Volume 22 Number 2
Do personality and mood difficulties predict foot self-care in diabetes?
Peter Thomas Murphy,1 Aaron Liew,2,4 Brian E. McGuire,1,3 John Bogue,1 Monika Pilch,1 Sean Dinneen,3,4 Aonghus O’Loughlin,5 Anne Doherty,6 & Sínead Conneely1
Keywords diabetic foot ulcer, diabetic foot self-care, personality, depression, diabetes-related distress, illness beliefs
DOI 10.35279/jowm202107.06
Abstract
Background The literature indicates the impact of psychological factors on the development and course of diabetes remains unclear.
Aim To explore personality, depression, diabetes-related distress and illness beliefs in adults attending routine diabetes clinics and investigate whether the extent of these difficulties can predict foot self-care.
Methods Participants were consecutive patients with diabetes attending diabetes outpatient and podiatry clinics in hospitals who completed self-administered questionnaires to access personality traits and evaluate them for personality disorders, depression, diabetes-related distress, beliefs about illness and foot self-care.
Results Approximately 1 in 5 participants screened positive for Type D personality, personality disorders and diabetic-related distress; 8% screened positive for major depression. A standard multiple regression model determined whether foot self-care was predicted by these variables. The results were non-significant, F (13, 106) = 1.63, p = .09. Having macrovascular complications was significantly positively related to foot self-care (r(118) = .20, p = .027). Participants with a current and/or past history of DFU had higher BMI, longer duration of diabetes, were more likely to be on insulin therapy and to have concomitant microvascular complications.
Conclusion Personality and mood disorders are prevalent in people attending diabetes clinics, but the variables measured here do not predict foot self-care.
Implications for clinical practice Adults attending specialist podiatry/diabetes clinics need clinical pathways to mental health support.
INTRODUCTION
There is a significant body of research on the psychological factors that influence the development and course of diabetes. It has focused on recognising and addressing lifestyle changes (including diet and exercise), adherence to practice guidelines and self-management behaviours, assisting with the implementation of technological treatments (including education around the uses of glucose monitors and diabetes education) and treating mental health co-morbidities that may impact adherence to diabetes treatment.1 One complication of diabetes, and a focus for this study, is that of diabetic foot ulcers (DFUs). The individual lifetime risk of developing a DFU is 34%; 20% of moderate to severe ulcers lead to amputation, and when this occurs, mortality at 5 years is about 70%.2 Studies that have examined the prevention and management of foot ulceration in diabetes highlights the significant challenges in this area.3,4
Much of the psychological literature on DFUs has focused on associations with mental health difficulties relating to personality disorders, depression, diabetes-related distress and dysfunctional beliefs about pathogenesis and treatment. However, there is some evidence that psychological supports that help to reduce stress and negative mood are associated with better wound healing5,6 and that psychoeducational interventions may be of benefit for the prevention and management of DFUs.7–10
Personality disorders have generally been associated with suboptimal health behaviours in diabetes,11,12 but we identified only one paper that examined the relationship between personality and foot self-care.13 The study, undertaken in the Netherlands, examined Type D personality and treatment behaviours in 3314 people with Type 1 or Type 2 diabetes. The Type D Scale-14 (DS14) was used to assess Type D Personality.14 Type D personality is characterised by a combination of high levels of negative affectivity and social inhibition.14 High negative affectivity individuals are prone to dysphoria and anxiety and tend to scan the world for potential trouble,15 while high social inhibition individuals tend to keep others at a distance, often inhibit the expression of their true feelings and experience low levels of perceived social support.16 The authors found that Type D personality was associated with sub-optimal health behaviours, including a relatively low rate of foot self-care, which has the potential to increase the risk of DFUs.13
Studies looking at mood have shown that depressive symptomatology and DFUs often co-occur,17–20 and one study showed a direct association between depressive symptomatology at baseline with reduced foot self-care at (on average) 9-month follow-up,21 whilst another showed a trend for poorer adherence to foot self-care where depressive symptomology was present.18 Similarly, while diabetes-related distress is a common experience affecting approximately one in five people with diabetes,22–24 it is unclear whether the experience of distress directly impacts foot self-care; one study found that diabetes-related distress was not associated with reduced levels of foot self-care,25 but another found that diabetes-related distress was associated with reduced diabetic foot self-care.26
Individuals’ cognitions or beliefs about illness may affect adherence to treatment.27, 28 In those with a significant disease burden related to wound care,29, 30 treatment that is person-centred has the potential to have a positive effect on beliefs and behaviours and, consequently, enhance their health outcomes.3,29,31,32 One UK study that examined illness beliefs in 169 people with diabetes attending podiatry clinics found that those who reported more symptoms, greater control over treatment and who had less diabetes-related knowledge were more likely to engage in adequate foot self-care.33 The finding for diabetes-related knowledge is counterintuitive and the authors suggested that patients reporting greater knowledge may have inaccurate knowledge which could translate to poorer foot self-care. Another study found that male gender, a more recent onset of illness, taking prescribed insulin, having Type 2 diabetes (as opposed to Type 1) and the presence of macrovascular complications were all predictive of less regular preventative foot care (self-care or medical care) in diabetes.34
In this study, we aimed to examine some of the key psychological factors noted in the literature where an association with foot self-care was found.13,21,25,26,33 While these factors have been reported on individually, our aim was to examine them together, for the first time, and to explore the relative contribution of each factor to foot self-care. In this context, we hypothesised that increased symptoms of personality disorders, depression, diabetes-related distress be associated with reduced foot self-care. With regard to illness beliefs, we hypothesised that a greater sense of personal control over diabetes, a greater number of symptoms reported, and reporting less diabetes-related knowledge would be associated with higher foot self-care. In addition, we used the prescription of insulin as a putative marker of chronicity and explored whether chronicity was an indicator of the extent of psychological difficulties. We also examined whether having a history of DFU was correlated with psychological variables (personality, depression, diabetes-related distress, illness cognition).
METHOD
Design
Participants were consecutive patients with diabetes attending diabetes outpatient and podiatry clinics in hospitals who completed self-administered questionnaires to access personality traits and evaluate them for personality disorders, depression, diabetes-related distress, beliefs about illness and foot self-care. Demographic data were obtained from case files. Ethical approval was granted by the research ethics committees at the National University of Ireland Galway and Health Service Executive West, and the study was conducted in compliance with the 1964 Declaration of Helsinki.
Sample size estimation
G*Power version 3.235 was used to determine the a priori sample size for standard multiple regression with continuous predictor variables. For linear multiple regression analysis with a medium effect size (.25); α=.05; power =.95; and 13 predictor variables relating to personality, depression, diabetes-related distress, illness perceptions and the six demographic variables, a total sample of 120 participants was required.
Two diabetes clinics and a podiatry clinic in two public hospitals were used to recruit and assess participants from a catchment area serving the west of Ireland.
Inclusion and Exclusion Criteria
Inclusion criteria were age 18 years or older, Type 1 or Type 2 diabetes and attending a diabetes or podiatry clinic in County Galway, which is in the west of Ireland. Exclusion criteria were significant cognitive impairment (dementia, intellectual disability or brain injury); unable to complete the questionnaires due to English language difficulty; and any recent significant medical event or co-morbid condition, such as cerebrovascular accident.
