Volume 22 Number 2
Protecting patients’ skin during prone ventilation - the PRONEtect practice guidance document
Anika Fourie RN, IIWCC, MSc, PhD candidate1, Dimitri Beeckman RN, BSc, MSc, PGDip (Ed.), PhD, FEANS1,2,3
Keywords Prone position; prone ventilation; pressure ulcers; tissue damage; critical care; moisture-associated skin damage
DOI 10.35279/jowm202107.05
Abstract
Background Ventilating the critically ill patient with acute respiratory distress syndrome in the prone position is a lifesaving strategy, but it is coupled with adverse consequences such as the development of pressure ulcers.
Aim To develop evidence-based recommendations for critical care clinicians in a concise, simple and visual practice guidance document.
Methods A gap analysis study conducted by the Skin Integrity Research Group and the Swedish Centre for Skin and Wound Research (currently submitted to a peer-reviewed international journal) formed the basis for the practice guidance document. The gap analysis study reviewed which guidelines, equipment/devices and other digital resources were available during a systemic, comprehensive literature and digital search conducted between August and November 2020. An international expert panel reviewed the identified gaps and provided their feedback. The information from the comprehensive search provided the foundation for the design of the practice guidance document.
Findings The “PRONEtect (Prone & Protect) practice guidance document – skin care considerations for the patient in the prone position” was developed by the research team, reviewed and approved by the expert panel and then launched on public platforms in December 2020.
Conclusions The PRONEtect document’s recommendations could assist clinicians in reviewing key considerations for tissue damage prevention in patients in the prone position.
Implications for clinical practice To date, the document has been translated into eight languages, and some critical care units have updated their prone protocols according data presented in this document. This will be a dynamic document and revised as more evidence-based practices and technologies become available, specifically for prone ventilation and the prevention of tissue damage.
INTRODUCTION
Mechanical ventilation in the prone position is a life-saving therapy for the critically ill patient with moderate to severe acute respiratory distress syndrome (ARDS) and has been used worldwide since its introduction in the late 1970s.1 The Proning Severe ARDS Patients (PROSEVA) trial2 — a hallmark study published in the New England Journal of Medicine in 2013 — solidified prone ventilation as the standard of care when the results showed that an early and prolonged prone position, that is, for more than 16 hours/day, for patients with severe ARDS decreased their mortality at 28 and 90 days. At 28 days, the prone position group’s mortality rate was 16%, compared to 32.8% in the supine position group; at 90 days, the prone position group’s mortality was significantly lower (P<0.001), at 23.6%, compared to 41% in the supine group, with a hazard ratio of 0.44 (95% CI, 0.29–0.67). The efficacy of prone ventilation is due, in part, to a reduction of lung compression by the heart and abdominal organs, the reversal of atelectasis, increased homogeneous pulmonary aeration, alveolar recruitment, the minimisation of ventilator-induced barotrauma and the drainage of pulmonary secretions — all of which lead to improved gas exchange.2,3 The rapid spread of SARS-CoV-2, a novel coronavirus (also known as COVID-19),4 has resulted in an increased number of patients presenting with typical ARDS-type pathological lung changes, prompting intensive care units to adopt prone positioning.
Unfortunately, prone posturing is not free from adverse events, such as endotracheal tube obstruction, unplanned extubations, tachy- and bradyarrythmias, loss of venous and arterial access, cardiac arrests and pressure ulcer (PU) development.5 Major airway complications and PUs are the most prevalent among these complications.6 Mora-Arteaga and colleagues7 reviewed seven randomised trials (2119 patients) and found that PU development in the prone position was the most frequently observed adverse event, at 34% (OR: 2.19; 95% CI: 1.55–3.09; p<0.0001; I2 0%). The 2017 meta-analyses and systematic review by Munshi and colleagues,8 reviewing three studies2,9,10 with a total of 1,109 participants, concluded that the prone position poses a higher risk for the development of PUs compared to the supine position (RR 1.22, 95% CI 1.06–1.41, I2.0%).
When in the prone position, there is an increased risk of developing a PU because the patient remains in this position for 16 hours or longer (up to 24 hours), and without the ability to turn sideways as easily as a patient in the supine position. More bony areas and thinner, soft tissue masses (e.g., at the forehead and chin) are exposed to the sustained weight of the body while in the prone position, compared to lying dorsally. Areas most affected by prolonged pressure and shear forces in the prone position are the face, chest, genitalia and lower costal margins, iliac crest and anterior bony prominences (knees, tibial crest, dorsum of feet), including medical device-related PUs, especially due to securement devices and endotracheal tubes.11
Other threats to skin integrity while in the prone position include moisture-associated skin damage resulting from increased respiratory secretions, fever, incontinence, skin tears due to mechanical forces when repositioning the patient and medical adhesive-related skin injuries due to the multitude of tapes and securement devices.
Figures 1 and 2 are photos of patients who were in the prone position for 16 hours during the first wave of COVID-19. The patient in Figure 1 developed Stage 1 and 2 PUs on the knees, while the patient in Figure 2 developed extensive unstageable PUs on the chest. The pillows used to relieve and prevent pressure on the abdomen moved lower than the area originally intended, causing increased pressure on the chest. The author of the photos provided formal consent to use both photos for this publication.

Figure 1: Patient with Stage 1 and 2 pressure ulcers on the knees. Credit source: V. Hanssens.

Figure 2: Patient with unstageable pressure ulcers on the chest. Credit source: V. Hanssens.
