Volume 22 Number 1
Translation and cross-cultural adaptation of a survey on skin tears among nurses in French-speaking Switzerland
Lucie Charbonneau, Sebastian Probst, Georgina Gethin
Keywords skin tear, translation, cross-cultural adaptation
DOI 10.35279/jowm202104.05
Abstract
Background There is a paucity of research investigating the experiences of nurses using a standardised skin tears programme and the influence that such a programme has on their clinical practice. The available literature is primarily in English, and there is a lack of validated instruments for use in other languages, including French.
Aim The aim of this study is to translate and cross-culturally adapt an original English language survey conducted among Australian nurses into Swiss French.
Method/results A structured methodological approach was used to translate, adapt and validate the survey based on Sousa and Rojjanasrirat’s translating process: (1) two independent bilingual experts were involved in the translation from English to Swiss French, and a synthesis version from both translations in Swiss French was obtained; (2) a blind back-translation of the synthesis version in English by two experts was completed, and consensus attained by a committee, to generate a pre-final version of the survey in Swiss French; (3) validation of the translated version was provided by postgraduate wound care students.
Conclusion The translated Swiss French 2020 survey is now ready to be used to assess the clinical reasoning of wound care specialists on the prevention and management of skin tears in Switzerland.
Implications for clinical practice Given the lack of research in this area, it is important for policymaking and improving patient outcomes that we understand the situation in Switzerland. Using an existing survey, updating it and doing a translation and cultural adaptation of it will allow an understanding of nurses’ clinical reasoning on skin tears in Switzerland, enabling comparisons with other countries.
INTRODUCTION
In 2018, the International Skin Tear Advisory Panel (ISTAP) published an updated definition of a skin tear: ‘A skin tear is a traumatic wound caused by mechanical forces, including removal of adhesives. Severity may vary by depth (not extending through the subcutaneous layer)’.1 There is a paucity of research literature investigating the experiences of nurses using a standardised skin tears programme and the influence that such a programme has on their clinical practice.2–4 An Australian study investigated the opinions, knowledge and clinical practice of nurses regarding skin tears. The findings revealed that skin tears were perceived as common wounds in aged residents, and nurses are directly involved in the reporting, assessment and management of these wounds. The study showed no uniform language used related to the description and classification of skin tears. Aging skin issues, risk assessment, skin tear classification, local wound management and preventative strategies were identified as important elements for future educational programmes.4 A recent study in Germany exploring nurses’ knowledge of skin tears5 showed that they do not know the international classification system for skin tears and lack knowledge on their prevention and treatment. The authors recommend that education on skin tears should start in nursing school and at the nursing college level.5
Given the lack of research in this area, it is important for both policymaking and improving patient outcomes that we understand the situation in Switzerland, as the current literature is not sufficiently generalisable to this setting.
The aim of this study is to translate and cross-culturally adapt an original English-language survey conducted by White4 in Australia into Swiss French, based on the seven-step methodology outlined by Sousa and Rojjanasrirat.6
METHOD
Survey
In 2001, White4 conducted a survey on the opinions, clinical practice and knowledgebase of Australian Registered Nurses concerning skin tears. The questionnaire was based on a literature review that included both open- and closed-ended questions, including: sociodemographic questions, nurses’ opinions on the incidence of skin tears, reporting, assessment and documentation. The authors explored nurses’ skin tear-related clinical practices, knowledge and education by asking questions on the definition and classification of tears, aging skin, risk factors, prevention strategies, educational programmes and existing literature.4
Skin tear prevention and treatment guidelines are now available1, and the initial questions on nurses’ opinions on clinical practice related to skin tear treatment and prevention have been updated accordingly in the 2020 survey. White used Payne and Martin’s7 definition of skin tears in her survey. This was also an opportunity to document which, if any, classification system nurses used in their clinical practice. The present study uses the validated French translation of the ISTAP definition and classification.8,9
The translation process
There are different methodological approaches for translating, adapting and validating instruments or scales for use in research. Unfortunately, the use of multiple processes leads to wide variations in health care literature and research. In this study, five out of the seven steps proposed by Sousa and Rojjanasrirat6 were adapted and deemed applicable to this context (see Figure 1).
