Volume 23 Number 2
Skin Tears in an aging population: Workforce empowerment - Evaluation of a First Responder Skin Tear Wound Management Pack
Chloe Jansz, Annette Ross, Sonja Cleary
Keywords skin tears, Keywords: Aged care wound management, first responder pack, unregulated worker
DOI 10.35279/jowm2022.23.02.03
Abstract
Skin tears are defined as a break in the skin greater than 2cm, also known as cuts, lacerations, grazes or skin tears. Skin tears can occur in many different scenarios, such as a mechanical fall or incidental shear or friction and are most common in the elderly population.2 The correct dressing choice is required to address coagulation status, infection risk, wound product wastage, pain and quality of life management for the resident. Sussman and Ryan (2019, p. 11)9 issued a statement to the Royal Commission into Aged Care Quality and Safety Royal Commission on behalf of Wounds Australia (2019) and noted that ‘The major risks of the use of inappropriate dressings are: delayed healing, wound deterioration, potential infection, pain and stress to the consumer. The impact on cost of treatment of using inappropriate products is significant’.
There are various products in place at present in the aged care sector to manage skins tears. Currently, these options require the skilled nurse to use an aseptic technique and a combination of various products, as well as a dressing pack, to address the complexity of the aging skin. This study evaluated the introduction of a First Responder Skin Tear Wound Management Pack (STWMP). The primary aim of the eight-week project, applied across four aged care sites, was to evaluate the implementation of a first responder STWMP in which any health care worker could apply the correct regime, decreasing the risk of progression of a skin tear to a chronic or complex wound.
The results showed a reduction in skin tear time, therefore an increased rate of healing and reduction in staff time, all creating a reduction in the burden of disease that skin tears have in the aged care sector. In addition, it highlighted some design features and early data to inform further research into the impact of pre-education and socialisation of the first responder STWMP in practice. The first responder STWMP clearly has the potential to promote best and early practices for all residents’ skin in a multidisciplinary team with a resident-centred approach.
INTRODUCTION
The International Skin Tear Advisory Panel’s (ISTAP) 2018 definition of a skin tear is ‘a traumatic wound caused by mechanical forces, including removal of adhesives. Severity may vary by depth (not extending through the subcutaneous layer)’. 1 (p. 2, para. 1) Skin tears can occur for a number of reasons, including: getting up during the night, low lighting, not having the appropriate mobility aid, changing environment from home to care, other people causing the fall, decreased muscle tone, altered gait or decreased range of ankle motion.2
Skin tears were once classified in stages; more recently, based on ISTAP’s classification system1, the stages have been simplified to aid in the assessment of a skin tear into three distinct types (Figure 1).
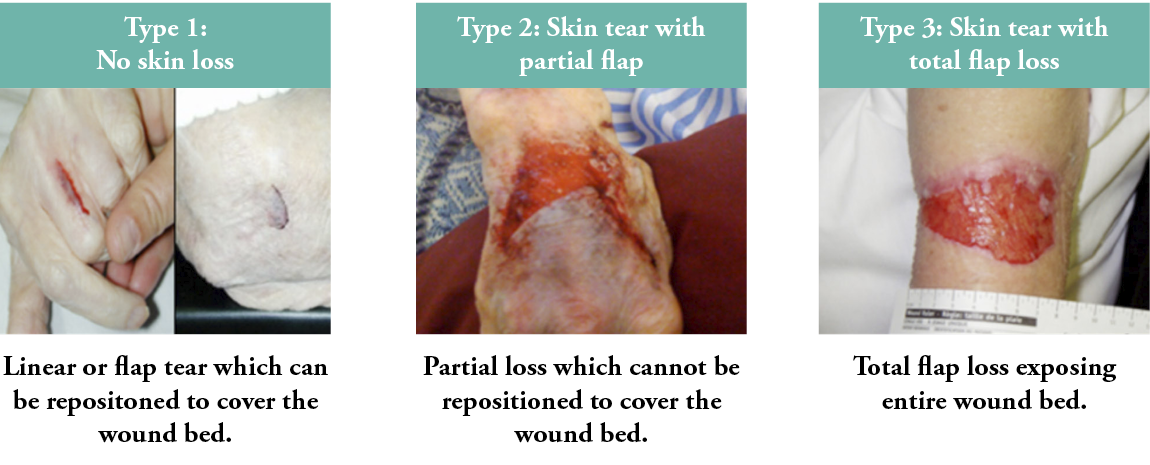
Figure 1: The International Skin Tear Advisory Panel’s classification system
Applying these types enables the care provider to categorise the skin tear correctly, in a timely manner and to apply the appropriate treatment.2 Early assessment and intervention reduces the risk of infection and the potential for continuation into a complex chronic wound.3
Early prevention and treatment
Early prevention and treatment of skin tears is multi-factorial and centred around three key concepts: skin care, skin tear education for staff and skin tear wound assessment and management.2,3 Skin care relates to decreasing the risk of skin tears, which may occur when completing tasks such as personal care needs and meal assistance.4 Skin tear education is centred around staff members being provided education on skin care and their being able to recognise residents who may be at potential or actual risk of a skin tear.5–7
All of these concepts should be evident in policies and procedures, particularly within an aged care facility where there is an increased risk of skin tears occurring. However, implementation of the correct assessment and management of a skin tear, in a timely manner, as reflected in these policies can be impacted by available resources, particularly the nursing workforce.
