amount of air moved in and out of the lungs with each breath, causing hypoxia and hypercarbia. This can be managed using an airtight seal, ideally vented. This prevents air entering during inhalation, whilst enabling trapped air to escape during exhalation.
The ability to inhale is affected by rising intrathoracic pressures, as would occur with a tension pneumothorax. This could be caused by either ballistic or blunt mechanisms, such as broken ribs. A valve-like hole in the lung or chest wall enables air to enter the pleural space during inspiration, as the body sucks air into the chest cavity. During expiration, if this valve closes, the air is trapped. Each inspiration increases the volume of air in the pleural space, negatively impacting the volume of air which can enter the lung. The increased pressure in the chest also impairs the ability for blood to return to the heart, contributing to hypotension or even cardiac arrest. Other signs supporting the presence of a tension pneumothorax could include haemoptysis and subcutaneous emphysema. Their absence does not exclude a tension pneumothorax.
The immediate management of this problem is the insertion of a needle into the pleural space, enabling some air to be released. There are several acceptable approaches, with a common one being the insertion of the needle through the 2nd intercostal space in the midclavicular line20. A hiss from release of air indicates appropriate placement and should lead to some improvement in ability to breath and blood pressure. More definitive management, which requires a higher level of expertise but may still appropriate in the warm zone, is a finger thoracostomy. An incision, followed by blunt dissection, making a hole into the pleural space in the 5th intercostal space in the midaxillary line21. Victims who have an injury which penetrates the pleural space may be able to be decompressed by inserting a finger through the wound.
The lungs can be adversely affected by the blast wave, with damage to the membrane separating the alveolus and the blood. There is no management required in the warm zone; however, the application of positive pressure to the airway may lead to systemic air embolism, which can then cause acute focal ischaemic events, such as strokes or myocardial infarction. The use of the lowest airway pressures and positioning the victim with the more injured side dependent can reduce the risk of this significant sequelae. As mentioned previously, positioning the patient left side down, semi prone, may decrease the risk of systemic air entering the coronary circulation.
Support of the circulation is considered next. Victims who have been thrown or crushed may have a fractured pelvis or long bone. A pelvic splint and splinting of long bone fractures may reduce ongoing blood loss and provide some degree of comfort. The patient is also evaluated head to toe for bleeding sites which, although not catastrophic, need to be managed. Packing with gauze or application of a compression bandage may be necessary.
Fluids to manage hypotension can be administered by intravenous or intraosseous routes. Targets for blood pressure with fluid replacement are controversial. Guidance will depend upon available fluids, distance to definitive care and the presence or absence of significant head injury, as suggested by decreased conscious state. Broadly, a target of a systolic blood pressure of 80mmHg in an awake patient is probably adequate, with a target of 110–120mmHg in unconscious patients. Older victims, as may happen in civilian blast events, probably require a higher target than a healthy military age soldier. If available, blood, either whole blood or packed red blood cells, is probably the preferable resuscitation fluid in these circumstances. Tranexamic acid has become a standard component of managing traumatic blood loss in the pre-hospital sphere. However, a recent study has cast some doubt on this practice22.
Efforts should be made to prevent the victim becoming cold. Wet clothing should be removed, and the patient sheltered from the elements. It may be appropriate to leave tactical wear intact. Situating the victim off the ground and using a space blanket can help reduce heat loss. Finally, the documentation of treatment administered and vital signs will enable a more acute and complete handover as the victim moves through the health system.
Cold zone
Subsequently, the victim will be moved to the cold zone. In this space there are no additional tactical risks, and so is like environments of other pre-hospital events. Depending on the availability of providers and transport options, victims may remain in this area for some time before they are able to be moved to higher echelons of care.
The victim is reassessed utilising the same MARCHH framework (Figure 1). Is the massive compressible haemorrhage still controlled? Is the tourniquet still appropriately positioned and occluding arterial flow? In some circumstances it may be appropriate to de-escalate from tourniquets to packing the wound with haemostatic gauze. Is the airway still patent? Is there a need for further intervention due to increased swelling?
Is the breathing pattern adequate? Is there adequate chest movement? Is there a need for further chest decompression? Is there a need for positive pressure ventilation due to nerve agents or developing stiff lungs? Is circulation adequate? What is an appropriate blood pressure target and the best method to attempt to achieve this? Are we maintaining body temperature? Is there a head injury?
Arriving at a safer place, with more and higher-level resources, attention can then be given to:
- Pain management, recognising the multiple injury mechanisms and the effects of pain control medications on cardiorespiratory and neurological function. Careful titration is important.
- Early administration of antibiotics; this may be advisable, particularly if there will be a delay to their administration at another site. Victims of blast injuries have multiple potential sources of infection, from dirty ball bearings, bacteria from the skin and gastrointestinal tract, compound fractures and tissue from other people involved in the incident.
- Cleaning and dressing of wounds, helping with pain, and reducing the risk of subsequent infection.
- Splinting of injured limbs; this will reduce some of the pain.
In summary, the multiple mechanisms of injury associated with a blast injury (and potential secondary events) impact on the needs of the victims. By following the principles of TECC with the details enlightened by understanding the relevant pathophysiology, optimal victim outcome can be achieved with minimal unnecessary risk being undertaken by the medial provider.