Materials
Personality. The Type D Scale-14 (DS14) was used to assess Type D Personality.14 This allowed for comparison with the study from the Netherlands described above.13 The scale has two components to allow for measurement of negative affectivity (NA) (7 items) and social inhibition (SI) (7 items); it is self-administered, with scores on each item ranging from 0 (false) to 4 (true). The NA and SI scales each have a maximum score of 14, with a maximum total score of 28. To be designated as having a Type D personality, the respondent must score 10 or more on both NA and SI. The reported internal consistency of the scales was very good (Cronbach’s α = .88 for NA and .86 for SI) (15), and this was confirmed in adults with Type 2 diabetes (Cronbach’s α = .87 for NA and .83 for SI).36 Cronbach’s α for this study was .82 for NA and .72 for SI.
With the aim of broadening the scope of our study, we used the Standardised Assessment of Personality-Abbreviated Scale (SAPAS)37 as a brief general screening interview for personality disorders. Based on DSM-IV,38 the SAPAS assesses interpersonal skills, social isolation, trust, anger control, impulsivity, propensity for anxiety, dependency and perfectionism as indicators of personality functioning. It is self-administered and consists of eight questions that are answered ‘yes’ (score = 1) or ‘no’ (score = 0), with the exception of one item that is reverse scored. In the validation study for the SAPAS with 60 psychiatric patients in the UK, a score of 3 or more was indicative of a personality disorder. Sensitivity and specificity were .94 and .85, respectively, and Cronbach’s α for the total score was modest, at .68.37 A study to validate the instrument in a community sample recommended a cut-off score of 4 or more39; sensitivity and specificity were .69 and .51, respectively, while Cronbach’s α was .51. Cronbach’s α for this study was .50.
Depression. The Patient Health Questionnaire-9 (PHQ-9)40 was used to assess for symptoms of depression over the previous two weeks. It consists of nine items with scores that range from 0 (‘not at all’) to 3 (‘nearly every day’). Scores range from 0 to 27, and a score of 10 or more is suggestive of major depression. Cut-offs of 5, 10, 15 and 20 are designated as mild, moderate, moderately severe and severe, respectively. In the validation study from a community sample, the internal consistency of the scale was very good (Cronbach’s α = .89).40 Two studies recommend using a cut-off of ≥ 12 in a population of participants with diabetes, given the co-occurrence of symptoms such as fatigue between diabetes and depression.41,42 Cronbach’s α for this study was .77.
Diabetes-related distress. The Problem Areas in Diabetes-5 (PAID-5) is a five-item Likert questionnaire that measures current diabetes-related distress.43 The PAID-5 questions examine fear, depressed mood, worry about the future, demands of living with diabetes and coping with the disease. The questionnaire is self-administered, and scores range from 0 (‘not a problem’) to 4 (‘serious problem’), with a maximum possible score of 20. To be designated as having ‘high distress’, the response must have a total score >8. The authors reported that the internal consistency of the scale was good (Cronbach’s α = .86) (43). Cronbach’s α for this study was .80.
Illness beliefs. The Brief Illness Perception Ques
tionnaire (BIPQ) is a nine-item Likert questionnaire designed to rapidly assess the cognitive and emotional representations a person may have in relation to symptoms or an illness, including the effect on life, likely duration of illness, how much control the person has over their illness, beliefs about the effectiveness of treatment, the experience of symptoms, concern about the illness, the impact on mood and understanding of the illness.44
The BIPQ is based on the common sense model of self-regulation (CSM).27,45 Scores for each item range from 0 to 10, indicating the strength of the respondent’s belief that they can recover from or control aspects of a specified illness. The total possible score is 90. The authors did not report Cronbach’s α for the instrument. To allow comparison with previous research,33 three questions from the BIPQ were used in this study; these specifically pertained to how much a person feels they have control over diabetes (personal control), how much they experience symptoms of diabetes (identity) and their self-reported extent of knowledge about diabetes (understanding/coherence). Data for each question were treated separately in the analyses.
Foot self-care. The Summary of Diabetes Self-Care Activities Measure (SDSCA)46 is a self-administered 25-item questionnaire used to examine general diet, specific diet, exercise, blood-glucose testing, foot care and smoking. The extent of self-care activities is examined by asking on how many of the past seven days the patient engaged in the named self-care activity. This study only examined the five possible foot self-care questions from the 25-item SDSCA that ask about checking the feet, checking the insides of shoes, washing the feet, soaking the feet and drying between the toes after washing. It is designated as SDSCA (FSC) in the text. Where a total score for the SDSCA (FSC) scale is reported in the text, it is the sum of the totals out of 7 (days) for each question, divided by 5. Cronbach’s α in this study was .50.
Demographic and medical information. Four demographic/medical variables (gender, duration of diabetic illness, insulin use and macrovascular complications) identified from the literature as predicting foot self-care34 were used, as was type of diabetes and whether the participant had any history of DFU. Additional demographic and medical data were used for descriptive statistics.
Recruitment. An invitation letter and participant information sheet were sent to 186 consecutive potential participants due to attend diabetes clinic (n = 171) and podiatry clinic appointments (n = 15). Of these, 35 people with diabetes did not attend their appointments, six were excluded from the study by the consultant endocrinologist (medical reason, n = 5; English language difficulty, n = 1) and 14 individuals declined to participate, three of whom were attendees at the podiatry clinic. Recruitment continued until the target of 120 participants was reached; 108 were attending diabetes clinics and 12 were attending a podiatry clinic. Informed consent was obtained, and the questionnaires were completed.
Statistical analysis. SPSS 24 was used to examine the data. The percentage of variance in the outcome variable explained by the overall model(s), and the relative contribution of each of the variables in predicting the outcome was assessed with the use of standard multiple regression. In addition, post hoc comparisons using t-tests (with transformations where appropriate) were used for continuous variables, and Chi-squared tests were used for categorical variables to examine associations between whether participants with/without a history of DFU or chronicity were associated with the independent variables from our study.