Personal care attendants, more commonly referred to as ‘unregulated workers’, are now the predominant workforce in the aged care sector in Australia, where this study was conducted. This group of workers has not previously been empowered or educated either to assess or dress wounds. Instead, they are required to report to a nurse (a regulated worker), which can delay the assessment and management of wounds by hours, if not days, in some instances. A key consideration in skin tear management is prompt attention to reduce the chance of a skin tear becoming a chronic wound.4
The economics of skin tears
There is currently a deficit of suitable regulated staff resources to undertake the early prevention and management of skin tears;3,4 this poses a great burden on already-stretched economic resources, particularly in the aged care sector. A study by Rando et al.3 in 2018 estimated that the cost of managing a skin tear using a standard dressing approach of an antimicro-bial iodine gauze, non-adherent pad and adherent clear film, or a crepe bandage, was approximately $65.53 AUD (based on seven dressing changes), compared to the use of a hydro-responsive wound dressing, which was $28.21 AUD (based on four dressing changes). These costs were inclusive of both the nurses’ time and dressings required for the duration of skin tear healing.
More recently, Rayner et al.8 examined the healing time and dressing costs of skins tears and found that cost variations are dependent on the presence of a haematoma under a skin tear flap. The cost of dressings alone for skin tears with a haematoma was estimated at $21.19 AUD, versus $13.68 AUD without a haematoma; this estimation did not include labour costs. This is important to consider, as haematomas are a common complication of skin tears.4
To meet the escalating demands and increasing costs in the aged care sector, there has been a move to change the skill mix of staff, favouring lower-cost unregulated healthcare workers.13 This change has been compounded by the COVID-19 pandemic in Australia9 The reality of these changes has had a number of consequences, including a timely first aid response when a skin tear occurs. Existing evidence suggests that, if skin tears are inappropri-ately dressed or left untreated, it can result in a chronic wound or infection.2 Therefore, it was identified that there was an urgent need to seek a solution that empowers unregulated healthcare workers, as they are often the first person to encounter a skin tear, so that they may act in a ‘first response assessor’ role to initiate management within the first 72 hours of the skin tear occurring.
Various products are used in the aged care sector to manage skin tears. This project is the first step in an implementation study that evaluated the introduction of a first responder Skin Tear Wound Management Pack (STWMP), to upskill the unregulated workers in the aged care sector with a view to improving healing rates. This article presents the results of the implementation of the STWMP in four aged care facilities in Australia.
Aim of the study
Currently, all aged care facilities within the consortium where the authors are based have a skin care policy in place to inform the assessment and management of skin tears. Therefore, treatment of a resident with a skin tear would routinely occur as per the facilities’ existing skin tear guidelines, which were last updated in 2020. This project introduced a first responder STWMP to identify the impact on outcomes across different aged care facility sites. The primary aim of the project was to implement a unified first response skin tear wound treatment protocol that any healthcare worker could apply promptly after a skin tear occurred. The intention was to prevent infection and the progression of a skin tear into a chronic or complex wound.
METHOD
The theoretical methodology that underpinned this project was implementation science11, the framework of which is based around the clarification of pathways or the integration of new practices into a clinical setting.12 Such was the case for this study, which sought to embed best practices in terms of undertaking an assessment when a skin tear has occurred and the implementation of a first-response treatment to reduce the risk of further complications.
Implementation science can promote improvements to care and ensure that policies surrounding healthcare remain up-to-date and rooted in evidence-based practices.11 Figure 2a shows the process of implementation, while Figure 2b represents the information as applied to this study.
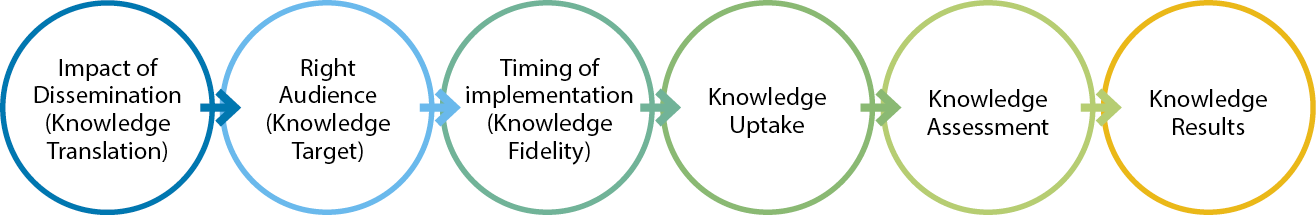
Figure 2a: The science of implementation phases
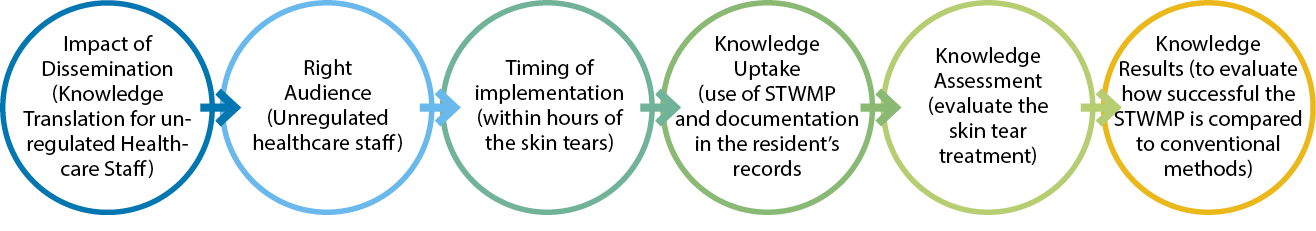
Figure 2b: The science of implementation phases using the STWMP
Site recruitment
Recruitment for this audit was from four aged care facility sites: South, Central, Rural and North, which are part of an overarching consortium in Australia. The Rural and Central facilities were the largest, with 200 beds each; the South and North were smaller, with 100 beds per site. These facilities were chosen because they represent different demographic mixes of residents, including gender. The age range of residents across the sites was 70–100 years old. At the time of the study, all sites had 100% occupancy rates.