Prone positioning might not be an unfamiliar intervention, but its widespread use during the COVID-19 pandemic prompted the Skin Integrity Research (SKINT) group at Ghent University (Belgium) and the Swedish Centre for Skin and Wound Research SCENTR (Sweden) to investigate (via a gap analysis study) what resources (guidelines, equipment, devices, educational tools) are available to assist clinicians in managing patients and preventing tissue damage.
At the stage of concluding the results of the gap analysis study, the second surge of COVID-19 infections started in many countries, and the research group realised that it was timely and important to immediately provide clinicians with evidence-based recommendations for the patient in the prone position. Thus, this gap analysis formed the basis for the development of the PRONEtect (Prone & Protect) practice guidance document – skin care considerations for the patient in the prone position. The goal of the PRONEtect practice guide was to provide a simple, non-text heavy, visual and concise document that included a one-page checklist for clinicians working with patients in the prone position in critical care.
METHODS
Based on the results of a gap analysis study completed at the end of November 2020, a practice guide was developed (currently submitted for peer review and publication). The gap analysis study reviewed what resources are available to prevent tissue damage to patients in the prone position using the following methods:
1. Systematic literature and digital search between
August and November 2020. An electronic database search for existing guidelines and key articles was conducted using Medline on the PubMed interface, CINAHL and The Cochrane Library. Digital searches were made to find all possible aids/tools (equipment, devices) that clinicians can use, either to assist in the prone manoeuvre or, mainly, to aid in minimising tissue damage. Media searches included YouTube videos, social media, industry websites and virtual conferences to broaden the search. If a study was found to mention a certain device, information regarding that device was gathered via the same method.
2. Evidence collection of equipment and devices.
When devices were identified that might help to prevent tissue damage, the website was searched for clinical evidence of efficacy, and if this was not found, direct email or online enquiries were made through the relevant company’s website. The aim was not to evaluate individual studies, but rather to collect the available evidence and list it according to the hierarchy of evidence.12
3. International expert consultation. Clinicians
and researchers known as experts in skin integrity and tissue viability were invited to be part of an 11-member international expert advisory panel. This group of experts’ knowledge covered both the basic science and bioengineering aspects of the issue and possessed the relevant medical/clinical expertise. A wide geographical spread (eight countries) was considered: two experts were from the United States; three were from Belgium; and one expert each was from Chile, Canada, Finland, Israel, Australia and South Africa. The role of the expert panel was to review the identified gaps, following completion of the comprehensive literature and digital review and evidence assessment by the research team during two recorded online sessions (25/26 November 2020). These sessions aimed to gather experts’ feedback, suggestions and evidence-based opinions on the current state of abdominal positioning and tissue injury prevention guidelines, equipment/devices, training and the need for future research.
Based on the results of the gap analysis study, the SKINT and SCENTR groups developed a draft practice guidance document in December 2020. The international expert group was invited to review the document in detail and to provide their feedback. Their recommendations were consolidated and, with the third round of review, all experts approved the guidance document.
RESULTS
The PRONEtect guidance document was launched publicly on social media (LinkedIn and Twitter) and on the SKINT website (www.SKINTghent.be) at the end of December 2020. The document consists of five pages explaining a 3-step procedure for preventing tissue damage i.e., 1) prepare, 2) position/reposition and 3) manage and check, with a 1-page checklist at the end summarising the recommended steps. Page 1, Figure 3 gives a broad overview of ‘key concerns’ concerning patients in the prone position, ‘considerations’, the ‘pressure points’ to be aware of (which are different to patients who are lying supine) and the introduction to the 3-step approach. According to literature5 and anecdotal testimonies,13 prone teams seem to be effective and helpful for safely repositioning patients from the supine to the prone position. A prone team usually consists of members from the operating room who are experienced with prone positioning during their daily tasks, and those specifically trained on the manoeuvre. It is suggested that medical facilities have easily available prepacked prone kits to access the needed devices (multi-layered foam dressings, alcohol-free liquid moisture barriers etc.), together with a checklist.