Author(s)
John Moloney*1, Matthew Richardson2
1Monash University, Department of Anaesthesiology and Pain Medicine, The Alfred, Melbourne, VIC, Australia
Medical Advisor, Ambulance Victoria, Field Emergency Medical Officer Program, St. Vincent’s Hospital, Fitzroy, VIC, Australia
2Mobile Intensive Care Ambulance Paramedic, Ambulance Victoria, VIC, Australia
*Corresponding author email john.moloney@ambulance.vic.gov.au
References
- Gold A, Strous RD. Second thoughts about who is first: the medical triage of violent perpetrators and their victims. Journal of Medical Ethics [Internet]. 2016 Aug 29;43(5):293–300. Available from: https://jme.bmj.com/content/43/5/293
- Moloney J, Welch M, Cardinal A. Applied Pathophysiology of Blast Injuries. Journal of High Threat & Austere Medicine. 2019 Sep 10;1(1).
- Ballivet de Régloix S, Crambert A, Maurin O, Lisan Q, Marty S, Pons Y. Blast injury of the ear by massive explosion: a review of 41 cases. Journal of the Royal Army Medical Corps. 2017 Feb 16;163(5):333–8.
- Lien SJ, J. David Dickman. Vestibular Injury After Low-Intensity Blast Exposure. Front Neurol. 2018 May 14;9.
- Sziklavari Z, Molnar TF. Blast injures to the thorax. Journal of Thoracic Disease. 2019 Feb;11(S2):S167–71.
- Smith JG. The epidemiology of blast lung injury during recent military conflicts: a retrospective database review of cases presenting to deployed military hospitals, 2003–2009. Philos Trans R Soc Lond B Biol Sci. 2011 Jan 27;366(1562):291–4.
- Kluger, MD, FACS Y, Nimrod, MD A, Biderman, MD P, Mayo, MD A, Sorkin, MD P. The quinary pattern of blast injury. Journal of Emergency Management. 2006 Jan 1;4(1):51.
- Responding to An Active Shooter Stop the Killing. Stop the Dying. Presented by Corporal Randy Baker ALERRT Instructor Texas Tech Police Department [Internet]. [cited 2024 Jan 27]. Available from: https://www.depts.ttu.edu/coe/safety/documents/ActiveShooterNotes.pdf
- Our History | Bureau of Alcohol, Tobacco, Firearms and Explosives [Internet]. www.atf.gov. [cited 2024 Jan 27]. Available from: https://www.atf.gov/our-history/
- Many Dead After Shooting Spree, Explosion At School In Russia’s Tatarstan [Internet]. RadioFreeEurope/RadioLiberty. 2021 [cited 2024 Jan 27]. Available from: https://www.rferl.org/a/many-dead-after-shooting-spree-explosion-at-school-in-russia-s-tatarstan/31249135.html
- NOVA | Dirty Bomb | Chronology of Events | PBS [Internet]. Pbs.org. 2019. Available from: https://www.pbs.org/wgbh/nova/dirtybomb/chrono.html
- Guidance [Internet]. www.c-tecc.org. Available from: https://www.c-tecc.org/our-work/guidance
- Kragh JF, O’Neill ML, Walters TJ, Dubick MA, Baer DG, Wade CE, et al. The Military Emergency Tourniquet Program’s Lessons Learned with Devices and Designs. Military Medicine. 2011 Oct;176(10):1144–52.
- Hooper N, Armstrong TJ. Hemorrhagic Shock [Internet]. National Library of Medicine. StatPearls Publishing; 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470382/
- ANZCOR Guideline 4 -Airway [Internet]. 2016 [cited 2024 Jan 27]. Available from: https://www.revive2survive.com.au/wp-content/uploads/2016/09/anzcor-guideline-4-airway-jan16.pdf
- Blast Injuries: Recognition and Management [Internet]. Brooksidepress.org. 2024 [cited 2024 Jan 27]. Available from: https://brooksidepress.org/Products/OperationalMedicine/DATA/operationalmed/MilitaryMedicine/ Blast%20Injuries/BlastInjuriesRecognitionandManagement.htm
- Manley J, Mitchell BT, DuBose JJ, Rasmussen TE. A Modern Case Series of Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA) in an Out-of-Hospital, Combat Casualty Care Setting. J Spec Oper Med. 2017 Jan 1;17(1):1–1.
- Schober P, Biesheuvel T, de Leeuw MA, Loer SA, Schwarte LA. Prehospital cricothyrotomies in a helicopter emergency medical service: analysis of 19,382 dispatches. BMC Emergency Medicine. 2019 Jan 23;19(1).
- Open Chest Injury [Internet]. REAL First Aid. Available from: https://www.realfirstaid.co.uk/openchestinjury
- Zengerink I, Brink PR, Laupland KB, Raber EL, Zygun D, Kortbeek JB. Needle Thoracostomy in the Treatment of a Tension Pneumothorax in Trauma Patients: What Size Needle? The Journal of Trauma: Injury, Infection, and Critical Care. 2008 Jan;64(1):111–4.
- Hannon L, St Clair T, Smith K, Fitzgerald M, Mitra B, Olaussen A, et al. Finger thoracostomy in patients with chest trauma performed by paramedics on a helicopter emergency medical service. Emergency Medicine Australasia. 2020 Jun 21;32(4):650–6.
- Gruen RL, Mitra B, Bernard SA, McArthur CJ, Burns B, Gantner DC, et al. Prehospital Tranexamic Acid for Severe Trauma. N Engl J Med. 2023 Jun 14.