Volume 6 Number 1
Safe and effective use of peripheral nerve blocks in the ROLE 2 maritime expeditionary environment
Eric H Twerdahl, Andy G Lum, Brian M Keuski, Andrew C Graf, Gregory H Freitag
Keywords military, austere medicine, pain management
For referencing Twerdahl EH et al. Safe and effective use of peripheral nerve blocks in the ROLE 2 maritime expeditionary environment. JHTAM 2024; 6(1):to be assigned.
DOI
10.33235/JHTAM.6.1.to be assigned
Submitted 8 January 2024
Accepted 12 January 2024
Abstract
From August through to October 2016, the amphibious assault ship USS WASP LHD 1 and embarked elements of the 22nd Marine Expeditionary Unit (MEU) were forward deployed in support of amphibious combat operations. The embarked medical assets included a fleet surgical team (FST) which included a general surgeon and an anaesthesia provider with expertise in regional anaesthesia (RA), including peripheral nerve blocks (PNBs). Here we report a case series demonstrating the safe and effective use of PNBs aboard USS WASP during the above-noted deployment. RA, and PNBs in particular, can play an important role in maritime expeditionary surgery and likely across the entire spectrum of high threat and austere environments.
Introduction
Peripheral nerve blocks (PNBs) in regional anaesthesia (RA) have evolved since their first clinical application in the early 20th century and today constitute an indispensable part of the practice of anaesthesia1,2. A PNB can be defined as the placement of a local anaesthetic agent adjacent to a sensory nerve or group of nerves, in order to provide analgesia to the associated anatomic region(s) of the body. When used as an adjunct to general anaesthesia (GA), a PNB can reduce the requirement for systemic anaesthesia and improve postoperative pain control. When used in place of GA, a PNB essentially eliminates the systemic effects of anaesthesia and obviates the need for airway manipulation.
Beyond the walls of the operating room, PNBs have demonstrated efficacy in the emergency department, on the battlefield, and in the wake of natural disasters3–9. In a comparison of PNBs and GA in the management of civilian upper extremity trauma, O’Donnell and colleagues demonstrated the superiority of PNBs with respect to pain control, opioid consumption, and length of hospital stay6. Buckenmaier and colleagues, in reports published in 2009 and 2012, highlighted the utility of PNBs for the reduction of pain and anxiety among soldiers injured in Iraq and Afghanistan3,4. In austere environments, where operations must be performed with minimal power, equipment and personnel, the benefits of PNBs are especially noteworthy. Such was demonstrated by Missair and colleagues who responded to the 2010 earthquake in Haiti, and by Pang and colleagues who responded to the 2009 earthquake in Sumatra5,7. Between their two groups, over 550 extremity PNBs were performed with no appreciable anaesthesia-related morbidity.
From August through to October 2016, the amphibious assault ship USS WASP LHD 1 and embarked elements of the 22nd Marine Expeditionary Unit (MEU) were forward deployed in support of amphibious combat operations. The total complement of personnel afloat numbered approximately 2,500, including sailors, marines, and navy and marine corps aviators. Most were between the ages of 18 and 30, and all had been pre-screened for major medical conditions. The ship’s medical department was augmented by a fleet surgical team (FST) which included one general surgeon, one certified registered nurse anaesthetist, one emergency medicine physician, and one family medicine physician.
Here we report a case series demonstrating the safe and effective use of PNBs in the maritime expeditionary environment.
Cases
Transversus abdominis plane (TAP) block
The transversus abdominis plane (TAP) block is a procedure in which local anaesthetic is injected into the anterolateral abdominal wall, providing analgesia to the periumbilical and lower abdominal regions. Our shipboard technique involves the use of a SonoSite M-Turbo ultrasound system (FUJIFILM SonoSite, Bothell, WA), fitted with a 10-5 MHz linear transducer to identify the external oblique (EO), internal oblique (IO) and transversus abdominis (TA) muscles at the intersection of the transverse plane of the umbilicus and the sagittal plane of the anterior axillary line (Figures 1A & 1B).