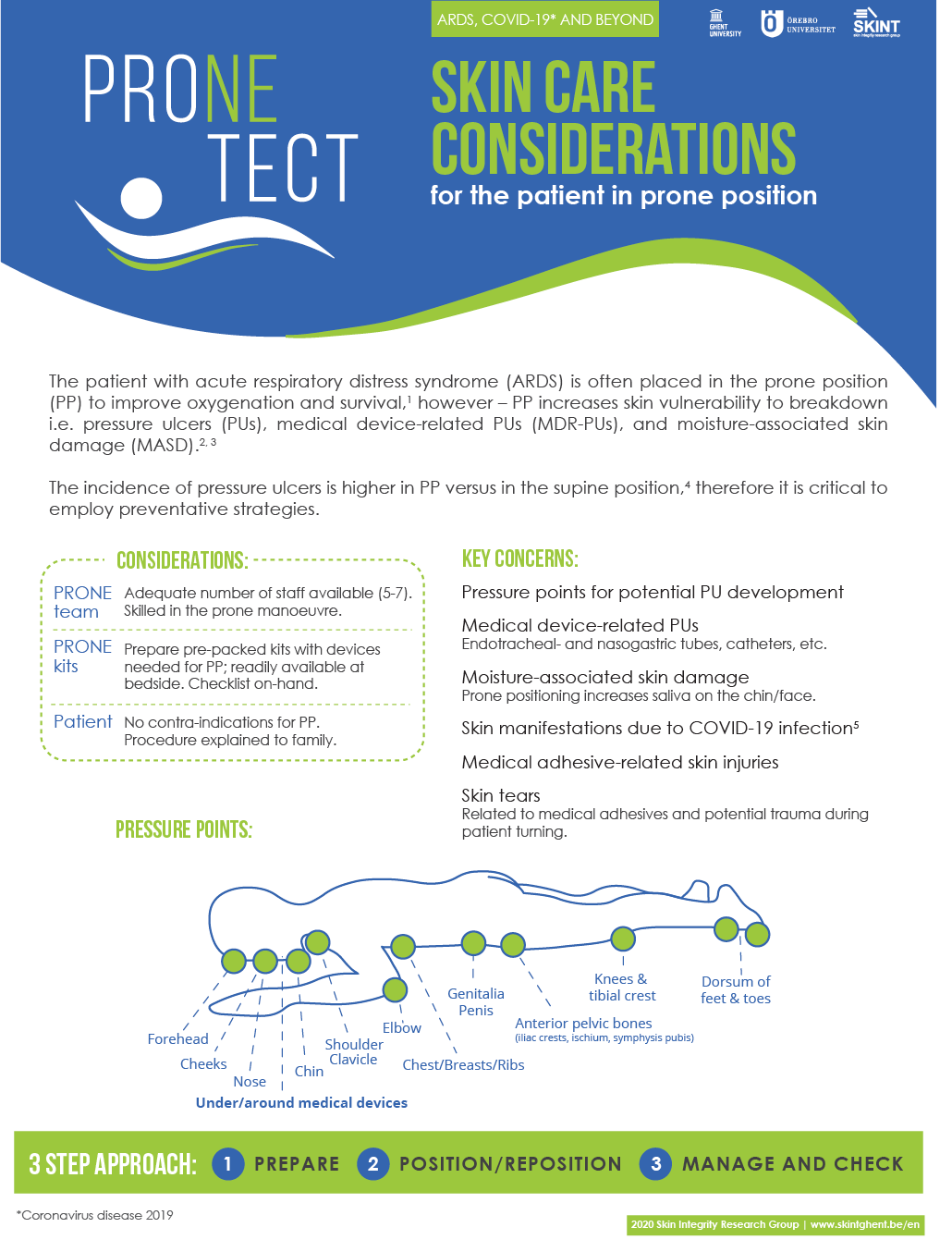
Figure 3: PRONEtect practice guidance document: Title and introductory page.
Figure 4 is a visual representation of the key recommendations before the prone man-oeuvre is performed and is based on other guidance documents,14,15 literature or experts’ recommendations. The Faculty of Intensive Care Medicine’s Guidance on Proning16 recommends the removal of endotracheal tube holders and the taping or securing of tubes with ties. If ties are used, the expert panel recommends first protecting the skin from pressure and friction. One of the benefits and consequences of prone positioning is the mobilisation of respiratory secretions; therefore, it is good practice to prophylactically protect the patient’s skin where it will be in contact with increased moisture, such as the cheeks, peri-oral and neck areas, with an evidence-based