RESULTS
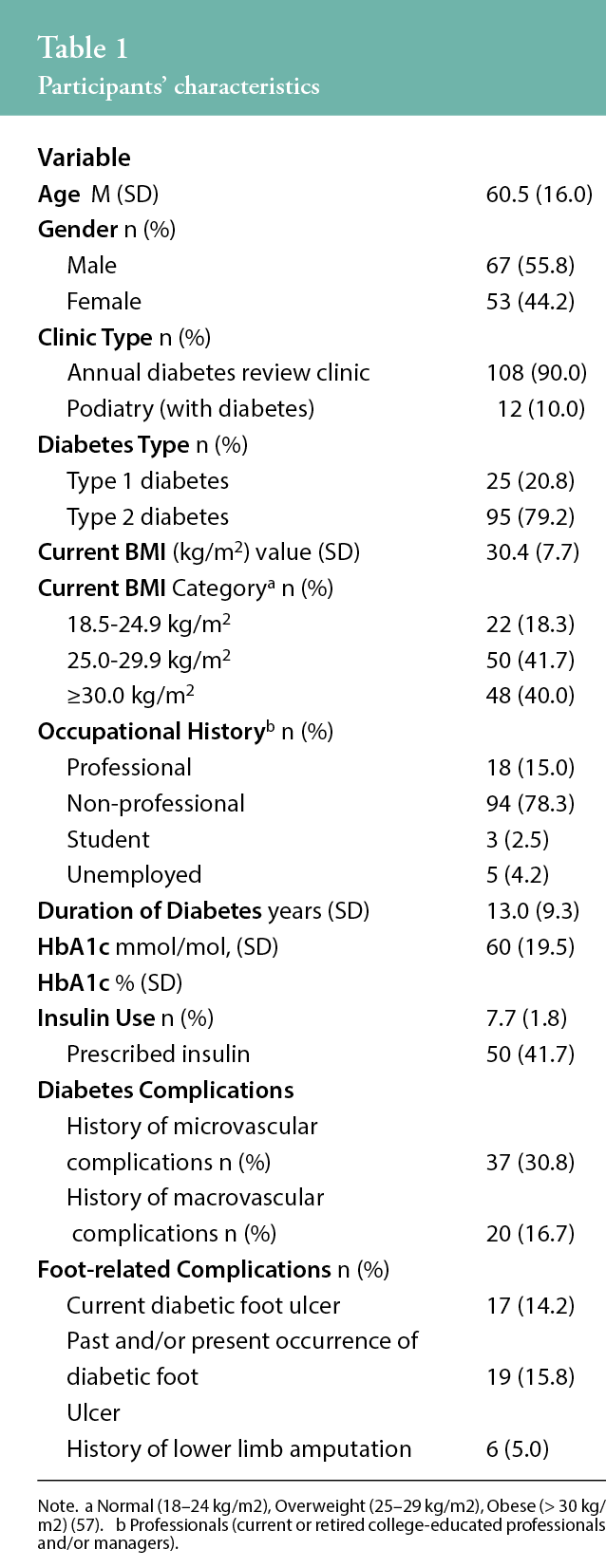
The descriptive statistics for demographic and medical data are presented in Table 1.
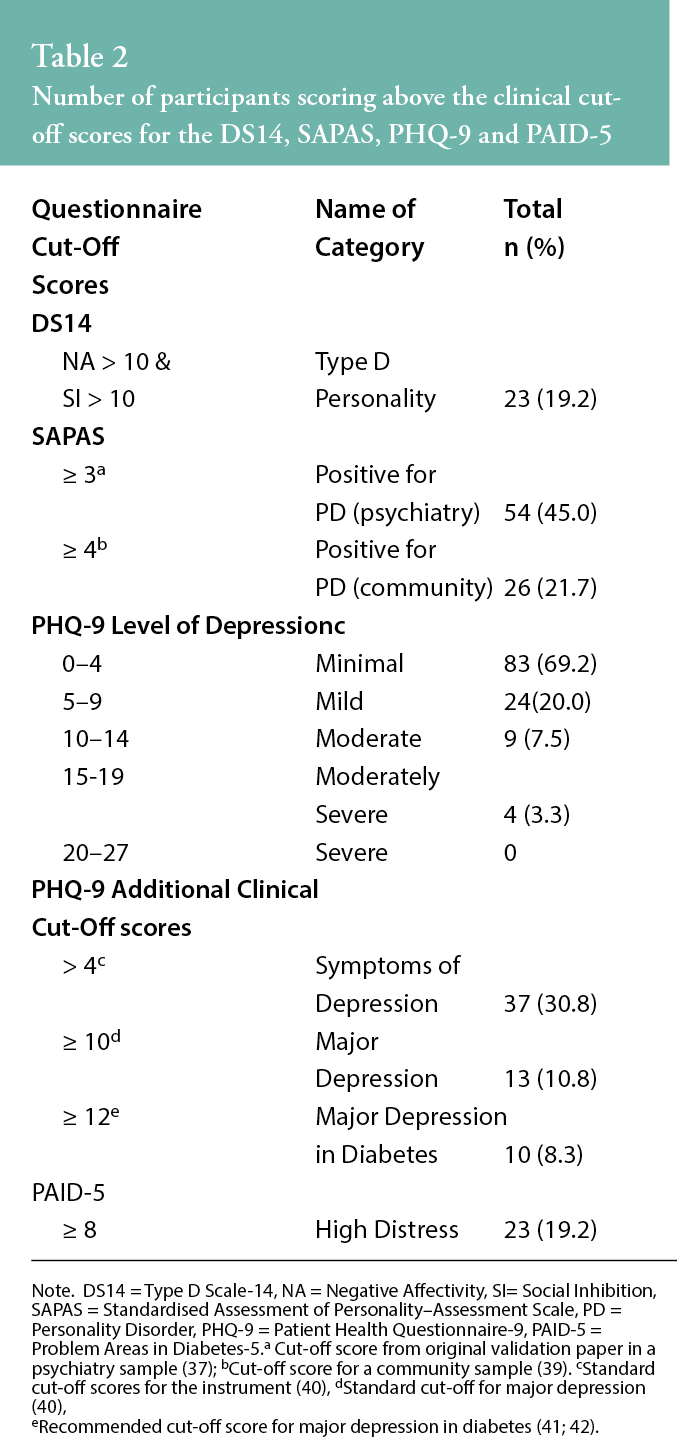
The summary statistics for participants scoring above the clinical cut-off scores for the DS14, SAPAS, PHQ-9 and PAID-5 are presented in Table 2. Of note, 19% had elevated diabetes-related distress, and 31% demonstrated some symptoms of depression (PHQ-9 > 4), with 8% screening above the cut-off for major depression in diabetes (PHQ-9 ≥ 12).
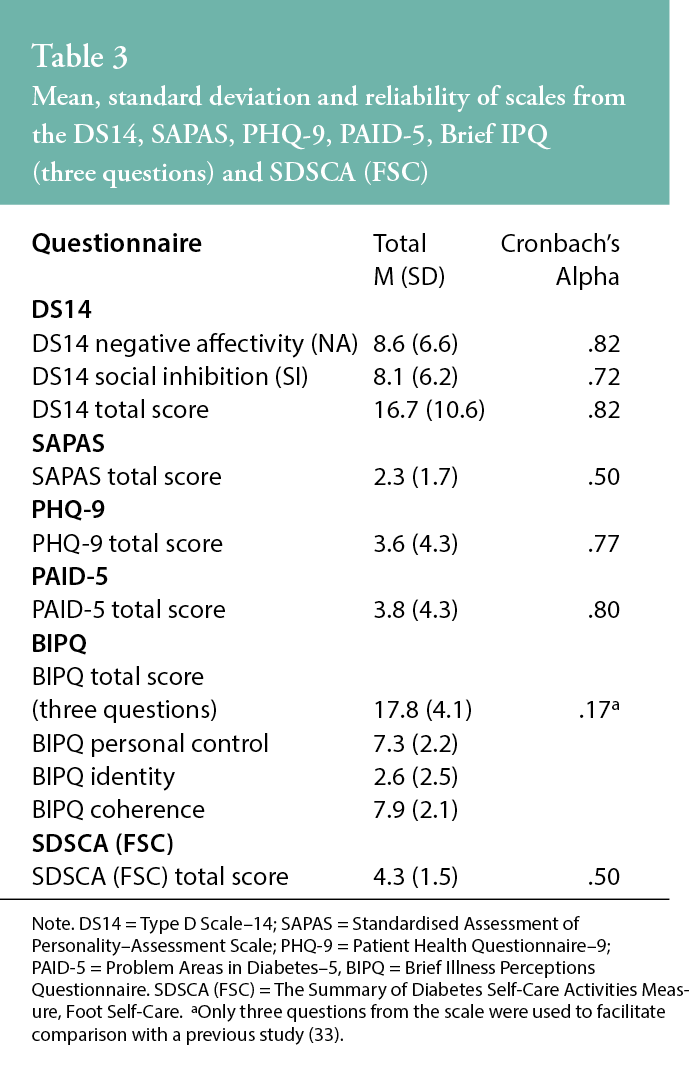
Mean and standard deviations for relevant scales and sub-scales (personality, depression and diabetes-related distress), together with Cronbach’s α, are presented in Table 3.