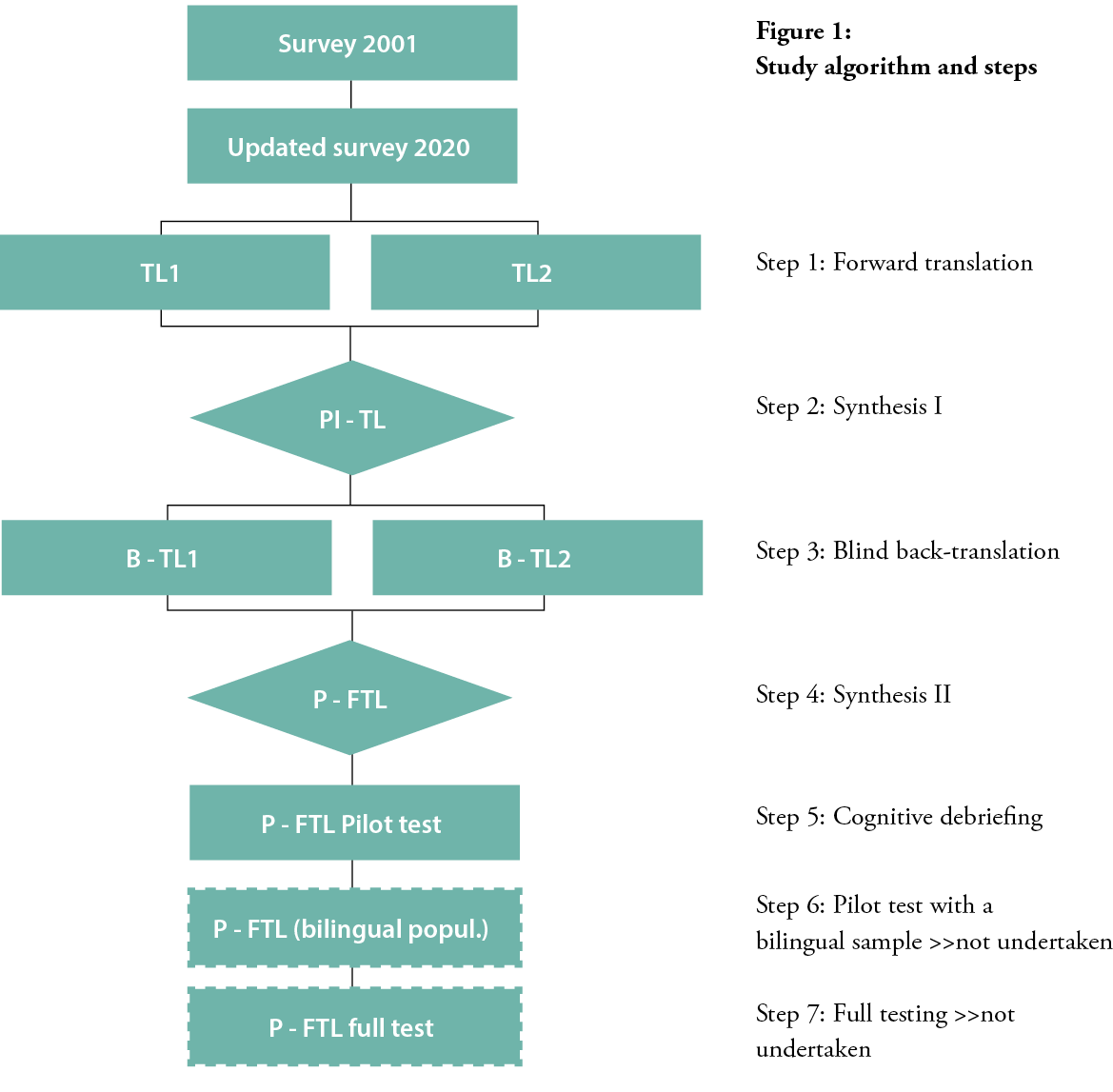
According to Sousa and Rojjanasrirat6, in Step 1, the original instrument must be translated by at least two independent, bilingual translators. They point out that the translators should have different backgrounds, one with knowledge of healthcare terminology and the other fluent in colloquialisms and popular expressions used in the desired language. It is preferable for the latter to have no knowledge of either medical terms or the construction of the instrument being translated.6 With this in mind, we worked with two bilingual experts with a health science background to complete a forward translation of the survey from English to Swiss French (TL1 and TL2). The choice to use translators with similar backgrounds was due to unavailable resources for meeting the full prerequisites outlined by Sousa and Rojjanasrirat.