liquid barrier film.17–22 To protect the skin from epidermal stripping (adhesive-related skin injuries), the use of a liquid barrier film underneath all non-silicone based adhesives is recommended. The 2018 best practices recommendation document23 from the International Skin Tear Advisory Panel advises caregivers to moisturise the skin twice daily to prevent skin tears — with a caution not to moisturise overhydrated skin often found in the peri-anal area due to incontinence.24 Areas exposed to bodily fluids should not be moisturised, adding more moisture to the skin, but rather protected from these fluids with barrier products.
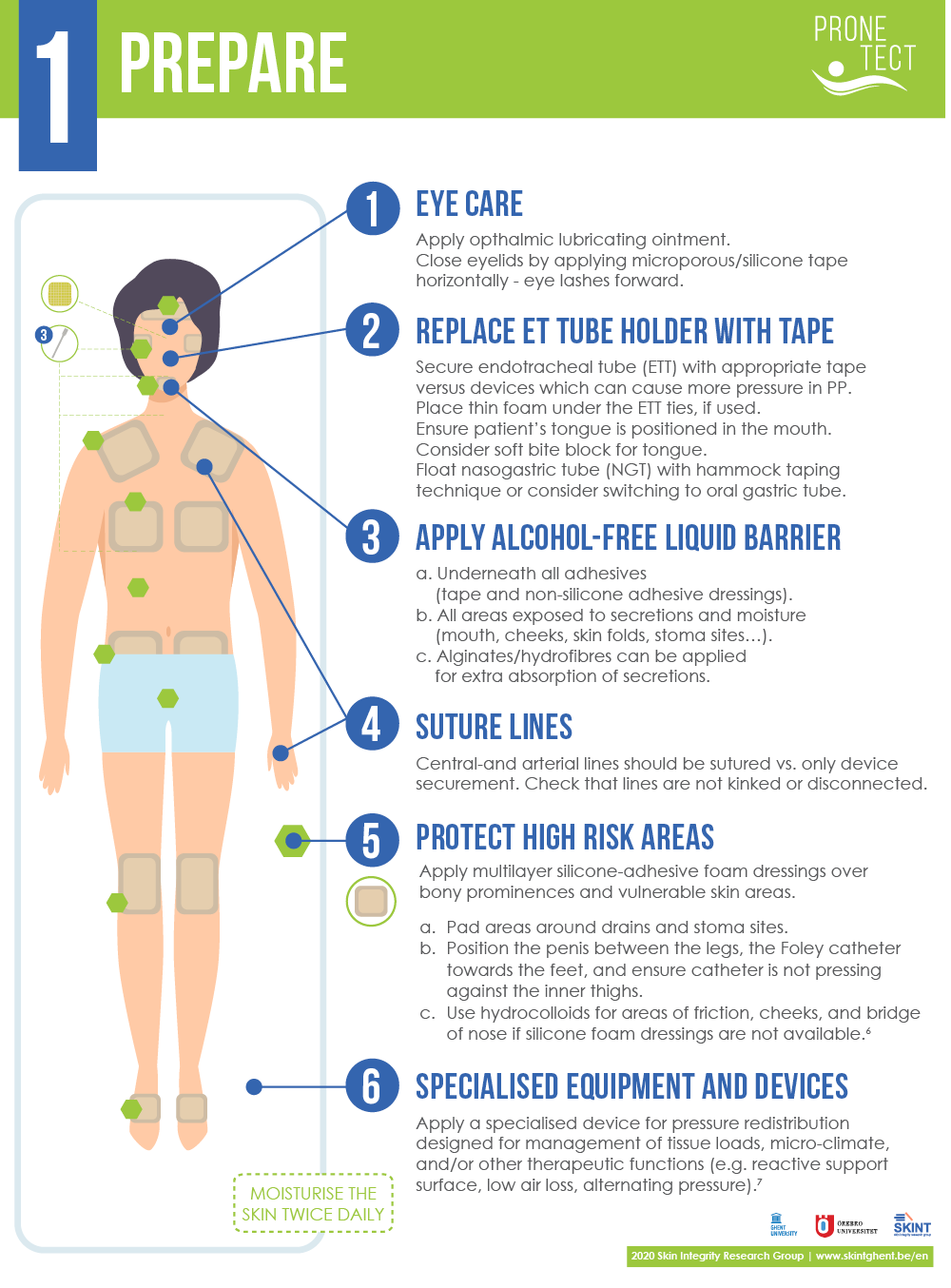
Figure 4: PRONEtect practice guidance document: Step 1 – Prepare.
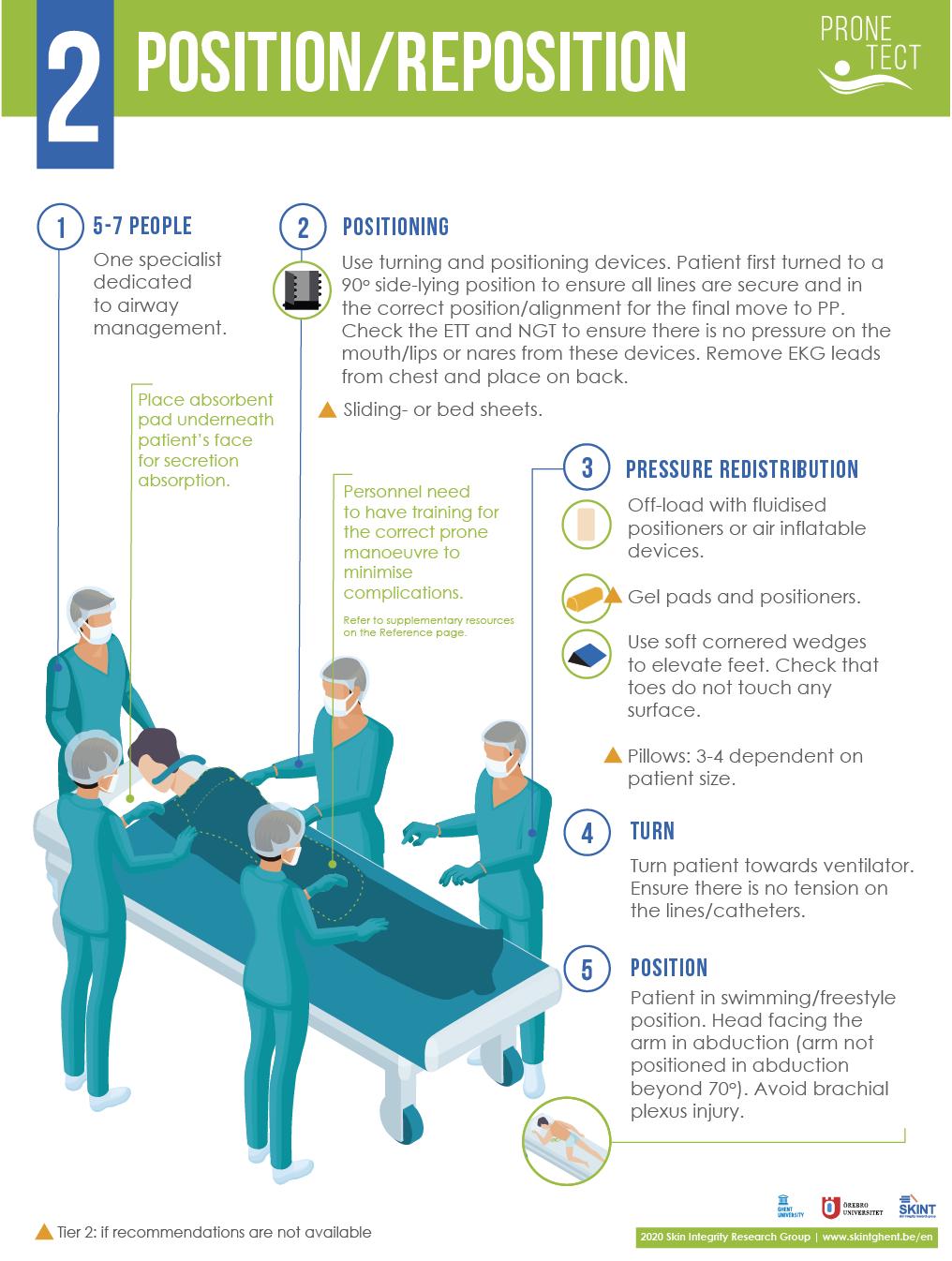
Figure 5: PRONEtect practice guidance document: Step 2 – Position/Reposition.