The number of participants scoring above the clinical cut-off scores for the DS14, SAPAS, PHQ-9 and PAID-5 are presented in Table 4.
We calculated Kendall’s tau for the association between the clinical cut-off categories for the DS14 (Type D personality), SAPAS, PHQ-9 (major depression in diabetes) and PAID-5, and there were statistically significant positive associations among all of the categories with at least p < .05 values. For example, for participants who met criteria for Type D personality (n = 23), 14 (60.9%) met criteria for SAPAS personality disorder, 11 (47.8%) met PAID-5 criteria for high distress and 6 (26.1%) met criteria for PHQ-9 major depression in diabetes. Similarly, for participants who met criteria for PAID-5 high distress, 5 (21.7%) also met criteria for PHQ-9 major depression in diabetes.
Of the demographic and medical variables, only macrovascular complications demonstrated a statistically significant relationship with foot self-care on the SDSCA (FSC) (r(118) = .20, p = .027), suggesting that the experience of macrovascular complications is associated with increased foot self-care in diabetes.
The standard multiple regression model was tested. There were no missing data, and continuous variables were used where possible; log10 transformations were undertaken where necessary. The assumptions of the model were checked in relation to multicollinearity, outliers and variables with undue influence on the model; no issues were identified.
The bivariate correlations among the variables are presented in Table 5.
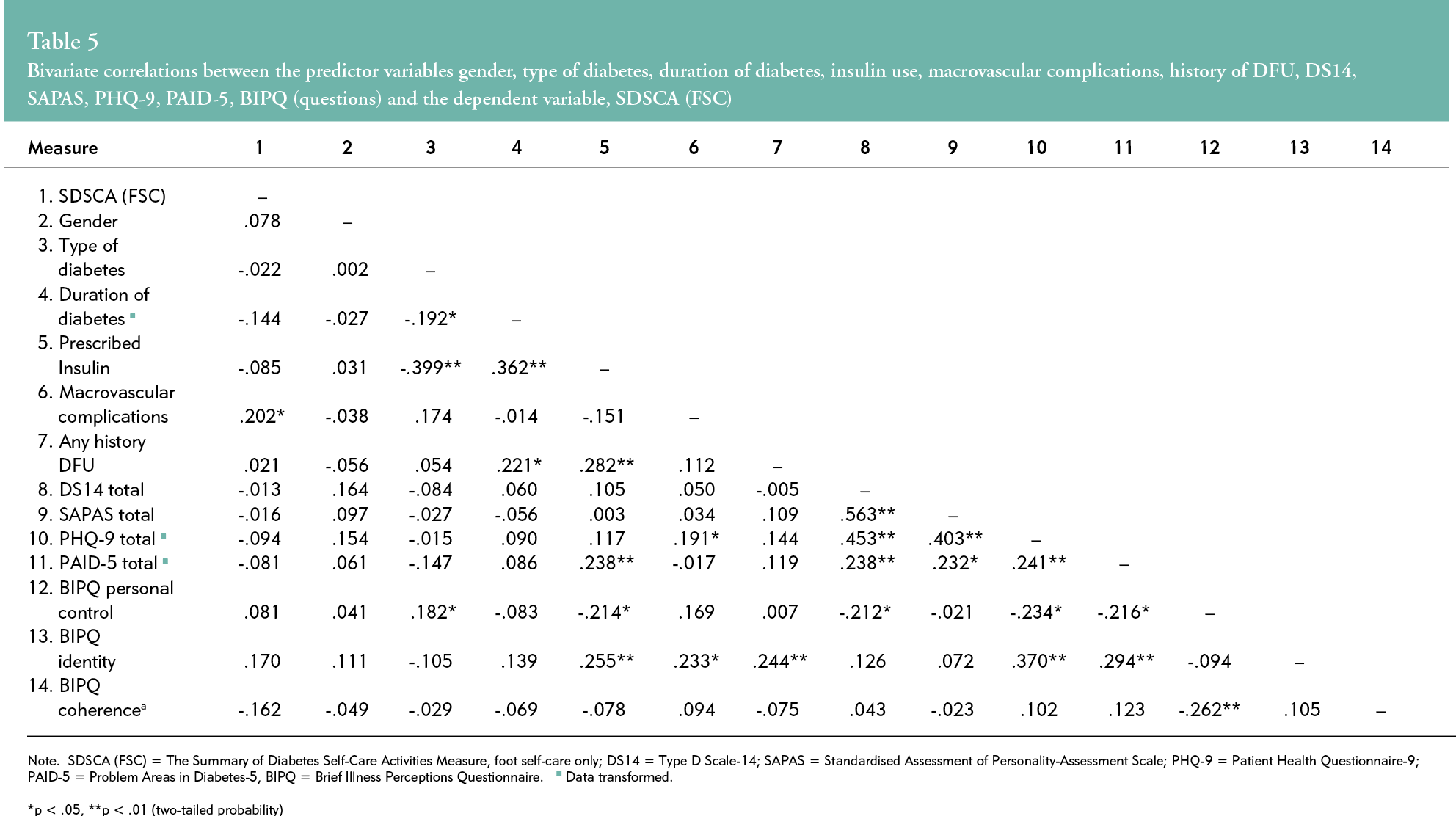
Of note, the total scores for all of the psychological variables relating to personality (Type D, SAPAS) and mood (PHQ-9, PAID-5) demonstrated statistically significant positive correlations within and among each other.
The standard multiple regression model was non-significant F (13, 106) = 1.63, p = .088, with an adjusted R2 of .064, such that 6.4% of the variance in foot self-care can be attributed to the predictor variables. Predicted foot self-care using standardized B coefficients was .09 (gender), -.12 (type of diabetes), -.16 (duration of diabetes), -.10 (prescribed insulin), .21 (macrovascular complications), .06 (any history DFU), .06 (DS14, total score), .002 (SAPAS, total score), -.21 (PHQ-9, total score), -.08 (PAID-5), -.04 (BIPQ personal control score), .21 (BIPQ identity score) and -.15 (BIPQ coherence).
Exploratory investigations examined associations among DFU history and demographic or medical variables. Participants with a current and/or past history of DFU had statistically significantly higher BMI (t (118) = -.32, p = .002) and were more likely to be overweight or obese, had a longer duration of diabetes (t (118) = -2.46, p = .015), were more likely to be on insulin therapy (χ2(1, N = 120) = 9.52, p = .002) and to have concomitant microvascular complications (χ2(1, N = 120) = 36.40, p < 0.001) (see Table 6). Of the psychological variables, only BIPQ identity demonstrated a statistically significant difference between normal and obese groups (t (118) = - 2.73, p = .007), where participants in obese categories reported greater symptoms of diabetes. There were no statistically significant differences in age, gender, occupational history, type of diabetes or HbA1c among participants with or without a current and/or past history of DFU.