Audit criteria
Inclusion criterion:
The only inclusion criterion was being a permanent resident in an aged care facility.
Exclusion criterion:
The only exclusion criterion was being a respite resident in an aged care facility. The exclusion of respite residents was related to the inability to track their progress over the duration of the study, as the average length of respite care is in two-week blocks, while the study period was eight weeks.
Intervention
First responder Skin Tear Management Pack
The STWMP packaging was designed to include on one side the steps of how to use the contents and document the skin tear. The other side of the packaging featured a pictorial diagram of the ISTAP classification system.1 The pack’s ‘user’ was required to examine the skin tear to determine if the first responder STWMP was appropriate for use in the first instance. Ideally, this was done within the first hour after the skin tear was identified.
The ISTAP (2018) guide suggests that an assessment of the viability of a skin tear flap’s re-approximation should be determined as soon as possible following the injury. It was envisaged that prompt use of the STWMP could ensure best practices for skin tear management by providing information in a simple and user-friendly way.
The contents of the STWMP included a calcium alginate dressing as the primary product, chosen for its coagulation properties and a foam dressing for protection of the wound and its non-adherent pro-perties, to reduce further trauma to the skin. A non-touch aseptic wound dressing pack was also included, to reduce the risk of infection.2,3,10
The STWMP packaging included instructions suitable for use by both registered/enrolled nurses (not specialised in wound care) and non-regulated workers. Figures 3a and 3b show the information provided on both sides of the package.
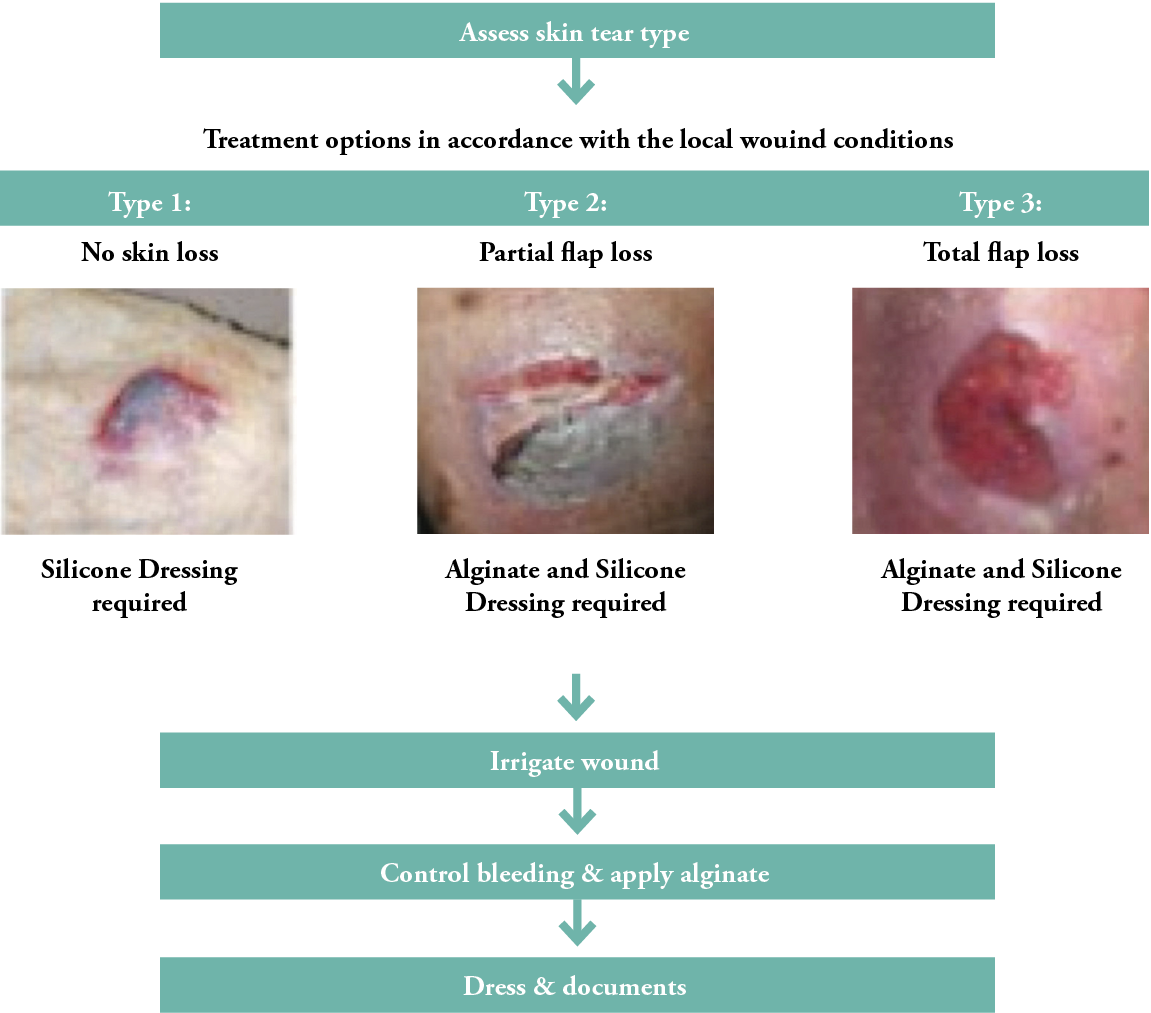
Figure 3a: Front side of the STWMP
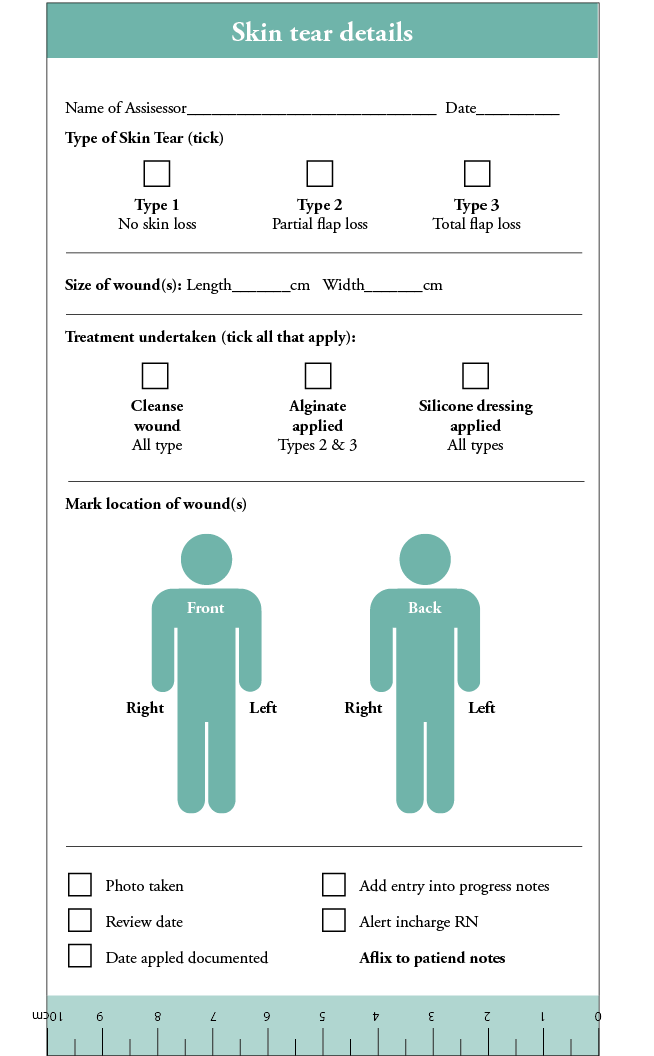
Figure 3b: Back side of the STWMP
Procedure
Each of the four aged care facility sites, South, Central, Rural and North, were considered to be a ‘cohort’. The assignment of the cohorts was undertaken at random by drawing the site names out of a hat by someone unrelated to the research group.
- The North site was given the STWMP pack with an instruction sheet on the use of the pack, but no education.
- The South site was given education only related to the contents of the STWMP.