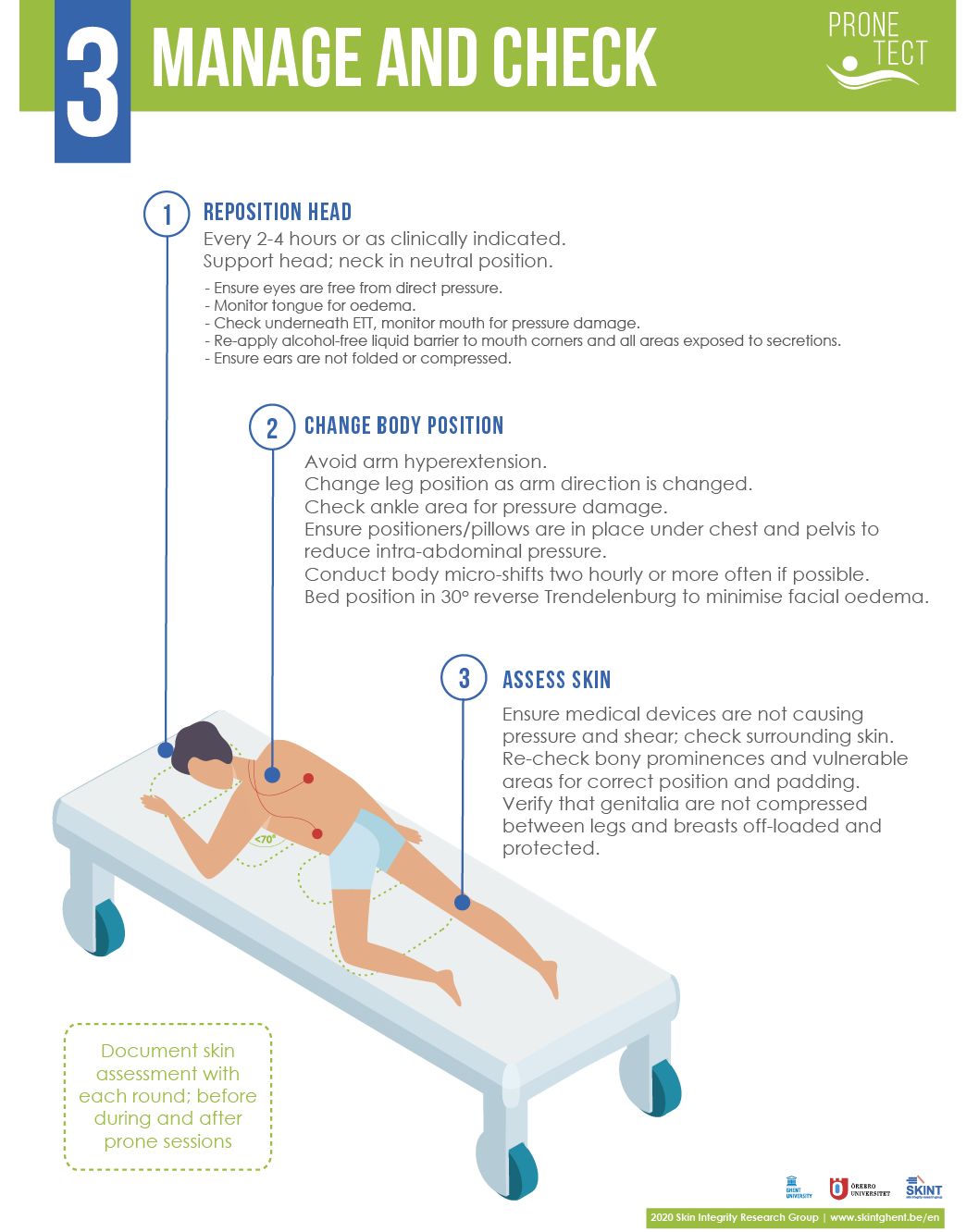
Figure 6: PRONEtect practice guidance document: Step 3 – Manage and Check.
Multi-layer silicone adhesive foam dressings can be applied over bony prominences (e.g., prominent clavicles, iliac crests, knees...) and sensitive skin areas (nipples, etc.) to protect high-risk areas. The effectiveness of these dressings in preventing PUs has been tested in several studies, but only in the supine position.25–27 A recent biomechanical study did, however, indicate a reduction of soft tissue stress exposure on the forehead (52%) and chin (78%) when multi-layered foam dressings are applied prophylactically in the prone position.28
This step provides guidance on how to position the patient in the correct way to avoid brachial plexus injury16 and offers recommendations for pressure redistributing equipment/devices. The pressure redistributing equipment/devices were added to the PRONEtect document according to the information gathered during the gap analysis and review by the expert panel. One example is a fluidised positioner consisting of viscoelastic material that can be moulded to the shape of the patient’s head or other body parts. It was evaluated for occiput PU reduction in a pilot post-test study,29 a computational modelling bench test30 and a quality improvement program.31 Pillows are traditionally used to reposition the patient when there is no access to specialist equipment in the unit and are therefore noted in the document as a Level 2 product. When positioning/re-positioning the patient from supine to prone or vice versa, a specialist (respiratory therapist, intensivist, etc.) should be responsible for airway management and will usually instruct the team on when to begin each step of the manoeuvre.