A 20 G x 4 in Stimuplex Ultra echogenic needle (B. Braun Medical, Bethlehem, PA) is advanced under continuous ultrasound visualisation into the coronal plane between the IO and TA muscles (Figures 1B & 1C). After aspirating to confirm extravascular needle placement, 10mL of 0.5% Bupivacaine is injected. If the operative plan requires bilateral analgesia, the procedure is repeated on the contralateral side.
We used a preoperative TAP block in the case of a 22-year-old male marine who underwent an open appendectomy under GA for acute, gangrenous, retrocecal appendicitis. The patient’s postoperative opioid requirement was 5mg of oral Oxycodone in total, and he returned to full duty within 1 week.
The oblique subcostal TAP (OSTAP) block is a variant of the TAP block in which the area of analgesia includes the upper abdomen. In our practice, 10mL of 0.5% Bupivacaine is injected by hydro-dissection into the plane between the IO and TA muscles, along a line from the intersection of the transverse plane of the inferior costal margin and the sagittal plane of the lateral rectus sheath toward the anterior iliac crest (Figures 1D, 1E & 1F). If bilateral analgesia is required, the procedure is repeated on the contralateral side.
We used a postoperative, bilateral OSTAP block in the case of a 37-year-old female sailor who presented with severe pain in the right iliac fossa, signs of peritonitis, and leukocytosis. Diagnostic laparoscopy disclosed thin, rust-coloured fluid above the left lobe of the liver, in the right pericolic gutter, and in the pelvis, and subsequent exploratory laparotomy revealed the cause to be a ruptured right ovarian cyst. The patient's postoperative opioid requirement was 18mg of intravenous (IV) morphine over the first 24 hours and 12mg of IV morphine over the next 24 hours. The patient’s preoperative ileus resolved over the first postoperative day (POD), she was advanced to a regular diet on POD 2, and she was discharged from the inpatient unit on POD 4. She returned to limited duty after 2 weeks and to full duty within 4 weeks.
Supraclavicular (SC) brachial plexus (BP) block
The supraclavicular (SC) brachial plexus (BP) block is a procedure in which local anaesthetic is injected around the SC BP, providing analgesia to the upper extremity distal to the shoulder. Our technique involves the use of the above-described ultrasound and transducer set-up to identify the BP, subclavian artery (SCA), and parietal pleura (PP) (Figures 1G & 1H). A 22 G x 2 in Stimuplex Ultra echogenic needle is advanced under continuous ultrasound visualisation into the plane superior to the BP (Figures 1H & 1I). After aspirating to confirm extravascular needle placement, two 5mL aliquots of 0.5% Bupivacaine are injected, with repeat aspiration between aliquots. The needle is then re-positioned into the plane inferior to the BP, and the injection is repeated.
We used a preoperative SC block in the case of a 26-year-old male marine who presented with a large complex abscess involving the extensor surface of the right upper extremity. He underwent drainage, debridement and irrigation of the abscess cavity through three separate incisions, requiring no perioperative sedation or opioid pain medication.