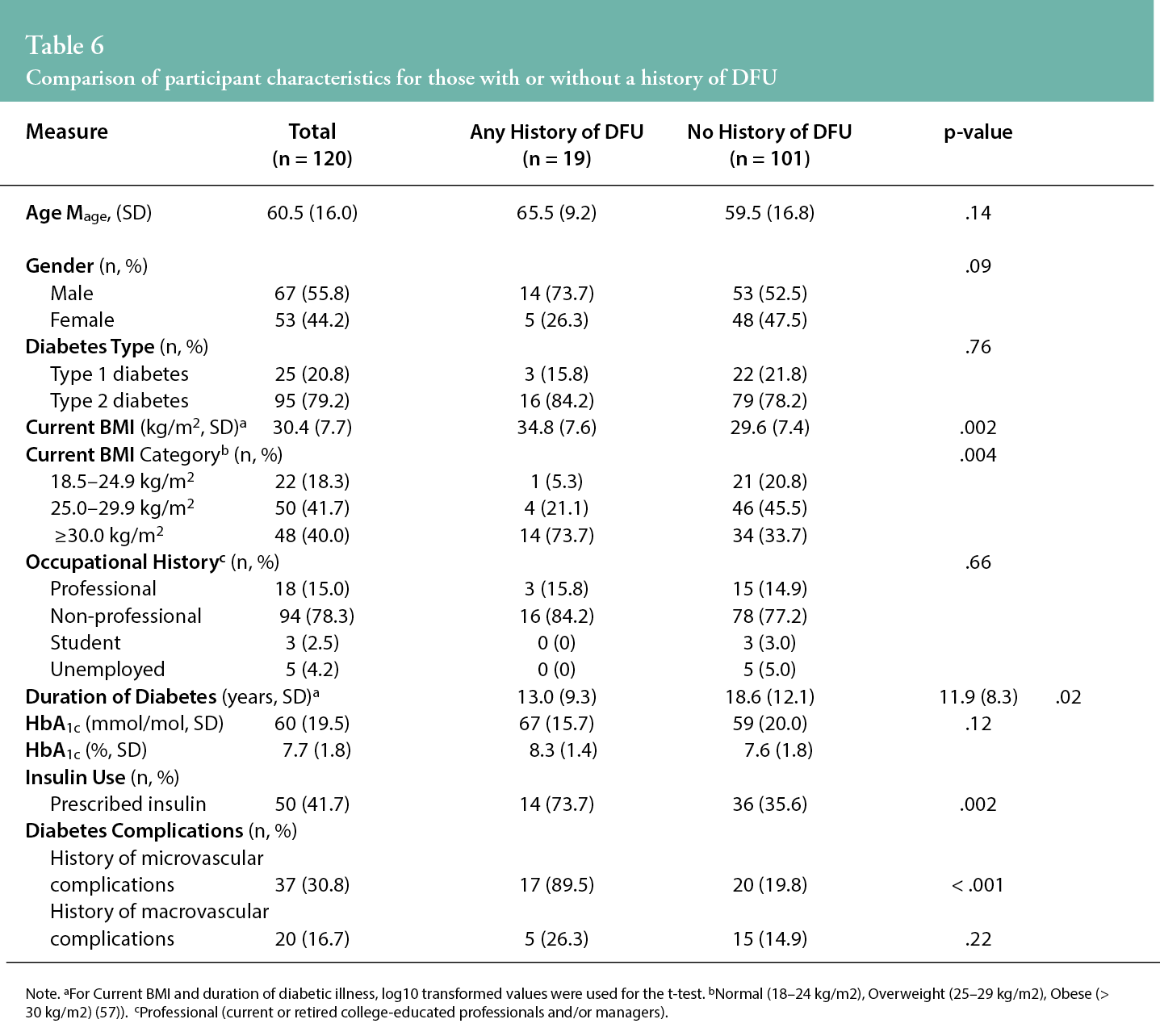
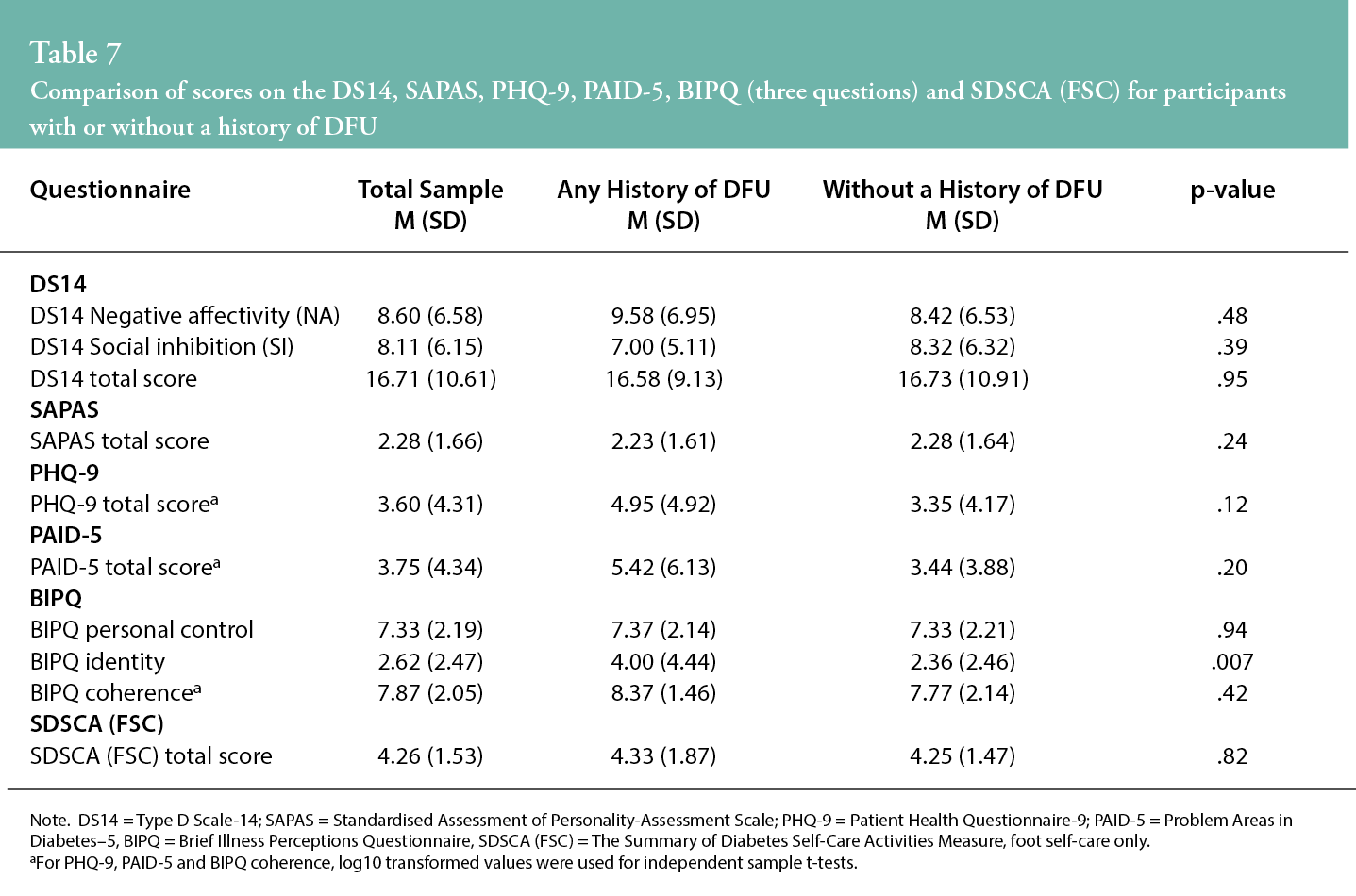
Table 7 presents a comparison between participants with and without a history of DFU in relation to continuous psychological variables. Only BIPQ identity (experience of symptoms of diabetes) demonstrated a statistically significant difference between the groups (t (118) = - 2.73, p = .007). In addition, none of the psychological categorical variables (use of clinical cut-off values from scales) demonstrated a statistically significant difference between the groups.