While the patient is in the prone position, regular repositioning and skin assessment are critical for preventing tissue damage, and this step highlights some key recommendations. The patient’s head should be repositioned every 2–4 hours, or as clinically indicated. During this step, the eyes, tongue, mouth and ears should be checked. Special attention is needed to review the endotracheal and oro/naso-gastric tube placement, to prevent device-related PUs. Tube rotation might be needed, as well as the replacement of wet tape or ties securing the tubes. The arm and leg position should be changed consecutively with care, so as not to hyperextend the abducted arm. A separate page is used to list key references and additional resources the clinicians can refer to, all of which are hyperlinked for easy access.
This checklist (Figure 7) summarises the 3-step recommendations in a simple manner and can be used with patients in the prone position. It can be used electronically, or if the ICU does not use electronic recording systems, it can be used as a paper-based check-off list. The ICU can create a ‘PRONE kit’ to have the necessary equipment together with this checklist in one bag.
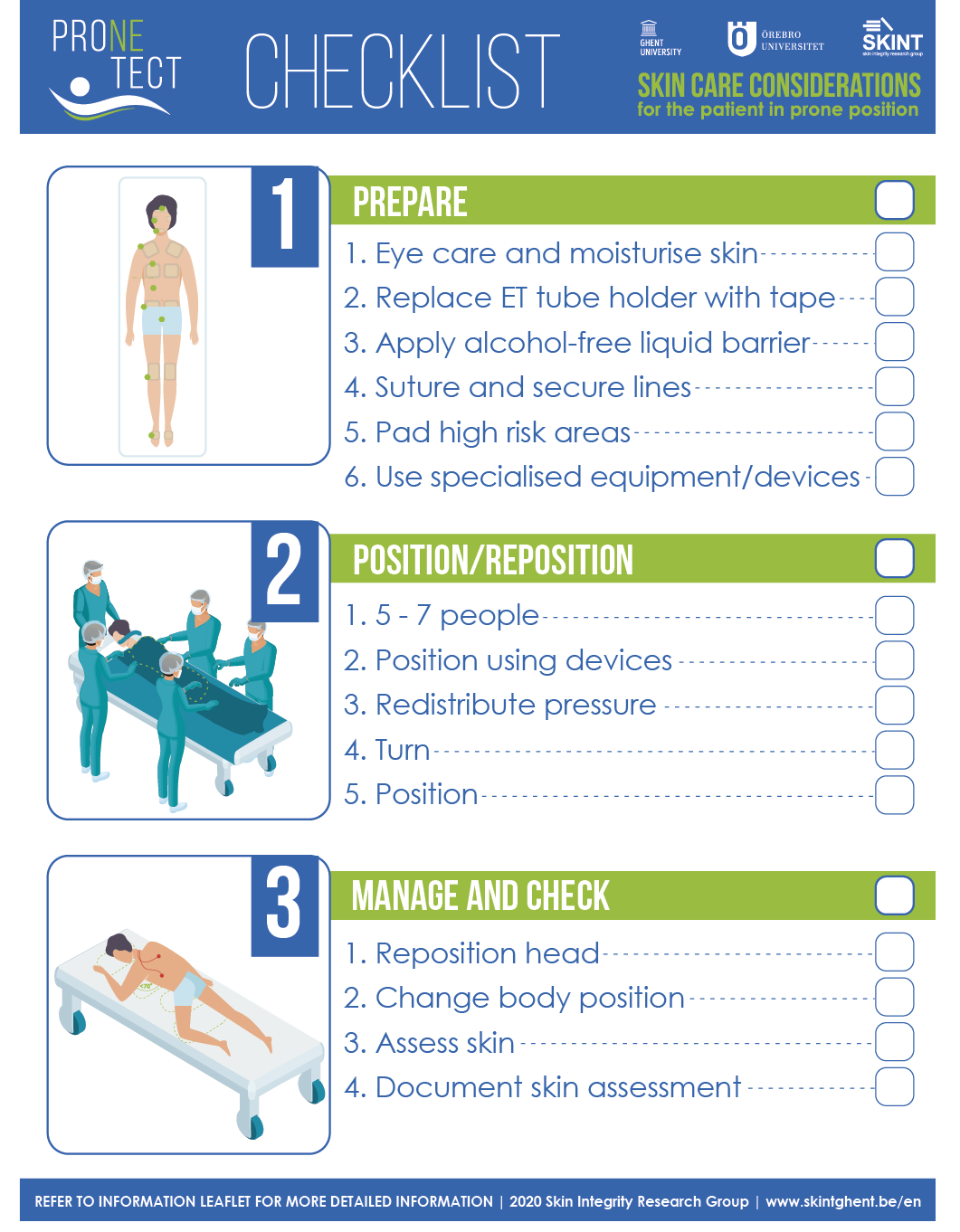
Figure 7: PRONEtect practice guidance document: Checklist.
DISCUSSION
The aim of developing the PRONEtect document was to provide clinicians with a simple and quick summary of recommendations that are evidence-based and approved by international experts.