- The Rural site was given comprehensive general skin tear wound management education, information on using the ISTAP guidelines and specific guidance on the application of the STWMP if a skin tear occurred, along with an explanation of the first responder STWMP’s instructions.
- The Central site was the control arm and continued to follow the current skin tear protocol that the facility already had in place. The only addition was that the STWMP was stored in the same location as the existing wound management products.
Data collection
The project collected data using electronic clinical software (eCase) that has been in use at the aged care facility sites since 2017. Data collection took place over a four-month period, from January 2021 through February 2021 (pre-study) and May 2021 through June 2021 (implementation phase).
All incidences of skin tears in the facilities were recorded in the electronic medical record system eCase, as per the facilities’ usual process. The data collected from the electronic medical records included data across the whole facility and the intervention sites. The data included the incidence of skin tears by type (1, 2 or 3), the dressings used initially when a skin tear was found and how many days a skin tear type was present.
Of note, the facilities all had an existing skin tear policy that had been in use for at least one year prior to the commencement of this project.
Ethical approval
Approval to conduct the project was granted by the Quality Committee of each aged care facility. The STWMP was approved by the Australian Register of Therapeutic Goods, ARTG number 362914.
RESULTS
Table 1 shows the ratio of unregulated and regulated staff to residents in the four facilities.
Table 1: Ratio of unregulated workers to regulated staff, per shift
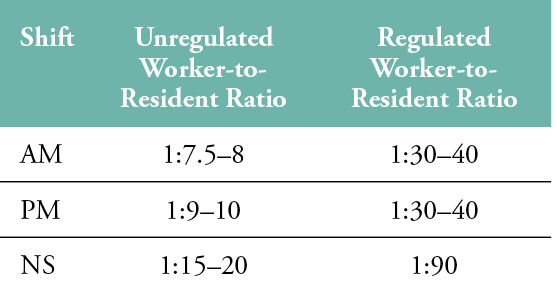
Ratios were dependent on resident acuity. The data shows that there are more unregulated workers in an aged care facility at any one time attending to residents’ care than there are regulated workers.
Skin tear data
Table 2 shows the incidence of skin tears in each aged care facility prior to and during the period when the first responder STWMP was available. Bold and italic text indicate the four sites where the first responder STWMP was introduced in May–June 2021. The data shows that the main reason reported for skin tears was related to falls. The study sites mirrored the entire consortiums trend, all being that falls were the main contribution.