Participants who were prescribed insulin (n = 50) and those not taking insulin were compared in relation to DFU history. Of these participants, there were 14 with and 36 without a current and/or past history of DFU. Data were explored in relation to demographic and continuous psychological variables using t-tests and chi-square tests. Participants who were prescribed insulin were more likely to be older (t (42) = - 3.85, p < .001), male (χ2(1, N = 50) = 4.73, p = .03), have a higher BMI (t (48) = - 2.74, p = .008), a longer duration of illness (t (48) = - 2.45, p = .018) and a history of microvascular complications (χ2(1, N = 50) = 13.00, p < .001). There were no statistically significant differences for HbA1c or history of macrovascular complications. With regard to the psychological variables, there were no significant between-group differences in terms of insulin use.
Finally, the results of all two-tailed comparisons in a series of Mann-Whitney U tests between participants scoring above and below clinical cut-off scores for the psychological variables and SDSCA (FSC) were non-significant.
DISCUSSION
Some 19% of participants met criteria for Type D personality using the DS14, and the findings are broadly in keeping with the literature for Type D rates in Europe47, but lower than in a previous study from Ireland (39%)48 in which the latter population comprised college students preparing for the professions. The present sample was older, and a majority were not from professional backgrounds.
The rate of just over 20% screening positive for personality disorder on SAPAS in this study is higher than might be expected in the general population, given that epidemiological studies generally cite prevalence rates of less than 15% in the general population49 and around 10% in older age groups.50 However, this was similar to the rates found in south-east London, an area with high rates of economic deprivation.51 However, some caution is warranted when interpreting these data, as the SAPAS was not found to have a good index of reliability in our study.
In terms of depression, 31% of participants demonstrated clinically relevant symptoms of depression (PHQ-9 >4), with 8% screening positive for major depression in diabetes using a cut-off score of PHQ-9 ≥ 12.41,42 Therefore, the results are in keeping with the international literature, thus suggesting a generally strong association between depression and diabetes.52 However, due care is required in interpreting these results, given the absence of a control group in our study. Diabetes-related distress (PAID-5 ≥ 8) was found in 19% of participants, which is in keeping with the international literature.53
It is noteworthy that the screening cut-off scores for personality dysfunction (DS14, SAPAS), diabetes-related distress (PAID-5) and major depression (PHQ-9) demonstrated a statistically significant positive correlation. This suggests that individuals who score high (or low) on one of the scales will also tend to do so on the others. This points to the possibility of an underlying negative affectivity in these individuals. We found no statistically significant relationship between the psychological variables and foot self-care, which precludes focused recommendations in relation to the same. One, more general, pragmatic consideration for specialist clinics in podiatry/diabetes would be to screen for diabetes distress and depression during routine appointments. There are very brief (1- or 2-item) screening tools available for this purpose, and where scores are high, consideration could be given for a referral to general practice and/or specialist mental health services available in the local community or online. Success, in terms of mental health outcomes at one year follow-up, has been achieved in the past with this type of approach as an outcome of the Monitoring of Individual Needs in Diabetes (MIND) study.54
The hypotheses of the study were that personality, depression, diabetes-related distress, aspects of illness beliefs and relevant demographic variables would significantly predict foot self-care in patients with diabetes. Contrary to the hypotheses, the results indicate that, except for macrovascular complications, the variables chosen provided very modest contributions to the variance in foot self-care. Again, however, the measure of foot self-care was found to have a low reliability value.
The illness perception identity was found to be significantly stronger in the DFU sub-group, meaning simply that patients had a stronger sense of their symptoms being associated with their diabetes, as would be expected when one has an obvious complication known to be caused by diabetes.
Macrovascular complications demonstrated a significant positive relationship with foot self-care. Previous research from Norway found that macrovascular complications had a negative association with foot self-care.34 This research argued for the possibility that less attention was likely to be paid to preventative foot-care where macrovascular complications were a focus of treatment. The reason for this difference is unclear, but it is possible that multidisciplinary care has generally improved in recent years, or that there are regional and cultural differences in terms of areas of clinical focus; for example, the clinicians in the current study have a particular interest in foot care.
Study strengths and limitations
The cross-sectional design and the absence of a control group limits the generalisability of our findings. The study had a relatively small number of participants from a podiatry clinic in the sample, and it is possible that the patients attending the podiatry clinic could have some differences in comparison to those not attending podiatry.
In relation to the variables measured, Cronbach’s alpha values were less than .7 for the SAPAS and the SDSCA (FSC), suggesting difficulties related to internal consistency. Difficulties with low Cronbach’s alpha values are often seen in scales with a small number of items, however, and do not necessarily indicate that the scales are not useful or valid.55 It is also the case that the SAPAS was designed to screen for a wide range of personality disorders using a small item pool, and this could limit internal consistency. Nevertheless, the interpretation of these measures should be approached with caution.
Potential mediating or moderating factors relating to foot self-care were not measured in this study. These might include physical ability, perceived importance of foot self-care, previous education on foot self-care, self-efficacy in relation to self-management, general educational level, income, social support, ulcer risk status (as a prompt for more intense professional input) and the quality of patient–provider communication.29 Foot self-care itself was assessed by self-reporting; greater accuracy might be achieved in future research by asking patients to keep a daily diary of foot self-care activities.
Although psychological constructs such as depression and personality disorders were assessed using validated and widely used measures, these were not formally diagnosed using semi-structured clinician interviews, perhaps at the expense of accuracy. Other mental health conditions such as generalised anxiety disorder were not examined. Positive and potentially protective aspects of mental health were also not examined; for example, a US study found that emotional expression, that is, actively communicating about emotional experiences with others, was positively related to self-care behaviours (including FSC).56 Finally, only three questions from the BIPQ were used to allow comparison with a study from the UK,33 and this limits interpretation.
Additional investigations were undertaken looking at DFU and insulin use. Apart from experiencing more physical symptoms of diabetes, there were no statistically significant differences in the psychology questionnaire results in participants with DFU versus those without DFU; however, the number in the DFU group was relatively small. It should be emphasised that these findings are exploratory in nature and, while worthy of further of investigation with a larger sample, no definitive conclusions can be drawn at the moment.
Implications for Clinical Practice
- It is clear from our study that psychological difficulties are a significant feature of many patients presenting with DFU; consequently, pathways to mental health care, where required, are important for patients attending specialist podiatry/diabetes clinics.