Critical care units might or might not have prone ventilation protocols in place that are focused on tissue damage prevention. Amidst a crisis like the COVID-19 pandemic, critical care units had to adapt quickly to the increased number of prone ventilated patients, and staff were often unfamiliar with working in these settings. To accommodate the immediate need for tissue damage prevention guidance for patients in the prone position, there was not necessarily the time to search for evidence-based practices, literature and clinical practice guidelines; to appraise the evidence; to update prone protocols; and then to teach and implement it. Furthermore, due to a lack of time and staff resources during a pandemic, long didactic or online educational sessions are not feasible for adapting to the situation. The SKINT and SCENTR groups realised the necessity of providing recommendations according to what we have learned from the gap analysis study conducted in late 2020 and the feedback from experts in tissue damage prevention.
The PRONEtect document was developed based on the results of the gap analysis study. One limitation of the gap analysis was that the search period was limited (3.5 months), and it is possible that devices/devices and their supporting clinical evidence may have been missed in the digital search. There was also a dependency on searching for information on device manufacturers’ websites and their responses to requests for supporting evidence. The strength of the PRONEtect document is that it is based on a review conducted by experts in the field of tissue damage prevention, both hands-on clinicians and academic researchers. The experts reviewed both the gap analysis results and the PRONEtect guidance document in depth and provided their feedback and recommendations, all of which are aggregated in the PRONEtect document.
CONCLUSIONS
The development of the PRONEtect document is a first step following the initial stage (gap analysis) of this PRONE and PROTECT project. It is a dynamic document that will be updated as we gain further insight into technology (equipment/devices) needs, build the evidence base to support these devices and share evidence-based practices across regions.
IMPLICATIONS FOR CLINICAL PRACTICE
The research group is aware of some hospitals in Belgium that have already adapted their critical care protocols according to the PRONEtect document.
Through LinkedIn, a platform where we published this document, we have received requests from clinicians to translate the document into their local language. The document has already been translated into eight languages, and versions in Ukrainian, Russian, Romanian and Portuguese are in progress.
Future research
It is important to note that very few equipment/devices have been designed for use in the prone position to avoid tissue damage, and that availability and affordability vary by settings, region and country. Dressings, for example, have been designed for wound healing/treatment, but have not been studied extensively for the prevention of skin/tissue damage in the prone position. This provides an opportunity for further research, both for robust clinical trials with a pragmatic design and for computer modelling with three-dimensional anatomically realistic models and computer software to analyse skin and subdermal tissue loading conditions with and without specific devices.
Further research is needed to address the areas where we do not yet have sufficient knowledge about the prevention of tissue damage in the prone patient. One recommendation is to develop a competency-based assessment of critical care nurses’ training needs. A needs assessment can identify competency gaps related to this topic and guide effective and appropriate competency development for clinicians caring for critically ill patients in the prone position.
Acknowledgements
The authors wish to thank the international expert panel for their invaluable contribution to the gap analysis and practice guideline review: Maarit Ahtiala, Joyce Black, Heidi Hevia Campos, Fiona Coyer, Amit Gefen, Kim LeBlanc, Steven Smet, Kathleen Vollman and Yolanda Walsh.
Key messages
Prone ventilation is a lifesaving strategy for patients with moderate to severe acute respiratory distress syndrome (ARDS). Some patients with a COVID-19 infection develop severe symptoms like ARDS and require prone ventilation. The incidence of tissue damage in the prone position is higher than the incidence in the supine position.
It was timely and relevant to develop a practice guidance document for clinicians working in critical care settings with patients in the prone position to provide a simple, not text-heavy, visual and concise guide recommending evidence-based strategies for preventing tissue damage, such as pressure ulcers.
The PRONEtect (Prone & Protect) practice guidance document – skin care considerations for the patient in the prone position was developed based on a gap analysis study. An international 11-member expert panel reviewed and approved the document before its launch in December 2020.
Author(s)
Anika Fourie RN, IIWCC, MSc, PhD candidate1, Dimitri Beeckman RN, BSc, MSc, PGDip (Ed.), PhD, FEANS1,2,3
1 Skin Integrity Research Group (SKINT), University Centre for Nursing and Midwifery (UCVV), Department of Public Health and
Primary Care, Ghent University, Ghent, Belgium
2 Swedish Centre for Skin and Wound Research, School of Health Sciences, Örebro University, Örebro, Sweden
3 Research Unit of Plastic Surgery, Department of Clinical Research, Faculty of Health Sciences, Odense, Denmark
Correspondence: Anika.Fourie@UGent.be
Conflicts of Interest: None
References
- Piehl MA, Brown RS. Use of extreme position changes in acute respiratory failure. Crit Care Med 1976; 4(1):13–4.
- Guérin C, Reignier J, Richard JC, Beuret P, Gacouin A, Boulain T, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med 2013; 368(23):2159–68.
- Scholten EL, Beitler JR, Prisk GK, Malhotra A. Treatment of ARDS with prone positioning. Chest 2017; 151(1):215–24.
- Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med 2020; 382(13):1199–207.
- Sud S, Friedrich JO, Adhikari NK, Taccone P, Mancebo J, Polli F, et al. Effect of prone positioning during mechanical ventilation on mortality among patients with acute respiratory distress syndrome: A systematic review and meta-analysis. CMAJ 2014; 186(10):E381–90.
- Lee JM, Bae W, Lee YJ, Cho YJ. The efficacy and safety of prone positional ventilation in acute respiratory distress syndrome: Updated study-level meta-analysis of 11 randomized controlled trials. Crit Care Med 2014; 42(5):1252–62.