Table 2: Skin Tear Incidence
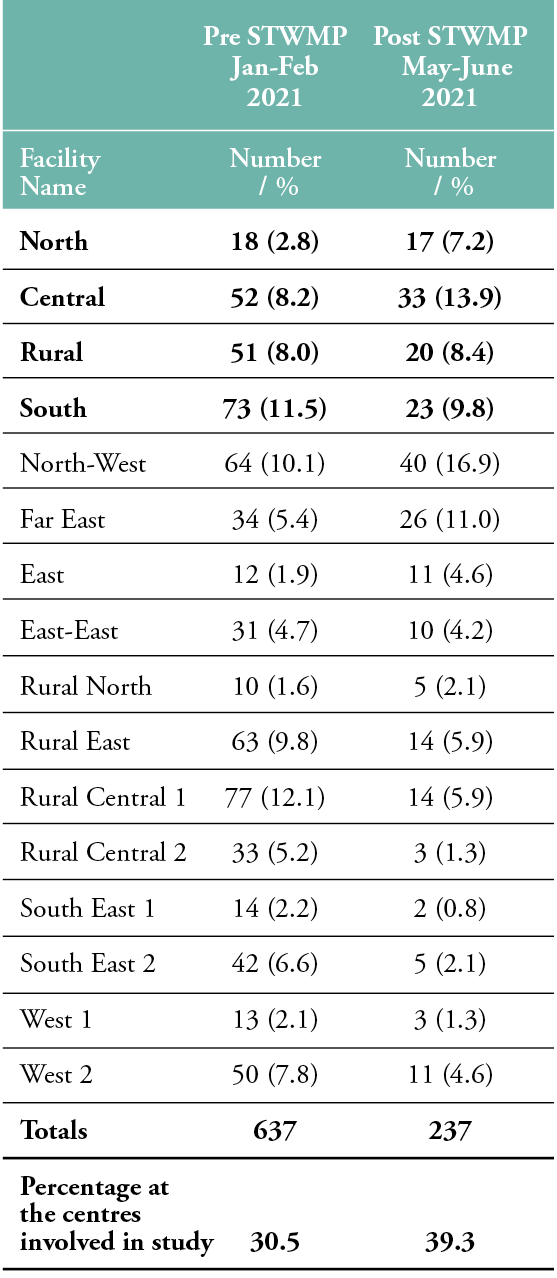
During the audit pre-intervention period, from January through February 2021, there were 637 skin tears, compared to 237 during the intervention phase, from May through June 2021. The percentage of the cases across the study cohort facilities represented 30–39% of the total number of cases across the aged care consortium.
Table 3 shows the documented causes of skin tears from the pre-intervention audit. This was used to inform the comprehensive education arm for staff at the rural site. For the 637 cases documented in January and February 2021, the causes of skin tears included: falls (n=205), self-inflicted (n=159), friction/shear (n=133) and other (n=140). Self-inflicted events were those witnessed by staff, such as residents scratching themselves. The facility defined ‘other causes’, as the default if staff could not identify the reason for the wound.
Table 3: Skin Tear Causes, January–February 2021
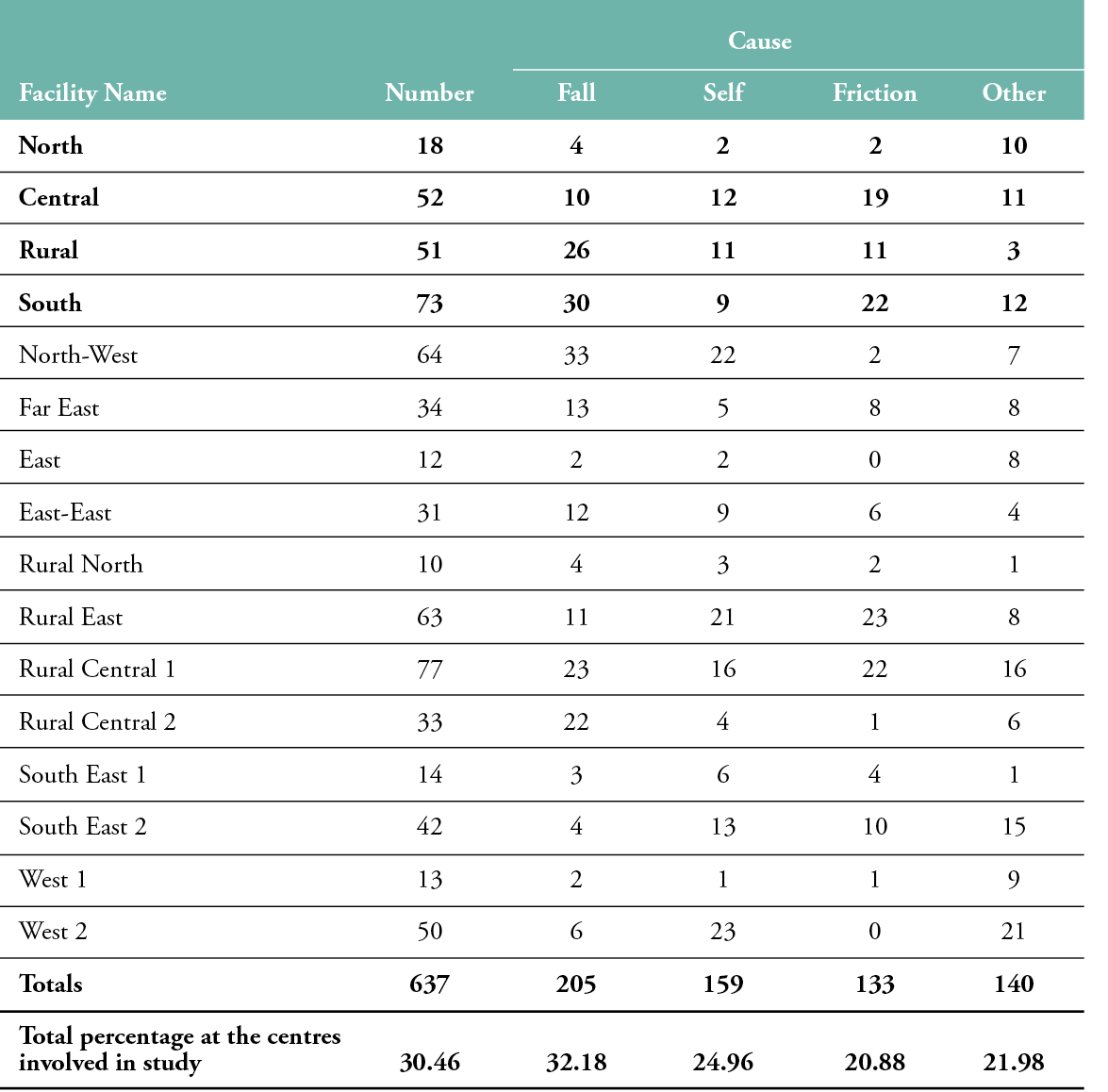
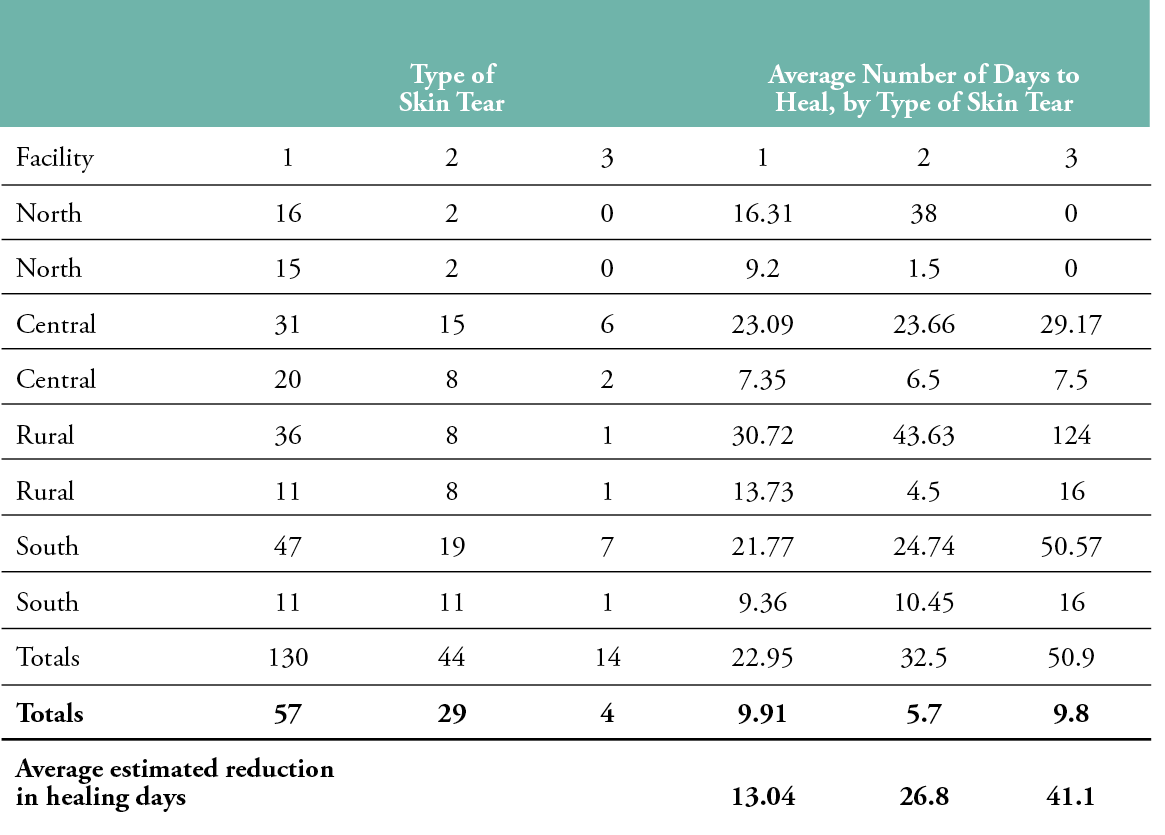
Table 4 shows the skin tear type and the average number of days each type took to heal, before and during the intervention, per facility. Type 1 skin tears were the most common across the four facilities, both before and during the intervention (n=130 vs n=57). Type 2 tears accounted for 44 pre-intervention, compared 29 during the project. Where Type 2 and 3 skin tears were reported, they took, on average, more days to heal during the pre-intervention period (January–February 2021) than afterward. Following implementation of the STWMP, the data for the North, Central and Rural sites show that it took less time to heal Type 2 skin tears than Type 1 wounds. This was demonstrated in the descriptive data on the average healing times when the first responder STWMP was available. Type 1 tears healed an average of 13.04 days faster, Type 2 healed 26.8 days faster and Type 3 wounds healed 41.1 days faster.
Table 4: Average Number of days to heal skin tears, before and during intervention
Skin Tear Types, January–February 2021 (pre-study period): no shading, May–June 2021
(during implementation): shaded, bolded and italics
Economics of the pack
Table 5 shows the estimated cost of the first res-ponder STWMP before and during the evaluation periods for the number of days the resident had a skin tear, as reported by the facility staff. For transparency, these costs were estimated using the total number of days to heal across all four study sites, divided by how often a dressing needed to be changed (every three days), and then multiplied by the cost of a staff member attending a dressing change.