- We suggest exploring the idea of routinely screening all patients for diabetes-related distress and depression. Where required, patients could be provided psychoeducational information and the possibility for an onward referral to local community or online mental health services.
Future research
- Personality disorders, depression and diabetes- related distress are prevalent in people attending specialist podiatry/diabetes clinics, but the variables measured here do not necessarily predict foot self-care.
- Future research should seek to identify specific psychological risk factors for DFU and foot self-care in diabetes, as this could facilitate the design of interventions that improve both physical and mental health outcomes for patients with diabetes.
Key messages
- It is established that medical factors such as being overweight and a longer duration of diabetes confer a significant risk of diabetic foot ulcer.
- Mood difficulties and personality disorders were common features in patients presenting to diabetic specialist clinics, and they may require additional interventions.
- Psychological variables were not identified as conferring an increased risk for foot ulcers or poor foot self-care.
- The relationship between psychological factors and diabetic foot self-care remains to be elucidated.
Author(s)
Peter Thomas Murphy,1 Aaron Liew,2,4 Brian E. McGuire,1,3 John Bogue,1 Monika Pilch,1 Sean Dinneen,3,4
Aonghus O’Loughlin,5 Anne Doherty,6 & Sínead Conneely1
1School of Psychology, National University of Ireland, Galway, Ireland
2Department of Medicine, Portiuncula University Hospital, Ballinasloe, County Galway, Ireland
3Centre for Diabetes, Endocrinology & Metabolism, Galway University Hospital, Galway, Ireland
4Discipline of Medicine, National University of Ireland, Galway, Ireland
5Podiatry Clinic, Merlin Park University Hospital, Galway, Ireland
6Department of Liaison Psychiatry, Galway University Hospital, Galway, Ireland
Correspondence: peter.murphy2@hse.ie
Conflicts of interest: None
References
- Hunter CM. Understanding diabetes and the role of psychology in its prevention and treatment. Am Psychol 2016; 71(7):515–25.
- Armstrong DG, Boulton AJM, Bus SA. Diabetic foot ulcers and their recurrence. NEJM 2017; 376(24):2367–75.
- Peters EJG, Lipsky BA, Senneville É, Abbas ZG, Aragón-Sánchez J, Diggle M, et al. Interventions in the management of infection in the foot in diabetes: A systematic review. Diabetes Metab Res Rev 2020; 36(S1):e3282.
- Crawford F, Nicolson DJ, Amanna AE, Martin A, Gupta S, Leese GP, et al. Preventing foot ulceration in diabetes: Systematic review and meta-analyses of RCT data. Diabetologia 2020; 63(1):49–64.
- Robinson H, Norton S, Jarrett P, Broadbent E. The effects of psychological interventions on wound healing: A systematic review of randomized trials. Br J Health Psychol 2017; 22(4):805–35.
- Broadbent E, Koschwanez HE. The psychology of wound healing. Curr Opin Psychiatry 2012; 25(2):135–40.
- Ahmad Sharoni SK, Minhat HS, Mohd Zulkefli NA, Baharom A. Health education programmes to improve foot self-care practices and foot problems among older people with diabetes: A systematic review. Int J Older People Nurs 2016; 11(3):214–39.
- van Netten JJ, Price PE, Lavery LA, Monteiro-Soares M, Rasmusson A, Jubiz Y, et al. Prevention of foot ulcers in the at-risk patient with diabetes: A systematic review. Diabetes Metab Res Rev 2016; 32(Suppl. 1):84–98.
- Rezende Neta DS, Vilarouca da Silva AR, Freitas da Silva GR. Adesão das pessoas com diabetes mellitus ao autocuidado com os pés. Rev Bras Enferm 2015; 68(1):111–6.
- Bus SA, van Netten JJ. A shift in priority in diabetic foot care and research: 75% of foot ulcers are preventable. Diabetes Metab Res Rev 2016; 32(1):195–200.
- Čukić I, Mõttus R, Realo A, Allik J. Elucidating the links between personality traits and diabetes mellitus: Examining the role of facets, assessment methods, and selected mediators. Pers Indiv Differ 2016; 94(Supplement C):377–82.
- Keuroghlian AS, Frankenburg FR, Zanarini MC. The relationship of chronic medical illnesses, poor health-related lifestyle choices, and health care utilization to recovery status in borderline patients over a decade of prospective follow-up. J Psychiatr Res 2013; 47(10):1499–506.
- Nefs G, Speight J, Pouwer F, Pop V, Bot M, Denollet J. Type D personality, suboptimal health behaviors and emotional distress in adults with diabetes: Results from diabetes MILES—The Netherlands. Diabetes Res Clin Pract 2015; 108(1):94–105.
- Denollet J. DS14: Standard assessment of negative affectivity, social Inhibition, and Type D personality. Psychosom Med 2005; 67(1):89–97.
- Denollet J. Negative affectivity and repressive coping: Pervasive influence on self-reported mood, health, and coronary-prone behavior. Psychosom Med 1991; 53:538–56.
- Denollet J, Sys SU, Stroobant N, Rombouts H, Gillebert TC, Brutsaert DL. Personality as independent predictor of long-term mortality in patients with coronary heart disease. Lancet 1996; 347(8999):417–21.
- Iversen MM, Midthjell K, Østbye T, Tell GS, Clipp E, Sloane R, et al. History of and factors associated with diabetic foot ulcers in Norway. Scand J Public Health 2008; 36:62–68.
- Pearson S, Nash T, Ireland V. Depression symptoms in people with diabetes attending outpatient podiatry clinics for the treatment of foot ulcers. J Foot Ankle Res [Internet]. 2014 Nov 25; 7(1):47. Available from: https://www.jfootankleres.biomedcentral.com/articles/10.1186/s13047-014-0047-4
- Steel A, Reece J, Daw A-M. Understanding the relationship between depression and diabetic foot ulcers. J Soc Health Diabetes 2016; 4(1):17–24.
- Williams LH, Rutter CM, Katon WJ, Reiber GE, Ciechanowski P, Heckbert SR, et al. Depression and incident diabetic foot ulcers: A prospective cohort study. Am J Med 2010; 123 (8):748–54.
- Gonzalez JS, Safren SA, Delahanty LM, Cagliero E, Wexler DJ, Meigs JB, et al. Symptoms of depression prospectively predict poorer self-care in patients with Type 2 diabetes. Diabet Med 2008; (9):1102–7.
- Chew B-H, Vos R, Mohd-Sidik S, Rutten GE. Diabetes-related distress, depression and distress-depression among adults with type 2 diabetes mellitus in Malaysia. PloS One. [Internet]. 2016 Mar 22; 11(3):e0152095. Available from: https://www.journals.plos.org/plosone/article?id=10.1371/journal.pone.0152095
- Schmidt CB, Potter van Loon BJ, Torensma B, Snoek FJ, Honig A. Ethnic minorities with diabetes differ in depressive and anxiety symptoms and diabetes-distress. J Diabetes Res [Internet]. 2017 Mar 8; 2017:1204237. Available from: https://care.diabetesjournals.org/content/diacare/early/2018/06/21/dc17-2181.full.pdf
- Skinner TC, Joensen L, Parkin T. Twenty-five years of diabetes distress research. Diabet Med s2020; 37(3):393–400.