- Mora-Arteaga J, Bernal-Ramirez O, Rodriguez S. The effects of prone position ventilation in patients with acute respiratory distress syndrome. A systematic review and metaanalysis. Med Intensiva (English ed.) 2015; 39(6):359–72.
- Munshi L, Del Sorbo L, Adhikari NKJ, Hodgson CL, Wunsch H, Meade MO, et al. Prone position for acute respiratory distress syndrome. A systematic review and meta-analysis. Ann Am Thorac Soc 2017; 14(Supplement_4):S280–s8.
- Gattinoni L, Tognoni G, Pesenti A, Taccone P, Mascheroni D, Labarta V, et al. Effect of prone positioning on the survival of patients with acute respiratory failure. N Engl J Med 2001; 345(8):568–73.
- Chan MC, Hsu JY, Liu HH, Lee YL, Pong SC, Chang LY, et al. Effects of prone position on inflammatory markers in patients with ARDS due to community-acquired pneumonia. J Formos Med Assoc 2007; 106(9):708–16.
- Gefen A, Creehan S, Black J. Critical biomechanical and clinical insights concerning tissue protection when positioning patients in the operating room: A scoping review. Int Wound J 2020; 17(5):1405–23.
- Polit D, Beck C. Essentials of nursing research. 8th ed. Philadelphia: Lippincott Williams & Wilkins; 2014.
- Blum, K [Internet]. Nurses lead creation of ‘prone team’ to help manage patients with coronavirus who are in crisis. Baltimore, MD: Johns Hopkins Medicine; [2020 May 6]. Available at: [https://www.hopkinsmedicine.org/coronavirus/articles/prone-team.html].
- National Pressure Injury Advisory Panel [Internet]. Pressure injury prevention: PIP tips for prone positioning [2020]. Available at: [https://cdn.ymaws.com/npiap.com/resource/resmgr/online_store/posters/npiap_pip_tips_-_proning_202.pdf].
- Nurses Specialized in Wound, Ostomy and Continence Canada [Internet]. NSWOCC Best practice recommendations for skin health among critically ill patients - with an emphasis on critically ill individuals suffering from COVID-19 [2020]. Available at: [http://nswoc.ca/wp-content/uploads/2020/06/nswocc-best-practice-recommendations-for-skin-health-among-critically-ill-patients-.pdf].
- Faculty of Intensive Care Medicine and Intensive Care Society. Guidance for: Prone positioning in adult critical care [2019]. Available at: [https://www.ficm.ac.uk/sites/default/files/prone_position_in_adult_critical_care_2019.pdf]
- Hampton S. Film subjects win the day. Nurs Times 1998; 94(24):80–2.
- Bliss D, Zehrer C, Savik K, Thayer D, Smith G. Incontinence-associated skin damage in nursing home residents: A secondary analysis of a prospective, multicenter study. Ostomy Wound Manage 2006; 52(12):46–55.
- Bliss D, Zehrer C, Savik K, Smith G, Hedblom E. An economic evaluation of four skin damage prevention regimens in nursing home residents with incontinence: economics of skin damage prevention. J Wound Ostomy Continence Nurs 2007; 34(2):143–52.
- Rolstad BS, Borchert K, Magnan S, Scheel N. A comparison of an alcohol-based and a siloxane-based peri-wound skin protectant. J Wound Care 1994; 3(8):367–8.
- Sämann S. Skin protection for intensive care patients. Krankenpfl J. 1999; 37(9):328–30.
- Williams C. 3M Cavilon No Sting Barrier Film in the protection of vulnerable skin. Br J Nurs 2013; 7(10): 613–5.
- International Skin Tear Advisory Panel [Internet]. Best practice recommendations for the prevention and management of skin tears in aged skin; [2018]. Available at: [https://www.woundsinternational.com/uploads/resources/57c1a5cc8a4771a696b4c17b9e2ae6f1.pdf].
- Carville K, Leslie G, Osseiran-Moisson R, Newall N, Lewin G. The effectiveness of a twice daily skin moisturising regimen for reducing the incidence of skin tears. Int Wound J 2014; 11:446¬–53.
- Clark M, Black J, Alves P, Brindle C, Call E, Dealey C, et al. Systematic review of the use of prophylactic dressings in the prevention of pressure ulcers. Int Wound J 2014; 11(5):460–71.
- Fulbrook P, Mbuzi V, Miles S. Effectiveness of prophylactic sacral protective dressings to prevent pressure injury: A systematic review and meta-analysis. Int J Nurs Stud 2019; 100:103400.
- Ramundo J, Pike C, Pittman J. Do prophylactic foam dressings reduce heel pressure injuries? J Wound Ostomy Continence Nurs 2018; 45(1):75–82.
- Peko L, Barakat-Johnson M, Gefen A. Protecting prone positioned patients from facial pressure ulcers using prophylactic dressings: A timely biomechanical analysis in the context of the COVID-19 pandemic. Int Wound J 2020; 17(6):1595–606.
- Barakat-Johnson M, Lai M, Gefen A, Coyer F. Evaluation of a fluidised positioner to reduce occipital pressure injuries in intensive care patients: A pilot study. Int Wound J 2019; 16(2):424–32.
- Katzengold R, Gefen A. What makes a good head positioner for preventing occipital pressure ulcers. Int Wound J 2018; 15(2):243–9.
- Brennan MR, Laconti D, Gilchrist R. Using conformational positioning to reduce hospital-acquired pressure ulcers. J Nurs Care Qual 2014; 29(2):182–7.