Table 5: Total cost of skin tears
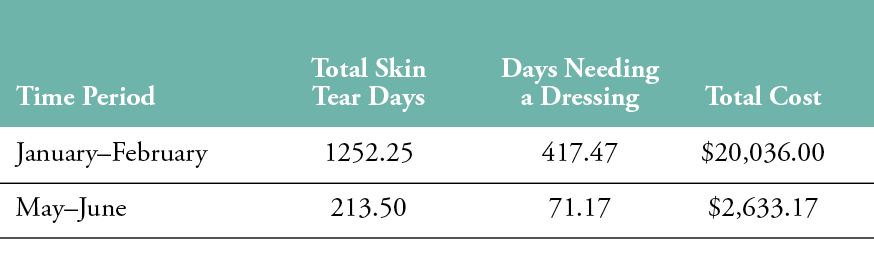
Prior to implementing the STWMP, only regulated workers were responsible for the management of skin tears. This relied on them being notified of the injury, which may have been a number of days after the skin tear was sustained. Our crude estimations of the associated costs equated to: pre-study RN, approximately $35/hr AUD + $15 for normal dressings not in a pack = $50 AUD. During the study, Personal Care Attendant (PCA) approximately $25/hr AUD + $12 STWMP pack= $37 AUD. Therefore, the study showed positive changes, as the savings will scale up with the increased need.
DISCUSSION
Regarding the ratio of unregulated to regulated staff, the audit found that there were four times more unregulated workers for each regulated worker on the day shifts. Overnight, there is usually one regulated worker for a whole site, which, on average, is home to 90 or more residents. The ratios recommended by Health and Human Services (2018)13 are one
regulated nurse to seven residents, plus an additional charge nurse. Overnight, they suggest one regulated nurse to 15 residents. However, anecdotally, the data from this audit seems to reflect the ongoing trends in the sector, which struggles to attract regulated nursing staff. It should also be taken into account that the differences in the suggested and actual ratios reflect the local situation during the COVID-19 pandemic, when it was acknowledged that resources were, and continue to be, prioritised to acute care hospitals over aged care facilities.
It is critical to have support for any actions that can provide a resident-centric model of care; save nurses’ time; and empower unregulated healthcare workers to maintain residents’ safety, prevent infection and achieve better care for all residents’ skin.14 The first responder STWMP appears to be a potential solution for guiding unregulated workers, so that regulated workers have an opportunity to implement care that is evidence-based.
Patient demographics
Like most aged care facilities in Australia and around the world, the most common comorbidities represented in this audit included individuals with dementia and Parkinson’s disease, both of which can increase the incidence of night-time wandering, the risk of falls and a resulting increased risk of skin tears.15 The issue of skin tears is made more complex by existing limits of Certificate III carer education16, which does not include the aetiology and co-morbidities of conditions such as Parkinson’s disease in the syllabus.15
There is clear evidence that there are gaps in the knowledge of regulated health professionals regarding knowledge of the assessment and management of wounds as a whole; furthermore, little is known about the ability of unregulated workers to classify wounds correctly. The consequences of both of these situations are that skin tears are often left untreated.16 The first responder STWMP was designed specifically to overcome this challenge in the aged care sector.
The design of the STWMP, including the steps to take accompanied by images, meant that it can assist unregulated workers, and perhaps regulated healthcare staff with minimal wound experience, in assessing and managing a skin tear in a timelier manner. One observation from the project was that, during the period when the first responder STWMP was made available, healing times decreased across all study sites. If healthcare workers and health professionals address skins tears when they are sustained, the risk of infection and the development of complex wounds are reduced.4 One fundamental aspect of wound management is choosing the correct wound product to decrease the risk of the skin tear becoming chronic. The results of this audit confirmed that, for all skin tear types, the first responder STWMP has the potential to reduce days to healing. Type 3 skin tears, the most severe, had the greatest reduction in average healing days.
Cost of skin tears
Within the aged care sector, cost is of concern, as there is limited government funding, yet there is pressure from families to provide the best care possible, and high-quality care expectations are at the core of every decision.16 The audit results following implementation of the first responder STWMP showed a reduction in the most severe type of skin tear (Type 3) days to heal rate. Based on using the first responder pack, the average time to heal of a Type 3 skin tear went from 50.9 days to 9.8 days. This alludes to a potential reduction in costs across both regulated and unregulated workers, with regards to time and resources. The estimated calculations proffered by this audit suggest that further research is warranted.
Limitations
The project has a number of limitations, the first of which is that unregulated healthcare workers do not report directly using eCase, as wound care is not considered a part of their scope of practice. Therefore, data entry related to eCase was only performed by regulated workers, which could have led to under-reporting, or incorrect skin tear type classification.
It is clear that the audit data provided some detail concerning the introduction of the first responder STWMP, and various levels of education at each site seemed to have decreased both skin tears and healing time, compared to before the study. However, it was difficult to link the data to the specific to which unregulated staff member who was directly rostered at the time. Therefore, when a skin tear was sustained, it was not possible to follow-up with the unregulated staff member for further clarification. There is a need to investigate further the actions or inaction of staff members related to the decision to use, or not use, the first responder STWMP. With this in mind, an additional qualitative study that includes interviews with the cohort of unregulated workers after implementation is underway and may provide more insight. Until that study is complete, conclusions remain speculative.