- Pintaudi B, Lucisano G, Gentile S, Bulotta A, Skovlund SE, Vespasiani G, et al. Correlates of diabetes-related distress in type 2 diabetes: Findings from the benchmarking network for clinical and humanistic outcomes in diabetes (BENCH-D) study. J Psychosom Res 2015; 79(5):348–54.
- Schmitt A, Reimer A, Kulzer B, Haak T, Ehrmann D, Hermanns N. How to assess diabetes distress: Comparison of the Problem Areas in Diabetes Scale (PAID) and the Diabetes Distress Scale (DDS). Diabet Med 2016; 33(6):835–43.
- Hagger MS, Koch S, Chatzisarantis NLD, Orbell S. The common sense model of self-regulation: Meta-analysis and test of a process model. Psychol Bull 2017; 143(11):1117–54.
- Williams DM, Rhodes RE, Connor MT. Affective determinants of health behavior. Oxford: Oxford University Press; 2018.
- Matricciani L, Jones S. Who cares about foot care? Barriers and enablers of foot self-care practices among non-institutionalized older adults diagnosed with diabetes: An integrative review. Diabetes Educ 2015; 41(1):106–17.
- Olsson M, Järbrink K, Divakar U, Bajpai R, Upton Z, Schmidtchen A, et al. The humanistic and economic burden of chronic wounds: A systematic review. Wound Repair Regen 2019; 27(1):114–25.
- Gethin G, Probst S, Stryja J, Christiansen N, Price P. Evidence for person-centred care in chronic wound care: A systematic review and recommendations for practice. J Wound Care. 2020; 29(Sup9b):S1–22.
- Walburn J, Weinman J, Norton S, Hankins M, Dawe K, Banjoko B, et al. Stress, illness perceptions, behaviors, and healing in venous leg ulcers: Findings from a prospective observational study. Psychosom Med 2017; 79(5):585–92.
- Vedhara K, Dawe K, Wetherell MA, Miles JNV, Cullum N, Dayan C, et al. Illness beliefs predict self-care behaviours in patients with diabetic foot ulcers: A prospective study. Diabetes Res Clin Pract 2014; 106(1):67–72.
- Iversen MM, Ostbye T, Clipp E, Midthjell K, Uhlving S, Graue M, et al. Regularity of preventive foot care in persons with diabetes: Results from the Nord-Trondelag Health Study. Res Nurs Health 2008; 31:226–37.
- Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav Res Methods 2009; 41(4):1149–60.
- Nefs G, Pouwer F, Pop V, Denollet J. Type D (distressed) personality in primary care patients with type 2 diabetes: Validation and clinical correlates of the DS14 assessment. J Psychosom Res 2012; 72(4):251–7.
- Moran P, Lesse M, Lee T, Walters P, Thornicroft G, Mann A. Standardised Assessment of Personality – Abbreviated Scale (SAPAS): Preliminary validation of a brief screen for personality disorder. Br J Psychiatry 2003; 183(3):228–32.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-IV). 4th ed. Washington: DC: Author; 1994.
- Fok M, Seegobin S, Frissa S, Hatch SL, Hotopf M, Hayes RD, et al. Validation of the standardised assessment of personality – abbreviated scale in a general population sample. Personal Ment Health 2015; 9(4):250–7.
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med 2001; 16(9):606–13.
- Twist K, Stahl D, Amiel SA, Thomas S, Winkley K, Ismail K. Comparison of depressive symptoms in type 2 diabetes using a two-stage survey design. Psychosom Med 2013; 75(8):791–7.
- van Steenbergen-Weijenburg KM, de Vroege L, Ploeger RR, Brals JW, Vloedbeld MG, Veneman TF, et al. Validation of the PHQ-9 as a screening instrument for depression in diabetes patients in specialized outpatient clinics. BMC Health Serv Res [Internet]. 2010 Aug 12; 10(1):235. Available from: https://www.bmchealthservres.biomedcentral.com/articles/10.1186/1472-6963-10-235
- McGuire BE, Morrison TG, Hermanns N, Skovlund S, Eldrup E, Gagliardino J, et al. Short-form measures of diabetes-related emotional distress: The Problem Areas in Diabetes Scale (PAID)-5 and PAID-1. Diabetologia 2010; 53(1):66–69.
- Broadbent E, Petrie KJ, Main J, Weinman J. The Brief Illness Perception Questionnaire. J Psychosom Res 2006; 60(6):631–7.
- Leventhal H, Phillips A, Burns, E. The common-sense model of self-regulation (CSM): A dynamic framework for understanding illness self-management. J Behav Med 2016; 39(6):935–46.
- Toobert DJ, Hampson SE, Glasgow RE. The Summary of Diabetes Self-Care Activities measure: Results from 7 studies and a revised scale. Diabetes Care 2000; 23(7):943–50.
- Mols F, Denollet J. Type D personality among noncardiovascular patient populations: A systematic review. Gen Hosp Psychiatry 2010; 32(1):66–72.
- Williams L, O’Connor RC, Howard S, Hughes BM, Johnston DW, Hay JL, et al. Type-D personality mechanisms of effect: The role of health-related behavior and social support. J Psychosom Res 2008; 64(1):63–69.
- Huang Y, Kotov R, de Girolamo G, Preti A, Angermeyer M, Benjet C, et al. DSM–IV personality disorders in the WHO World Mental Health Surveys. Br J Psychiatry. 2009; 195(1):46–53.
- Mattar S, Khan F. Personality disorders in older adults: Diagnosis and management. Prog Neuro Psychiatry 2017; 21(2):22–27.
- Hatch SL, Frissa S, Verdecchia M, Stewart R, Fear NT, Reichenberg A, et al. Identifying socio-demographic and socioeconomic determinants of health inequalities in a diverse London community: The South East London Community Health (SELCoH) study. BMC Public Health [Internet]. 2011 Nov 11; 11(1):861. Available from: http://www.bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-11-861
- van Dooren FEP, Denollet J, Verhey FRJ, Stehouwer CDA, Sep SJS, Henry RMA, et al. Psychological and personality factors in type 2 diabetes mellitus, presenting the rationale and exploratory results from The Maastricht Study, a population-based cohort study. BMC Psychiatry [Internet]. 2016 Jan 27; 16:17. Available from: https://www.bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-016-0722-z
- Fisher L, Gonzalez JS, Polonsky WH. The confusing tale of depression and distress in patients with diabetes: A call for greater clarity and precision. Diabet Med 2014; 31(7):764–72.
- Snoek FJ, Kersch NYA, Eldrup E, Harman-Boehm I, Hermans N, Kokoszka A, et al. (2012). Monitoring of individual needs in diabetes (MIND)-2: Follow-up data from the cross-national diabetes attitudes, wishes, and needs (DAWN) MIND study. Diabetes Care 2012; (35):2018–132.
- Pallant J. SPSS survival manual: A step by step guide to data analysis using IBM SPSS. 6th ed. London: McGraw-Hill Education; 2016.
- Smalls BL, Walker RJ, Hernandez-Tejada MA, Campbell JA, Davis KS, Egede LE. Associations between coping, diabetes knowledge, medication adherence and self-care behaviors in adults with type 2 diabetes. Gen Hosp Psychiatry 2012; 34(4):385–9.
- World Health Organization [Internet]. Obesity and overweight. Geneva: WHO; [2021 April 1]. Available at: http://www.who.int/mediacentre/factsheets/fs311/en/.