In Step 2 of Sousa and Rojjanasrirat’s process6, a third independent translator compares the two translated versions and the original version of the instrument, to detect any hesitations and ambiguities. Ambiguities must be discussed and a consensus obtained from a committee composed of the third translator, the translators from Step 1 and the research team. This process engenders the ‘preliminary initial translated version of the instrument (PI–TL)’.6 Step 2 was adapted for this study because no third translator was used, again due to a lack of resources. The research team achieved consensus for the PI–TL version.
In Step 3, the preliminary translated version (PI–TL) is translated back into the original language. This step requires two new translators whose mother tongue matches the original instrument. The same prerogatives as Step 1 apply to both translators in Step 3, and they should be unaware of the original version of the instrument. This results in two back-translated versions of the original instrument (B-TL1 and B-TL2).6 In this study, two different experts back-translated the PI–TL from Swiss French into English in a blinded fashion.
As Step 4, both versions (B-TL1 and B-TL2) were compared by a multidisciplinary committee with the original version of the instrument in terms of format, words and sentences, meaning, similarities and relevance.6 Sousa and Rojjanasrirat6 highly recommend that the committee involve a methodologist, who may also be the investigator or a member of the research team; one healthcare professional familiar with the topics of the instrument; and all four translators from Steps 1 and 3. When possible, the creator of the original instrument should be involved in this process, too. Similar to Step 2, the role of the committee is to discuss and to resolve any ambiguities and discrepancies regarding the meaning, sentences and wording of the instrument. Consensus must be obtained to generate a pre-final version of the instrument (P-FTL).6 We also adapted Step 4; no methodologist was involved in this process. The committee was composed of three of the four experts involved in the translation, the co-supervisor and the author. One expert, the co-supervisor and the author are healthcare professionals at ease with the topic.
In Step 5, the pre-final version of the instrument (P-FTL) is pilot tested. Participants whose first language matches the translated version of the instrument and who will use the instrument are recruited to pilot test the P-FTL to evaluate its items for clarity and intelligibility. Each participant rates the instructions and items of the instrument using a dichotomous scale (clear or unclear). When an item is rated unclear, the participant is asked to document the reason why, suggest how it should be written or rewrite the item to make it clearer. The minimum inter-rater agreement among participants for content equivalency (clarity) is 80%.6 In this step, the nurses recruited to pilot the French survey were completing their Certificate of Advanced Studies (CAS HES-SO) in wound care in 2020 at the Geneva School of Health Sciences, HES-SO University of Applied Sciences and Arts Western Switzerland.
Steps 6 and 7 in Sousa and Rojjanasrirat’s6 process were not used in this study. Step 6 allows a comparison between the P-FTL and the original instrument in its original language, to establish criterion equivalency.6 This was not possible in the present study, due to the unavailability of a sample of bilingual participants. Step 7 calls for revising and refining the final translated version of the instrument based on a full psychometric testing among individuals from the target population. This step confirms sensitivity and specificity reliability, stability reliability, homogeneity, construct-related validity, criterion-related validity, factor structure and the model fit of the instrument.6 Since the original survey was initially tested for its accuracy and consistency by cross-referencing questions asked against the research questions, peer-reviewed and subject to a pilot study involving RNs, the present study omitted this step.