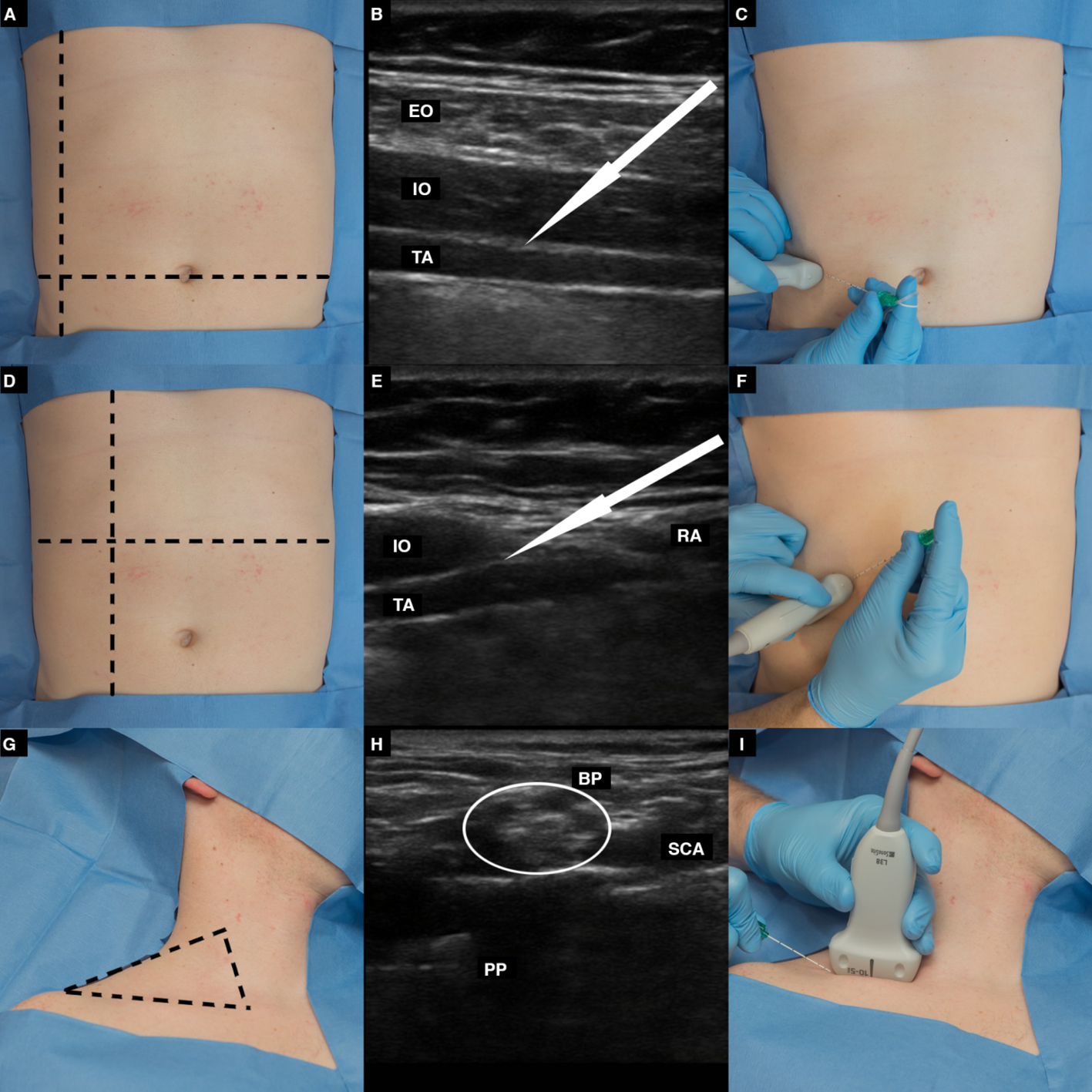
Figure 1.
A: Surface anatomy of the TAP block. The dashed lines indicate the transverse plane of the umbilicus and the sagittal plane of the anterior axillary line
B: Ultrasound view of the EO, IO and TA muscles. The arrow indicates the direction of needle advancement into the plane between the IO and TA muscles
C: Surface orientation of the transducer and needle
D: Surface anatomy of the OSTAP block. The dashed lines indicate the transverse plane of the inferior costal margin and the sagittal plane of the lateral rectus sheath
E: Ultrasound view of the IO, TA and rectus abdominis (RA) muscles. The arrow indicates the direction of needle advancement into the plane between the IO and TA muscles
F: Surface orientation of the transducer and needle
G: Surface anatomy of the SC BP block. The dashed lines indicate the superior border of the clavicle, lateral border of the sternocleidomastoid muscle, and superolateral border of the trapezius muscle
H: Ultrasound view of the BP, SCA and PP. The BP (circled) appears as a ‘honeycomb’. The arrows indicate the direction of needle advancement into the planes superior and inferior to the BP.