The findings of this audit have provided preliminary indications that the use of the STWMP shows significant promise for addressing some of the challenges related to the late assessment and management of individuals with skin tears in aged care settings. Further research is needed to explore potential barriers and facilitators of skin tear assessment and management among the unregulated workforce.
IMPLICATIONS FOR CLINICAL PRACTICE
This implementation study provides good indications that a first responder STWMP has the potential to be a solution that can facilitate timely, effective and evidence-based assessment and management of skin tears by aged care regulated nurses and unregulated workers. Therefore, it may offer potential for the wider aged care sector, where there is a need for novel solutions to complex problems. If further evidence shows that unregulated healthcare workers can apply dressings, instead of leaving skin tears untreated and at risk of infection, there is an opportunity to provide better care for all residents. The first responder STWMP may ultimately improve long-term health outcomes for the residential aged care sector by involving all providers in the residents’ model of care.
Declaration of interest
Sentry Medical provided the dressings for the first responder STWMP at no cost to the aged care facilities for the 8-week testing period.
Acknowledgements
Thank you to ISTAP for providing approval to adapt the skin tear guidelines for the STWMP instruction sheet.
Key messages
- An implementation study to show how unregulated workers can contribute to residents’ health care needs to reduce the risk of infection and wound complexity.
- The primary aim of the project was to create a unified first responder skin tear wound treatment that any health care worker could apply to prevent infection and the progression of a skin tear into a chronic or complex wound.
- The first responder skin tear pack reduced overall costs and days with a wound over the study period.
Author(s)
Chloe Jansz, Nurse Practitioner/ Healthcare United Nursing Director, Prof Doc. Candidate, LaTrobe University, Healthcare United
Annette Ross, Executive Director - Quality, Safety & Innovation, Royal Freemasons Aged Care
Sonja Cleary, Professor RMIT University , Dean Learning & Teaching Science & Health Cluster, RMIT University
Correspondence: admin@healthcareunited.com.au
Conflict of interest: None
References
- International Skin Tear Advisory Panel [Internet]. ISTAP Skin Tear Classification. Available at https://www.skintears.org/resources
- LeBlanc K, Campbell K, Wood E, Beeckman D. Best practice recommendations for the prevention and management of skin tears in aged skin. Wounds Int 2018., 29(4):31-39 Available to download from www. woundsinternational.com. doi: 10.1097/WON.0000000000000481
- Rando T, Kang, AC, Guerin, M, Boylan, J, Dyer, A. Simplifying wound dressing selection for residential aged care. J Wound Care 2018; 27(8):504-511.
- Langemo D, Campbell K, Holloway S, LeBlanc K, Tariq G, Beeckman D. Applying frailty syndrome to the skin: A review and guide for prevention and management. Adv Skin Wound Care 2021; 34(8):444–7 doi: 10.1097/01.ASW.0000757392.83467.8a
- Hahnel E, Lichterfeld A, Blume-Peytavi U, Kottner J. The epidemiology of skin conditions in the aged: A systematic review. J Tissue Viability 2017; 26(1):20–8.
- Rayner RL, Carville KJ, Leslie GD, Roberts PA. A review of patient and skin characteristics associated with skin tears. J Wound Care 2015; 24(9):406-414.
- Velnar T, Bailey T, Smrkolj V. The wound healing process: An overview of the cellular and molecular mechanisms. J Int Med Res 2009; 37(5):1528-1542.
- Rayner R, Carville K, Maguire C, Smith J. The STAR classification: Utility for determining healing times and dressing costs associated with skin tear management. Wound Pract Res 2021; 29(4):190–7. https://doi.org/10.33235/wpr.29.4.190-197
- Krzyzaniak N, Scott A, Bakhit M, Bryant A, Taylor M, Del Mar C. Impact of the COVID-19 pandemic on the Australian residential aged care facility (RACF) workforce. Aust J Adv Nurs 2021; 38(3).47-58. https://www.ajan.com.au/index.php/AJAN/article/view/490
- Angel D, Swanson T, Sussman G, Shultz G, Ousey K, Keast, D, et al. IWII: Wound infection in clinical practice. Wounds Int 1(2): 1-19. https://www.woundsinternational.com/resources/details/iwii-wound-infection-clinical-practice.2016
- Rapport F, Clay‐Williams R, Churruca K, Shih P, Hogden A, Braithwaite J. The struggle of translating science into action: Foundational concepts of implementation science. Eval Clin Pract 2018; 24:6. 117-126.
- Casey M, O’ Leary D, Coghlan D. Unpacking action research and implementation science: Implications for nursing. J Adv Nurs 2018; 74(5):1051– 8. https://doi.org/10.1111/jan.13494
- Health and Human Services [Internet]. Skin tears: Standardised care process, 2018. Available at www2.health.vic.gov.au/ageing-and-aged-care/residential-aged-care/safety-and-quality/improving-resident-care/standardised-care-processes
- Dky C, Mclaws M-L, Forsyth DR. COVID-19 in aged care homes: A comparison of effects initial government policies had in the UK (primarily focussing on England) and Australia during the first wave. Int J Qual Health Care 2021;33(1). https://doi.org/10.1093/intqhc/mzab033
- Wilfling D, Dichter MN, Trutschel D, Kopke S. Nurses’ burden caused by sleep disturbances of nursing home residents with dementia: Multicentre cross-sectional study. BMC Nurs 2020; (19):83.
- Weller C, Team V, Sussman G. First-Line interactive wound dressing update: A comprehensive review of the evidence. Front Pharmacol 2020; (11): 155. doi: 10.3389/fphar.2020.00155