RESULTS
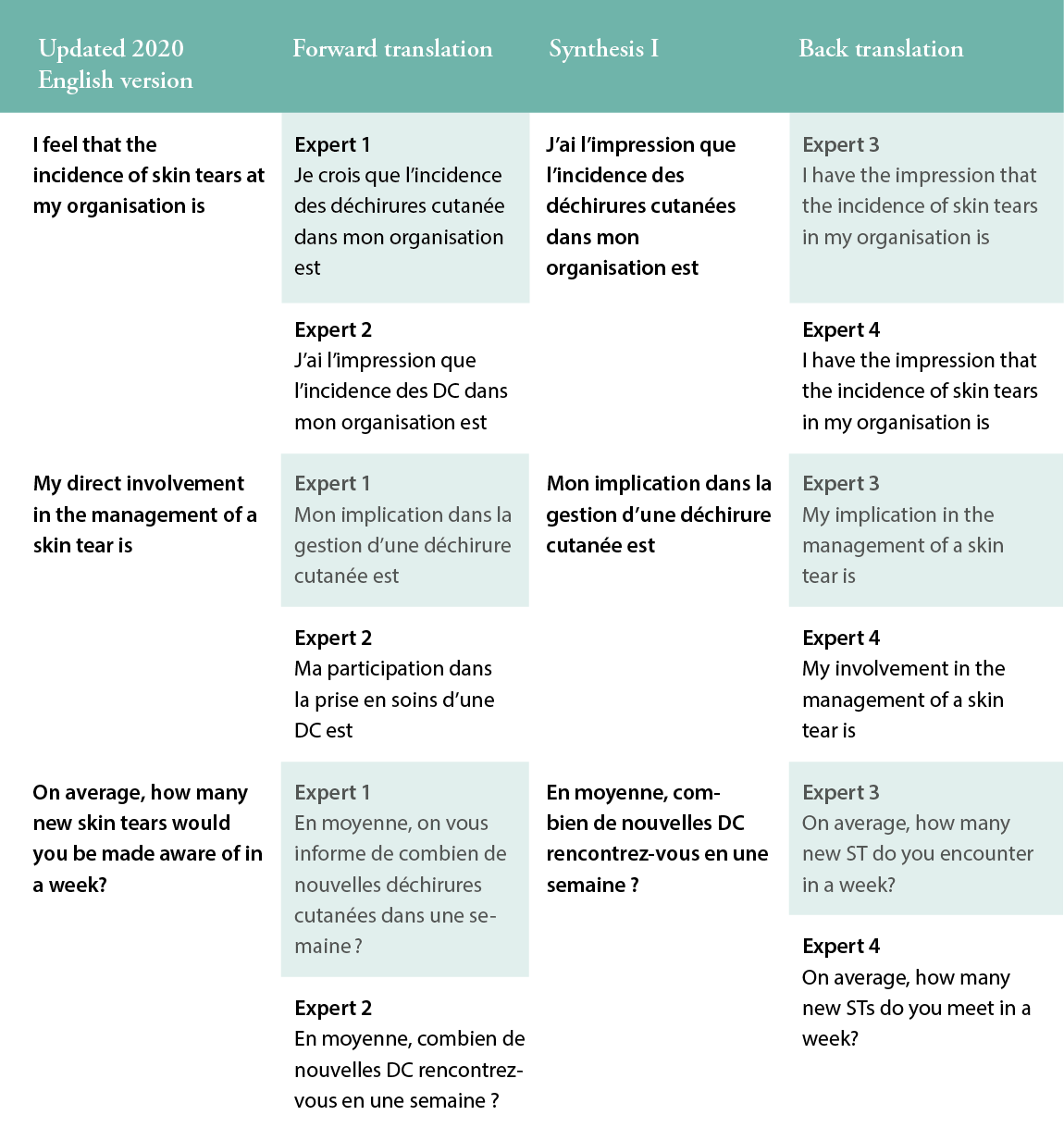
For the first step in the translation process, two MScN holders translated the survey forward from English into French (TL1 and TL2). The co-supervisor of the Master’s thesis and the author compared the TL1 and TL2 translations and discussed the discrepancies to agree on a preliminary initial translated version of the survey in Swiss French (PI-TL). In Step 3, one PhD holder and one nurse clinician back-translated from Swiss French into English (B-TL1 and B-TL2) in a blinded fashion. The example in Table 1 illustrates these three first steps.
Table 1: Example of Steps 1, 2 and 3 of the translation process for three questions.