I: Surface orientation of the transducer and needle
Distal extremity block
A wrist block is a procedure in which local anaesthetic is injected around one or more of the radial, median and ulnar nerves at the level of the wrist, providing analgesia to the corresponding sensory region(s) of the hand. Our technique involves the use of palpable landmarks and the 20 G x 4 in Stimuplex Ultra needle to inject 5mL of 0.5% Bupivacaine around each of the required nerves.
We used a radial nerve block to reduce a right thumb carpometacarpal traumatic dislocation in the case of a 20-year-old male marine. We also used a combined radial and median nerve block to reduce a displaced right thumb basal metacarpal fracture in the case of another 20-year-old male marine. Neither patient required periprocedural sedation or opioid pain medication.
An ankle block is a related procedure in which local anaesthetic in injected around one or more of the tibial, superficial peroneal, deep peroneal, saphenous and sural nerves at the level of the ankle, providing analgesia to the corresponding sensory region(s) of the foot. Our technique involves the use of palpable landmarks and the 20 G x 4 in Stimuplex Ultra needle to inject 5mL of 0.5% Bupivacaine – 3mL in the case of the deep peroneal nerve – around each of the required nerves.
We used a preoperative ankle block in the case of a 35-year-old male sailor who presented with a chronic complex abscess involving the lateral right forefoot, and underwent drainage, debridement and irrigation of the abscess cavity through two separate incisions. The patient did require mild sedation at the start of the operation, but his postoperative opioid requirement was negligible.
Discussion
For health service support (HSS) in the operational environment, the United States military maintains a tiered system of medical and surgical care, the goal of which is to keep resuscitative and stabilising care at or near the point of injury10. ROLE 1 care is commonly known as first-responder/buddy aid. Casualties are either treated and returned to duty or stabilised and prepared for medical evacuation (MEDEVAC) to a higher level of care. ROLE 2 care includes forward resuscitative surgery and associated capabilities, such as the transfusion of blood and blood products. ROLE 3 care occurs in theatre-based hospitals configured with both the medical and surgical resources to support theatre combat operations. ROLE 4 and ROLE 5 facilities are large overseas and continental United States (CONUS) hospitals and medical centres capable of providing definitive and rehabilitative care.
The cases presented in this series are compiled from our experience aboard a maritime ROLE 2 platform where, compared to the land-based ROLE 2 environment, a number of specific challenges arise. The first is the relative complexity of resupply at sea, which is affected by weather, sea state, operational tempo, and the availability of resupply ships. Due to irregular resupply, medical and surgical care at any given time is limited by the availability of materials on board, and those materials can be exhausted quickly by multiple patients or by even a single critically ill patient if timely MEDEVAC is not available. The second is the relative complexity of using rotary-wing aircraft with limited range and launched from a single flight deck to support combat operations, personnel movement and MEDEVAC, again taking weather, sea state, operational tempo, and crew availability into account. The third specific challenge has to do with the environment itself. A naval vessel is an inherently dangerous industrial setting, which contains occupational hazards such as loud noise, heavy machinery and toxic chemicals. The overall goal of medical and surgical care in the maritime ROLE 2 environment, therefore, is to provide safe and high quality care with minimal resources, minimal personnel, minimal complexity, and minimal need for MEDEVAC. The use of PNBs as an adjunct to or in place of GA can help to accomplish that end.
We made safe and effective use of PNBs across a variety of clinical scenarios. In a case of appendectomy through a right lower quadrant incision, we used a preoperative TAP block to virtually eliminate the need for postoperative opioid analgesia. In a case of exploratory laparotomy through a vertical midline incision, we used a bilateral OSTAP block to minimise the patient’s postoperative opioid requirement. And, in several cases of extremity infection or trauma, we used PNBs to reduce or eliminate the need for periprocedural sedation and/or opioid pain medication. No patient experienced an anaesthesia-related complication. Each patient recovered uneventfully aboard the ship.