For Step 4, the committee focused on the technicality of the B-TL1 and B-TL2 versions of the survey and the precision of the terms and questions translated. The following example illustrates this process. The committee had a long discussion about the item ‘dressing choices relating to skin tears’ as a topic that should be included in future educational programmes for Registered Nurses. The two experts involved in Step 1 translated this differently. One expert interpreted this item as ‘what kind of wound dressing would be used on a skin tear’, and the other as ‘how should a person dress to avoid skin tears’. In Step 2, the co-supervisor and the author agreed on using ‘what kind of wound dressing would be used on a skin tear’. After discussion about the meaning of the term in the original survey4, an agreement was reached to ask participants to identify if education would be useful concerning which ‘wound dressing/pansement’ to use on a skin tear. At the end of Step 4, consensus was attained to generate a pre-final version of the instrument (P-FTL).
Finally, for Step 5, a sample of 27 postgraduate wound care nurses were recruited for the pilot test. They were asked to complete the survey to: a) determine the time required to complete the questionnaire and b) evaluate the clarity and intelligibility of the different questions and answers in the survey. This step was very enlightening for the author. First, the time required to complete the questionnaire was nearly identical for all participants. Second, regarding clarity and intelligibility, 25 out of 36 questions reached 100% agreement among the participants. Even though participants declared nine questions to be ‘unclear’, these questions reached more than 80% agreement. Nonetheless, the author made some modifications or specifications to enhance the questions’ comprehensibility. For example, three questions relating to skin tears’ incidence and implications for the management of these wounds reached 93% agreement: two participants declared they did not know what a skin tear was. With this in mind, a picture of what a skin tear could look like was added to the survey’s introductory text (Figure 2). Some words used in French have different meanings depending on their context, which could lead to significant differences in the responses of future survey participants. Some participants (15%, n=4) interpreted the original author’s meaning differently and declared one question to be ambiguous. For example, the word ‘organisation’ has two meanings in English, as it does in French: a) ‘a group of people who work together in an organised way for a shared purpose’ or b) ‘the planning of an activity or event’.10 The author used ‘organisation’ to refer to a group of people working together as an institution, or the hospital where the participant works. However, some participants (n=4) interpreted the word ‘organisation’ to refer to their own planning or way of working. Therefore, the translation was good, but the item was misinterpreted and had to be rephrased to refer to the ‘care setting/milieu de soins’ in French, to reflect the reality of the Swiss healthcare environment. Based on these findings, the author adapted the survey and proposed its final version.
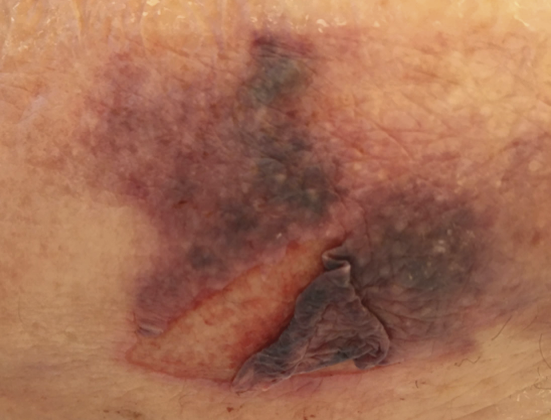
Figure 2: Skin tear
DISCUSSION
The aim of this study was to translate and cross-culturally adapt an original English survey into Swiss French. This is essential for enhancing the validity, generalisation and translation of cross-cultural health care research.6 It is relatively easy to translate a questionnaire literally, but some translators are not necessarily conscious of the rigorous requirements of translation for cross-cultural research, therefore they may not pay enough attention to cultural nuances while maintaining the original meaning and intent.11 Terwee et al. developed quality criteria for the design, methods and outcomes of studies on the development and evaluation of health status questionnaires. Criteria were defined to yield a positive, negative or indeterminate rating. These criteria make a significant impact in defining the explicit quality standards for the measurement properties of health status questionnaires.12 All of the present questions’ ratings were well accepted during this translation process. In the French part of Switzerland, it is difficult to find bilingual translators with a health sciences background. As demonstrated in this study, there are also potential cultural and literal differences in the interpretation of many terms. This underscores the importance of achieving consensus among the research team and the translators, and the necessity of pilot testing, to ensure the new version’s fit to the original intent of the survey. If high quality translation methodologies are employed, as was the case in this study, translated clinical tools can be culturally equivalent, valid and bring awareness of relevant issues when interpreting the information obtained from the tools.13
CONCLUSION AND IMPLICATIONS For CLINICAL PRACTICE
The translated Swiss French 2020 survey is now ready to be used in the next phase of the methodological study. Using an existing survey, updating it and completing a translation and cultural adaptation of it will facilitate the understanding of nurses’ clinical reasoning on skin tears in Switzerland, enabling comparisons with other countries.