Several requirements must be met for PNBs to be employed safely in the ROLE 2 environment. The first requirement is an anaesthesia provider with the appropriate level of knowledge and training. Importantly, however, the knowledge and skills necessary to perform PNBs safely can be taught to other members of the medical and surgical team, broadening the applicability of PNBs across the spectrum of high threat and austere environments. The second requirement is a space with (1) the necessary equipment, including oxygen, electrocardiographic monitoring equipment and an ultrasound machine and (2) the necessary rescue equipment, including cardiopulmonary resuscitation equipment, intubation equipment and intralipid. The third requirement is appropriate patient selection, which is based upon a risk–benefit analysis accounting for the patient’s physical and medical status, the patient’s comorbid conditions, the surgical procedure to be performed, and the patient’s history of opioid use.
The benefits of PNBs have been well described, but there are still a number of potential complications to consider. The specific risks vary on the basis of the particular block being performed, but common to them all are the risks of infection, local anaesthetic toxicity, bleeding and neurological injury11. Fortunately, many of those risks can be minimised with appropriate patient selection and by the use of appropriate technique11. Nevertheless, some complications, such as neurologic injury, can be more difficult to avoid. A meta-analysis of 32 PNB studies covering a 10-year period reported a neurologic event rate of 3%12. Most of the events reported were transient and resolved within 3 months, and there was only one case of permanent neuropathy noted. Moreover, routine use of ultrasound guidance has been shown to decrease both the dose of anaesthetic necessary and the number of attempts required to achieve a successful block13.
Other modes of anaesthesia merit discussion in the context of PNBs, among them IV local anaesthesia and local anaesthetic wound infiltration14,15. IV local anaesthesia, known eponymously as a Bier block, involves the injection of a local anaesthetic agent into the superficial venous circulation of an extremity, following exsanguination of the extremity and application of an inflow (i.e., arterial) tourniquet. One advantage of IV local anaesthesia compared to a PNB is the creation of a bloodless operative field, though the disadvantages include risks of systemic toxicity, extremity compartment syndrome, superficial venous thrombosis/thrombophlebitis, deep venous thrombosis, arterial thrombosis, and pain at the site of the tourniquet. In the setting of non-penetrating trauma, when the degree of subcutaneous injury might extend beyond the visible wound, the potential complications of IV local anaesthesia are especially relevant. Local anaesthetic wound infiltration, which includes both single infiltration and continuous infiltration through a catheter or catheters placed in or around a surgical wound, has a broad spectrum of potential applications, particularly in postoperative analgesia. Despite potential complications including local anaesthetic toxicity, wound infection, haematoma and catheter dislodgement in the case of continuous infiltration, the technique is a useful multi-modal adjunct in the resource-limited environment.
The fundamental goal of expeditionary military medicine is to provide safe and high-quality medical and surgical care on the front lines of armed conflict. PNBs represent a particularly valuable asset in the maritime expeditionary environment because they allow for surgery to be performed with minimal intra-operative and postoperative monitoring and minimal controlled medications, and they have the potential to simplify MEDEVAC operations in cases where the use of systemic analgesia and/or the need for airway manipulation can be reduced or avoided. Though the preceding case series was compiled from specific experience in the maritime environment, it nevertheless demonstrates the utility of PNBs across the spectrum of austere environments, where medical and surgical care is constrained by the availability of resources and personnel.
Acknowledgements
Petty Officer First Class Eric Garst and Petty Officer Third Class Daniel Herzberg, both US Navy, helped with the preparation of the Figure.
Prior presentation
None.
Clinical trial registration
Not applicable.
Institutional review board (Human subjects)
Not applicable.
Institutional Animal Care and Use Committee (IACUC)
Not applicable.
Individual author contribution statement
EHT collected and analysed the data and drafted the original manuscript. All authors reviewed, edited and approved the final manuscript.
Data availability statement
The case files are available on request from the corresponding author.
Disclaimer
The opinions or assertions contained herein are the private ones of the authors and are not to be construed as official or reflecting the views of the Department of Defense, the Uniformed Services University of the Health Sciences or any other agency of the US Government.
Institutional clearance
Obtained from the Uniformed Services University of the Health Sciences, Bethesda, MD, USA.
Conflict of interest
The authors declare no conflicts of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author(s)
Eric H Twerdahl*1,2, Andy G Lum3, Brian M Keuski4, Andrew C Graf5, Gregory H Freitag6
1Department of Surgery, Uniformed Services University of the Health Sciences, Bethesda, MD, USA
2Department of Surgery, Walter Reed National Military Medical Center, Bethesda, MD, USA
3Department of Anesthesia, Naval Medical Center Camp Lejeune, Camp Lejeune, NC, USA
4Naval Special Operations Medical Institute, Fort Bragg, NC, USA
53rd Medical Battalion, Marine Corps Base Hawaii, Oahu, HI, USA
6National Defense University, Washington, DC, USA
*Corresponding author email eric.h.twerdahl.mil@health.mil
References
- Larson MD. History of anesthesia. In: Miller RD, Pardo MC, editors. Basics of anesthesia. Philadelphia: Elsevier; 2011. p. 3–10.
- De Buck F, Devroe S, Missant C, Van de Velde M. Regional anesthesia outside the operating room: indications and techniques. Curr Opin Anaesthesiol 2012;25(4):501–7.
- Buckenmaier C 3rd, Mahoney PF, Anton T, Kwon N, Polomano RC. Impact of an acute pain service on pain outcomes with combat-injured soldiers at Camp Bastion, Afghanistan. Pain Med 2012;13(7):919–26.
- Buckenmaier CC 3rd, Rupprecht C, Mcknight G, McMillan B, White RL, Gallagher RM, et al. Pain following battlefield injury and evacuation: a survey of 110 casualties from the wars in Iraq and Afghanistan. Pain Med 2009;10(8):1487–96.
- Missair A, Gebhard R, Pierre E, Cooper L, Lubarsky D, Frohock J, et al. Surgery under extreme conditions in the aftermath of the 2010 Haiti earthquake: the importance of regional anesthesia. Prehosp Disaster Med 2010;25(6):487–93.
- O’Donnell BD, Ryan H, O’Sullivan O, Iohom G. Ultrasound-guided axillary brachial plexus block with 20 milliliters local anesthetic mixture versus general anesthesia for upper limb trauma surgery: an observer-blinded, prospective, randomized, controlled trial. Anesth Analg 2009;109(1):279–83.
- Pang HN, Lim W, Chua WC, Seet B. Management of musculoskeletal injuries after the 2009 western Sumatra earthquake. J Orthop Surg (Hong Kong) 2011;19(1):3–7.
- Richman JM, Liu SS, Courpas G, Wong R, Rowlingson AJ, McGready J, et al. Does continuous peripheral nerve block provide superior pain control to opioids? A meta-analysis. Anesth Analg 2006;102(1):248–57.
- Stojadinovic A, Auton A, Peoples GE, McKnight GM, Shields C, Croll S, et al. Responding to challenges in modern combat casualty care: innovative use of advanced regional anesthesia. Pain Med 2006;7(4):330–8.
- NATO. Chapter 16: medical support (role support). In: NATO logistics handbook. Brussels: NATO; 1997. p. 1610–1640.
- Wedel DJ, Horlocker TT. In: Miller RD, editor. Miller’s anesthesia. Philadelphia: Churchill Livingstone; 2010. p. 1639–72.
- Brull R, McCartney CJ, Chan VW, El-Beheiry H. Neurological complications after regional anesthesia: contemporary estimates of risk. Anesth Analg 2007;104(4):965–74.
- Casati A, Danelli G, Baciarello M, Corradi M, Leone S, Di Cianni S, et al. A prospective, randomized comparison between ultrasound and nerve stimulation guidance for multiple injection axillary brachial plexus block. Anesthesiol 2007;106(5):99.
- Kraus GP, Rondeau B, Fitzgerald BM. Bier block; 2023 [updated 2023 Aug 5]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430760/
- Stamenkovic DM, Bezmarevic M, Bojic S, Unic-Stojanovic D, Stojkovic D, Slavkovic DZ, et al. Updates on wound infiltration use for postoperative pain management: a narrative review. J Clin Med 2021;10(20):4659. doi:10.3390/jcm10204659