Key messages
- The seven-step method by Sousa andvRojjanasrirat provides an accepted best practices structure for translating the English version of White’s updated survey on opinions, clinical practice and the knowledgebase of skin tears among Registered Nurses into Swiss French.
- The translated Swiss French 2020 survey was culturally adapted for the Swiss French setting and was validated by students on a postgraduate wound care education programme.
- The translated Swiss French 2020 survey is now ready to assess the clinical reasoning of wound care specialists on the prevention and management of skin tears in French-speaking Switzerland.
Author(s)
Lucie Charbonneau, MSc student, RN1,2,3, Sebastian Probst, DClinPrac, MScN RN, Professor of Tissue Viability and Wound Care1
Georgina Gethin, Senior lecturer, Director of Alliance for Research and Innovation in Wounds3
1 Geneva School of Health Sciences, HES-SO University of Applied Sciences and Arts Western Switzerland, Geneva, Switzerland
2 Lausanne University Hospital, Lausanne, Switzerland · 3 School of Nursing and Midwifery, NUI Galway, Galway, Ireland
Correspondence: lucie.charbonneau@hesge.ch
Conflicts of Interest: None
References
- LeBlanc K, Campbell K, Dunk AM, Harley C, Hevia H, Holloway S, et al. [Internet]. Best practice recommendations for the prevention and management of skin tears in aged skin. Wounds Int 2018. Available at https://www.woundsinternational.com/
- Pagan M, Harvey P. Implementing a pilot skin and wound care programme in two residential aged care facilities. Wound Practice & Research. 2019; 27(4):184–92.
- Welsh L. Wound care evidence, knowledge and education amongst nurses: A semi-systematic literature review. Int Wound J 2018; 15(1):53–61.
- White W. Skin tears: A descriptive study of the opinions, clinical practice and knowledge base of RNs caring for the aged in high care residential facilities. Primary Intention 2001; 9(4):138–49.
- Scheele CM, Gohner W, Schumann H. Cross-sectional study on skin tears in fragile, aging skin: Nursing deficits in a common problem in Germany. Pflege 2020; 33(3):123–32.
- Sousa VD, Rojjanasrirat W. Translation, adaptation and validation of instruments or scales for use in cross-cultural health care research: A clear and user-friendly guideline. J Eval Clin Pract 2011; 17(2):268–74.
- Payne RL, Martin ML. Defining and classifying skin tears: Need for a common language. Ostomy Wound Manage 1993; 39(5):16–20, 22–4, 26.
- Chaplain V, Labrecque C, Woo K, LeBlanc K. French Canadian translation and the validity and inter-rater reliability of the ISTAP skin tear classification system. J Wound Care 2018; 27(Sup9):S15–20.
- Beeckman D, Van Tiggelen H. [Internet]. International Skin Tear Advisory Panel (ISTAP) classification system – French version 2018. [2018]. Available at https://www.skintghent.be.
- Cambridge University Press. Organization | signification, définition dans le dictionnaire Anglais de Cambridge 2020 [2020 Dec 29]. Available at https://dictionary.cambridge.org/fr/dictionnaire/anglais/organization.
- Sperber AD. Translation and validation of study instruments for cross-cultural research. Gastroenterology 2004; 126:S124–8.
- Terwee CB, Bot SDM, De Boer MR, Van Der Windt DAWM, Knol DL, Dekker J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol 2007; 60(1):34–42.
- Dunckley M, Hughes R, Addington-Hall JM, Higginson IJ. Translating clinical tools in nursing practice. J Adv Nurs 2003; 44(4):420–6.
